Abstract
Invasive aspergillosis is a life-threatening fungal infection, especially in immunocompromised patients. Pulmonary aspergillosis is the most common type of the infection, while urinary tract infection is relatively rare. Here, we describe a case of a 46-year-old man with chronic renal disease presenting with intermittent abdominal pain. The diagnosis of aspergillosis was established by pathological findings of the fungal ball in the bladder. The patient underwent multiple antimicrobial treatments and surgical interventions and was finally cured by posaconazole.
Keywords: Infectious Diseases, Urinary Tract Infections
Background
Invasive aspergillosis, a severe fungal infection, usually affects patients with immunocompromising conditions such as diabetes mellitus, haematological malignancy and neutropenia.1 Aspergillosis limited to the urinary tract is an uncommon type of invasive aspergillosis, which has been reported to more frequently involve the lung. A combined approach of medical and urological management for renal aspergillosis is recommended. However, no antifungal drug has been advised for urinary tract aspergillosis due to the low urine concentration.2
Posaconazole, an extended-spectrum triazole antifungal agent, has great activity against the Aspergillus and Mucorales.3 Guidelines recommend posaconazole as salvage therapy for invasive pulmonary aspergillosis, but whether it could be used in invasive urinary tract aspergillosis remains uncertain. Here, we report a case of invasive urinary tract aspergillosis with chronic kidney disease that was successfully treated with posaconazole, which suggests that it may be a suitable alternative antifungal agent for urinary tract infections.
Case presentation
A 46-year-old man presenting with intermittent fever, abdominal pain and flocculi in urine for 1 year was admitted in a local hospital.
He provided a history of well-controlled hypertension for 10 months, type 2 insulin-dependent diabetes for 10 years, HBeAg-negative chronic hepatitis B for 20 years and liver cirrhosis for 12 years.
On physical examination, the patient was febrile (T=39°C) with a heart rate of 78 beats/min, blood pressure 111/77 mm Hg and epigastric pain radiating to the lower back, without abdominal mass. Urinalysis showed urine protein (+), red blood cell (RBC) count ×106/LL and white cell (WBC) count 0.3774×109/L. Liver and renal function tests were normal. Serological testing was positive for hepatitis B surface antigen. Renal ultrasonography and CT were normal. Repeated urine cultures were negative for bacterium and fungus. On the basis of clinical presentations and investigations, clinical diagnosis of urinary tract infection was suggested, and empirical antibiotics treatment was initiated with ceftriaxone sodium and levofloxacin for 2 weeks but failed. The patient developed anuria and bilateral double J stents were inserted immediately to relieve obstructions. The repeated urinalysis showed RBC count 39.4×106/L and WBC count 0.4506×109/L, and microscopic examination of floccule in urine revealed fungal hyphae and spores. Imipenem/cilastatin (0.5 g every 8 hours) and caspofungin (50 mg daily) were commenced for 10 days, and imipenem/cilastatin was then switched to cefoperazone sulbactam sodium (2 g every 12 hours) for 3 weeks.
However, the patient still complained of flocculi in the urine and laboratory investigation showed that 3–4 g protein was excreted over 24 hours. A renal biopsy revealed mesangioproliferative glomerulonephritis which indicated chronic kidney disease. Intravenous methylprednisolone (0.2 g daily) was used for 3 days and fluconazole (0.4 g daily) was later added. The patient then developed confusion, sensory disturbances, speech disorder and high blood ammonia level up to 118.5 µg/dL, which indicated hepatic encephalopathy and improved after symptomatic treatments.
Two months later, after the patient experienced sudden difficulty in urination, a cystoscopy was performed showing an intraurethral obstruction by a fungal ball, which was found to consist of fungal hyphae. Indwelling catheters were used to address this. But the patient experienced hypourocrinia, bilateral renal pain, nausea and vomiting; and subsequent ultrasonography revealed mild bilateral hydronephrosis with ureterectasis, which was attributed to fungal obstruction. Bilateral pelviostomy and drainage were performed and antifungal therapy was initiated with intravenous itraconazole (0.2 g daily) for 16 days, after which the patient was switched to caspofungin (50 mg daily) for 21 days. During this time, left ureteral patency and obstruction of the right ureter were observed again.
