Abstract
Purpose of Review
The current standard therapy for type 1 diabetes (T1D) is insulin replacement. Autoimmune diseases are typically treated with broad immunosuppression, but this has multiple disadvantages. Induction of antigen-specific tolerance is preferable. The application of nanomedicine to the problem of T1D can take different forms, but one promising way is the development of tolerogenic nanoparticles, the aim of which is to mitigate the islet-destroying autoimmunity. We review the topic and highlight recent strategies to produce tolerogenic nanoparticles for the purpose of treating T1D.
Recent Findings
Several groups are making progress in applying tolerogenic nanoparticles to rodent models of T1D, while others are using nanotechnology to aid other potential T1D treatments such as islet transplant and islet encapsulation.
Summary
The strategies behind how nanoparticles achieve tolerance are varied. It is likely the future will see even greater diversity in tolerance induction strategies as well as a greater focus on how to translate this technology from preclinical use in mice to treatment of T1D in humans.
Keywords: Tolerance, Type 1 diabetes, PLG nanoparticles, Diabetogenic antigens, Regulatory T cells
Introduction
Type 1 diabetes (T1D) is an autoimmune disease in which cells of the immune system destroy the insulin-producing β cells located in the pancreatic islets of Langerhans. Disease onset can occur at any time, but most often happens at 5–7 years of age or puberty, and there are about 280 million cases worldwide today [1, 2]. Currently, the most common therapy for T1D is insulin replacement [1–3]. Unfortunately, insulin replacement is not without its drawbacks. The discomfort of subcutaneous injection and imperfect knowledge of patient glucose levels make managing T1D difficult and suboptimal [2], with significant risk of severe hypoglycemia, so that there is a need for better and more efficient therapies.
Nanotechnology as a concept has been in existence for approximately 60 years, but its application to medical therapy dates back about half that time [4, 5•]. While nanomedicine may have a multitude of incarnations ranging from diagnostic devices to tissue regeneration, much of it has focused on the reformulation and delivery of small molecules or biologic drugs such as proteins or nucleic acids [2, 4, 5•]. More recently, researchers have turned to nanoparticles for immunomodulation and as potential therapeutics for immune-related diseases [4, 5•, 6]. The end goal of many of these new approaches is to reestablish immune tolerance. Tolerance can be defined in many ways [6] but may generally be thought of as a restoration of the balance between the different components of the immune system resulting in inability of the immune system to respond to self-antigens, a process that breaks down when autoimmunity arises.
In this review, we will discuss the application of tolerogenic nanoparticles to islet autoimmunity. We will review the latest views of T1D and some of its treatments, both broad-based immunosuppression and specific tolerogenic therapies, discuss the influence of nanoparticle properties on their ability to induce immunomodulation, and present recent approaches to producing tolerogenic nanoparticles, with a specific focus on those studies that are aimed at developing new treatments for T1D.
Islet Autoimmunity and T1D Treatment
Though it has been difficult to characterize islet autoimmunity in humans and many details of it remain unknown, several features are well accepted. Post-mortem examination of the pancreases of patients at various stages of T1D shows heterogeneous infiltration of CD8+ and CD4+ T cells, macrophages, and B cells [7–11]. Additionally, antibodies with specificities for the β cell antigens insulin, glutamic acid decarboxylase 65 (GAD65), insulinoma-associated protein 2 (IA-2), and zinc transporter 8 (ZnT8) are found in the serum of people with T1D and at risk for T1D [12–17]. In fact, detection of islet-reactive antibodies has become a technique for predicting development of T1D in at-risk subjects [18–20]. However, the islet-reactive antibodies appear to be neither cytotoxic nor pathogenic [21, 22].
An important requirement for the development of tolerance therapies is precise identification of the antigenic targets of autoreactive T cells. CD4+ cells specific for the C-peptide of proinsulin, the precursor to insulin, have been found in the pancreas of a patient with T1D [23]. CD8+ cells specific for the beta cell antigens insulin, islet-glucose-6-phosphatase catalytic subunit-related protein (IGRP), IA-2, GAD65, and prepro islet amyloid protein (ppIAP) have also been found [10]. It has also been found that CD8+ T cells specific for β cell antigens, isolated from the blood of patients with T1D, can kill beta cells [24–26]. Thus far, however, no epitope has been found to be solely responsible for T1D pathogenesis [27] and it is likely that multiple autoantigens are targeted. A recent study of 50 T cell lines from human donors found reactivity to “a broad range of studied native islet antigens and to posttranslationally modified peptides” [28••].
Safety issues prevent obtaining pancreas biopsies from living patients, and fewer people dying of ketoacidosis results in fewer pancreases available post-mortem [1]. The establishment of the Network for Pancreatic Organ Donors with Diabetes (nPOD) in 2007 has increased research access to human pancreas from patients with active disease, which prior to that was a very rare event. Therefore, the vast majority of research on the pathogenesis of T1D has relied on a number of mouse models. Since its development in the 1980s, the non-obese diabetic (NOD) mouse has become a favored model for studying T1D, with spontaneous disease incidence of up to 80–90% in females [1, 29, 30]. Many different T cell autoantigens have been discovered in NOD mice, though insulin, and particularly the Ins B9–23 peptide, seems to be the dominant and initial target [29, 30, 31••, 32••, 33]. While many of these antigens overlap with those found in humans, it is important to note that there are many significant differences between T1D in humans and NOD mice, including disease onset time and amount and morphology of islet infiltration [1, 20]. The utility of the NOD mouse can be seen by the many potential T1D therapies developed using it that have been tested in clinical trials, as has been reviewed elsewhere [29, 34•]. However, it has also been noted that many treatments that were successful in NOD mice have shown little efficacy in humans [1, 29, 34•]. Several groups have also made use of models involving the adoptive transfer of diabetogenic cells into either young NOD or immunocompromised mouse strains, i.e., NOD.Scid, in certain cases leading to a more time-efficient, accelerated model of T1D [35–38]. In these studies, cells with the BDC2.5 T cell receptor (TCR), specific for the beta cell protein chromogranin A (CHrA), are often used [39–41].
Many studies suggest that patients with T1D may retain a significant number of β cells at the time of diagnosis [1], a time when a substantial amount of insulin is still produced [3]. This represents a “window of opportunity” for therapeutic intervention [1]. Clinical trials with immunosuppressants such as cyclosporine, prednisone, and azathioprine near time of T1D onset led to remission, although all have associated adverse effects [27]. Safer methods are being explored, among them monoclonal antibodies against CD3 (teplizumab and otelixizumab) and CD20 (rituximab), and a fusion protein of portions of CTLA-4 and IgG1 (abatacept) [27]. Another potential approach is targeting microbiota and the related interaction with the innate immune system [30], including, for example, administration of the antibiotic vancomycin [42]. It has been noted that general immunosuppression does not cure underlying autoimmunity [43–45]. Therefore, antigen-specific tolerance that does not affect the rest of the immune system and would avoid side effects is a preferable alternative [46].
Several tolerance approaches used for the treatment of T1D are summarized in Table 1. One involves the administration of soluble antigens, as has been done with GAD, insulin, and proinsulin, delivered through a variety of routes, including intraperitoneal (i.p.), intravenous (i.v.), intranasal (i.n.), oral, and subcutaneous (s.c.) [43]. Preclinical and clinical trials using tolerance approaches have proven largely ineffective [47–58]. Significantly, s.c. or i.v. infusion of BDC2.5 mimotopes to either NOD mice or BDC2.5 transgenic mice was able to protect against T1D development [60, 61]. Another approach is DNA vaccination, using either plasmid DNA or viral vectors. Thus far, their clinical progress has been limited, though at least plasmid vaccination is noted for its economy and safety [43]. Finally, cell-based therapies have shown potential as T1D therapies. Regulatory T cells (Tregs) have been shown to be effective in NOD mice [62–64] and recent clinical trials show they are well tolerated in humans [65•], but there is still concern with the plasticity of Tregs and their possible reversion to effector cell phenotypes. Another cell-based technique is to use diabetogenic antigens linked to apoptotic cells targeting the body’s natural tolerogenic clearance pathways. These have proven protective in NOD [32••, 59, 66], transgenic NOD [67], and adoptive transfer T1D mouse models [66].
Table 1.
