Abstract
Peer-led interventions may be an effective means of addressing the childhood obesity epidemic; however, few studies have looked at the long-term sustainability of such programs. As part of a multilevel obesity prevention intervention, B’More Healthy Communities for Kids, 16 Baltimore college students were trained as youth-leaders (YLs) to deliver a skill-based nutrition curriculum to low-income African American children (10–14 years old). In April 2015, formative research was used to inform sustainability of the YL program in recreation centers. In-depth interviews were conducted with recreation center directors (n = 4) and the YLs (n = 16). Two focus groups were conducted with YLs (n = 7) and community youth-advocates (n = 10). Barriers to this program included difficulties with transportation, time constraints, and recruiting youth. Lessons learned indicated that improving trainings and incentives to youth were identified as essential strategies to foster continuity of the youth-led program and capacity building. High school students living close to the centers were identified as potential candidates to lead the program. Based on our findings, the initial intervention will be expanded into a sustainable model for implementation, using a train-the-trainer approach to empower community youth to be change agents of the food environment and role models.
Keywords: adolescent, youth-led, African American, nutrition, sustainability, mentoring
INTRODUCTION
Obesity rates in the United States have doubled in children and quadrupled in adolescents in the past three decades (Ogden, Carroll, Kit, & Flegal, 2014). Obesity and childhood eating behaviors have also been shown to track into adolescence and are maintained into adulthood (Clarke & Lauer, 1993; Rasmussen et al., 2006).
Many public health education researches, including prevention of health risk behaviors, child development, and mental health, have incorporated youth into intervention teams as mentors to interact directly with younger children (Wong, Zimmerman, & Parker, 2010; Yancey, Siegel, & McDaniel, 2002). Childhood obesity prevention programs that incorporate youth-mentors have shown increased sales of healthier options in school cafeterias (Bogart et al., 2014; Hamdan, Story, French, Fulkerson, & Nelson, 2005), decreased sugar sweetened beverage consumption in youth (Cawley et al., 2011) and youth-leaders (Bogart et al., 2011), improved psychosocial outcomes (Bogart et al., 2014; Smith, 2011), decreased intake of snacks and desserts (Black et al., 2010), and decreased weight gain (Black et al., 2010; Ronsley, Lee, Kuzeljevic, & Panagiotopoulos, 2013; Santos et al., 2014).
Social modeling or observational learning principles, with origins in social cognitive theory, provide part of the rationale for involving peers in behavior change interventions (McHugh et al., 2016), in which mentoring operates through a mentor–mentee relationship based on support and guidance, enabling the mentee to model health promoting activities suggested by the mentor (Sipe, 2002). The results of youth-led interventions have been equivalent, or superior, to adult-led interventions (Mellanby, Rees, & Tripp, 2000; Smith & Holloman, 2013), resulting in greater improvement in physical activity, diet, and psychosocial factors (Dzewaltowski et al., 2009; Woodgate & Sigurdson, 2015).
BACKGROUND
The use of youth-led participatory programs has increased in the past years, especially in schools, to promote youth empowerment and engagement and to improve health (Roth & Brooks-Gunn, 2003). For instance, a youth-led school-based program in which middle school–aged students helped deliver a nutrition education curriculum to their classmates found that mentors and mentees exposed to the program improved their diet (Birnbaum, Lytle, Story, Perry, & Murray, 2002). Another youth-led school-based health promotion program in Canada improved youths’ knowledge and attitudes about health, building youths’ capacity for health promotion (Woodgate & Sigurdson, 2015). Thus, youth-mentors in nutrition interventions contribute to positive health outcomes while playing a leadership role in health-related programs (Black et al., 2010; Coleman, Geller, Rosenkranz, & Dzewaltowski, 2008).
Despite previous work, relatively few youth-led programs have focused on obesity prevention and healthy eating practices. While prior school-based obesity prevention research has yielded mixed results (Gittelsohn & Kumar, 2007; Hung et al., 2015), after-school programs have become a promising venue to combat childhood obesity (Ajja, Beets, Huberty, Kaczynski, & Ward, 2012). In the Baltimore Health Eating Zones obesity trial, in which youth led a nutrition program in Baltimore recreation centers, body mass index percentiles decreased in children receiving the program (Gittelsohn et al., 2013).
A big gap in the peer mentoring literature is in the area of sustainability. Many youth-led community programs have focused only on program efficacy rather than on the long-term viability of the program success (Godfrey, 2008). This study aimed to inform future scale-up and sustainability of an ongoing youth-leader program in Baltimore recreation centers. We conducted formative research to develop approaches to sustain the youth-leader intervention and maintain continuity (Gittelsohn et al., 2006).
The aim of this study was to answer the following questions:
What are the lessons learned from the Wave 1 youth-leader program to enhance the likelihood of sustainability?
