Abstract
Human intestinal spirochaetosis is a well-established micro-organism existing in the colon. It is less commonly seen in the appendix, and rarely presents as acute appendicitis. We present a case of a man presenting with symptoms consistent with acute appendicitis. The literature on spirochaetosis presenting as acute appendicitis is also reviewed.
Keywords: Surgery, General Surgery, Pathology
Background
Human intestinal spirochaetosis is a well-established micro-organism existing in the colon. It is less commonly seen in the appendix, and rarely presents as acute appendicitis. We present a case of man presenting with symptoms consistent with acute appendicitis and review the literature of this relatively rare pathogen. The literature on spirochaetosis presenting as acute appendicitis is also reviewed below.
Case presentation
A 24-year-old man presented with a 2-day history of abdominal pain. This was associated with vomiting, headache and a mild fever. Significant medical history included asthma, and at the time of presentation, he was on a course of prednisolone for a recent attack.
On examination, there was right iliac fossa tenderness and percussion tenderness with a positive Rovsing’s sign. The white cell count was 20.3×109/L, neutrophils 17.0×109/L and C reactive protein 2 mg/L.
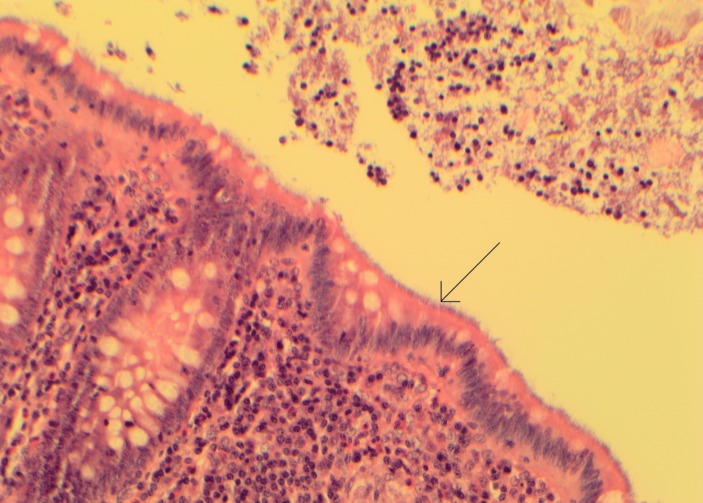
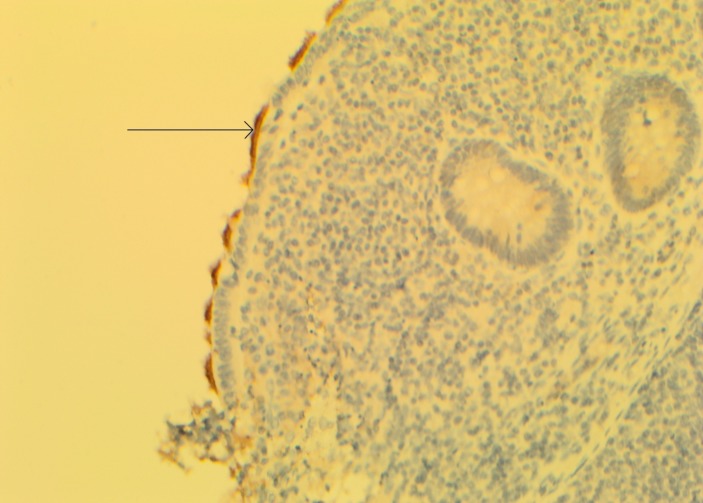
The clinical diagnosis was acute appendicitis and the patient underwent a laparoscopic appendicectomy. Despite the symptoms being suggestive of acute appendicitis, on visualisation, the appendix appeared normal. Histologically, there was no acute inflammation; however, there was widespread colonisation by spirochaetes (figures 1 and 2).
Figure 1.
Appendiceal mucosa colonised with spirochaetes (arrow points to mucosa lined by spirochaetes staining pale purple with H&E histological stain).
Figure 2.
Immunohistochemical staining for spirochaetes (arrow points to spirochaetes, staining positively with specific immunohistochemical stain).
Outcome and follow-up
The patient recovered well postoperatively and was discharged.