Summary of non-nanoparticle antigen-specific therapies tested for treatment of T1D
| Antigen | Treatment method | References |
|---|---|---|
| GAD | Soluble Ag | [43, 47–53] |
| DNA vaccination | [43] | |
| Insulin and proinsulin | Soluble Ag | [43, 54–58] |
| DNA vaccination | [43] | |
| Cell-based | [32••, 43, 59] | |
| BDC2.5 mimotopes | Soluble Ag | [43, 60, 61] |
| Cell-based/Treg | [43, 62] | |
| Other cell-based | Cell-based/Treg | [43, 63, 64, 65•, 66, 67] |
Nanoparticles and the Immune System
An examination of tolerogenic nanoparticles requires understanding of their inherent properties which determine how they interact with the immune system. Notable ones include size, charge, and shape, as well as composition of the resulting protein corona. An additional consideration concerns the route of nanoparticle administration.
The biodistribution of administered particles in the “nano-” range (1–1500 nm) [5•] depends largely on a convolution of particle size and route of administration. Subcutaneous, intramuscular, intradermal, and mucosal injection leads to interaction with the lymphatic system and, ultimately, transport to the draining lymph nodes. Smaller particles (< 100–200 nm) drain there freely. Larger particles (> 100–200 nm) must be transported there by APCs [4, 5•, 68, 69]. Particles less than 30 nm seem to be able to escape the lymph node once there [70].
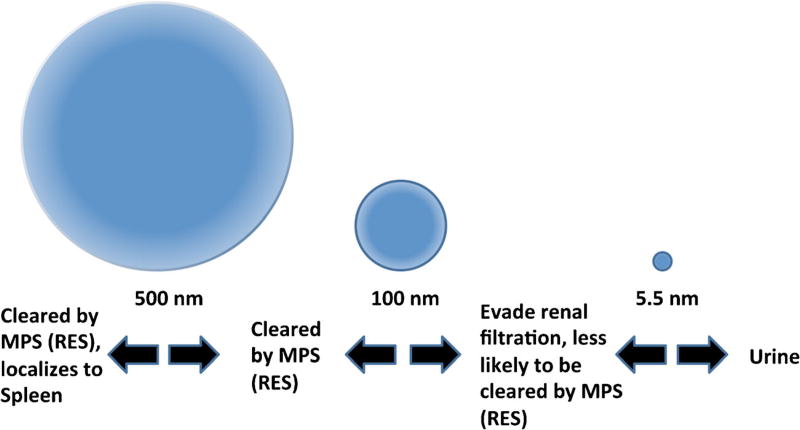
Systemic administration of nanoparticles (Fig. 1) favors accumulation in the organs and tissues such as the spleen, bone marrow, liver, lungs, and kidneys [6, 71]. The site of accumulation is also dependent on particle size as particles < 100 nm can evade clearance by the reticuloendothelial system (RES), a.k.a. the mononuclear phagocyte system [72]. Particles < 5.5 nm undergo renal filtration and may be excreted via the urine [73]. Nanoparticle size also impacts which cells nanoparticles interact with. Dendritic cells preferentially internalize smaller-sized particles, while macrophages tend to take up larger ones [72].
Fig. 1.
Effect of nanoparticle size on biodistribution following systemic administration. MPS mononuclear phagocyte system, RES reticuloendothelial system
Nanoparticle charge can be influenced by surfactants and other coating materials, thereby allowing manipulation of their interaction with the immune system [4]. Cationic particles are more likely to elicit a Th1 response, be taken up by dendritic cells, and engage the MHC class I loading pathway following phagocytosis [4, 74–78], but they have also potentially toxic properties [79, 80]. Conversely, anionic particles exhibit low toxicity in a number of studies [81–86] and associate with the macrophage scavenger receptor MARCO favoring tolerance induction [4, 87].
Various studies have shown that nanoparticle shape and structure are also important in determining the favorability and nature of nanoparticle uptake by cells [88, 89]. Furthermore, the shape/structure of a nanoparticle can also be important for interaction with the immune system, especially in terms of proper conformational display of an antigen in vaccine particles [90–94].
Lastly, the interaction of nanoparticles with biomolecules following administrations is important to consider. For instance, it is thought that the corona can have an effect on important characteristics such as cellular uptake and biodistribution [95]. Though multiple models of the protein corona have been proposed, one recent study suggests that it forms early and is mostly stable in composition 2 min following formation [96]. Another study stressed the influence of nanoparticle size and charge on the corona’s protein composition [97]. Additionally, nanoparticles decorated with antigen may attract antibodies in pre-sensitized individuals, leading to anaphylaxis in certain cases [98•].
Tolerogenic Nanoparticles
The tolerogenic nanoparticles we review here can be broadly separated into two categories: (1) carrier particles that target or reformulate immunomodulatory agents and (2) antigen or disease-specific nanoparticles. Many of the former have been reviewed elsewhere [6, 71, 99], but certain examples merit repeating here. Phillips et al. were able to incorporate antisense oligonucleotides for the costimulatory molecules CD40, CD80, and CD86 within PEG/PVP nano/microparticles, in order to convert DCs uptaking them to a suppressive phenotype [100]. Leuschner et al. used small lipid nanoparticles to deliver small interfering ribonucleic acid (siRNA) to inflammatory monocytes, in order to silence expression of the chemokine receptor CCR2, thus limiting their recruitment to tissues [101]. Wang et al. synthesized nanoparticles consisting of a dextran-coated iron oxide core labeled with Cy5.5 and conjugated to siRNA targeting β2 microglobulin to downregulate MHC class I expression as well as acting as a fluorescent and magnetic detection probe [102]. Lastly, Shah et al. loaded diblock polymer-based nanoparticles with the soluble immunosuppressant molecule rapamycin in order to limit its exposure to the kidneys and provide slow release, thereby reducing its toxicity [103]. Although not directly related to T1D, the rapamycin-loaded nanoparticles showed signs of being as or more effective than free rapamycin as a therapeutic for Sjogren syndrome, another autoimmune disease that uses the NOD mouse as a spontaneous model, with the additional effect of reduced toxicity.
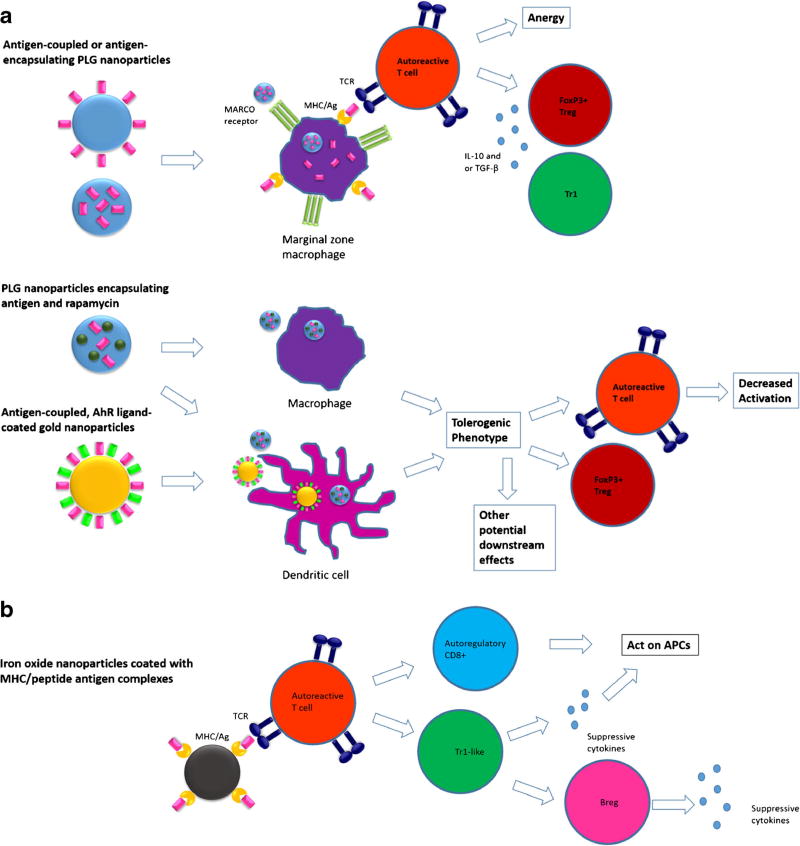
Other studies have made use of nanoparticle strategies that are specific or related to particular autoantigens (Table 2 and Fig. 2). One approach made use of iron oxide nanoparticles coated with major histocompatibility complex (MHC) class I or II molecules loaded with peptides related to autoimmune disease [104, 105••, 106]. This resulted in the expansion of cognate cells with regulatory potential present as part of a negative feedback loop in response to the autoantigen [104] or conversion of effector/memory T cells into regulatory TR1-like cells [105••]. An advantage of this technique is that, while it requires the presence of cells specific for and experienced with the antigen/peptide loaded onto the MHC molecule, it is not antigen specific. Instead, the authors classify it as “disease specific.” This can be seen as a benefit because it requires no knowledge of the antigen’s role in disease pathogenesis or progression. When the particles were coated with MHC II molecules, they showed efficacy in multiple disease models, including experimental autoimmune encephalomyelitis (EAE) and collagen-induced arthritis (CIA) [105••]. Both the MHC I and MHC II approach were also tested in models of T1D [104, 105••], as will be described in the next section. An added benefit is that the degradation of the iron oxide particles will fold into natural iron metabolism pathways and, indeed, initial tests show that the particles have low potential for dangerous side effects [106] and do not suppress the ability of the immune system to clear a pathogen [105••].