What are the challenges perceived by the study participants to sustaining the youth-leader program?
What are the potential applications to foster sustainability of the youth-leader program?
METHOD
The B’more Healthy Communities for Kids (BHCK) Trial
BHCK is an ongoing multilevel obesity prevention trial in Baltimore implemented in two waves from July 2014 to January 2015 and November 2015 to August 2016 (Gittelsohn et al., 2014). Youth-leaders provide education and nutrition skills to children ages 10 to 14 in community recreation centers and corner stores/carryouts. Other intervention components include policy, wholesaler, small food stores, social media, and family/caregivers.
Each wave of the intervention takes place in 14 low-income, predominantly African American communities in Baltimore City. Recreation centers were randomly selected into intervention (n = 7) and comparison (n = 7) groups for each wave. BHCK Wave 1 recruited 16 youth-leaders (local college and GED students, 18–22 years), who were trained to deliver the nutrition intervention to youth in the recreation centers. Twelve youth-leaders completed the entire Wave 1 intervention (Sato et al., 2016). For the comparison group, we selected a cohort of youth (n = 10) who applied for the youth-leader position but were not selected to deliver the program due to schedule conflicts and as they did not meet age criteria (mean age = 17.9 years). BHCK youth-leaders received an initial 12-session training program (total of 27 hours), as well as biweekly booster sessions throughout the intervention. After successfully completing the training, teams of three to five youth-leaders were formed to implement the program in the intervention recreation centers (n = 7). The youth-leader program was a skill-based nutrition education program, which used social cognitive theory and observational learning principles to integrate basic nutrition, cooking and teamwork skills, with the goal to facilitate behavior change using role models. The intervention in both the recreation centers and small stores consisted of three phases: (1) healthier beverages, (2) healthier snacks, and (3) healthier food preparation. Center directors were also trained in BHCK curriculum content.
Recreation Center Communication Materials
The nutrition curriculum consisted of 14 sessions (60 minutes) taught by youth-leaders over the course of 6 months. Each session of the recreation center nutrition curriculum involved a brief instructional period (5–15 minutes of information giving), followed by interactive games, activities, and cooking classes. Recipes or handouts were delivered after each session to the youth. Social media and text messaging reinforced these health-related messages to parents. Interventionists displayed relevant posters with information on nutrition sessions at each recreation center that received the intervention.
Taste Test and Giveaways
Food samples and theme-related giveaway items were also distributed to youth in order to draw their attention to the promoted foods. For example, during the healthier beverage phase, children sampled fruit-flavored water and received a BHCK water bottle.
Formative Research to Understand Program Implementation and Plan for Sustainability
Following the completion of Wave 1, we conducted formative research to gather lessons learned from youth-leader program. Participants included Recreation Center Directors (n = 4), BHCK youth-leaders (n = 16), Baltimore City Youth Commission Members (youth-advocates not directly involved in BHCK; n = 8), and youth-advocates in Baltimore working in different health-related community programs (n = 2). The interviewer (AT) was trained at the graduate level in qualitative research methods. The interviews lasted an average of 60 minutes and were recorded and transcribed for coding and analysis.
Data collection was intended to inform program implementation in seven additional intervention centers for BHCK Wave 2 and the sustainability of this intervention component beyond the grant funding period. Methodological and stakeholder triangulations were used to improve accuracy and gather detailed information on the program. We used in-depth interviews (IDIs) and focus group discussions (FGDs) with recreation center directors, youth-leaders, and community youth-advocates.
This study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (IRB No. 00004203).
In-depth Interviews With Recreation Center Directors
From the seven directors invited to be part of the formative research, four agreed to participate (one male and three female). All directors were affiliated with Baltimore City Recreation and Parks (BCRP) department. Participating directors were asked questions about perceptions, challenges, benefits, and financial avenues to sustain the youth-leader program (e.g., “Can you think of ways that a youth-leader program in the rec center can be improved?” and “Can you think of ways to cover the costs of a youth-leader program [i.e. cooking supplies or youth-leader payroll])?”
In-depth Interviews With BHCK Youth-Leaders
We invited 16 BHCK youth-leaders to participate in the IDIs. We asked youth-leaders to comment on their perceptions of youth-leader program, benefits and challenges of being a youth-leader, and ways to improve the youth-leader program. Some questions from the interview guide used with BHCK youth-leaders were “How did you decide to become a youth-leader?” and “If you could implement the youth-leader in other recreations centers, how would you do it?”
In-depth Interviews With Youth-Advocates
Using snowball sampling, we recruited two female youth (high school and college-aged) who participated in a different youth-led program in Baltimore to explore youth-led experiences outside BHCK. One interviewee (Baltimore college student) coordinated a youth-led program where teenagers teach a curriculum at the YMCA. The other was a teenager delivering the curriculum to middle school students. Youth were asked about their experience working with children and the benefits and challenges of leading a youth-led program: “Can you think about different groups of people in your community who could implement a nutrition curriculum in the rec center?” and “What would motivate teenagers to be leaders?”
