Abstract
Objective
To determine the relationship between performance on a clinical quadriceps activation battery (QAB) with 1) activation measured by doublet interpolation and 2) recovery of quadriceps strength and functional performance following total knee arthroplasty (TKA).
Design
This was a planned secondary analysis of a randomized controlled trial.
Setting
University research laboratory
Participants
One hundred sixty-two patients (aged 63 ± 7 (mean ± sd) years; 89 females) undergoing TKA participated.
Outcome Measures
Patients were classified as HIGH (QAB ≥ 4/6) or LOW (QAB ≤3/6) based upon performance on the QAB measured 4 days after TKA. Differences between groups in activation and recovery at 1, 2, 3, 6, and 12 months after TKA were compared using a repeated measures maximum likelihood model.
Results
The LOW QAB group demonstrated poorer quadriceps activation via doublet interpolation (p=0.01), greater quadriceps strength loss (p=0.01), and greater functional performance decline (all p<0.001) at 1 month after TKA compared to the HIGH QAB group. Differences between LOW and HIGH QAB groups on all measures did not persist at 3 and 12 months (all p>0.05).
Conclusion
Poor performance on the QAB early after TKA is related to poor quadriceps activation and poor recovery in the early postoperative period. Patients in the LOW QAB group took 3 months to recover to the same level as the HIGH QAB group. The QAB may be useful in identifying individuals who need specific interventions to target activation deficits or different care pathways in the early postoperative period to speed recovery after TKA.
Keywords: Prognosis, Outcomes, Rehabilitation
Total knee arthroplasty (TKA) is the most commonly performed surgery in the United States with over 700,000 procedures performed annually.1 While TKA reliably reduces the pain, recovery of strength and function to the level of healthy adults is rare, which predisposes patients to future disability with increasing age.2–5 In the first month following surgery, quadriceps strength decreases by 60% despite initiating rehabilitation immediately after surgery.6–8 Quadriceps strength loss is strongly related to decreased functional performance.9–11 Thus, in the first month following surgery when quadriceps strength loss is greatest, walking distance decreases by 40 % and stair climbing performance decreases by 90% compared to preoperative levels.6 Physical function does recover to preoperative levels by 3 months; however, it remains 30–50% lower than age-matched healthy adults for years after surgery.3–6
Quadriceps strength loss is a primary factor leading to the observed short-term and long-term deficits in functional performance.9–11 In the first month after surgery, when quadriceps strength loss is greatest, the largest factors contributing to this loss are impaired muscle activation from the central nervous system and muscle atrophy.7 Impairments in muscle activation have been shown to be the primary factor at this time point and they account for nearly twice the amount of change in strength as muscle atrophy.7 Quadriceps activation deficits are commonly referred to as arthrogenic muscle inhibition and have been linked to knee pain, swelling, inflammation, and structural damage, all of which are present after TKA.12,13 The exact mechanisms of quadriceps activation deficits have not yet been determined but they are theorized to be caused by a change in the discharge of the sensory receptors of the knee. This alteration may reduce the excitability of the quadriceps α-motor neuron thereby limiting full activation of the muscle.14
Identification of individuals with clinically significant activation deficits is very important because certain interventions, such as progressive resistive exercise, may be less effective in the presence of large activation deficits.15,16 Additionally, there are several interventions that may be more effective at reducing activation deficits or preventing quadriceps strength loss, such as joint aspiration and neuromuscular electrical stimulation (NMES).17,18 Thus, identification of individuals with large activation deficits may allow for more efficient selection of postoperative interventions to improve recovery as well as potentially influence number of visits and length of care needed to achieve maximum benefit. However, quantifying activation deficits early after surgery via laboratory methods such as doublet interpolation presents several challenges clinically including specialized training, equipment expense, patient discomfort with testing, and potential challenges with supramaximal electrical stimulation secondary to the large amount of postoperative swelling. To date, the only clinical measure that has been studied to examine its ability to identify individuals with a quadriceps activation deficit is the brush and sweep test for knee effusion.19 Lynch and colleagues19 demonstrated in individuals after anterior cruciate ligament (ACL) injury that the level of effusion, as determined by the brush and sweep test, was not a significant predictor of quadriceps activation deficits. They theorized that this was potentially due to the variability in time since injury and some individuals may have accommodated to the level of effusion in their knee. Several other unstudied methods have been utilized clinically to assess quadriceps activation in the early postoperative period such as isometric quadriceps contraction (also called quadriceps setting or ‘quad sets’) or ability or time to perform a straight leg raise. However, the ability to perform these tests and their relationship to laboratory measures of quadriceps activation or to recovery of quadriceps strength and function have not been studied. Therefore, the purpose of this study was to determine the relationship between performance on a clinical quadriceps activation battery (QAB) with 1) a laboratory measure of activation (doublet interpolation) and 2) recovery of quadriceps strength and functional performance after TKA. Our hypothesis was that individuals with poor performance on the QAB initially after surgery would have poorer activation, poorer strength recovery, and poorer functional recovery compared to those individuals with higher performance on the QAB in both the short (<3 months) and long term (12 months).