Table 2.
Summary of antigen- or disease-specific tolerogenic nanoparticle strategies
| Approach | Disease models | References |
|---|---|---|
| Iron oxide-pMHC | EAE, T1D, CIA | [104, 105••, 106] |
| Peptide-HLA/IgM-epoxy | N/A | [107, 108] |
| PLG nanoparticles encapsulating antigen and rapamycin | EAE, allergy/hypersensitivity, factor VIII tolerance | [109, 110] |
| Gold PEG-Ag-ITE | EAE, T1D | [111, 112••] |
| Lipid Ag-Siglec C or CD22 | Factor VIII tolerance | [113, 114] |
| PLG coated with RBC membrane | Pathogenic antibodies | [115] |
| Carboxylated PLG nanoparticles coupled with or encapsulating antigen | Allergy, EAE, T1D, bone marrow transplantation, islet transplantation | [98•, 116••, 117••, 118••, 119•, 120••, 121•] |
Italicized text indicates studies relevant to T1D
Fig. 2.
Proposed mechanisms of tolerance induction of selected tolerogenic nanoparticle treatments. a Nanoparticles targeting APCs. Top: MARCO receptor dependent uptake of antigen-coupled and antigen-encapsulating PLG [98•, 116••, 117••, 118••, 119•, 120••, 121•, 122]. Middle: PLG encapsulating both antigen and rapamycin [109, 110]. Bottom: gold nanoparticles decorated with both antigen and AhR ligand [111, 112••]. b Iron oxide nanoparticles coated with peptide-MHC that interact directly with T cells to expand autoregulatory cell populations [104, 105••, 106]. APC antigen presenting cell, PLG poly(lactide-co-glycolide), AhR aryl hydrocarbon receptor, MHC major histocompatibility complex
Another approach used gold particles surrounded by polyethylene glycol (PEG) and loaded with both the EAE T cell epitope myelin oligodendrocyte glycoprotein residues 35 to 55 (MOG35–55) and a small molecule aryl hydrocarbon receptor (AhR) ligand [111]. DCs were shown to take up the nanoparticles and subsequently expanded Foxp3+ Tregs in vitro. This approach was shown to reduce severity in EAE and the mechanism of action was shown to be related to the presence of Foxp3+ Tregs. It was later extended to tolerance induction in the NOD model of T1D [112••], also described in the next section.
Other studies employing antigen-specific tolerogenic nanoparticles have made use of such diverse strategies as co-encapsulation of autoantigens with rapamycin in poly(lactide-co-glycolide) (PLG) nanoparticles [109, 110], decoration of liposomal nanoparticles with antigen and inhibitory co-receptor ligands [113, 114], coating PLG nanoparticles with red blood cell membranes [115], and coupling both peptide-loaded HLA and apoptosis-inducing IgM to epoxy beads [107, 108].
Lastly, our group and collaborators have used highly negatively charged biodegradable PLG nanoparticles to treat a variety of mouse models of immune-related diseases. Both antigen-conjugated and antigen-encapsulating particles have been used in Th1/Th17-mediated EAE [116••, 117••, 118••], Th2-mediated allergic airway inflammation [98•], and minor antigen mismatched bone marrow transplant [119•]. The exact mechanisms behind the tolerance induction in this model are still under investigation, but it is thought that intravenous administration leads to uptake of the carboxylated PLG nanoparticles by splenic marginal zone macrophages via the MARCO scavenger receptor, thereafter triggering various tolerogenic pathways including cell-intrinsic anergy and the activation of Foxp3+ Tregs and IL-10-producing Tr1 cells. A recent study, however, has highlighted the importance of liver macrophages in addition to those in the spleen [118••].
Application of Tolerogenic Nanoparticles to T1D
Several strategies to reformulate immunomodulatory agents using nanoparticles have shown efficacy in T1D models. For example, the nano/microparticles described by Phillips et al. [100] prevented or reversed disease in NOD mice and prevented it when T cells from treated mice were co-transferred with NOD diabetogenic cells into NOD.Scid mice.
Antigen-specific therapies have also been applied to the treatment of T1D. The nanoparticles used by Tsai et al. [104] were able to protect against development of T1D in young NOD mice, reverse recent-onset NOD T1D, and restore normal glucose levels in a humanized mouse model. The particles interacted directly with low-avidity CD8+ T cells and expanded them into a population of regulatory CD8+ T cells that prevented or reversed disease. Building on these results, Clemente-Casares et al. [105••] expanded TR1-like cells out of antigen-experienced CD4+ T cells and eventually created a “regulatory network” that also included regulatory B cells and was able to reverse hyperglycemia in NOD mice and prevent its onset in adoptive transfer models involving NOD.Scid mice.
Yeste et al. [112••] used gold nanoparticles coated with PEG, proinsulin, and the tolerogenic AhR ligand ITE to target dendritic cells. The induced tolerogenic phenotype of the DCs in turn led to induction of CD4+ Treg cells which were able to suppress T1D onset when administered to NOD mice at 8 weeks of age in both spontaneous and cyclophosphamide-accelerated models. Additionally, bone marrow-derived dendritic cells (BMDC) that had been incubated in vitro with the nanoparticles were able to reduce T1D development in the spontaneous NOD model. Perhaps most interestingly, the nanoparticles used in this study were also incubated in vitro with human dendritic cells (hDCs), swapping out insulin for the human T1D antigen GAD555–567. Measurements of gene expression and costimulatory cell surface markers suggested that a tolerogenic phenotype was induced in hDCs as well. Subsequently, the treated hDCs were able to decrease IFN-γ secretion in a human GAD-specific CD4+ T cell.
Our group has used insulin and the P31 CHrA mimetope of transgenic BDC2.5 CD4+ T cells in various formulations to treat T1D in two different mouse models [120••]. P31 coupled to apoptotic splenocytes was able to delay and significantly reduce spontaneous T1D onset in NOD mice and a single intravenous infusion was enough to protect NOD.Scid mice from hyperglycemia for 90 days following adoptive transfer of BDC2.5 cells. Envisioning clinical translation of this tolerance induction pathway, we began to focus instead on biodegradable PLG nanoparticles as antigen-carriers. P31-coupled or P31-encapsulating nanoparticles were able to protect against adoptive transfer mediated T1D by sequestering autoreactive T cells in the spleen and decreasing inflammation in the pancreas. Tolerization was shown to be mediated by PD-L1 and CTLA-4 signaling and long-term maintenance of tolerance was found to depend on the induction of Tregs. We have been further able to show similar efficacy using the same approach with a mimotope of CD8+ NY8.3 transgenic T cells.
The approach of Yeste [112••], as well as our group’s research, indicates the need for loading a tolerogenic nanoparticle with insulin when used in the NOD spontaneous onset model. Indeed, when apoptotic splenocytes were used as the antigen carrier, only insulin and InsB9–23 proved effective in preventing disease [32••]. Furthermore, only full-length insulin was fully tolerogenic when the particles were administered later in life (19–21 weeks of age). Data from our group has shown that nanoparticles which encapsulate antigen may be preferable to ones in which the antigen is displayed on the particle surface in terms of patient safety [98•]. Taken together, this means a nanoparticle that encapsulates full-length insulin or proinsulin is a promising therapeutic for testing in the NOD mouse model. While encapsulating insulin remains challenging, efforts are underway to optimize its loading while still controlling nanoparticle size [123].