Focus Group Discussions
We conducted two FGDs to refine the program based on youths’ experience. One FGD was conducted with seven BHCK youth-leaders (same as the interviewees in the IDIs) and lasted approximately 3 hours. The remaining youth-leaders could not participate due to schedule conflicts or change in their phone numbers. Example of questions asked were “How would you make other teenagers from the community interested in becoming a leader like you?” and “Can you think of ways to make this program successful and long lasting?” The other FGD was conducted with the youth commission from the Baltimore Mayor’s Office (n = 8) and lasted 1 hour. The youth commission provides recommendations to the City Mayor and Council on the development of government policies and programs serving youth in the City. Sample questions from the discussion guide include “What do you imagine a youth-leader program in the rec center should look like?” and “What would motivate other teenagers to be part of the youth-leader program?”
Data Analysis
This study adopted a grounded theory approach (Charmaz, 2000). After reading all transcripts and field notes, the research team identified emergent patterns and used inductive coding to identify key themes and concepts to develop a list of common codes to analyze the data (Miles, Huberman, & Saldaña, 2013). To identify and eliminate inconsistencies in application of the codebook, researchers individually applied the code-book to the same two transcripts. After they coded the two interviews and standardized application of the codebook, each researcher coded three to five interview transcripts using qualitative data analysis software ATLAS.ti Version 4.2 (Berlin). Nineteen codes emerged, including mentoring, nutrition curriculum, programming support, youth-led program characteristics in the recreation centers, impact of BHCK, BHCK challenges, barriers to working with teenagers, and incentives to youth. Memos were also developed to capture the overall sense and meaning of each interview (Miles et al., 2013). We used extracted text and reflections from memos to generate analysis content, themes, and findings across the groups.
RESULTS
The youth-leader Wave 1 program had an average of 10 African American children (10–14 years old) per session, reaching over 1,600 children in recreation centers and community venues combined.
Lessons Learned From the BHCK Youth-Leader Program
Enhance Training Sessions for Youth-Leaders With Scenarios Based on Their Experiences
Role-playing different situations based on experiences at the recreation center (e.g., handling conflicts with kids and with youth-leaders, team accountability, dealing with discipline, and role modeling) were recommendations from youth-leaders to improve their ability to tailor the curriculum to each context. According to leaders, trainings were helpful to permit team building and familiarity with lesson content.
Based on Wave 1, we learned that additional topics could be included in the training curriculum. For instance, adapting activities according to the possible different age ranges of the targeted audience beforehand would allow leaders to improve their ability to adjust to each situation.
Reduce Complexity for Each Session
Simplifying activities and discussion material was recommended to improve the lessons. Youth-leaders noted that many steps within one activity were confusing to children. Consequently, children did not understand the game, and the objective of the lesson was only partially achieved.
We would get confused, are you supposed to be standing? I think you’re out? We were like “How do we keep score for this game? Who wins?” Just too many steps. (BHCK youth-leader FGD)
Involve Parents During Nutrition Education Sessions at Recreation Centers
For future programing, all the groups interviewed recommended including parents during some activities sessions, such as the cooking classes (see Figure 1).
So maybe we have a meeting where their parents come maybe like one night per month and they actually cook with their kids, so not only are you creating closer family dynamics but you are actually teaching the parent along with the child so that in turn will have much more of a long-lasting impact. (Baltimore youth-advocate FGD)
FIGURE 1.
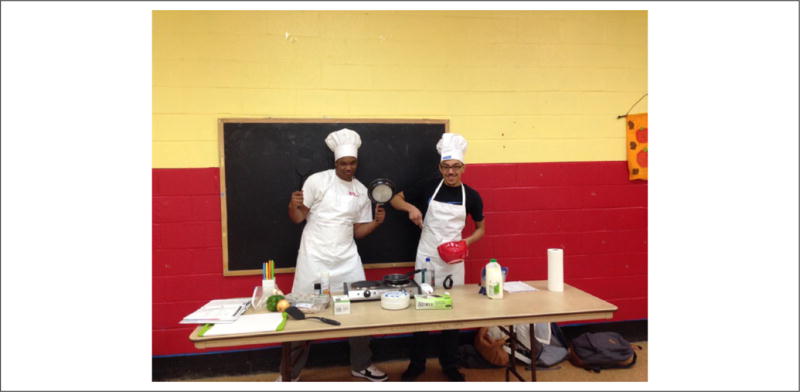
Youth-Leaders in a Recreation Center During a Cooking Lesson
Although flyers, handouts, and the texting component were targeted to parents, not all of the caregivers received the information from the recreation center, as it depended on a parent’s engagement in the centers. Strategies to improve communication with parents included posting the handouts on bulletin boards or handing it directly to parents when they pick up their children.