METHODS
Study Design
This study was a planned secondary analysis of a randomized controlled trial that examined the difference between a high-intensity (HI) rehabilitation program compared to a low-intensity (LI) rehabilitation program. Full details of this clinical trial have been published elsewhere.16
Subjects
Patients were consecutively recruited by nine participating orthopedic surgeons from four institutions from August 2011 to November 2014. Patients aged 50 to 85 years were included if they were awaiting a primary, unilateral TKA secondary to knee osteoarthritis (OA). Exclusion criteria were:1) current smoker, 2) current cancer treatment, 3) uncontrolled diabetes (hemoglobin A1c level <7.0), 4) body mass index (BMI) greater than 40 kg/m2, 5) neurological, vascular, or cardiac problems that limited function, 6) discharge to location other than home after surgery (e.g. skilled nursing facility), 7) severe contralateral knee OA (> 5/10 pain with stair climbing) or other orthopedic conditions that limited function and necessitated alternative concurrent intervention (e.g. severe lumbar spinal stenosis, severe hip or ankle OA). Informed consent was obtained from all participants. The study was approved by the University of Colorado Multiple Institutional Review Board and registered at ClinicalTrials.gov (NCT01537328).
Interventions
Following surgery, all patients received inpatient physical therapy twice daily prior to discharge. The HI and LI interventions were initiated 4.2 ± 1.2 (mean ± sd) days after surgery. All patients were seen 2–3 times per week over 11 weeks in an outpatient physical therapy setting for a total of 26 visits. The HI intervention consisted of a progressive resistive exercise program targeting major lower extremity muscle groups and a rapid progression to weight-bearing exercises targeting key activities in addition to balance and agility training. The LI intervention had an initial focus on isometric exercise and active range of motion exercise with a slower progression to weight-bearing exercises and activities compared to the HI intervention. Both interventions included patient education on pain, swelling, and wound management; training on transfers, gait, and stair climbing; range of motion techniques; and instruction in a home exercise program.
Outcomes
All outcomes were assessed 1–2 weeks preoperatively and at 1, 2, 3, 6 and 12 months postoperatively by a blinded outcome assessor. In addition to these testing time points, the QAB was assessed at the initial outpatient physical therapy evaluation (4.2 ± 1.2 days after surgery) by the treating physical therapist.
Quadriceps Activation Battery
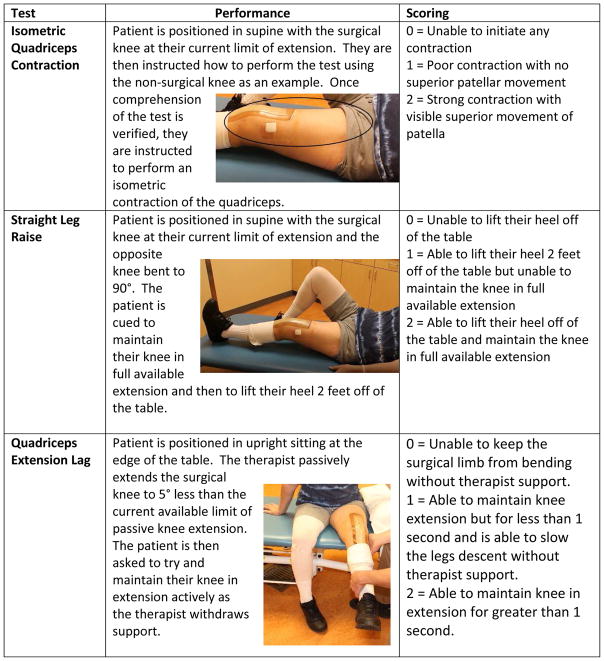
The QAB consisted of three separate clinical tests: isometric quadriceps contraction, straight leg raise, and the quadriceps extension lag test (see Figure 1). Each test is scored on a 3-point scale from 0 (unable to perform) to 2 (able to perform fully). The three tests are summed to determine the final score on the QAB (range 0–6) with higher scores indicating better performance. These three test items were selected for inclusion in the QAB based upon the position of the knee joint, muscles that are preferentially recruited, and type of muscular contraction required. The magnitude of quadriceps activation deficit varies by joint angle and peak inhibition occurs in end range extension in an acutely effused knee.20 This is theorized to result from greater intra-articular pressure which leads to joint capsule distension and reflex inhibition.20 Isometric quadriceps contraction and straight leg raises are commonly performed early postoperative exercises designed to recruit and strengthen the quadriceps. They differ in that isometric quadriceps contraction leads to greater recruitment of the vastus medialis and the straight leg raise leads to greater recruitment of the rectus femoris.21 The straight leg raise test also utilizes a concentric contraction of the rectus femoris muscle and requires maintaining the lower leg in extension against gravity whereas the isometric quadriceps contraction is exclusively isometric in a supported position. The quadriceps extension lag test is a novel testing procedure that was designed to contract the quadriceps muscle isometrically against gravity and if the patient is unable to maintain the knee in the available range of extension to eccentrically control the descent of the lower leg. Eccentric control of quadriceps theoretically requires less motor unit activity than isometric or concentric contractions and evidence suggests that neural control of eccentric contractions, in particular sub-maximal efforts, differs from concentric contractions.22
Figure 1. Clinical quadriceps activation battery test components and scoring.