Finally, nanoparticles may be used in tolerance induction in conjunction with pancreatic islet cell transplantation. Transplant of either stem cell or deceased donor origin islet cells is a promising technique for curing T1D, especially for those suffering from severe hypoglycemia. Sadly, however, recipients of allogeneic islet grafts require lifelong immunosuppression to avoid host rejection of the transplanted cells [3, 46]. Our group and collaborators have explored the use of negatively charged antigen-coupled or encapsulating nanoparticles to induce tolerance in transplant models [122] and have used ECDI-treated donor splenocytes to tolerize recipients of islet transplants [124•]. A recent study investigated the feasibility of using donor antigen-coupled PLG nanoparticles in place of apoptotic cells. The treatment was successful in producing tolerance in about 20% of recipient mice. Adding a small dose of rapamycin to the nanoparticle treatment increased that number to approximately 60% [121•]. Wang et al. [102] used the previously described magnetic nanoparticles conjugated to siRNA to inhibit rejection in a kind of xenograft of human islet to NOD.Scid mice reconstituted with NOD splenocytes. Another potential application of nanotechnology to islet transplant is the encapsulation of islets using engineered capsules to protect the islet from an immune response. A comprehensive discussion of this approach can be found elsewhere [125], but two key points can be addressed. Firstly, one of the most pressing concerns is the need for precise control of pore size in the capsule material to protect from immune components but also to allow for proper β cell function and viability. Additionally, materials need to be engineered to promote vascularization and prevent fibrosis at the site of the transplant.
Conclusions and Future Directions
The uptake of nanoparticles by phagocytic cells makes them a natural choice for testing as tolerogenic agents. The properties of nanoparticles, including size, charge, and shape, as well as their route of administration, may be altered to specifically target their effect to one or several populations of immune cells. Here, we have reviewed approaches using nanoparticles that aim to induce antigen- or disease-specific tolerance, particularly in regards to treatment of T1D. For many of the remaining studies referenced in this manuscript that have not been tested in models of T1D, there is no reason why they cannot be modified to blunt, prevent, or delay islet cell-directed autoimmunity.
Given the increasing uses in which nanotechnology is being employed in the medical arena, it is likely that future development of tolerogenic nanoparticles will not be limited to simply abrogating islet autoimmunity. Innovative applications, such as the induction of donor-specific tolerance in order to allow pancreas or islet transplant, may be used either alone or in concert with autoantigen-specific tolerance. Future work in this area is also likely to focus on considerations not discussed in this review, such as the safety versus toxicity of nanoparticles, their cost benefit, and the ability of their manufacture to be scaled up to industry levels. The very fact that these concerns are being addressed demonstrates the translational potential of this promising new technology.
Acknowledgments
Stephen D. Miller reports grants and personal fees from Cour Pharmaceutical Development Co. In addition, Dr. Miller has a patent US 14/410,011 issued.
Footnotes
Compliance with Ethical Standards
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Conflict of Interest Tobias Neef declares that he has no conflict of interest.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.In’t VP. Insulitis in human type 1 diabetes: a comparison between patients and animal models. Semin Immunopathol. 2014;36(5):569–79. doi: 10.1007/s00281-014-0438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Veiseh O, Tang BC, Whitehead KA, Anderson DG, Langer R. Managing diabetes with nanomedicine: challenges and opportunities. Nat Rev Drug Discov. 2015;14(1):45–57. doi: 10.1038/nrd4477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kyi M, Wentworth JM, Nankervis AJ, Fourlanos S, Colman PG. Recent advances in type 1 diabetes. Med J Aust. 2015;203(7):290–3. doi: 10.5694/mja14.01691. [DOI] [PubMed] [Google Scholar]
- 4.McCarthy DP, Hunter ZN, Chackerian B, Shea LD, Miller SD. Targeted immunomodulation using antigen-conjugated nanoparticles. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2014;6(3):298–315. doi: 10.1002/wnan.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5•.Getts DR, Shea LD, Miller SD, King NJ. Harnessing nanoparticles for immune modulation. Trends Immunol. 2015;36(7):419–27. doi: 10.1016/j.it.2015.05.007. A comprehensive review on the use of nanoparticles for immune modulation and tolerance. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Serra P, Santamaria P. Nanoparticle-based autoimmune disease therapy. Clin Immunol. 2015;160(1):3–13. doi: 10.1016/j.clim.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Hanninen A, Jalkanen S, Salmi M, Toikkanen S, Nikolakaros G, Simell O. Macrophages, T cell receptor usage, and endothelial cell activation in the pancreas at the onset of insulin-dependent diabetes mellitus. J Clin Invest. 1992;90(5):1901–10. doi: 10.1172/JCI116067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lernmark A, Kloppel G, Stenger D, Vathanaprida C, Falt K, Landin-Olsson M, et al. Heterogeneity of islet pathology in two infants with recent onset diabetes mellitus. Virchows Arch. 1995;425(6):631–40. doi: 10.1007/BF00199353. [DOI] [PubMed] [Google Scholar]
- 9.Willcox A, Richardson SJ, Bone AJ, Foulis AK, Morgan NG. Analysis of islet inflammation in human type 1 diabetes. Clin Exp Immunol. 2009;155(2):173–81. doi: 10.1111/j.1365-2249.2008.03860.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coppieters KT, Dotta F, Amirian N, Campbell PD, Kay TW, Atkinson MA, et al. Demonstration of islet-autoreactive CD8 T cells in insulitic lesions from recent onset and long-term type 1 diabetes patients. J Exp Med. 2012;209(1):51–60. doi: 10.1084/jem.20111187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eisenbarth GS. Banting lecture 2009: an unfinished journey: molecular pathogenesis to prevention of type 1A diabetes. Diabetes. 2010;59(4):759–74. doi: 10.2337/db09-1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pihoker C, Gilliam LK, Hampe CS, Lernmark A. Autoantibodies in diabetes. Diabetes. 2005;54(Suppl 2):S52–61. doi: 10.2337/diabetes.54.suppl_2.s52. [DOI] [PubMed] [Google Scholar]
- 13.Wenzlau JM, Juhl K, Yu L, Moua O, Sarkar SA, Gottlieb P, et al. The cation efflux transporter ZnT8 (Slc30A8) is a major autoantigen in human type 1 diabetes. Proc Natl Acad Sci U S A. 2007;104(43):17040–5. doi: 10.1073/pnas.0705894104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wenzlau JM, Liu Y, Yu L, Moua O, Fowler KT, Rangasamy S, et al. A common nonsynonymous single nucleotide polymorphism in the SLC30A8 gene determines ZnT8 autoantibody specificity in type 1 diabetes. Diabetes. 2008;57(10):2693–7. doi: 10.2337/db08-0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palmer JP, Asplin CM, Clemons P, Lyen K, Tatpati O, Raghu PK, et al. Insulin antibodies in insulin-dependent diabetics before insulin treatment. Science. 1983;222(4630):1337–9. doi: 10.1126/science.6362005. [DOI] [PubMed] [Google Scholar]
- 16.Baekkeskov S, Aanstoot HJ, Christgau S, Reetz A, Solimena M, Cascalho M, et al. Identification of the 64K autoantigen in insulin-dependent diabetes as the GABA-synthesizing enzyme glutamic acid decarboxylase. Nature. 1990;347(6289):151–6. doi: 10.1038/347151a0. [DOI] [PubMed] [Google Scholar]