Three months later, the patient was admitted to our hospital complaining of intermittent flocculi in his urine. Pathological examination of the bladder fungal ball was reviewed and demonstrated that the hyphae are parallel, uniform and septate at regular intervals. Branching is at 45° angle suggestive of invasive aspergillosis (figures 1 and 2). Posaconazole oral suspension was administrated (0.4 g every 12 hours) for 6 months. The efficacy was excellent, and the patient tolerated well during the treatment. He was asymptomatic at 13-month follow-up.
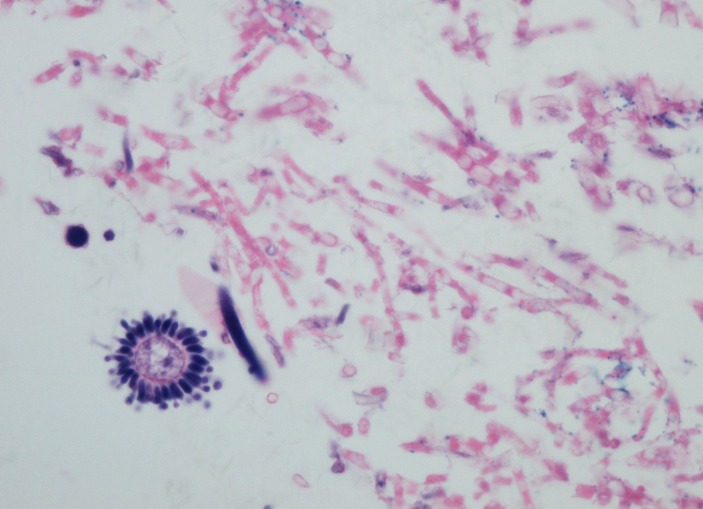
Figure 1.
The conidial head (bottom left) consists of a vesicle with sterigmata and chains of conidia, with hyphae (right) beside it (H&E, 20×).
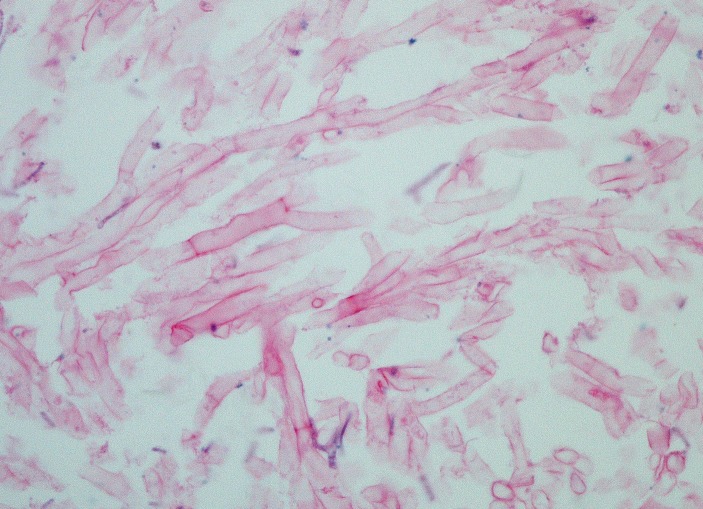
Figure 2.
The hyphae are parallel, uniform and septate at regular intervals. Branching is at 45° angle (H&E, 40×).
Investigations
Laboratory investigation revealed a WBC count of 3.21×109/L. Urinalysis showed urine protein (+), nitrite (2+), leucocyte esterase (4+), RBC count 16.6×106/L and WBC count 1.472×109/L. The liver function tests showed the glutamic-oxaloacetic transaminase level 41 U/L, total bile acid 31 μmol/L, alkaline phosphatase 194 U/L, gamma-glutamyltransferase 194 U/L, total protein 59 g/L, albumin 32 g/L and prealbumin 137 mg/L. The renal function tests showed the serum creatinine level 73 μmol/L. The carbon dioxide combining power was 14.30 mmol/L. The serum CA125 was 46.46 U/mL, CA72-4 26.17 U/mL, cytokeratin 19 fragment 4.02 ng/mL and 1–3-beta-D-glucan measurement was 191.20 pg/mL. Renal ultrasonography showed mild pyelic separation and rigid bladder, without renal abscess. Pathological examination of fungal ball specimens revealed parallel, uniform hyphae suggestive of invasive aspergillosis.