The clinical quadriceps activation battery (QAB) consisted of three components A) Straight Leg Raise, B) Isometric Quadriceps Contraction, and C) Quadriceps Extension Lag Test. Each component was scored separately on a scale of 0–2 and summed together to yield a final QAB score (range 0–6) with scores ≤3 indicating poorer quadriceps activation.
Quadriceps Strength and Activation
Quadriceps strength was measured utilizing a maximal voluntary isometric contraction (MVIC) and quadriceps activation was quantified using a doublet interpolation test.23 An electromechanical dynamometer (HUMAC NORM, CSMi, Stoughton, MA) was utilized to measure torque while data were acquired with a Biopac Data Acquisition System (Biodex Medical Systems Inc, Shirley, NY) at 2,000 samples per second and analyzed with Acqknowledge software, version 3.8.2 (Biodex Medical Systems Inc). Doublet interpolation testing was carried out utilizing a Grass S48 stimulator and SIU8T stimulus isolation unit (Grass Instruments Co, West Warwick, Rhode Island).
To assess the quadriceps strength, patients were tested in seated position with the knee flexed to 60°. Following a warm-up, they were asked to perform MVIC of the quadriceps with visual and verbal encouragement. Testing was repeated, with one-minute rests between trials, until two trials were within 5% of each other. The highest of the two trials was then normalized to the patient’s body mass.
To assess quadriceps activation, a 2-pulse electrical stimulus (600 μs pulse duration, 100 pulse per second frequency) was delivered to the patient’s quadriceps muscle in a relaxed state. Intensity was then increased in 10-volt increments until the electrically induced torque from the muscle reached a plateau (supramaximal doublet in resting). The patient was then asked to perform a quadriceps MVIC and a supramaximal stimulus was applied during the performance of the MVIC and again immediately afterward when the patient had relaxed his or her quadriceps muscle. Quadriceps activation was calculated with the following formula:
where a is the torque produced by the supramaximal stimulus during MVIC and b is the torque produced by the supramaximal stimulus at rest after the MVIC. A value of 100% represents full voluntary activation of the quadriceps and values less than 100% represent decreased motor unit discharge rates or incomplete motor unit recruitment.23
Functional Performance
Functional performance was assessed utilizing the stair climbing test (SCT), six-minute walk test (6MW), and timed up and go test (TUG). The SCT measures the total amount of time it takes for a patient to ascend and descend a flight of stairs and was assessed on a 12-step (17.1 cm step height) flight of stairs. The 6MW test measures the distance a patient can walk in six-minutes and was assessed with a 30.5m walkway. The TUG measures the amount of time it takes for an individual to rise from a chair (seat height 46cm), walk 3 meters, turn-around, and walk back to the chair and sit down. These measures have been shown to be valid, reliable, and responsive measures to quantify functional performance in individuals after TKA.24
Statistical Analysis
Descriptive statistics were utilized to report patient characteristics and QAB scores over time. Based on a median split of the QAB score at initial evaluation, patients were classified as HIGH (QAB≥4) or LOW (QAB≤3). The difference between the HIGH and LOW QAB groups in outcome measures at 1, 2, 3, 6 and 12 months was estimated using a repeated-measures maximum likelihood, cell means model regressing the measure on the baseline value of the measure, treatment group, sex, clinic site, month, and an indicator for HIGH/LOW QAB. HIGH/LOW QAB differences were evaluated with linear contrasts. Sex and clinic site were included in the model because these variables were used to stratify individuals during the randomization.16 Baseline for each outcome and treatment group were included to improve precision of the model. Data are reported pooling across treatment groups from the main trial because outcomes by treatment group were not different for any outcome measure (p >.0.05). Effect sizes for differences between groups at 1 and 2 months were estimated by Cohen’s d calculated from a least squares regression of the measure on HIGH/LOW QAB controlling for its baseline value, sex, and site..25 Cohen’s d values of 0.20, 0.50, and 0.80 represent small, moderate, and large effect sizes respectively.26 A 2-sided p value of 0.05 was designated a priori for statistical significance. SAS version 9.4 (SAS Institute Inc, Cary, NC) was utilized for all statistical analyses.
RESULTS
Patient characteristics at baseline are described in table 1 and the patient flow diagram is shown in figure 2. The QAB scores by time point are shown in table 2. Greater than 90% of patients scored a 6 on the QAB at the preoperative time point. Greater than 90% of patients scored 5 or 6 on the QAB at 1 month. At the initial outpatient physical therapy evaluation four days after TKA, QAB scores were more evenly distributed and ranged from 0 to 6.