- 17.Lampasona V, Bearzatto M, Genovese S, Bosi E, Ferrari M, Bonifacio E. Autoantibodies in insulin-dependent diabetes recognize distinct cytoplasmic domains of the protein tyrosine phosphatase-like IA-2 autoantigen. J Immunol. 1996;157(6):2707–11. [PubMed] [Google Scholar]
- 18.Bingley PJ, Christie MR, Bonifacio E, Bonfanti R, Shattock M, Fonte MT, et al. Combined analysis of autoantibodies improves prediction of IDDM in islet cell antibody-positive relatives. Diabetes. 1994;43(11):1304–10. doi: 10.2337/diab.43.11.1304. [DOI] [PubMed] [Google Scholar]
- 19.Skyler JS, Ricordi C. Stopping type 1 diabetes: attempts to prevent or cure type 1 diabetes in man. Diabetes. 2011;60(1):1–8. doi: 10.2337/db10-1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Atkinson MA, Eisenbarth GS, Michels AW. Type 1 diabetes. Lancet. 2014;383(9911):69–82. doi: 10.1016/S0140-6736(13)60591-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vives M, Somoza N, Soldevila G, Gomis R, Lucas A, Sanmarti A, et al. Reevaluation of autoantibodies to islet cell membrane in IDDM. Failure to detect islet cell surface antibodies using human islet cells as substrate. Diabetes. 1992;41(12):1624–31. doi: 10.2337/diab.41.12.1624. [DOI] [PubMed] [Google Scholar]
- 22.Koczwara K, Bonifacio E, Ziegler AG. Transmission of maternal islet antibodies and risk of autoimmune diabetes in offspring of mothers with type 1 diabetes. Diabetes. 2004;53(1):1–4. doi: 10.2337/diabetes.53.1.1. [DOI] [PubMed] [Google Scholar]
- 23.Pathiraja V, Kuehlich JP, Campbell PD, Krishnamurthy B, Loudovaris T, Coates PT, et al. Proinsulin-specific, HLA-DQ8, and HLA-DQ8-transdimer-restricted CD4+ T cells infiltrate islets in type 1 diabetes. Diabetes. 2015;64(1):172–82. doi: 10.2337/db14-0858. [DOI] [PubMed] [Google Scholar]
- 24.Skowera A, Ellis RJ, Varela-Calvino R, Arif S, Huang GC, Van-Krinks C, et al. CTLs are targeted to kill beta cells in patients with type 1 diabetes through recognition of a glucose-regulated preproinsulin epitope. J Clin Invest. 2008;118(10):3390–402. doi: 10.1172/JCI35449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Panina-Bordignon P, Lang R, van Endert PM, Benazzi E, Felix AM, Pastore RM, et al. Cytotoxic T cells specific for glutamic acid decarboxylase in autoimmune diabetes. J Exp Med. 1995;181(5):1923–7. doi: 10.1084/jem.181.5.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Unger WW, Pearson T, Abreu JR, Laban S, van der Slik AR, der Kracht SM, et al. Islet-specific CTL cloned from a type 1 diabetes patient cause beta-cell destruction after engraftment into HLA-A2 transgenic NOD/scid/IL2RG null mice. PLoS One. 2012;7(11):e49213. doi: 10.1371/journal.pone.0049213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mannering SI, Pathiraja V, Kay TW. The case for an autoimmune aetiology of type 1 diabetes. Clin Exp Immunol. 2016;183(1):8–15. doi: 10.1111/cei.12699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28••.Babon JA, ME DN, Blodgett DM, Crevecoeur I, Buttrick TS, Maehr R, et al. Analysis of self-antigen specificity of islet-infiltrating T cells from human donors with type 1 diabetes. Nat Med. 2016;22(12):1482–7. doi: 10.1038/nm.4203. The first comprehensive description of specificity of islet-infiltrating T cells from human donors with T1D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jayasimhan A, Mansour KP, Slattery RM. Advances in our understanding of the pathophysiology of type 1 diabetes: lessons from the NOD mouse. Clin Sci (Lond) 2014;126(1):1–18. doi: 10.1042/CS20120627. [DOI] [PubMed] [Google Scholar]
- 30.Pearson JA, Wong FS, Wen L. The importance of the non obese diabetic (NOD) mouse model in autoimmune diabetes. J Autoimmun. 2016;66:76–88. doi: 10.1016/j.jaut.2015.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31••.Nakayama M, Abiru N, Moriyama H, Babaya N, Liu E, Miao D, et al. Prime role for an insulin epitope in the development of type 1 diabetes in NOD mice. Nature. 2005;435(7039):220–3. doi: 10.1038/nature03523. Genetic evidence indicating that an autoimmune response to an insulin epitope drives development of T1D in NOD mice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32••.Prasad S, Kohm AP, JS MM, Luo X, Miller SD. Pathogenesis of NOD diabetes is initiated by reactivity to the insulin B chain 9–23 epitope and involves functional epitope spreading. J Autoimmun. 2012;39(4):347–53. doi: 10.1016/j.jaut.2012.04.005. Tolerogenic evidence that an autoimmune response to a dominant insulin epitope drives development of T1D in NOD mice and evidence for epitope spreading as disease progresses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Babad J, Geliebter A, DiLorenzo TP. T-cell autoantigens in the non-obese diabetic mouse model of autoimmune diabetes. Immunology. 2010;131(4):459–65. doi: 10.1111/j.1365-2567.2010.03362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34•.Luo X, Herold KC, Miller SD. Immunotherapy of type 1 diabetes: where are we and where should we be going? Immunity. 2010;32(4):488–99. doi: 10.1016/j.immuni.2010.04.002. A comprehensive review of immune-based clinical trials in T1D patients. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berry G, Waldner H. Accelerated type 1 diabetes induction in mice by adoptive transfer of diabetogenic CD4+ T cells. J Vis Exp. 2013;75:e50389. doi: 10.3791/50389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Presa M, Chen YG, Grier AE, Leiter EH, Brehm MA, Greiner DL, et al. The presence and preferential activation of regulatory T cells diminish adoptive transfer of autoimmune diabetes by polyclonal nonobese diabetic (NOD) T cell effectors into NSG versus NOD-scid mice. J Immunol. 2015;195(7):3011–9. doi: 10.4049/jimmunol.1402446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martin-Orozco N, Chung Y, Chang SH, Wang YH, Dong C. Th17 cells promote pancreatic inflammation but only induce diabetes efficiently in lymphopenic hosts after conversion into Th1 cells. Eur J Immunol. 2009;39(1):216–24. doi: 10.1002/eji.200838475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Feuerer M, Shen Y, Littman DR, Benoist C, Mathis D. How punctual ablation of regulatory T cells unleashes an autoimmune lesion within the pancreatic islets. Immunity. 2009;31(4):654–64. doi: 10.1016/j.immuni.2009.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haskins K, Portas M, Bradley B, Wegmann D, Lafferty K. T-lymphocyte clone specific for pancreatic islet antigen. Diabetes. 1988;37(10):1444–8. doi: 10.2337/diab.37.10.1444. [DOI] [PubMed] [Google Scholar]
- 40.Katz JD, Wang B, Haskins K, Benoist C, Mathis D. Following a diabetogenic T cell from genesis through pathogenesis. Cell. 1993;74(6):1089–100. doi: 10.1016/0092-8674(93)90730-e. [DOI] [PubMed] [Google Scholar]
- 41.Stadinski BD, Delong T, Reisdorph N, Reisdorph R, Powell RL, Armstrong M, et al. Chromogranin A is an autoantigen in type 1 diabetes. Nat Immunol. 2010;11(3):225–31. doi: 10.1038/ni.1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hansen CH, Krych L, Nielsen DS, Vogensen FK, Hansen LH, Sorensen SJ, et al. Early life treatment with vancomycin propagates Akkermansia muciniphila and reduces diabetes incidence in the NOD mouse. Diabetologia. 2012;55(8):2285–94. doi: 10.1007/s00125-012-2564-7. [DOI] [PubMed] [Google Scholar]
- 43.Xu D, Prasad S, Miller SD. Inducing immune tolerance: a focus on type 1 diabetes mellitus. Diabetes Manag (Lond) 2013;3(5):415–26. doi: 10.2217/dmt.13.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Michels AW, Eisenbarth GS. Immune intervention in type 1 diabetes. Semin Immunol. 2011;23(3):214–9. doi: 10.1016/j.smim.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bluestone JA, Herold K, Eisenbarth G. Genetics, pathogenesis and clinical interventions in type 1 diabetes. Nature. 2010;464(7293):1293–300. doi: 10.1038/nature08933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Luo X, Miller SD, Shea LD. Immune tolerance for autoimmune disease and cell transplantation. Annu Rev Biomed Eng. 2016;18:181–205. doi: 10.1146/annurev-bioeng-110315-020137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Plesner A, Worsaae A, Dyrberg T, Gotfredsen C, Michelsen BK, Petersen JS. Immunization of diabetes-prone or non-diabetes-prone mice with GAD65 does not induce diabetes or islet cell pathology. J Autoimmun. 1998;11(4):335–41. doi: 10.1006/jaut.1998.0206. [DOI] [PubMed] [Google Scholar]
