Abstract
Patient: Female, 29
Final Diagnosis: Missed ureteral injury
Symptoms: Abdominal pain • anemia • fever • loose stools
Medication: —
Clinical Procedure: Ureteroureterostomy
Specialty: Urology
Objective:
Mistake in diagnosis
Background:
Ureteral injuries are considered to be uncommon in cases of trauma. The possibility of damage to the ureters may not be considered in the setting of acute trauma when life-threatening injuries take clinical management priority. A case of acute ureteral injury is described in a patient with acute penetrating gunshot abdominal injury that had a delay in diagnosis, with a review of the literature.
Case Report:
A29-year-old woman presented to our hospital with a missed ureteral injury following a self-inflicted gunshot injury to the abdomen. She underwent abdominal computed tomography (CT) imaging and a retrograde pyelogram, which showed complete transection of the left upper ureter with contrast extravasation and the formation of a large urinoma. She underwent a percutaneous nephrostomy and drainage of the urinoma. An end-to-end ureteric anastomosis with excision of the intervening injured ureter, or ureteroureterostomy, was performed three weeks following the diagnosis.
Conclusions:
Ureteral injuries following trauma are rare, but a delay in diagnosis can be associated with clinical morbidity. A high index of clinical suspicion is important for early identification of ureteral injury in cases of acute abdominal trauma.
MeSH Keywords: Abdominal Injuries; Ureter; Wounds, Gunshot
Background
The diagnosis of ureteral injury can be delayed in the setting of acute trauma, as life-threatening injuries take clinical management priority. Also, trauma to the ureter is a rare occurrence in emergency cases, accounting for less than 1% of all cases of urologic trauma [1]. The ureter is protected by its retroperitoneal location and by the surrounding anatomy, especially by the psoas muscles and the bony pelvis [2,3]. Most ureteral injuries are iatrogenic and occur during open, laparoscopic, or ureteroscopic procedures, while less than 25% of ureteral injuries are due to other causes [1,2,4–6].
In the setting of trauma, penetrating injuries account for most cases of ureteral injury, and include gunshot wounds, with the ureter being injured in between 2–5% of abdominal gunshot injuries [2]. However, due to the life-threatening injuries associated with abdominal trauma, up to 38.2% of the ureteral injuries are reported to undergo a delay in diagnosis, which can result in a significant rate of morbidity and even mortality [1,4,7].
A case of acute ureteral injury is described in a patient with acute penetrating gunshot abdominal injury that had a delay in diagnosis, with a review of the literature.
Case Report
A 29-year-old women presented to our hospital 6 weeks following a self-inflicted gunshot injury to the abdomen, with three wounds that involved the epigastrium, the left hypochondrium, and the left lumbar area. She underwent laparotomy at another hospital. Intra-operative findings showed perforation in the antrum of the stomach antrum and multiple small bowel perforations, which all underwent primary surgical repair. There were also bilateral lateral (zone 2) retroperitoneal hematomas, which were non-expanding and non-pulsatile, and were initially not explored.
The patient was transferred to the intensive care unit (ICU), where she later developed a pulmonary embolism (PE) and disseminated intravascular coagulation (DIC). She was managed with blood products and recovered over a period of one month and was discharged home in a stable condition.
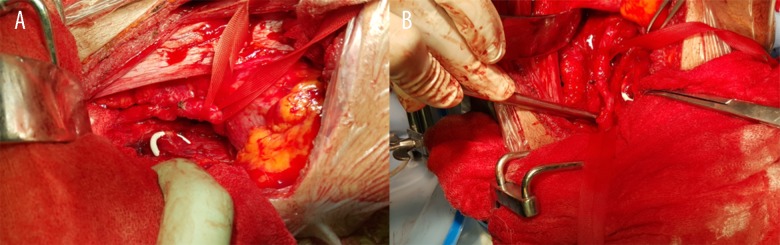
The patient presented two weeks later to a local health center with left iliac fossa (LIF) pain, watery stool, a reduced hemoglobin level, and a raised serum C-reactive protein (CRP). She underwent an abdominal; computed tomography (CT) scan (contrast-enhanced), which showed a large, left-sided, well-enhanced retroperitoneal collection with contrast extravasation into the retroperitoneal space, with the appearance of contrast in the left retroperitoneal space, indicating left ureteral injury with urinoma formation and colonic fistula.