Table 1.
Baseline characteristics (N=162)
| Sex N(%) | |
| Men | 73 (45) |
| Women | 89 (55) |
| Age (years) | 63 (7) |
| BMI (kg/m2) | 30 (5) |
| Stair Climbing Test (s) | 16.8 (8.3) |
| Timed-Up-and-Go Test (s) | 8.9 (2.7) |
| 6-minute Walk Test (m) | 460 (102) |
| Quadriceps Strength (Nm/kg) | 1.2 (0.5) |
| Quadriceps Activation (%) | 71.5 (15.5) |
| High-Intensity Intervention | |
| High QAB N(%) | 35 (41.7) |
| Low QAB N(%) | 49 (58.3) |
| Low-Intensity Intervention | |
| High QAB N(%) | 38 (48.7) |
| Low QAB N(%) | 37 (47.4) |
| Missing N(%) | 3 (3.8) |
Sex is reported as N (%). All other characteristics are reported as mean (sd). Abbreviations: BMI, body mass index; QAB, quadriceps activation battery.
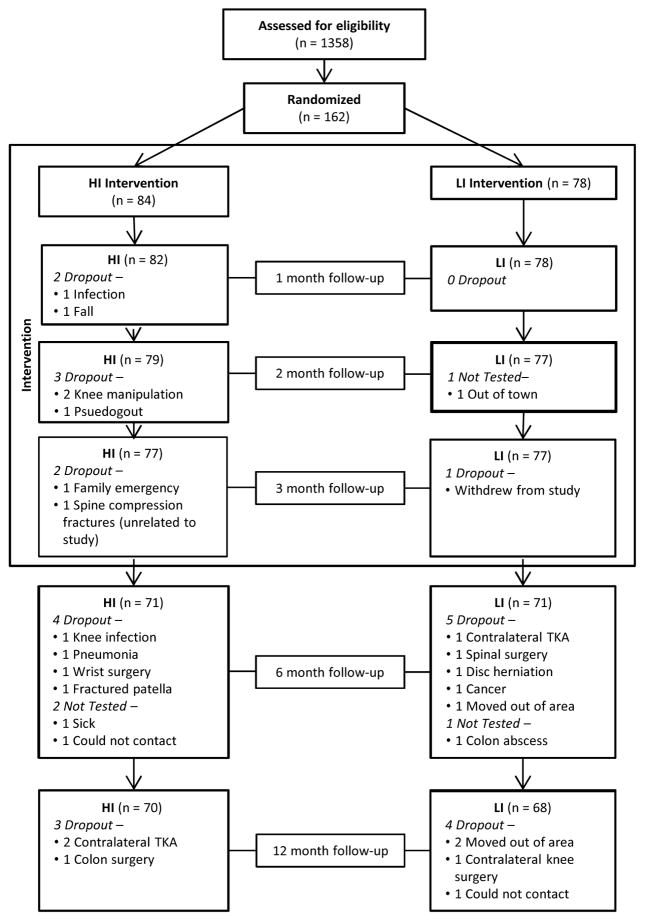
Figure 2.
Flow diagram over the course of the study
Abbreviations: HI=High-intensity intervention group; LI=Low-intensity intervention group.
Table 2.
Quadriceps activation battery scores over time
| QAB Score | Baseline (2 weeks preoperative) N(%) | Initial Postoperative Evaluation (4 days) N(%) | One Month Postoperative N(%) |
|---|---|---|---|
| 0 | 8 (5.0) | ||
| 1 | 25 (15.7) | ||
| 2 | 24 (15.1) | ||
| 3 | 29 (18.2) | ||
| 4 | 1 (0.6) | 24 (15.1) | 4 (2.6) |
| 5 | 14 (8.8) | 25 (15.7) | 59 (38.3) |
| 6 | 144 (90.6) | 24 (15.1) | 91 (59.1) |
Abbreviations: QAB, quadriceps activation battery
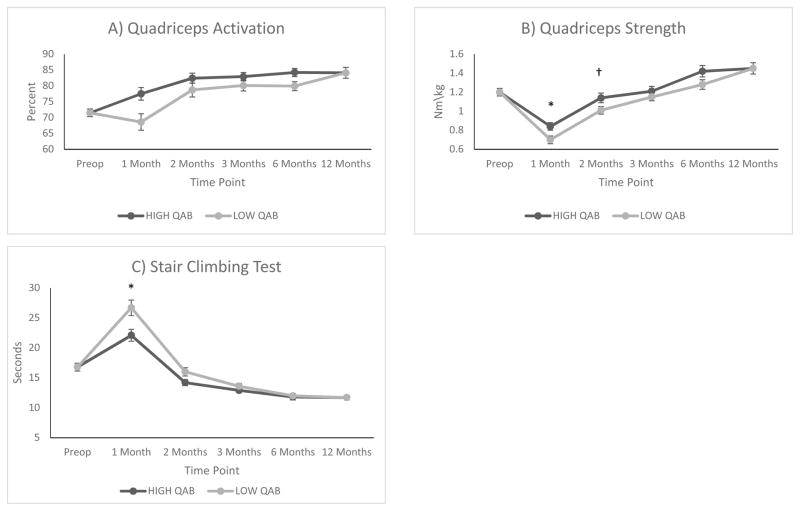
Quadriceps activation, measured via doublet interpolation, by QAB group over time is shown in Figure 3A and reported in Table 3. The LOW QAB group had significantly poorer quadriceps activation at 1 month (p=0.02) compared to the HIGH QAB group. By 2 months, the difference between the LOW QAB group and the HIGH QAB group was no longer significant (p=0.52). There were no differences in activation between groups at 3, 6, and 12 months.