Treatment
On the basis of this evidence, the patient was administered posaconazole 400 mg two times per day for 6 months.
Outcome and follow-up
The patient was discharged on day 14 with a prescription for posaconazole at a dosage of 400 mg two times per day for 6 months. After a follow-up of 13 months, clinical symptoms including dysuria, urination frequency and urgency were relieved. The efficacy was excellent and the patient tolerated the treatment well. Urine cultures were negative and positron emission tomography/ CT showed no abnormalities.
Discussion
Invasive fungal infection of urinary tract, commonly found in immunocompromised patients, remains a great challenge in both the diagnosis and the treatment. There are three main transmission routes, including ascending infections (usually from indwelling bladder catheters), trauma or surgical interventions and haematogenous spread (common in immunocompromised patients). Candida is the most common pathogen, followed by Aspergillus.1 Clinical symptoms vary based on whether the underlying pathology is an Aspergillus abscess or if there is formation of fungal ball. A fungal ball can originate from agglutination of a necrotic tissue nucleus, mucosus debris and foreign or lithiasic debris.4 Typically, if the fungal ball blocks the ureters, the infection manifests as acute onset fever, flank pain, nausea, vomiting, dysuria and haematuria.5 Further diagnosis of the disease is extremely difficult in the early stage, and direct microscopy or culture of floccules in urine could be helpful. This patient’s diagnosis was finally confirmed by pathological examination.
Management of urinary tract aspergillosis remains a therapeutic challenge in clinical settings. Current Infectious Diseases Society of America guidelines recommend a combined therapy of medical and urological management for renal aspergillosis, and voriconazole has been recommended for parenchymal disease.1 However, it is uncertain whether voriconazole, posaconazole, itraconazole, amphotericin B (AmB) formulations and the echinocandins could be used in the treatment of urinary tract aspergillosis as all exhibit poor urinary concentrations.2
Nevertheless, these antifungal regimens have been used successfully in the treatment of urinary tract fungal infection in a few case reports.2 6–10 In our patient, AmB formulations and voriconazole were limited due to its nephrotoxicity and hepatotoxicity, and itraconazole and caspofungin did not show favourable efficacy. Though cystoscopy was performed to remove the fungal ball, the patient still complained of flocculi in the urine, and the obstruction of ureter was revealed by ultrasonography. Posaconazole was then commenced. The patient recovered gradually with no relapse at 13-month follow-up. There are two possible reasons for our successful antifungal treatment. First, recent studies revealed that posaconazole provides a high concentration in renal tissue, and the levels of which could be 40-fold higher than serum levels.11 12 Though it is generally assumed that posaconazole penetration in the urine is low, since the elimination occurs primarily through faecal excretion (77%) and to a lesser extent through urinary excretion (14%), only 0.28% of active drug is eliminated in the urine.13–15 However, owing to the several surgeries our patient underwent, including cystoscopy, bilateral pelviostomy and drainage, which may lead to the physiological barrier of renal parenchyma and renal pelvis broken, the patient might achieve high concentration of posaconazole in urine. The second possible reason was that the source of infection of our patient was both in renal tissue and bladder, since the flocculi were still found in urine after the fungal ball removed. According to a recent study, while fungal balls are found in the ureters, the disease originates in or involves the renal parenchyma, and our successful treatment of posaconazole support it.5
In conclusion, the diagnosis and treatment of invasive urinary tract aspergillosis is still a great challenge. Patients with iterative flocculi in urine were suspected of infection with a non-Candida fungus such as Aspergillus or Mucorales. Further diagnosis depends more on pathological examination and culture. Regarding management, surgical interventions in addition to effective antifungal therapy are strongly recommended. For patients with immunocompromised states, posaconazole may be a suitable alternative antifungal option for urinary tract fungal infections.
Learning points.