- 48.Uibo R, Lernmark A. GAD65 autoimmunity-clinical studies. Adv Immunol. 2008;100:39–78. doi: 10.1016/S0065-2776(08)00803-1. [DOI] [PubMed] [Google Scholar]
- 49.Agardh CD, Cilio CM, Lethagen A, Lynch K, Leslie RD, Palmer M, et al. Clinical evidence for the safety of GAD65 immunomodulation in adult-onset autoimmune diabetes. J Diabetes Complicat. 2005;19(4):238–46. doi: 10.1016/j.jdiacomp.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 50.Ludvigsson J, Faresjo M, Hjorth M, Axelsson S, Cheramy M, Pihl M, et al. GAD treatment and insulin secretion in recent-onset type 1 diabetes. N Engl J Med. 2008;359(18):1909–20. doi: 10.1056/NEJMoa0804328. [DOI] [PubMed] [Google Scholar]
- 51.Ludvigsson J, Hjorth M, Cheramy M, Axelsson S, Pihl M, Forsander G, et al. Extended evaluation of the safety and efficacy of GAD treatment of children and adolescents with recent-onset type 1 diabetes: a randomised controlled trial. Diabetologia. 2011;54(3):634–40. doi: 10.1007/s00125-010-1988-1. [DOI] [PubMed] [Google Scholar]
- 52.Cheramy M, Skoglund C, Johansson I, Ludvigsson J, Hampe CS, Casas R. GAD-alum treatment in patients with type 1 diabetes and the subsequent effect on GADA IgG subclass distribution, GAD65 enzyme activity and humoral response. Clin Immunol. 2010;137(1):31–40. doi: 10.1016/j.clim.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 53.Wherrett DK, Bundy B, Becker DJ, DiMeglio LA, Gitelman SE, Goland R, et al. Antigen-based therapy with glutamic acid decarboxylase (GAD) vaccine in patients with recent-onset type 1 diabetes: a randomised double-blind trial. Lancet. 2011;378(9788):319–27. doi: 10.1016/S0140-6736(11)60895-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Harrison LC, Honeyman MC, Steele CE, Stone NL, Sarugeri E, Bonifacio E, et al. Pancreatic beta-cell function and immune responses to insulin after administration of intranasal insulin to humans at risk for type 1 diabetes. Diabetes Care. 2004;27(10):2348–55. doi: 10.2337/diacare.27.10.2348. [DOI] [PubMed] [Google Scholar]
- 55.Fourlanos S, Perry C, Gellert SA, Martinuzzi E, Mallone R, Butler J, et al. Evidence that nasal insulin induces immune tolerance to insulin in adults with autoimmune diabetes. Diabetes. 2011;60(4):1237–45. doi: 10.2337/db10-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Skyler JS, Krischer JP, Wolfsdorf J, Cowie C, Palmer JP, Greenbaum C, et al. Effects of oral insulin in relatives of patients with type 1 diabetes: the diabetes prevention trial—type 1. Diabetes Care. 2005;28(5):1068–76. doi: 10.2337/diacare.28.5.1068. [DOI] [PubMed] [Google Scholar]
- 57.Skyler JS, Greenbaum CJ, Lachin JM, Leschek E, Rafkin-Mervis L, Savage P, et al. Type 1 diabetes TrialNet—an international collaborative clinical trials network. Ann N Y Acad Sci. 2008;1150:14–24. doi: 10.1196/annals.1447.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pozzilli P, Pitocco D, Visalli N, Cavallo MG, Buzzetti R, Crino A, et al. No effect of oral insulin on residual beta-cell function in recent-onset type I diabetes (the IMDIAB VII). IMDIAB group. Diabetologia. 2000;43(8):1000–4. doi: 10.1007/s001250051482. [DOI] [PubMed] [Google Scholar]
- 59.Fife BT, Guleria I, Gubbels Bupp M, Eagar TN, Tang Q, Bour-Jordan H, et al. Insulin-induced remission in new-onset NOD mice is maintained by the PD-1-PD-L1 pathway. J Exp Med. 2006;203(12):2737–47. doi: 10.1084/jem.20061577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Daniel C, Weigmann B, Bronson R, von Boehmer H. Prevention of type 1 diabetes in mice by tolerogenic vaccination with a strong agonist insulin mimetope. J Exp Med. 2011;208(7):1501–10. doi: 10.1084/jem.20110574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Judkowski V, Rodriguez E, Pinilla C, Masteller E, Bluestone JA, Sarvetnick N, et al. Peptide specific amelioration of T cell mediated pathogenesis in murine type 1 diabetes. Clin Immunol. 2004;113(1):29–37. doi: 10.1016/j.clim.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 62.Tarbell KV, Petit L, Zuo X, Toy P, Luo X, Mqadmi A, et al. Dendritic cell-expanded, islet-specific CD4+ CD25+ CD62L+ regulatory T cells restore normoglycemia in diabetic NOD mice. J Exp Med. 2007;204(1):191–201. doi: 10.1084/jem.20061631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Weber SE, Harbertson J, Godebu E, Mros GA, Padrick RC, Carson BD, et al. Adaptive islet-specific regulatory CD4 T cells control autoimmune diabetes and mediate the disappearance of pathogenic Th1 cells in vivo. J Immunol. 2006;176(8):4730–9. doi: 10.4049/jimmunol.176.8.4730. [DOI] [PubMed] [Google Scholar]
- 64.Jaeckel E, von Boehmer H, Manns MP. Antigen-specific FoxP3-transduced T-cells can control established type 1 diabetes. Diabetes. 2005;54(2):306–10. doi: 10.2337/diabetes.54.2.306. [DOI] [PubMed] [Google Scholar]
- 65•.Bluestone JA, Buckner JH, Fitch M, Gitelman SE, Gupta S, Hellerstein MK, et al. Type 1 diabetes immunotherapy using polyclonal regulatory T cells. Sci Transl Med. 2015;7(315):315ra189. doi: 10.1126/scitranslmed.aad4134. Description of the use of Tregs for therapy of T1D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xia CQ, Peng R, Qiu Y, Annamalai M, Gordon D, Clare-Salzler MJ. Transfusion of apoptotic beta-cells induces immune tolerance to beta-cell antigens and prevents type 1 diabetes in NOD mice. Diabetes. 2007;56(8):2116–23. doi: 10.2337/db06-0825. [DOI] [PubMed] [Google Scholar]
- 67.Marin-Gallen S, Clemente-Casares X, Planas R, Pujol-Autonell I, Carrascal J, Carrillo J, et al. Dendritic cells pulsed with antigen-specific apoptotic bodies prevent experimental type 1 diabetes. Clin Exp Immunol. 2010;160(2):207–14. doi: 10.1111/j.1365-2249.2009.04082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Manolova V, Flace A, Bauer M, Schwarz K, Saudan P, Bachmann MF. Nanoparticles target distinct dendritic cell populations according to their size. Eur J Immunol. 2008;38(5):1404–13. doi: 10.1002/eji.200737984. [DOI] [PubMed] [Google Scholar]
- 69.Fifis T, Gamvrellis A, Crimeen-Irwin B, Pietersz GA, Li J, Mottram PL, et al. Size-dependent immunogenicity: therapeutic and protective properties of nano-vaccines against tumors. J Immunol. 2004;173(5):3148–54. doi: 10.4049/jimmunol.173.5.3148. [DOI] [PubMed] [Google Scholar]
- 70.Kourtis IC, Hirosue S, de Titta A, Kontos S, Stegmann T, Hubbell JA, et al. Peripherally administered nanoparticles target monocytic myeloid cells, secondary lymphoid organs and tumors in mice. PLoS One. 2013;8(4):e61646. doi: 10.1371/journal.pone.0061646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Garciafigueroa Y, Trucco M, Giannoukakis N. A brief glimpse over the horizon for type 1 diabetes nanotherapeutics. Clin Immunol. 2015;160(1):36–45. doi: 10.1016/j.clim.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 72.Shao K, Singha S, Clemente-Casares X, Tsai S, Yang Y, Santamaria P. Nanoparticle-based immunotherapy for cancer. ACS Nano. 2015;9(1):16–30. doi: 10.1021/nn5062029. [DOI] [PubMed] [Google Scholar]