Staff and Group Support Needed to Conduct the Program
Youth-leaders reported needing a recreation center staff present to help with classroom management. Some youth-leaders found that it was sometimes difficult to work with children between 10 and 14 years of age when they were loud and disruptive, and the presence of a staff person would aid in behavioral management.
Another recommendation was to improve support within the youth-leader group to conduct the sessions and address nonattendance. Youth-leaders felt the need to have a better communication with each other, as toward the end of the program rates of lateness and absenteeism increased among the youth-leaders. Problems with transportation, last-minute family emergencies, or schoolwork were among the most common reasons for lateness and absences among the youth-leaders.
Lessons learned from Wave 1 will inform BHCK youth-leader Wave 2 program (Table 1). This participatory process had a secondary effect of building community ownership and support, thus aiding in sustainability.
TABLE 1.
Lessons Learned and Recommendations for Youth-Led Programming
| Theme | Lessons Learned | Recommendations |
|---|---|---|
| Training sessions |
|
|
| Nutrition education sessions |
|
|
| Program support |
|
|
| Future program youth-leaders |
|
|
Challenges to Sustainability
Perceived Challenges With Youth-Led Programs
Although BHCK youth-leaders, youth-advocates, and directors perceived benefits of a peer-led nutrition program, all expressed concerns about youths’ difficulties with transportation, low maturity levels, and competing priorities. Interestingly, most of these concerns were similar to the feedback BHCK youth-leaders provided about each other. For instance, youth-leaders either had consistent problems getting to sessions when relying on public transportation or had competing priorities, such as schoolwork.
The hours it requires and the locations you have to go, it would probably be best to do it with people who are old enough to drive or old enough to be out of their house at certain times like that. I don’t think the high schoolers would even be able to make it to the recs on time, unless they went to high school by the rec, because they kind of get out around the same time, so they would have to come to wherever we are going. (BHCK youth-leader FGD)
Issues Recruiting and Identifying Youth
Despite the fact that directors could identify youth to be part of the teen council and implement the nutrition program, they worried that some of the youth interested in becoming involved in the program would already be enrolled in other after-school activities or would need to focus more on their schoolwork. Also, not all centers have high teenager participation rates in their after-school programs. According to youth-leaders and youth-advocates, participation could be improved if centers provided more structured activities tailored to teenagers and applied behavioral rules appropriate for this age-group, rather than those for younger children.
Lack of Funding and Support for Recreation Centers
Recreation center directors expressed funding concerns when discussing sustainability. Directors were unsure how BCRP would fund youth incentives or supplies (e.g., for cooking lessons). According to BCRP operations, directors are accountable for their respective center budgets and are able to request funding for programming; however, they must follow Baltimore City and BCRP’s financial procedure and procurement process. As long as the requested program meets core programmatic components and follows departmental ethics and policy guidelines within the budget available, there are no specific funding restrictions. A program proposal, justification, and all core components must be submitted to the Mayor’s Office and Board of Estimates for funding approval. Funding approval typically takes less than 30 days.
Ways to Achieve Program Sustainability
Develop Health Promotion Capacity
The perceived success of the program motivated directors to implement nutrition-related activities in the recreation centers. For instance, directors started nutrition activities with those children outside the BHCK age range (5–8 years old), while youth-leaders were teaching older youth. Therefore, the program started to form its own roots due to enthusiasm for the project. Signs of behavior change may affect buy-in from recreation director, children, and parents to aid in sustainability.
We did a taste test with the [younger] kids. I did, V8 Fusion, V8 Splash, and V8 juice. So I put the three cups there and lined them up around the table and they had to drink all 3 of the juices. When I told them that fruits and vegetables were in there they were like “blahhh.” But I said “You drank it and it tasted good, now that you know what’s in there you can encourage your moms to buy this at the store versus sodas and stuff that’s got a lot of sugar in it.” (Recreation center director IDI)
Routinize of the Youth-Leader Program
Recreation center directors expressed the desire for more regularity in the youth-led activities and for long-term institutionalization of the program. In their opinion, having the youth-leaders at the center every week, versus every other week, would have made it easier to engage kids and adapt to the recreation schedule.
The kids are already ready and know, “Oh, B’more Healthy is this week, what time is so and so going to be here?” They got used to certain things supposed to happen, they adapt very quickly and they grow accustomed to it. So when things stop abruptly or stop before they’re supposed to stop, a lot of times, the kids get disappointed quickly, which changes their whole mindset about the program and what they would like to do. (Recreation center director IDI)
Work with Teen Councils for Institutionalization of the Program
The preexisting teen councils in a few recreation centers in Baltimore are composed of teenagers volunteering in the centers with younger children. The teen council—part of the mission of Baltimore City Recreation and Parks—was identified by BCRP leaders as a possible strategy for sustainability of the youth-leader program. Recreation center directors, youth-leaders, and Baltimore youth perceived benefits in this model, for example, young youth would still learn from peers, and may inspire them to continue their education and open their minds for life opportunities.