Figure 3.
Quadriceps activation (A), quadriceps strength (B), and stair climbing performance (C) by group over time.
Data are mean ± SE. *Significant difference between groups p<0.05. † p=0.06
Table 3.
Differences in outcomes between groups over time
| Outcome Measure | HIGH QAB 1 Month Mean (SEE) N | LOW QAB 1 Month Mean (SEE) N | Difference Between Groups at 1 month Point estimate (95% CI) p-value | Effect Size | HIGH QAB 2 Months Mean (SEE) N | LOW QAB 2 Months Mean (SEE) N | Difference Between Groups at 2 months Point estimate (95% CI) p-value | Effect Size |
|---|---|---|---|---|---|---|---|---|
| Stair Climbing Test (s) | 21.7 (0.6) 71 |
26.6 (0.6) 86 |
−4.9 (−6.6, −3.3) <0.001 |
0.56 | 14.2 (0.6) 69 |
16.1 (0.6) 84 |
−1.9 (−3.5, −0.3) 0.02 |
0.53 |
| Timed Up and Go Test (s) | 9.7 (0.2) 71 |
11.3 (0.2) 86 |
−1.6 (−2.1, −1.1) <0.001 |
0.61 | 8.0 (0.2) 69 |
8.5 (0.2) 84 |
−0.5 (−1.0, 0.0) 0.04 |
0.39 |
| 6-minute Walk Test (m) | 408 (7) 71 |
372 (6) 86 |
37 (18, 55) <0.001 |
0.54 | 477 (7) 69 |
464 (6) 84 |
13 (−5, 31) 0.16 |
0.18 |
| Quadriceps Strength (nM/kg) | 0.85 (0.04) 71 |
0.73 (0.03) 84 |
0.12 (0.02, 0.21) 0.01 |
0.49 | 1.13 (0.04) 68 |
1.03 (0.03) 84 |
0.09 (0.00, 0.19) 0.06 |
0.40 |
| Activation (%) | 76.0 (1.6) 63 |
70.3 (1.6) 64 |
5.8 (1.2, 10.3) 0.01 |
0.34 | 81.4 (1.7) 62 |
79.9 (1.6) 65 |
1.5 (−3.0, 6.1) 0.52 |
0.17 |
Estimates are based on a Maximum Likelihood model for repeated measures controlling for baseline, sex, site, and treatment group. Abbreviations: QAB, quadriceps activation battery; SEE, standard error of the estimate.
Change in strength and functional performance by QAB groups over time are shown in Figure 3B–C and reported in Table 3. There was a significant difference between HIGH and LOW QAB groups 1 month postoperatively in quadriceps strength (p = 0.01), SCT (p<0.001), TUG (p<0.001) and the 6MW (p<0.001). The LOW QAB group had significantly poorer strength and functional performance compared the HIGH QAB group. The LOW QAB group also had significantly poorer performance on the SCT (p=0.02) and TUG (p=0.04) at 2 months and tended to have poorer quadriceps strength (p=0.06) compared to the HIGH QAB group; however, performance on the 6MW test did not differ between groups (p=0.16). Quadriceps strength did not differ between the HIGH and LOW QAB groups at 3 and 12 months. The LOW QAB group had significantly poorer quadriceps strength compared to the HIGH QAB group at 6 months (p=0.05, 95% CI: 0.0, 0.20). There were no differences in functional performance between groups at 3, 6, or 12 months.
DISCUSSION
The purpose of this study was to determine the relationship between performance on a QAB with 1) a laboratory measure of activation (measured via doublet interpolation) and 2) recovery of quadriceps strength and functional performance after TKA. Performance on the QAB was significantly related to recovery of activation in the early postoperative period as well as strength and functional performance recovery. However, performance on the QAB was not related to longer-term (> 3 months) recovery of activation, strength, or functional performance although this may have been affected by the intensive rehabilitation provided.