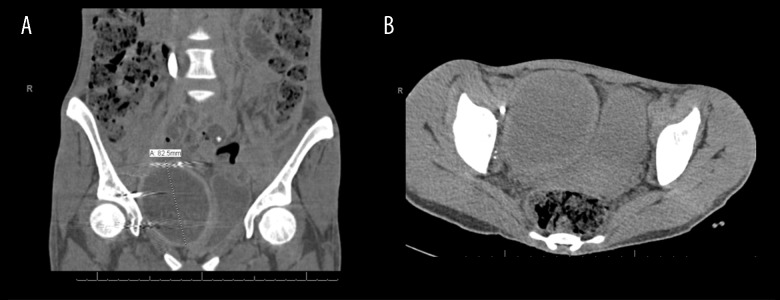
The patient was referred to our trauma center and underwent cystoscopy with a retrograde pyelogram (Figure 1), which showed complete transection of the left upper ureter with contrast extravasation into the retroperitoneal space. She underwent left percutaneous nephrostomy, and a left-sided pigtail drain was inserted into the urinoma. The patient was treated with antibiotics throughout her hospital admission as her sepsis workup investigations showed the presence of a multi-drug-resistant coliform. Clear urine was draining from the urinoma during the patient’s hospital stay.
Figure 1.
Left retrograde pyelogram. Retrograde pyelography shows complete transection of the left upper ureter with contrast extravasation into the retroperitoneal space.
A repeat CT scan one week later showed a reduction in the size of the left-sided urinoma collection. However a further well-defined, peripherally enhancing collection in the right side of the pelvis was identified, compressing the urinary bladder (Figure 2A, 2B). The patient underwent another pigtail drain insertion, which drained only minimal dark reddish fluid, resulting in its removal after 48 hours. The patient was discharged in a stable condition and brought back to the hospital, three weeks later, for elective surgery.
Figure 2.
Computed tomography (CT) of the lower abdomen and pelvis. (A, B) Computed tomography (CT) imaging of the lower abdomen and pelvis shows a further well-defined, peripherally enhancing collection in the left side of the pelvis, compressing the urinary bladder.
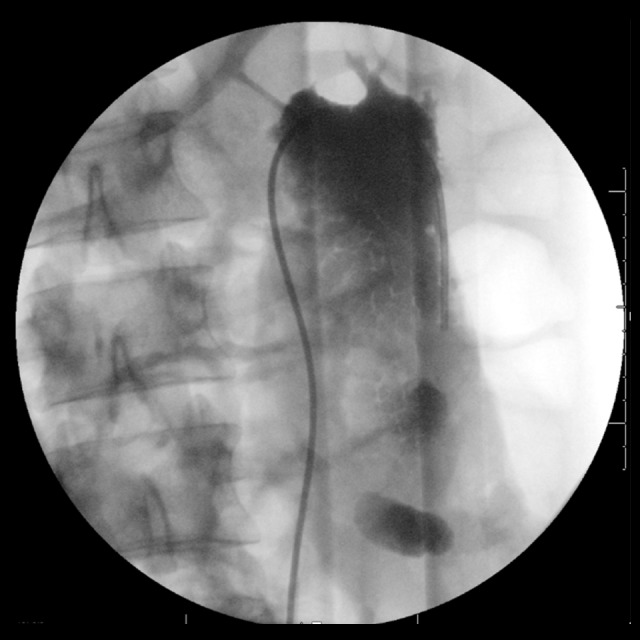
Cystoscopy was done prior to the surgery, which was normal apart from extra-luminal compression of the bladder from the pelvic hematoma. Intraoperatively, a 2.5 cm segment of dense fibrosis was seen in the upper ureter at the site of complete ureteral transection (Figure 3A, 3B). The ureter was mobilized and a left end-to-end ureteric anastomosis with excision of the intervening injured ureter, or ureteroureterostomy, was performed, after spatulation of the ends with a tension-free waterproof anastomosis over a double J stent (DJS). Colonoscopy was done intra-operatively with methylene blue instillation through the pigtail drain to check for any persistent fistula. However, methylene blue testing was negative suggesting spontaneous fistula healing. The patient was discharged from hospital on the third post-operative day, in good condition. She was seen in the outpatient department (OPD) two months later and underwent flexible cystoscopy with removal of the left DJS. The patient failed to show up for further follow-up.