According to community youth-leaders and youth-advocates, future youth-leaders should reflect the demographics of the local population (mix of male and female and a combination of interests), feel comfortable in the community, recognize the problems and inequalities affecting the city, communicate effectively, and handle themselves in a mature manner (see Figure 2).
FIGURE 2.

Youth-leaders Interacting With Children in the After-School Program During an Educational Session
Identify and Engage Teenagers for Continuity of the Youth-Led Program
For continuity of the program, several strategies emerged: Recreation center directors, staff, and volunteers could identify potential youth-leaders; social media could capture teenagers’ attention; and current BHCK youth-leaders could also help select new youth-leaders. Directors identified community service hours as a form of incentive for future programs, since youth in Baltimore require service hours to graduate from high school. All directors agreed that gift cards or taking them to fun activities in the community would be appropriate incentives for youth-leaders. Paying for youth-leaders’ SAT or college application fees was among other ideas from recreation center directors.
Furthermore, youth-advocates stressed the importance of having a hook to gain teenagers’ interest in applying. If community service hours by themselves would not be enough to pique teenagers’ curiosity in the program, the addition of gift cards could be a complementary incentive.
It starts with marketing and branding … A lot of key words for productive programs and like those that are trying to help the society, like things that automatically tune out in their ear. So you kind of have to figure out what’s the hook. […] You gotta be like “So who is interesting in food and cooking?” and doing those kinds of things and then from there educate them in food deserts. (Baltimore youth-advocate FGD)
Use Train-the-Trainer Approach to Build Capacity
Training new youth to implement and continue the program was highlighted as necessary by BHCK youth-leaders. Experienced leaders identified themselves as appropriate mentors for the new leaders to demonstrate how sessions are conducted.
I felt like even if we did not bring back a lot of the old youth-leaders and got new people fresh, we should come in and help with training and go out to the rec centers and do like a mock situation, what is like being with the kids. [BHCK youth-leader IDI]
DISCUSSION
BHCK is one of few studies implemented by youth in an after-school setting aimed at improving nutrition in middle-school aged children. Our study evaluated the BHCK Wave 1 youth-leader program to identify lessons learned and directions for future studies and sustainability. Findings will aid in institutionalization of the program by BCRP based on recommendations and lessons learned, as well as supporting training for center director, staff, and teen council members to build capacity. Institutionalization of the youth-leader program may be possible using existing youth organizations where teenagers volunteering in the recreation centers could be trained to deliver the BHCK nutrition curriculum. BHCK youth-leaders and recreation center directors recognized program benefits across all participant types: the children, the youth-leaders, and the community.
Among the strategies to help in continuity of the youth-led nutrition program, the recreation centers’ directors and staff were identified as key people supporting youth-leaders in the program. In the TEENS study, school staff also recognized the positive influence of peers on children, and staff were considered important people for providing support to leaders (Lytle et al., 2004). In the literature, the youth–adult shared program involvement (where youth come to adults for advice and support) is considered to be beneficial to the development of the youth-mentor development and empowerment (Wong et al., 2010). Thus, in a youth-led program in recreation centers, center staff should provide their expertise, institutional resources, and support to the program and to youth-leaders to facilitate sustainability.
Another important way to achieve sustainability of the nutrition program is to ensure that the program will not have an unexpected termination, for example, due to lack of program funding or change in staff. This was a concern raised by centers’ directors based on children’s frustration with previous programming in the after-school setting. Furthermore, youth-advocates worried that sudden ending of programs delivered to children could lead to trust issues and may affect children’s enthusiasm and engagement with future programing. Therefore, it is important to plan the long-term viability of a community intervention to avoid unintended consequences when funding is terminated (Godfrey, 2008).
As suggested by our results, others have also found that involving experienced peer educators (from prior study years) to train new leaders was worthwhile (Walker & Avis, 1999). Therefore, using Wave 1 BHCK youth-leaders to train new leaders in Wave 2 may enhance the quality of the training and consequently build capacity for sustainability. Moreover, BHCK developed a youth-leader training curriculum based on Wave 1 experiences, currently available to aid in capacity building and institutionalization of youth-led projects in community settings.