Performance on the QAB was largely dependent on the time point it was assessed. Nearly all individuals scored highly on this measure preoperatively and one-month postoperatively, whereas, at the initial evaluation four days after surgery scores for the QAB were evenly distributed across individuals. This suggests that timing of assessment is important in the utilization of this clinical battery because patients will rapidly recover their ability to perform this test battery in the first month after surgery. Given that many patients are beginning post-acute rehabilitation in either skilled nursing, home health, or outpatient rehabilitation settings the first week after surgery, utilization of the QAB should be feasible within these settings during the initial evaluation.
While the LOW QAB group did recover strength and function to the level of the HIGH QAB group by the 3-month postoperative time point, recovery for the LOW QAB group was slower and effect sizes for strength and functional recovery between groups at 1 and 2 months were moderate in size. However, it should be noted that both groups were undergoing physical therapy intervention as part of an ongoing clinical trial. Results from the main trial indicate that outcomes for both the HI and LI groups were superior to what has been observed in related physical therapy research.16 It is possible that recovery of activation, strength, and function may be quite different for those individuals receiving less intervention following surgery. In particular, it is possible that individuals in the LOW QAB group would not have recovered to the level of the HIGH QAB group if they had not received such an extended length of intervention (26 visits over 3 months). Future clinical trials will need to examine the effects of different rehabilitation paradigms on the recovery of activation, strength, and function.
The findings of our study are in contrast to those by Lynch and colleagues who found no relationship between a clinical assessment of effusion (brush and sweep test) and quadriceps activation.19 They hypothesized the lack of relationship between clinically evaluated effusion level and activation may be due to timing of the assessment as they enrolled subjects within 100 days of anterior cruciate injury (ACL). Moreover, they did see a significant effect of time from injury on quadriceps activation levels in their analysis. This may be due to an accommodation effect as a majority of laboratory studies utilize experimentally induced activation deficits via saline injection and examine only short-term effects on activation.27–29 The nervous system may adapt to activation deficits over time.
Given the observed relationship between performance on the QAB and recovery of activation, strength, and function, alternative interventions should be considered in this population in order to facilitate a faster recovery. Several interventions have demonstrated the ability to improve strength and function in individuals with quadriceps activation deficits. Neuromuscular electrical stimulation (NMES) has been shown to produce strength and functional gains in individuals after TKA.18,30 The mechanism by which NMES is thought to produce these changes is that it can directly stimulate α-motor neurons despite activation deficits and thereby decrease muscle atrophy in the longer-term. The results of the present study suggest that NMES may be an effective intervention strategy to target patients with low QAB and potentially increase rate of recovery. Transcutaneous electrical nerve stimulation (TENS) has demonstrated positive effects on improving quadriceps activation in individuals with knee OA, however, the effect of this modality on activation has not been studied in individuals after TKA. 31,32 Swelling has been shown to affect quadriceps strength acutely after TKA and the timing of the QAB at postoperative day four corresponds to near peak swelling levels following surgery.33 Cryotherapy combined with compression is frequently utilized to address swelling and has been shown to reduce activation deficits in individuals with knee OA, however, the effect of this treatment on activation has not been studied in individuals after TKA.32 More invasive methods such as joint aspiration, corticosteroid injections, and anesthetic injections have also demonstrated the ability to decrease activation deficits in individuals after menisectomy, with rheumatoid arthritis, and with knee OA, however, there is an increased risk for infection with these procedures.14
Study Limitations
The primary limitation to this study is the lack of a control group that received no intervention which prevents inference on the effect of the physical therapy on the recovery of activation; thus, the true natural history of activation and functional recovery is unknown.
CONCLUSIONS
In conclusion, poor performance on the QAB early after TKA is related to poor quadriceps activation and poor recovery in the early postoperative period. The QAB may be useful in identifying individuals who need specific interventions to target activation deficits or different care pathways in the early postoperative period to speed recovery after TKA.
HIGHLIGHTS.
The quadriceps activation battery (QAB) is the first clinical battery of tests shown to be related to recovery of activation, strength, and function following total knee arthroplasty (TKA).
Timing of assessment of the QAB is critical as patient performance on the QAB was most informative in the initial postoperative period (4 days after surgery).
The QAB could be utilized to identify individuals who may need specific interventions such as neuromuscular electrical stimulation (NMES) to target activation deficits or prolonged physical therapy intervention to achieve optimal results after TKA.
Acknowledgments
We would like to acknowledge the following individuals for their contributions to this investigation: Tawnya Downing, Allison Gustavson, Jennifer Ivey, Roseann Johnson, Brian Loyd, Michelle Reynolds, Krista Sanchez, Kendall Slutzky, Colorado Joint Replacement, and the patient participants.