Figure 3.
Intra-operative appearance of the site of transection of the left upper ureter. (A, B) A segment of dense fibrosis was noted intra-operatively at the site of complete transection in the left upper ureter.
Discussion
Patients with ureteral injuries are usually asymptomatic, and the diagnosis can be difficult to make. However, the presence of hematuria should alert the clinician to a possibility of a ureteral injury [2,3,5,8]. Also, patients with penetrating injuries are usually hemodynamically abnormal at the time of presentation and require urgent surgical intervention, that may be without prior computed tomography (CT) scan or intravenous pyelography (IVP), which are investigations that identify up to 90% of ureteral injuries [5]. Since ureteral injuries are infrequent and few surgeons have significant experience with their management, a high index of suspicion is required during surgery.
Bageacu and colleagues divided the retroperitoneal abdominal injuries into three zones that correspond to the major underlying structures that could be injured [9]. The central zone (zone 1) extends from the hiatus of the esophagus to the sacral promontory; the lateral zone (zone 2) extends from the lateral diaphragm to the iliac crests; the pelvic zone (zone 3) contains the retroperitoneal space of the pelvis [9]. The decision to perform surgical exploration in blunt injury depends on the zone, and whether the hematoma is expanding or pulsatile. However, this does not apply to penetrating injury, in which the trajectory of a sharp object can be identified. Therefore, all zones should be explored if involved [9]. In unclear cases, retrograde or antegrade urography is the gold standard for confirmation of the diagnosis [10].
In patients who are hemodynamically normal, the radiological diagnostic modalities of choice for ureteral injury are CT urography and IVP. However, IVP is not usually used in the setting of trauma and is usually used as follow-up after surgical intervention [2]. Although the sensitivity of IVP ranges from between 60–90%, it is associated with high rate of false-negative diagnoses (33%), as a demonstration of urinary extravasation is seen in less than 50% of patients [11]. Findings that increase the suspicion of ureteral injury on CT urography or IVP include delayed excretion of contrast, poor function on one side, hydronephrosis, failure to visualize the entire course of the ureter, and extravasation of the contrast material [2].
With the availability of CT scanning and its sensitivity, contrast-enhanced CT has been the recent diagnostic modality of choice; it is recommended that a five-minute to eight-minute delay is included in the use of contrast-enhanced spiral CT after contrast infusion, to increase the sensitivity [11]. Approximately 80% of injuries can be missed on initial CT and detected only on delayed CT imaging [11]. In hemodynamically normal patients or during surgery, a definitive diagnosis can be achieved by retrograde pyelography via cystoscopy, which is the most accurate method for establishing the diagnosis [2,12]. Also, cystoscopy allows for possible treatment intra-operatively with retrograde indwelling stent placement [12,13].
Ureteral injuries can be missed, or the diagnosis can be delayed, usually due to hemodynamic abnormalities or other distracting injuries or due to a low index of suspicion. Penetrating abdominal injuries affecting the ureters are usually associated with other injuries 90% of cases, and include injuries to the small bowel (75%), colon (40%), and inferior vena cava (IVC) (20%) [5,6]. These injuries can also change the management of the ureteral injuries based on the hemodynamic status, the extent of intra-abdominal organ injuries, and the amount of bleeding [5].
The most common location for ureteral injuries is at the vesico-ureteral junction and the upper part of the ureter [2,12]. However, in case of delayed diagnosis of ureteral injuries, a review of the literature has shown that 59.5% of all the missed ureteral injuries involved the proximal ureter [14]. There are no specific signs and symptoms of ureteral injuries, but some of the patients may present a few days following the injury with lower abdominal pain, prolonged ileus, low-grade fever, nausea, vomiting, persistent hematuria, urinary tract infection (UTI), oliguria, and anuria, with laboratory investigations showing leukocytosis and raised inflammatory markers [12]. In some cases, a transient increase in serum creatinine levels can be found [15]. If ureteral damage remains undiagnosed for up to 6–12 days, patients can develop urinary leakage intra-abdominally, urinary obstruction, urinomas, fistulas, and sepsis [2,3,5,16–18].