Training sessions seemed to improve leadership and team-building skills of mentors and were considered important to youth-leaders. In another study with middle school peer leaders teaching nutrition in a school, an intensive 1-day training was provided to youth (Lytle et al., 2004). However, 45% of the peer-leaders in the TEENS study reported they would have liked to have more training. A review conducted in 1999 addressing the reasons for failure of peer education programs mentioned that most programs underestimated the time and level of training required to form interventionists (Walker & Avis, 1999). Our 12-session training and the continued training during the intervention seemed appropriate to empower youth-leaders with nutrition and program information, and also allowed time for reflection on interpersonal skills. In addition, role-play opportunities for youth to practice activities and public speaking were one of the recommendations made by King et al. (2015) where youth felt the need to include this component into the trainings. According to the feedback provided by BHCK youth-leaders, role-playing opportunities and activities prior to teaching children were very effective.
Among the challenges of a youth-led program, restrictions in after-school time and transportation were themes that emerged from the interviews. Time constraints during the afternoon for high school students due to familial and scholastic obligations, as well as transportation issues, have been described as barriers in previous youth-led study (Mellanby et al., 2000). Another study with high school students also perceived the same barriers; however, the program was school based and was able to implement activities during the lunchtime to increase participation and address after-school time constraints (Bush, Laberge, & Laforest, 2010). Recruiting youth from the community, either living or studying near the program, may be an effective way to address transportation problems.
However, personal concerns and fears surrounding how to relate to high school students as future program leaders were also listed as an important barrier to Wave 1 BHCK youth-leaders. Previous research using college students to mentor teens in a healthy lifestyle behavior intervention found that discussing other topics in addition to those from the program helped college students relate better with students (Black et al., 2012). The program was successful in changing teens’ diet and physical activity behavior by using college students as mentors to teens (Black et al., 2010). This example suggests that the relationship between college/high school students and middle school–aged students (mentor–mentee) can be rewarding to all groups. Furthermore, involving youth-leaders in the process of identifying and recruiting new leaders may be effective to promote youth-leaders’ confidence and respect toward younger leaders.
Selection of youth to participate in the program is another issue that needs to be considered for future programing. Previous research with youth has used peer selection or volunteer opportunities (Lytle et al., 2004). However, regarding programs conducted outside of the school setting and led by adolescents, little data exist on the identification and selection process. Our findings indicated that recreation center staff could aid in identification and selection of youth-leaders. Social media and other communication materials should have a hook to gain youths’ interest in the program.
Our findings suggest that youth programs should include activities in the community to maintain youth involvement. Going on field trips to community sites helped adolescents feel connected to the Challenge! program (Black et al., 2012). Black et al. (2012) also reported that college mentors received an hourly stipend, similar to those offered to BHCK youth-leaders in Wave 1, and another study with high school mentors provided a stipend distributed over the course of their study (Smith, 2011). However, other studies did not report any payments or recognition to youth implementing those programs.
These findings and recommendations may be transferrable to other youth-led programs in urban, low-income, predominantly African American settings. However, results may not be relevant to other populations with different cultural or socioeconomic demographics. Also, our youth-leaders’ views may differ from those youth-leaders who did not participate in this study on the basis of relevant programming issues. Moreover, we were able to reach only four recreation center staff to participate in IDIs. Personal and professional schedules and family emergencies precluded participation in the other three interviews. However, we do not believe those reasons were likely be related to experiences with the program. A strength of this study was methodological triangulation through informal meetings and observations to confirm IDI data. Finally, all participants knew that the interviewer was affiliated with the program, which may have affected responses. However, good rapport with interviewees was established, and trust was built to ensure data accuracy.
CONCLUSION
This formative work contributes to our understanding of the activities led by youth to build capacity and institutionalize a nutrition program in Baltimore recreation centers. The successful delivery and sustained implementation of youth-led interventions require support to youth-leaders. Our findings suggest that this support includes responsive supervision and assistance, effective trainings, and incentives for future leaders. Lessons from Wave 1 can be used to find ways to sustain and disseminate important work by youth-leaders in after-school programming. More research on innovative ways to involve youth in obesity prevention programs is needed.
Acknowledgments
The authors would like to thank Baltimore City Recreation Center staff and youth-leaders for their work and participation in the research project. Research reported in this article was supported by the Johns Hopkins Urban Health Institute and the Global Obesity Prevention Center at Johns Hopkins, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Office of the Director, National Institutes of Health, under Award No. U54HD070725. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. AT is supported by a doctoral fellowship from 646 CNPq (GDE: 249316/2013-7).