- 73.Choi HS, Liu W, Misra P, Tanaka E, Zimmer JP, Itty Ipe B, et al. Renal clearance of quantum dots. Nat Biotechnol. 2007;25(10):1165–70. doi: 10.1038/nbt1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kwon YJ, Standley SM, Goh SL, Frechet JM. Enhanced antigen presentation and immunostimulation of dendritic cells using acid-degradable cationic nanoparticles. J Control Release. 2005;105(3):199–212. doi: 10.1016/j.jconrel.2005.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Murthy N, Xu M, Schuck S, Kunisawa J, Shastri N, Frechet JM. A macromolecular delivery vehicle for protein-based vaccines: acid-degradable protein-loaded microgels. Proc Natl Acad Sci U S A. 2003;100(9):4995–5000. doi: 10.1073/pnas.0930644100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fromen CA, Robbins GR, Shen TW, Kai MP, Ting JP, DeSimone JM. Controlled analysis of nanoparticle charge on mucosal and systemic antibody responses following pulmonary immunization. Proc Natl Acad Sci U S A. 2015;112(2):488–93. doi: 10.1073/pnas.1422923112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bal SM, Hortensius S, Ding Z, Jiskoot W, Bouwstra JA. Co-encapsulation of antigen and toll-like receptor ligand in cationic liposomes affects the quality of the immune response in mice after intradermal vaccination. Vaccine. 2011;29(5):1045–52. doi: 10.1016/j.vaccine.2010.11.061. [DOI] [PubMed] [Google Scholar]
- 78.Koppolu B, Zaharoff DA. The effect of antigen encapsulation in chitosan particles on uptake, activation and presentation by antigen presenting cells. Biomaterials. 2013;34(9):2359–69. doi: 10.1016/j.biomaterials.2012.11.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lockman PR, Koziara JM, Mumper RJ, Allen DD. Nanoparticle surface charges alter blood-brain barrier integrity and permeability. J Drug Target. 2004;12(9–10):635–41. doi: 10.1080/10611860400015936. [DOI] [PubMed] [Google Scholar]
- 80.Malik N, Wiwattanapatapee R, Klopsch R, Lorenz K, Frey H, Weener JW, et al. Dendrimers: relationship between structure and biocompatibility in vitro, and preliminary studies on the biodistribution of 125I-labelled polyamidoamine dendrimers in vivo. J Control Release. 2000;65(1–2):133–48. doi: 10.1016/s0168-3659(99)00246-1. [DOI] [PubMed] [Google Scholar]
- 81.Pensado A, Fernandez-Pineiro I, Seijo B, Sanchez A. Anionic nanoparticles based on span 80 as low-cost, simple and efficient non-viral gene-transfection systems. Int J Pharm. 2014;476(1–2):23–30. doi: 10.1016/j.ijpharm.2014.09.032. [DOI] [PubMed] [Google Scholar]
- 82.Ruenraroengsak P, Tetley TD. Differential bioreactivity of neutral, cationic and anionic polystyrene nanoparticles with cells from the human alveolar compartment: robust response of alveolar type 1 epithelial cells. Part Fibre Toxicol. 2015;12:19. doi: 10.1186/s12989-015-0091-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Liu Y, Li W, Lao F, Liu Y, Wang L, Bai R, et al. Intracellular dynamics of cationic and anionic polystyrene nanoparticles without direct interaction with mitotic spindle and chromosomes. Biomaterials. 2011;32(32):8291–303. doi: 10.1016/j.biomaterials.2011.07.037. [DOI] [PubMed] [Google Scholar]
- 84.Tagalakis AD, Lee DH, Bienemann AS, Zhou H, Munye MM, Saraiva L, et al. Multifunctional, self-assembling anionic peptide-lipid nanocomplexes for targeted siRNA delivery. Biomaterials. 2014;35(29):8406–15. doi: 10.1016/j.biomaterials.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 85.Sun Y, Guo F, Zou Z, Li C, Hong X, Zhao Y, et al. Cationic nanoparticles directly bind angiotensin-converting enzyme 2 and induce acute lung injury in mice. Part Fibre Toxicol. 2015;12:4. doi: 10.1186/s12989-015-0080-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yang SH, Heo D, Park J, Na S, Suh JS, Haam S, et al. Role of surface charge in cytotoxicity of charged manganese ferrite nanoparticles towards macrophages. Nanotechnology. 2012;23(50):505702. doi: 10.1088/0957-4484/23/50/505702. [DOI] [PubMed] [Google Scholar]
- 87.Chao Y, Makale M, Karmali PP, Sharikov Y, Tsigelny I, Merkulov S, et al. Recognition of dextran-superparamagnetic iron oxide nanoparticle conjugates (Feridex) via macrophage scavenger receptor charged domains. Bioconjug Chem. 2012;23(5):1003–9. doi: 10.1021/bc200685a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Champion JA, Mitragotri S. Role of target geometry in phagocytosis. Proc Natl Acad Sci U S A. 2006;103(13):4930–4. doi: 10.1073/pnas.0600997103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Verma A, Uzun O, Hu Y, Hu Y, Han HS, Watson N, et al. Surface-structure-regulated cell-membrane penetration by monolayer-protected nanoparticles. Nat Mater. 2008;7(7):588–95. doi: 10.1038/nmat2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Stone JW, Thornburg NJ, Blum DL, Kuhn SJ, Wright DW, Crowe JE., Jr Gold nanorod vaccine for respiratory syncytial virus. Nanotechnology. 2013;24(29):295102. doi: 10.1088/0957-4484/24/29/295102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Karch CP, Li J, Kulangara C, Paulillo SM, Raman SK, Emadi S, et al. Vaccination with self-adjuvanted protein nanoparticles provides protection against lethal influenza challenge. Nanomedicine. 2017;13(1):241–51. doi: 10.1016/j.nano.2016.08.030. [DOI] [PubMed] [Google Scholar]
- 92.Doll TA, Neef T, Duong N, Lanar DE, Ringler P, Muller SA, et al. Optimizing the design of protein nanoparticles as carriers for vaccine applications. Nanomedicine. 2015;11(7):1705–13. doi: 10.1016/j.nano.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Babapoor S, Neef T, Mittelholzer C, Girshick T, Garmendia A, Shang H, et al. A novel vaccine using nanoparticle platform to present immunogenic M2e against avian influenza infection. Influenza Res Treat. 2011;2011:126794. doi: 10.1155/2011/126794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wahome N, Pfeiffer T, Ambiel I, Yang Y, Keppler OT, Bosch V, et al. Conformation-specific display of 4E10 and 2F5 epitopes on self-assembling protein nanoparticles as a potential HIV vaccine. Chem Biol Drug Des. 2012;80(3):349–57. doi: 10.1111/j.1747-0285.2012.01423.x. [DOI] [PubMed] [Google Scholar]
- 95.Monopoli MP, Aberg C, Salvati A, Dawson KA. Biomolecular coronas provide the biological identity of nanosized materials. Nat Nanotechnol. 2012;7(12):779–86. doi: 10.1038/nnano.2012.207. [DOI] [PubMed] [Google Scholar]
- 96.Tenzer S, Docter D, Kuharev J, Musyanovych A, Fetz V, Hecht R, et al. Rapid formation of plasma protein corona critically affects nanoparticle pathophysiology. Nat Nanotechnol. 2013;8(10):772–81. doi: 10.1038/nnano.2013.181. [DOI] [PubMed] [Google Scholar]
- 97.Lundqvist M, Stigler J, Elia G, Lynch I, Cedervall T, Dawson KA. Nanoparticle size and surface properties determine the protein corona with possible implications for biological impacts. Proc Natl Acad Sci U S A. 2008;105(38):14265–70. doi: 10.1073/pnas.0805135105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98•.Smarr CB, Yap WT, Neef TP, Pearson RM, Hunter ZN, Ifergan I, et al. Biodegradable antigen-associated PLG nanoparticles tolerize Th2-mediated allergic airway inflammation pre- and postsensitization. Proc Natl Acad Sci USA. 2016;113(18):5059–64. doi: 10.1073/pnas.1505782113. Demonstration that infusion of antigen-encapsulating PLG nanoparticles induce tolerance in Th2 cells useful in prevention and treatment in an animal model of allergic airway disease. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ilinskaya AN, Dobrovolskaia MA. Immunosuppressive and anti-inflammatory properties of engineered nanomaterials. Br J Pharmacol. 2014;171(17):3988–4000. doi: 10.1111/bph.12722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Phillips B, Nylander K, Harnaha J, Machen J, Lakomy R, Styche A, et al. A microsphere-based vaccine prevents and reverses new-onset autoimmune diabetes. Diabetes. 2008;57(6):1544–55. doi: 10.2337/db07-0507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Leuschner F, Dutta P, Gorbatov R, Novobrantseva TI, Donahoe JS, Courties G, et al. Therapeutic siRNA silencing in inflammatory monocytes in mice. Nat Biotechnol. 