Abbreviations
- 6MW
Six-Minute Walk Test
- ACL
Anterior Cruciate Ligament
- BMI
Body Mass Index
- HI
High-Intensity
- LI
Low-Intensity
- MVIC
Maximum Voluntary Isometric Contraction
- NMES
Neuromuscular Electrical Stimulation
- OA
Osteoarthritis
- SCT
Stair Climbing Test
- TKA
Total Knee Arthroplasty
- TUG
Timed Up and Go test
- QAB
Quadriceps Activation Battery
Footnotes
Previous Presentation of the Research:
Loyd BJ, Bade MJ, Paxton RJ, Stackhouse S, Dayton MR, Eckhoff D, Stevens-Lapsley JE. Poor quadriceps activation 72 hours after total knee replacement is related to poor functional performance at 1 month. Abstracted presented at the American Physical Therapy Association Combined Sections Meeting Feb, 2016.
Clinical Trial Registration: Clinicaltrials.gov NCT01537328
Author Disclosures:
Conflict of interest: None of the authors have any conflicts of interest to report
Funding: NIH R01-HD065900, NIH/NCATS UL1-TR001082, NIH T32 AG00279, and the Foundation for Physical Therapy Promotion of Doctoral Studies (PODS) I and II Scholarships
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Most Frequent Operating Room Procedures Performed in US Hospitals, 2003–2012 #186 [Internet] [cited 2016 Jul 8];Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb186-Operating-Room-Procedures-United-States-2012.jsp.
- 2.Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes Before and After Total Knee Arthroplasty Compared to Healthy Adults. J Orthop Sports Phys Ther. 2010;40:559–67. doi: 10.2519/jospt.2010.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.March LM, Cross MJ, Lapsley H, Tribe KL, Courtenay BG, Brooks PM. Outcomes after hip or knee replacement surgery for osteoarthritis. Med J Aust [Internet] 1999 [cited 2016 Jul 8];171. Available from: https://www.mja.com.au/journal/1999/171/5/outcomes-after-hip-or-knee-replacement-surgery-osteoarthritis. [PubMed]
- 4.Walsh M, Woodhouse LJ, Thomas SG, Finch E. Physical Impairments and Functional Limitations: A Comparison of Individuals 1 Year After Total Knee Arthroplasty With Control Subjects. Phys Ther. 1998;78:248–58. doi: 10.1093/ptj/78.3.248. [DOI] [PubMed] [Google Scholar]
- 5.Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB. Does total knee replacement restore normal knee function? Clin Orthop. 2005:157–65. doi: 10.1097/01.blo.0000150130.03519.fb. [DOI] [PubMed] [Google Scholar]
- 6.Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes Before and After Total Knee Arthroplasty Compared to Healthy Adults. J Orthop Sports Phys Ther. 2010;40:559–67. doi: 10.2519/jospt.2010.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mizner RL, Petterson SC, Stevens JE, Vandenborne K, Snyder-Mackler L. Early quadriceps strength loss after total knee arthroplasty. J Bone Jt Surg. 2005;87:1047–1053. doi: 10.2106/JBJS.D.01992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stevens JE, Mizner RL, Snyder-Mackler L. Quadriceps strength and volitional activation before and after total knee arthroplasty for osteoarthritis. J Orthop Res Off Publ Orthop Res Soc. 2003;21:775–9. doi: 10.1016/S0736-0266(03)00052-4. [DOI] [PubMed] [Google Scholar]
- 9.Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther. 2005;35:424–436. doi: 10.2519/jospt.2005.35.7.424. [DOI] [PubMed] [Google Scholar]
- 10.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examing outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech. 2008;23:320–8. doi: 10.1016/j.clinbiomech.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marmon AR, Milcarek BI, Snyder-Mackler L. Associations between knee extensor power and functional performance in patients after total knee arthroplasty and normal controls without knee pain. Int J Sports Phys Ther. 2014;9:168–78. [PMC free article] [PubMed] [Google Scholar]
- 12.Palmieri-Smith RM, Villwock M, Downie B, Hecht G, Zernicke R. Pain and Effusion and Quadriceps Activation and Strength. J Athl Train. 2013;48:186–91. doi: 10.4085/1062-6050-48.2.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurley MV, Jones DW, Newham DJ. Arthrogenic quadriceps inhibition and rehabilitation of patients with extensive traumatic knee injuries. Clin Sci. 1994;86:305–310. doi: 10.1042/cs0860305. [DOI] [PubMed] [Google Scholar]
- 14.Rice DA, McNair PJ. Quadriceps Arthrogenic Muscle Inhibition: Neural Mechanisms and Treatment Perspectives. Semin Arthritis Rheum. 2010;40:250–66. doi: 10.1016/j.semarthrit.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 15.Jakobsen TL, Kehlet H, Husted H, Petersen J, Bandholm T. Early progressive strength training to enhance recovery after fast-track total knee arthroplasty: a randomized controlled trial. Arthritis Care Res. 2014;66:1856–66. doi: 10.1002/acr.22405. [DOI] [PubMed] [Google Scholar]