References
- Ajja R, Beets MW, Huberty J, Kaczynski AT, Ward DS. The Healthy Afterschool Activity and Nutrition Documentation instrument. American Journal of Preventive Medicine. 2012;43:263–271. doi: 10.1016/j.amepre.2012.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum AS, Lytle LA, Story M, Perry CL, Murray DM. Are differences in exposure to a multicomponent school-based intervention associated with varying dietary outcomes in adolescents? Health Education & Behavior. 2002;29:427–443. doi: 10.1177/109019810202900404. [DOI] [PubMed] [Google Scholar]
- Black MM, Arteaga SS, Sanders J, Hager ER, Anliker JA, Gittelsohn J, Wang Y. College mentors: A view from the inside of an intervention to promote health behaviors and prevent obesity among low-income, urban, African American adolescents. Health Promotion Practice. 2012;13:238–244. doi: 10.1177/1524839910385899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black MM, Hager ER, Le K, Anliker J, Arteaga SS, Diclemente C, Wang Y. Challenge! Health promotion/ obesity prevention mentorship model among urban, black adolescents. Pediatrics. 2010;126:280–288. doi: 10.1542/peds.2009-1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Cowgill BO, Elliott MN, Klein DJ, Hawes-Dawson J, Uyeda K, Schuster MA. A randomized controlled trial of students for nutrition and eXercise: A community-based participatory research study. Journal of Adolescent Health. 2014;55:415–422. doi: 10.1016/j.jadohealth.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Elliott MN, Uyeda K, Hawes-Dawson J, Klein DJ, Schuster MA. Preliminary healthy eating outcomes of SNaX, a pilot community-based intervention for adolescents. Journal of Adolescent Health. 2011;48:196–202. doi: 10.1016/j.jadohealth.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush PL, Laberge S, Laforest S. Physical activity promotion among underserved adolescents: “Make it fun, easy, and popular”. Health Promotion Practice. 2010;11(3 Suppl):79S–87S. doi: 10.1177/1524839908329117. [DOI] [PubMed] [Google Scholar]
- Cawley J, Cisek-Gillman L, Roberts R, Cocotas C, Smith-Cook T, Bouchard M, Oz M. Effect of HealthCorps, a high school peer mentoring program, on youth diet and physical activity. Childhood Obesity. 2011;7:364–371. doi: 10.1089/chi.2011.0022. [DOI] [Google Scholar]
- Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- Clarke W, Lauer R. Does childhood obesity track into adulthood? Critical Reviews in Food Science and Nutrition. 1993;33:423–430. doi: 10.1080/10408399309527641. [DOI] [PubMed] [Google Scholar]
- Coleman KJ, Geller KS, Rosenkranz RR, Dzewaltowski DA. Physical activity and healthy eating in the after-school environment. Journal of School Health. 2008;78:633–640. doi: 10.1111/j.1746-1561.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- Dzewaltowski DA, Estabrooks PA, Welk G, Hill J, Milliken G, Karteroliotis K, Johnston JA. Healthy youth places: A randomized controlled trial to determine the effectiveness of facilitating adult and youth leaders to promote physical activity and fruit and vegetable consumption in middle schools. Health Education & Behavior. 2009;36:583–600. doi: 10.1177/1090198108314619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Dennisuk LA, Christiansen K, Bhimani R, Johnson A, Alexander E, Coutinho AJ. Development and implementation of Baltimore healthy eating zones: A youth-targeted intervention to improve the urban food environment. Health Education Research. 2013;28:732–744. doi: 10.1093/her/cyt066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Kumar MB. Preventing childhood obesity and diabetes: Is it time to move out of the school? Pediatric Diabetes. 2007;8:55–69. doi: 10.1111/j.1399-5448.2007.00333.x. [DOI] [PubMed] [Google Scholar]
- Gittelsohn J, Steckler A, Johnson CC, Pratt C, Grieser M, Pickrel J, Staten LK. Formative research in school and community-based health programs and studies: “State of the art” and the TAAG approach. Health Education & Behavior. 2006;33:25–39. doi: 10.1177/1090198105282412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Steeves EA, Mui Y, Kharmats A, Hopkins L, Dennis D. B’More Healthy Communities for Kids: Design of a multi-level intervention for obesity prevention for low-income African American children. BMC Public Health. 2014;14:942. doi: 10.1186/1471-2458-14-942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godfrey E. Proceedings of the 19th annual conference of the Australasian Association for Engineering Education: To Industry and Beyond. North Rockhampton, Queensland, Australia: Central Queensland University; 2008. Sustainability of peer mentoring and peer tutoring initiatives to increase student engagement and reduce attrition; pp. 37–37. [Google Scholar]
- Hamdan S, Story M, French SA, Fulkerson JA, Nelson H. Perceptions of adolescents involved in promoting lower-fat foods in schools: Associations with level of involvement. Journal of the American Dietetic Association. 2005;105:247–251. doi: 10.1016/j.jada.2004.11.030. [DOI] [PubMed] [Google Scholar]