In a case of delayed diagnosis or missed diagnosis of ureteral injuries, it is important to divert the urine, which can be achieved with either a retrograde stent placement or percutaneous nephrostomy [4]. Also, drainage of any urinoma or abscess that has formed should be done [1]. Surgical repair of the ureters in such cases is deferred for 6–8 weeks to allow any edema or inflammation to subside. However, there is no evidence to support that there is a worse outcome if the surgical repair is done immediately after identifying the injury [6]. Ureteral contusions are usually treated by stenting [11]. Complete transections of the ureter can be repaired using a tension free, end-to-end, spatulated anastomosis over a ureteral stent. As with all urologic injuries, initial debridement should be conservative in order to preserve all viable tissue. In cases of inadequate ureteral length to re-anastomose, a pediatric feeding tube or other tubes may be placed in the proximal ureter and brought out through the skin for closed drainage. Reconstruction of the ureter can then be performed later.
The surgical approach to ureteral repair can be classified according to the level of injury [11,12]. Distal ureteral injuries can be repaired by performing a ureteroneocystostomy with or without performing a vesico-psoas hitch, with the former preferred in case of a lengthy ureteral defect, which would result in tension if anastomosed directly to the bladder. Ureteroneocystostomy can be performed using different surgical techniques and require stenting of the re-implanted ureter for at least 6 weeks [12]. In performing the vesico-psoas hitch, the bladder is mobilized and hitched to the psoas muscle, followed by ureteral re-implantation [11,12].
Upper and mid-ureteral injuries can be surgically managed using multiple methods. End-to-end ureteric anastomosis with excision of the intervening injured ureter, or ureteroureterostomy can be performed directly, and the anastomosis should be done over a stent. In cases where the distal part of the ureter is not suitable or available for anastomosis, a Boari tabularized bladder flap can be performed. The bladder is opened anteriorly, and a full thickness bladder flap is anastomosed to the proximal ureter. Other less common surgical procedures include transureteroureterostomy, renal autotransplantation, and ureteral substitution with the ileum or appendix [11,12]. Ureteral pelvic junction (UPJ) avulsion injuries should undergo re-anastomosis of the ureter to the renal pelvis, in which case, a stent and drain need to be placed [11].
The importance of early identification of ureteral injuries has been shown to be associated with better clinical outcomes [5]. Early diagnosis is considered to be the single most important prognostic factor [6]. Patients with a delayed diagnosis of ureteral injury have been reported to develop complications in up to 40% of cases, compared with 10% of cases with immediate diagnosis [19]. These complications, associated with diagnostic delay, include infected urinoma formation, hydronephrosis, ureteral fistulae, ureteral strictures, prolonged hospitalization, multiple invasive procedures, acute renal failure, and patient mortality [5,6,16,20].
Conclusions
Ureteral injuries following trauma are rare, but a delay in diagnosis can be associated with clinical morbidity. Patients with ureteral injuries can present with non-specific symptoms including abdominal pain, fever, nausea and vomiting, hematuria, and urinary tract infections. The most sensitive radiological diagnostic test for ureteral injury is retrograde pyelography via cystoscopy, which can show contrast extravasation. An abdominal CT scan can identify the presence of urinoma or an intra-abdominal collection. In unclear cases, retrograde urography can be used as a confirmatory test. A high index of suspicion, for ureteral injury is warranted for patients with penetrating abdominal trauma.
Footnotes
Conflict of interest
None.