2011;29(11):1005–10. doi: 10.1038/nbt.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang P, Yigit MV, Ran C, Ross A, Wei L, Dai G, et al. A theranostic small interfering RNA nanoprobe protects pancreatic islet grafts from adoptively transferred immune rejection. Diabetes. 2012;61(12):3247–54. doi: 10.2337/db12-0441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shah M, Edman MC, Janga SR, Shi P, Dhandhukia J, Liu S, et al. A rapamycin-binding protein polymer nanoparticle shows potent therapeutic activity in suppressing autoimmune dacryoadenitis in a mouse model of Sjogren’s syndrome. J Control Release. 2013;171(3):269–79. doi: 10.1016/j.jconrel.2013.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tsai S, Shameli A, Yamanouchi J, Clemente-Casares X, Wang J, Serra P, et al. Reversal of autoimmunity by boosting memory-like autoregulatory T cells. Immunity. 2010;32(4):568–80. doi: 10.1016/j.immuni.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 105••.Clemente-Casares X, Blanco J, Ambalavanan P, Yamanouchi J, Singha S, Fandos C, et al. Expanding antigen-specific regulatory networks to treat autoimmunity. Nature. 2016;530(7591):434–40. doi: 10.1038/nature16962. Demonstration that iron oxide nanoparticles expressing peptide-MHC molecules can induce tolerance for treatment of autoimmune disease. [DOI] [PubMed] [Google Scholar]
- 106.Singha S, Shao K, Yang Y, Clemente-Casares X, Sole P, Clemente A, et al. Peptide-MHC-based nanomedicines for autoimmunity function as T-cell receptor microclustering devices. Nat Nanotechnol. 2017 doi: 10.1038/nnano.2017.56. [DOI] [PubMed] [Google Scholar]
- 107.Schutz C, Fleck M, Mackensen A, Zoso A, Halbritter D, Schneck JP, et al. Killer artificial antigen-presenting cells: a novel strategy to delete specific T cells. Blood. 2008;111(7):3546–52. doi: 10.1182/blood-2007-09-113522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Schutz C, Fleck M, Schneck JP, Oelke M. Killer artificial antigen presenting cells (KaAPC) for efficient in vitro depletion of human antigen-specific T cells. J Vis Exp. 2014;90:e51859. doi: 10.3791/51859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Maldonado RA, LaMothe RA, Ferrari JD, Zhang AH, Rossi RJ, Kolte PN, et al. Polymeric synthetic nanoparticles for the induction of antigen-specific immunological tolerance. Proc Natl Acad Sci U S A. 2015;112(2):E156–65. doi: 10.1073/pnas.1408686111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhang AH, Rossi RJ, Yoon J, Wang H, Scott DW. Tolerogenic nanoparticles to induce immunologic tolerance: prevention and reversal of FVIII inhibitor formation. Cell Immunol. 2016;301:74–81. doi: 10.1016/j.cellimm.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 111.Yeste A, Nadeau M, Burns EJ, Weiner HL, Quintana FJ. Nanoparticle-mediated codelivery of myelin antigen and a tolerogenic small molecule suppresses experimental autoimmune encephalomyelitis. Proc Natl Acad Sci U S A. 2012;109(28):11270–5. doi: 10.1073/pnas.1120611109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112••.Yeste A, Takenaka MC, Mascanfroni ID, Nadeau M, Kenison JE, Patel B, et al. Tolerogenic nanoparticles inhibit T cell-mediated autoimmunity through SOCS2. Sci Signal. 2016;9(433):ra61. doi: 10.1126/scisignal.aad0612. Demonstration that gold nanoparticles expressing antigen and an AhR agonist can prevent development of T1D in NOD mice. [DOI] [PubMed] [Google Scholar]
- 113.Macauley MS, Pfrengle F, Rademacher C, Nycholat CM, Gale AJ, von Drygalski A, et al. Antigenic liposomes displaying CD22 ligands induce antigen-specific B cell apoptosis. J Clin Invest. 2013;123(7):3074–83. doi: 10.1172/JCI69187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pfrengle F, Macauley MS, Kawasaki N, Paulson JC. Copresentation of antigen and ligands of Siglec-G induces B cell tolerance independent of CD22. J Immunol. 2013;191(4):1724–31. doi: 10.4049/jimmunol.1300921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Copp JA, Fang RH, Luk BT, Hu CM, Gao W, Zhang K, et al. Clearance of pathological antibodies using biomimetic nanoparticles. Proc Natl Acad Sci U S A. 2014;111(37):13481–6. doi: 10.1073/pnas.1412420111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116••.Getts DR, Martin AJ, DP MC, Terry RL, Hunter ZN, Yap WT, et al. Microparticles bearing encephalitogenic peptides induce T-cell tolerance and ameliorate experimental autoimmune encephalomyelitis. Nat Biotechnol. 2012;30(12):1217–24. doi: 10.1038/nbt.2434. Initial description that antigen coupled to polystyrene and PLG nanoparticles can induce tolerance active in prevention of EAE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117••.Hunter Z, DP MC, Yap WT, Harp CT, Getts DR, Shea LD, et al. A biodegradable nanoparticle platform for the induction of antigen-specific immune tolerance for treatment of autoimmune disease. ACS Nano. 2014;8(3):2148–60. doi: 10.1021/nn405033r. Description of the ability of antigen-coupled PLG nanoparticles to treat ongoing EAE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118••.McCarthy DP, Yap JW, Harp CT, Song WK, Chen J, Pearson RM, et al. An antigen-encapsulating nanoparticle platform for TH1/17 immune tolerance therapy. Nanomedicine. 2017;13(1):191–200. doi: 10.1016/j.nano.2016.09.007. Description of the ability of antigen-encapsulating PLG nanoparticles to prevent and treat EAE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119•.Hlavaty KA, DP MC, Saito E, Yap WT, Miller SD, Shea LD. Tolerance induction using nanoparticles bearing HY peptides in bone marrow transplantation. Biomaterials. 2016;76:1–10. doi: 10.1016/j.biomaterials.2015.10.041. Description of the ability of either antigen-coupled or antigen encapsulating nanoparticles to prevent bone marrow transplant rejection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120••.Miller SD, Prasad S, Neef T. Antigen-encapsulating PLG nanoparticles induce long-lived regulatory T cell control of activated diabetogenic CD4 and CD8 T cells (Abstract); Immunology of Diabetes Society 15th International Congress; 2017. Demonstration of nanoparticle tolerance for the treatment of adoptive transfer models of T1D. [Google Scholar]
- 121•.Bryant J, Hlavaty KA, Zhang X, Yap WT, Zhang L, Shea LD, et al. Nanoparticle delivery of donor antigens for transplant tolerance in allogeneic islet transplantation. Biomaterials. 2014;35(31):8887–94. doi: 10.1016/j.biomaterials.2014.06.044. Demonstration that antigen-coupled nanoparticles can induce tolerance to protect transplanted allogeneic islets. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hlavaty KA, Luo X, Shea LD, Miller SD. Cellular and molecular targeting for nanotherapeutics in transplantation tolerance. Clin Immunol. 2015;160(1):14–23. doi: 10.1016/j.clim.2015.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chopra S, Bertrand N, Lim JM, Wang A, Farokhzad OC, Karnik R. Design of insulin-loaded nanoparticles enabled by multistep control of nanoprecipitation and zinc chelation. ACS Appl Mater Interfaces. 2017;9(13):11440–50. doi: 10.1021/acsami.6b16854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124•.Luo X, Pothoven KL, McCarthy D, DeGutes M, Martin A, Getts DR, et al. ECDI-fixed allogeneic splenocytes induce donor-specific tolerance for long-term survival of islet transplants via two distinct mechanisms. Proc Natl Acad Sci U S A. 2008;105(38):14527–32. doi: 10.1073/pnas.0805204105. Description of the ability of tolerance induced by the i.v. infusion of apoptotic donor leukocytes to long-term survival of transplanted donor islets. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Desai T, Shea LD. Advances in islet encapsulation technologies. Nat Rev Drug Discov. 2016 doi: 10.1038/nrd.2016.232. [DOI] [PMC free article] [PubMed] [Google Scholar]