- Hung LS, Tidwell DK, Hall ME, Lee ML, Briley CA, Hunt BP. A meta-analysis of school-based obesity prevention programs demonstrates limited efficacy of decreasing childhood obesity. Nutrition Research. 2015;35:229–240. doi: 10.1016/j.nutres.2015.01.002. [DOI] [PubMed] [Google Scholar]
- King KM, Rice JA, Steinbock S, Reno-Weber B, Okpokho I, Pile A, Carrico K. Kentucky Teen Institute: Results of a 1-year, health advocacy training intervention for youth. Health Promotion Practice. 2015;16:885–896. doi: 10.1177/1524839915588294. [DOI] [PubMed] [Google Scholar]
- Lytle LA, Murray DM, Perry CL, Story M, Birnbaum AS, Kubik MY, Varnell S. School-based approaches to affect adolescents’ diets: Results from the TEENS study. Health Education & Behavior. 2004;31:270–287. doi: 10.1177/1090198103260635. [DOI] [PubMed] [Google Scholar]
- McHugh JE, Lee O, Aspell N, Connolly L, Lawlor BA, Brennan S. Peer volunteer perspectives following a complex social cognitive intervention: A qualitative investigation. International Psychogeriatrics. 2016;28:1545–1554. doi: 10.1017/S1041610216000144. [DOI] [PubMed] [Google Scholar]
- Mellanby AR, Rees JB, Tripp JH. Peer-led and adult-led school health education: a critical review of available comparative research. Health Educ Res. 2000;15(5):533–545. doi: 10.1093/her/15.5.533. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM, Saldaña J. Qualitative data analysis A methods sourcebook. 3rd. Thousand Oaks, CA: Sage; 2013. [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. Journal of the American Medical Association. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen M, Krølner R, Klepp KI, Lytle L, Brug J, Bere E, Due P. Determinants of fruit and vegetable consumption among children and adolescents: A review of the literature. Part I: Quantitative studies. International Journal of Behavioral Nutrition and Physical Activity. 2006;3:22–22. doi: 10.1186/1479-5868-3-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronsley R, Lee AS, Kuzeljevic B, Panagiotopoulos C. Healthy Buddies™ reduces body mass index z-score and waist circumference in Aboriginal children living in remote coastal communities. Journal of School Health. 2013;83:605–613. doi: 10.1111/josh.12072. [DOI] [PubMed] [Google Scholar]
- Roth JL, Brooks-Gunn J. Youth development programs: Risk, prevention and policy. Journal of Adolescent Health. 2003;32:170–182. doi: 10.1016/S1054-139X(02)00421-4. [DOI] [PubMed] [Google Scholar]
- Santos RG, Durksen A, Rabbanni R, Chanoine JP, Lamboo Miln A, Mayer T, McGavock JM. Effectiveness of peer-based healthy living lesson plans on anthropometric measures and physical activity in elementary school students: A cluster randomized trial. JAMA Pediatrics. 2014;168:330–337. doi: 10.1001/jamapediatrics.2013.3688. [DOI] [PubMed] [Google Scholar]
- Sato PM, Anderson Steeves E, Carnell S, Cheskin LJ, Trude ACB, Shipley C, Gittelsohn J. A youth mentor-led nutritional intervention in urban recreation centers: A promising strategy for childhood obesity prevention in low-income neighborhoods. Health Education Research. 2016;31:195–206. doi: 10.1093/her/cyw011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sipe CL. Mentoring programs for adolescents: A research summary. Journal of Adolescent Health. 2002;31:251–260. doi: 10.1016/S1054-139X(02)00498-6. [DOI] [PubMed] [Google Scholar]
- Smith LH. Piloting the use of teen mentors to promote a healthy diet and physical activity among children in Appalachia. Journal for Specialists in Pediatric Nursing. 2011;16:16–26. doi: 10.1111/j.1744-6155.2010.00264.x. [DOI] [PubMed] [Google Scholar]
- Smith LH, Holloman C. Comparing the effects of teen mentors to adult teachers on child lifestyle behaviors and health outcomes in Appalachia. Journal of School Nursing. 2013;29:386–396. doi: 10.1177/1059840512472708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker SA, Avis M. Common reasons why peer education fails. Journal of Adolescence. 1999;22:573–577. doi: 10.1006/jado.1999.0250. [DOI] [PubMed] [Google Scholar]
- Wong NT, Zimmerman MA, Parker EA. A typology of youth participation and empowerment for child and adolescent health promotion. American Journal of Community Psychology. 2010;46:100–114. doi: 10.1007/s10464-010-9330-0. [DOI] [PubMed] [Google Scholar]
- Woodgate RL, Sigurdson CM. Building school-based cardiovascular health promotion capacity in youth: a mixed methods study. BMC Public Health. 2015;15(1):421–421. doi: 10.1186/s12889-015-1759-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancey AK, Siegel JM, McDaniel KL. Role models, ethnic identity, and health-risk behaviors in urban adolescents. Archives of Pediatrics & Adolescent Medicine. 2002;156:55–61. doi: 10.1001/archpedi.156.1.55. [DOI] [PubMed] [Google Scholar]