References:
- 1.Pereira BM, Ogilvie MP, Gomez-Rodriguez JC, et al. A review of ureteral injuries after external trauma. Scand J Trauma Resusc Emerg Med. 2010;18:6. doi: 10.1186/1757-7241-18-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bent C, Iyngkaran T, Power N, et al. Urological injuries following trauma. Clin Radiol. 2008;63(12):1361–71. doi: 10.1016/j.crad.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Tezval H, Tezval M, Von klot C, et al. Urinary tract injuries in patients with multiple trauma. World J Urol. 2007;25(2):177–84. doi: 10.1007/s00345-007-0154-y. [DOI] [PubMed] [Google Scholar]
- 4.Pirani Y, Talner LB, Culp S. Delayed diagnosis of ureteral injury after gunshot wound to abdomen. Curr Probl Diagn Radiol. 2012;41(4):138–39. doi: 10.1067/j.cpradiol.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 5.Fraga GP, Gustavo MB, Mantovani M, et al. Penetrating ureteral trauma. International Braz J Urol. 2007;33(2):142–50. doi: 10.1590/s1677-55382007000200003. [DOI] [PubMed] [Google Scholar]
- 6.Abboudi H, Kamran A, Royle J, et al. Ureteric injury: A challenging condition to diagnose and manage. Nat Rev Urol. 2013;10(2):108–15. doi: 10.1038/nrurol.2012.254. [DOI] [PubMed] [Google Scholar]
- 7.Siram SM, Gerald SZ, Greene WR, et al. Ureteral trauma: Patterns and mechanisms of injury of an uncommon condition. Am J Surg. 2010;199(4):566–70. doi: 10.1016/j.amjsurg.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Akay AF, Girgin S, Akay H, et al. Gunshot injuries of the ureter: One center 15-years experience. Acta Chir Belg. 2006;106(5):572–77. doi: 10.1080/00015458.2006.11679954. [DOI] [PubMed] [Google Scholar]
- 9.Bageacu S, Kaczmarek D, Porcheron J. Management of traumatic retroperitoneal hematoma. J Chir. 2004;141(4):243–49. doi: 10.1016/s0021-7697(04)95603-7. [DOI] [PubMed] [Google Scholar]
- 10.Lynch TH, Martínez-piñeiro L, Plas E, et al. EAU guidelines on urological trauma. Eur Urol. 2005;47(1):1–15. doi: 10.1016/j.eururo.2004.07.028. [DOI] [PubMed] [Google Scholar]
- 11.Holevar M, Ebert J, Luchette F, et al. Chicago: 2004. The EAST Practice Management Guidelines Work Group (US). Practice management guidelines for the evaluation of genitourinary trauma. Available from: https://www.east.org/education/practice-management-guidelines/genitourinary-trauma-management-of. [Google Scholar]
- 12.Burks FN, Santucci RA. Management of iatrogenic ureteral injury. Ther Adv Urol. 2014;6(3):115–24. doi: 10.1177/1756287214526767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghali AM, El Malik EM, Ibrahim AL, et al. Ureteric injuries: Diagnosis, management, and outcome. J Trauma. 1999;46(1):150–58. doi: 10.1097/00005373-199901000-00026. [DOI] [PubMed] [Google Scholar]
- 14.Kunkle DA, Kansas BT, Pathak A, et al. Delayed diagnosis of traumatic ureteral injuries. J Urol. 2006;176:2503–7. doi: 10.1016/j.juro.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Stanhope CR, Wilson TO, Utz WJ, et al. Suture entrapment and secondary ureteral obstruction. Am J Obstet Gynecol. 1991;164:1513–17. doi: 10.1016/0002-9378(91)91430-5. [DOI] [PubMed] [Google Scholar]
- 16.Brandes S, Coburn M, Armenakas N, et al. Diagnosis and management of ureteric injury: An evidence-based analysis. BJU Int. 2004;94(3):277–89. doi: 10.1111/j.1464-410X.2004.04978.x. [DOI] [PubMed] [Google Scholar]
- 17.Abid AF, Hashem HL. ureteral injuries from gunshots and shells of explosive devices. Urol Ann. 2010;2(1):17–20. doi: 10.4103/0974-7796.62920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carver BS, Bozeman CB, Venable DD. Ureteral injury due to penetrating trauma. South Med J. 2004;97(5):462–64. doi: 10.1097/00007611-200405000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Campbell EW, Jr, Filderman PS, Jacobs SC. Ureteral injury due to blunt and penetrating trauma. Urology. 1992;40(3):216–20. doi: 10.1016/0090-4295(92)90477-e. [DOI] [PubMed] [Google Scholar]
- 20.Azimuddin K1, Ivatury R, Porter J, et al. Damage control in a trauma patient with ureteric injury. J Trauma. 1997;43(6):977–79. doi: 10.1097/00005373-199712000-00022. [DOI] [PubMed] [Google Scholar]