- 16.Bade M, Struessel T, Dayton M, Foran J, Kim R, Miner T, et al. Early high-intensity versus low-intensity rehabilitation after total knee arthroplasty: a randomized controlled trial. Arthritis Care Res. doi: 10.1002/acr.23139. In Review; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reeves ND, Maffulli N. A case highlighting the influence of knee joint effusion on muscle inhibition and size. Nat Clin Pract Rheumatol. 2008;4:153–8. doi: 10.1038/ncprheum0709. [DOI] [PubMed] [Google Scholar]
- 18.Stevens-Lapsley JE, Balter JE, Wolfe P, Eckhoff DG, Kohrt WM. Early Neuromuscular Electrical Stimulation to Improve Quadriceps Muscle Strength After Total Knee Arthroplasty: A Randomized Controlled Trial. Phys Ther. 2012;92:210–26. doi: 10.2522/ptj.20110124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lynch AD, Logerstedt DS, Axe MJ, Snyder-Mackler L. Quadriceps Activation Failure After Anterior Cruciate Ligament Rupture Is Not Mediated by Knee Joint Effusion. J Orthop Sports Phys Ther. 2012;42:502–10. doi: 10.2519/jospt.2012.3793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stratford P. Electromyography of the Quadriceps Femoris Muscles in Subjects with Normal Knees and Acutely Effused Knees. Phys Ther. 1982;62:279–83. doi: 10.1093/ptj/62.3.279. [DOI] [PubMed] [Google Scholar]
- 21.Soderberg GL, Minor SD, Arnold K, Henry T, Chatterson JK, Poppe DR, et al. Electromyographic Analysis of Knee Exercises in Healthy Subjects and in Patients with Knee Pathologies. Phys Ther. 1987;67:1691–6. doi: 10.1093/ptj/67.11.1691. [DOI] [PubMed] [Google Scholar]
- 22.Duchateau J, Enoka RM. Neural control of lengthening contractions. J Exp Biol. 2016;219:197–204. doi: 10.1242/jeb.123158. [DOI] [PubMed] [Google Scholar]
- 23.Behm DG, St-Pierre DM, Perez D. Muscle inactivation: assessment of interpolated twitch technique. J Appl Physiol Bethesda Md 1985. 1996;81:2267–73. doi: 10.1152/jappl.1996.81.5.2267. [DOI] [PubMed] [Google Scholar]
- 24.Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3. doi: 10.1186/1471-2474-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosnow RL, Rosenthal R. Computing contrasts, effect sizes, and counternulls on other people’s published data: General procedures for research consumers. Psychol Methods. 1996;1:331. [Google Scholar]
- 26.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Eearlbaum Associates; 1988. [Google Scholar]
- 27.Palmieri RM, Weltman A, Edwards JE, Tom JA, Saliba EN, Mistry DJ, et al. Pre-synaptic modulation of quadriceps arthrogenic muscle inhibition. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2005;13:370–6. doi: 10.1007/s00167-004-0547-z. [DOI] [PubMed] [Google Scholar]
- 28.Palmieri RM, Ingersoll CD, Edwards JE, Hoffman MA, Stone MB, Babington JP, et al. Arthrogenic muscle inhibition is not present in the limb contralateral to a simulated knee joint effusion. Am J Phys Med Rehabil. 2003;82:910–6. doi: 10.1097/01.PHM.0000098045.04883.02. [DOI] [PubMed] [Google Scholar]
- 29.Palmieri-Smith RM, Kreinbrink J, Ashton-Miller JA, Wojtys EM. Quadriceps inhibition induced by an experimental knee joint effusion affects knee joint mechanics during a single-legged drop landing. Am J Sports Med. 2007;35:1269–75. doi: 10.1177/0363546506296417. [DOI] [PubMed] [Google Scholar]
- 30.Avramidis K, Karachalios T, Popotonasios K, Sacorafas D, Papathanasiades AA, Malizos KN. Does electric stimulation of the vastus medialis muscle influence rehabilitation after total knee replacement? Orthopedics. 2011;34:175. doi: 10.3928/01477447-20110124-06. [DOI] [PubMed] [Google Scholar]
- 31.Pietrosimone BG, Saliba SA, Hart JM, Hertel J, Kerrigan DC, Ingersoll CD. Effects of transcutaneous electrical nerve stimulation and therapeutic exercise on quadriceps activation in people with tibiofemoral osteoarthritis. J Orthop Sports Phys Ther. 2011;41:4–12. doi: 10.2519/jospt.2011.3447. [DOI] [PubMed] [Google Scholar]
- 32.Pietrosimone BG, Hart JM, Saliba SA, Hertel J, Ingersoll CD. Immediate effects of transcutaneous electrical nerve stimulation and focal knee joint cooling on quadriceps activation. Med Sci Sports Exerc. 2009;41:1175–81. doi: 10.1249/MSS.0b013e3181982557. [DOI] [PubMed] [Google Scholar]
- 33.Pua Y-H. The Time Course of Knee Swelling Post Total Knee Arthroplasty and Its Associations with Quadriceps Strength and Gait Speed. J Arthroplasty. 2015;30:1215–9. doi: 10.1016/j.arth.2015.02.010. [DOI] [PubMed] [Google Scholar]