Discussion
Intestinal spirochaetosis is a histological diagnosis, confirmed by the presence of spirochaete micro-organisms on the luminal surface of colorectal mucosa.1 In animals, particularly in pigs, it is an established cause of diarrhoea, malnutrition and poor growth.2 In humans, the clinical significance remains unclear.
In humans, Brachyspira pilosicoli and B. aalborgi are the two micro-organisms of the spirochaetes phylum which predominate, typically seen in poor socioeconomic regions, HIV individuals and homosexuals.1 The prevalence depends on the method of detection. Rectal biopsies have demonstrated a prevalence between 2% and 7% in the Western world, compared with much higher levels seen in India and other Asian countries.3–6 Faecal analysis reports detection rates of between 1.1% and 5% in developed countries,1 compared with rates as high as 64.3% in Indian villages.1 7 It has been postulated that the variation between different geographical locations is in part due to varying levels of hygiene and antibiotic use.3
As discussed above, the clinical significance of intestinal spirochaetosis remains up for debate. There are studies which argue that the bacteria exist as commensal organisms and are unlikely to be of pathological significance. These studies report the majority of infected patients as being asymptomatic.1 3 8 However, other studies report symptoms in up to 86% of colonised individuals.9 In patients where the micro-organisms has invaded the epithelium, rather than simply existing on the surface of the luminal epithelium, it is more commonly symptomatic, presenting with chronic watery diarrhoea and abdominal pain, with no other obvious underlying cause.1 9 Other rare cases of abdominal pathology should be ruled out.10 The degree of microscopic invasion into the mucosa, loss of microvilli and microscopic burden of spirochaete organisms on the luminal surface often correlates with the severity of the symptoms.11 In symptomatic individuals, coinfection with other pathogens including Shigella flexneri, Helicobacter pylori, Enterobius vermicularis and Neisseria gonorrhoeae further clouds the pathological significance of spirochaete infection.1
Response to treatment with antibiotic therapy, typically metronidazole targeting the anaerobic spirochaete bacteria, is varied. Some patients have an excellent response, with complete resolution of gastrointestinal symptoms; others remain symptomatic with or without the spirochaete micro-organisms remaining on the luminal epithelial layer.1 12 Despite the varied response, initial treatment with antibiotics is still widely accepted as the initial treatment. Metronidazole is typically used; however, there are reports of macrolide use as well.13
The spirochaete micro-organism has been widely reported as existing in the colorectum8 14 15; however, colonisation of the appendix is less reported, and even less have reported cases of intestinal spirochaetosis presenting as acute appendicitis. To our knowledge, there are only a few publications in the literature which have found patients with spirochaetosis presenting clinically as acute appendicitis. Between 1971 and 1997, three studies were published reporting the presence of spirochaetes in 0.7%–4.8% of confirmed cases of appendicitis. In 0.9%–12.3% of cases, appendicitis was clinically suspected, but the appendix was histologically normal, except for spirochaete colonisation. This latter group has been termed ‘pseudoappendicitis’ by Henrik-Nielsen et al.5 16 17
More recently in 2010, 113 cases of confirmed intestinal spirochaetosis were reported, 16 of which were in the appendix. Of these 16 cases, 5 had confirmed appendicitis.8 In 2012, a case report was published on a histologically confirmed case of appendicitis with spirochaetosis.18
It is evident from the review of the literature, that in individuals with histologically confirmed acute appendicitis, the appendix is rarely concurrently infected with spirochaetes. In comparison, individuals who have pseudoappendicitis, as in the case we present above, the incidence of spirochaete colonisation is slightly higher. It has been postulated that this group present with symptoms of appendicitis due to a rapid and massive colonisation of the appendix by spirochaetes.16
Learning points.
The clinical significance of intestinal spirochaetosis is uncertain.
If symptomatic, intestinal spirochaetosis commonly presents with watery diarrhoea and abdominal pain.
Intestinal spirochaetosis rarely presents as acute appendicitis.
Colonisation of the appendix with spirochaetes may result in pseudoappendicitis.