Invasive urinary tract aspergillosis is a rare disease and it poses considerable difficulty to diagnosis and treatments.
Physicians should remain on high alert for patients presenting with flocculi in urine.
Posaconazole may be a suitable alternative agent for chronic kidney disease patients with invasive urinary tract aspergillosis.
Footnotes
Contributors: LpZ designed this case. LhZ and HzZ collected the data from medical records and wrote the manuscript. ZqC analysed the pathological findings and revised the discussion. All authors read and approved the final manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Patterson TF, Thompson GR, Denning DW, et al. Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis 2016;63:e1–e60. 10.1093/cid/ciw326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kauffman CA. Diagnosis and management of fungal urinary tract infection. Infect Dis Clin North Am 2014;28:61–74. 10.1016/j.idc.2013.09.004 [DOI] [PubMed] [Google Scholar]
- 3.Campoli P, Perlin DS, Kristof AS, et al. Pharmacokinetics of posaconazole within epithelial cells and fungi: insights into potential mechanisms of action during treatment and prophylaxis. J Infect Dis 2013;208:1717–28. 10.1093/infdis/jit358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Praz V, Burruni R, Meid F, et al. Fungus ball in the urinary tract: Aa rare entity. Can Urol Assoc J 2014;8:E118–20. 10.5489/cuaj.1254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sivasubramanian G, Sobel JD. Urinary Tract Infections Caused by Aspergillus Species. Netherlands: Springer, 2009. [Google Scholar]
- 6.Mathis AS, Shah NK, Friedman GS. Combined use of sirolimus and voriconazole in renal transplantation: a report of two cases. Transplant Proc 2004;36:2708–9. 10.1016/j.transproceed.2004.09.043 [DOI] [PubMed] [Google Scholar]
- 7.Fisher JF, Sobel JD, Kauffman CA, et al. Candida urinary tract infections: treatment. Clin Infect Dis 2011;52(Suppl 6):S457–S466. 10.1093/cid/cir112 [DOI] [PubMed] [Google Scholar]
- 8.Greenberg RN, Mullane K, van Burik JA, et al. Posaconazole as salvage therapy for zygomycosis. Antimicrob Agents Chemother 2006;50:126–33. 10.1128/AAC.50.1.126-133.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Linden E, Restrepo D, Dikman S, et al. Aspergillus infection limited to renal allograft: case report and review of literature. Transpl Infect Dis 2006;8:177–81. 10.1111/j.1399-3062.2006.00134.x [DOI] [PubMed] [Google Scholar]
- 10.Cuervo G, Garcia-Vidal C, Puig-Asensio M, et al. Echinocandins Compared to Fluconazole for Candidemia of a Urinary Tract Source: A Propensity Score Analysis. Clin Infect Dis 2017;64:1374–9. 10.1093/cid/cix033 [DOI] [PubMed] [Google Scholar]
- 11.Campoli P, Al Abdallah Q, Robitaille R, et al. Concentration of antifungal agents within host cell membranes: a new paradigm governing the efficacy of prophylaxis. Antimicrob Agents Chemother 2011;55:5732–9. 10.1128/AAC.00637-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blennow O, Eliasson E, Pettersson T, et al. Posaconazole concentrations in human tissues after allogeneic stem cell transplantation. Antimicrob Agents Chemother 2014;58:4941–3. 10.1128/AAC.03252-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krieter P, Flannery B, Musick T, et al. Disposition of posaconazole following single-dose oral administration in healthy subjects. Antimicrob Agents Chemother 2004;48:3543–51. 10.1128/AAC.48.9.3543-3551.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herbrecht R. Posaconazole: a potent, extended-spectrum triazole anti-fungal for the treatment of serious fungal infections. Int J Clin Pract 2004;58:612–24. 10.1111/j.1368-5031.2004.00167.x [DOI] [PubMed] [Google Scholar]
- 15.Courtney R, Sansone A, Smith W, et al. Posaconazole pharmacokinetics, safety, and tolerability in subjects with varying degrees of chronic renal disease. J Clin Pharmacol 2005;45:185–92. 10.1177/0091270004271402 [DOI] [PubMed] [Google Scholar]