Footnotes
Contributors: JG: drafted article, collated information and images for case report. CB: critically revised article. DA: critically revised article, chose histology images and drafted histological entry into case report discussion. CP: chose patient for case report, was overall supervisor and critically revised article. All authors have approved final article and are accountable for the article.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Tsinganou E, Gebbers JO. Human intestinal spirochetosis--a review. Ger Med Sci 2010;8:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee JI, McLaren AJ, Lymbery AJ, et al. . Human intestinal spirochetes are distinct from Serpulina hyodysenteriae. J Clin Microbiol 1993;31:16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Mook WN, Koek GH, van der Ven AJ, et al. . Human intestinal spirochaetosis: any clinical significance? Eur J Gastroenterol Hepatol 2004;16:83–7. [DOI] [PubMed] [Google Scholar]
- 4.Surawicz CM, Roberts PL, Rompalo A, et al. . Intestinal spirochetosis in homosexual men. Am J Med 1987;82:587–92. 10.1016/0002-9343(87)90104-5 [DOI] [PubMed] [Google Scholar]
- 5.Lee FD, Kraszewski A, Gordon J, et al. . Intestinal spirochaetosis. Gut 1971;12:126–33. 10.1136/gut.12.2.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nielsen RH, Orholm M, Pedersen JO, et al. . Colorectal spirochetosis: clinical significance of the infestation. Gastroenterology 1983;85:62–7. [PubMed] [Google Scholar]
- 7.Teglbjaerg PS. Intestinal spirochaetosis. Curr Top Pathol 1990;81:247–56. [PubMed] [Google Scholar]
- 8.Carr NJ, Mahajan H, Tan KL, et al. . The histological features of intestinal spirochetosis in a series of 113 patients. Int J Surg Pathol 2010;18:144–8. 10.1177/1066896908330203 [DOI] [PubMed] [Google Scholar]
- 9.Alsaigh N, Fogt F. Intestinal spirochetosis: clinicopathological features with review of the literature. Colorectal Dis 2002;4:97–100. 10.1046/j.1463-1318.2002.00284.x [DOI] [PubMed] [Google Scholar]
- 10.Conzo G, Mauriello C, Gambardella C, et al. . Isolated repeated anastomotic recurrence after sigmoidectomy. World J Gastroenterol 2014;20:16343–8. 10.3748/wjg.v20.i43.16343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper C, Cotton DW, Hudson MJ, et al. . Rectal spirochaetosis in homosexual men: characterisation of the organism and pathophysiology. Genitourin Med 1986;62:47–52. 10.1136/sti.62.1.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Körner M, Gebbers JO. Clinical significance of human intestinal spirochetosis--a morphologic approach. Infection 2003;31:341–9. 10.1007/s15010-003-3145-y [DOI] [PubMed] [Google Scholar]
- 13.Marthinsen L, Willén R, Carlén B, et al. . Intestinal spirochetosis in eight pediatric patients from Southern Sweden. APMIS 2002;110:571–9. [DOI] [PubMed] [Google Scholar]
- 14.Ogata S, Shimizu K, Nakanishi K. Human intestinal spirochetosis: right-side preference in the large intestine. Ann Diagn Pathol 2015;19:414–7. 10.1016/j.anndiagpath.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 15.Lindboe CF, Tostrup NE, Nersund R, et al. . Human intestinal spirochaetosis in mid-Norway. A retrospective histopathological study with clinical correlations. APMIS 1993;101:858–64. [PubMed] [Google Scholar]
- 16.Henrik-Nielsen R, Lundbeck FA, Teglbjaerg PS, et al. . Intestinal spirochetosis of the vermiform appendix. Gastroenterology 1985;88:971–7. 10.1016/S0016-5085(85)80016-0 [DOI] [PubMed] [Google Scholar]
- 17.Yang M, Lapham R. Appendiceal spirochetosis. South Med J 1997;90:30–2. 10.1097/00007611-199701000-00006 [DOI] [PubMed] [Google Scholar]
- 18.Zerhouni S, Melck A, Bugis S. Intestinal spirochetosis presenting as acute appendicitis. J Surg Case Rep 2012;2012:6 10.1093/jscr/2012.3.6 [DOI] [PMC free article] [PubMed] [Google Scholar]