Abstract
Objective:
The aim of our study was to compare the biomechanical stability of the Proximal Femoral Nail Antirotation (PFNA) (with 200 mm, 240 mm and 280 mm-long main nails) for the management of unstable intertrochanteric femoral fractures.
Methods:
Tronzo-Evans Type IV and V fractures were built by applying a three-dimensional finite element model. Further, PFNA-II with 200 mm, 240 mm and 280 mm-long main nails were applied for fixation. The above model is the creation of 3 researchers designed in order to obtain average values of numerical stress. Von Mises stress distribution and medial & lateral stress peak of the femur and PFNA were compared.
Results:
240 mm and 280 mm PFNA medial stress peak was reduced significantly in comparison to 200 mm PFNA (p<0.05). However, there was no difference between 240 mm and 280 mm PFN. Also, no statistical difference was observed with any of 3 lengths in both medial & lateral stress peak for Evans Type IV and V PFNA.
Conclusion:
240 mm and 280 mm PFNA could reduce femur fixation medial stress peak. Further, they were more efficient in comparison to the 200 mm PFNA, and their biomechanical stability was similar to that of the 280 mm nail.
Keywords: Proximal Femoral Nail Antirotation, Unstable Intertrochanteric Fractures, Stress Peak
Introduction
Unstable intertrochanteric femoral fractures are extra-articular fractures, with a high incidence in the elderly, are mainly caused by low-energy trauma, and account for approximately 50% of hip fractures[1]. Surgical treatment of these fractures includes extramedullary fixation, intramedullary fixation or hip replacement. Intramedullary nailing has been shown both in animal model studies and clinical trials in humans to be associated with improved weight-bearing capacity and function overall, as compared to fixation with dynamic hip screws[2,3]. However, major complications include anterior thigh pain and implant failure/secondary fracture, with a reported incidence rate of approximately 2.0~3.5%, thus seriously affecting the patients’ quality of life[4]. A recently published study reported that elongated PFNA increased fracture distal action length and the contact area between the main nail and the femur; dispersion of stress levels lead, according to the authors, to a significant reduction in the rate of complications[5]. However, another recent study suggested that elongated PFNA had no significant benefit to reduce postoperative re-fracture incidence[6]. Based on these studies, the present study assessed the distribution of stress within the femur with the internal fixator by building a three-dimensional finite element model of unstable fracture (Tronzo-Evans Type IV and V). The study thus provides reference basis for improving the PFNA internal fixation biomechanical stability.
Materials and methods
Three-dimensional finite element model
One healthy Chinese male volunteer was chosen; age: 25 years, weight: 72 kg, height: 175 cm, limb length: 97 cm. He had no history of prior trauma, infection or arthritis or any other condition known to affect the musculoskeletal system. 64-slice spiral CT (American GE) was performed for the hip joints at both sides. Recording parameters included voltage: 120 kv, current: 120 mA, time: 1s and thickness at 0.625 mm. The scanning area range was from the top of greater trochanter to knee joint and data were saved in DICOM format. Right proximal femur data were chosen to import into Mimics 13.0 software, and grey threshold was set for partition. Evans Type IV and V fractures were simulated for cutting and curved surface was fitted. PFNA-II with 200 mm, 240 mm and 280 mm-long main nails was chosen. The proE 4.0 three-dimensional drawing software was applied for three-dimensional virtual reconstruction. A Geometric model of femur and internal fixation was imported to finite element analysis pre-processing software Hypermesh 10.0 for assemble. The solid 85 element was adopted. The specific nodes and elements number for fractures are shown in Table 1. Internal fixation and bone materials were homogeneous, and references are referred for isotropy and material property. Fixation position followed the standard operation method, and main nail was located in the middle and lower back part of femoral head. It was imported to Abaqus, post-processing software to obtain the finite element model (Figure 1). Boundary conditions and loading processing were as follows: the surface was set as complete fracture in contact status, friction coefficient was 0.2, freedom constraint of all nodes for medial & lateral infra-glenoid margin was 0, i.e. the displacement of distal nodes on X, Y and Z axis was 0. Simplified model was adopted, the force of abducts muscle adjacent to the greater trochanter and lateral femur muscles were chosen as external loads. Femur stress distribution allowed a bearing of 70 kg load.
Table 1.
Number of nodes and elements for 2 types of fracture by PENA fixation with three kinds of length.
| Fracture type | 200 mm | 240 mm | 280 mm | |||
|---|---|---|---|---|---|---|
| Number of nodes | Number of elements | Number of nodes | Number of elements | Number of nodes | Number of elements | |
| Evans Type IV | 25614 | 95647 | 26459 | 98546 | 27485 | 10235 |
| Type V | 28549 | 11524 | 27645 | 12514 | 30265 | 13206 |
Figure 1.
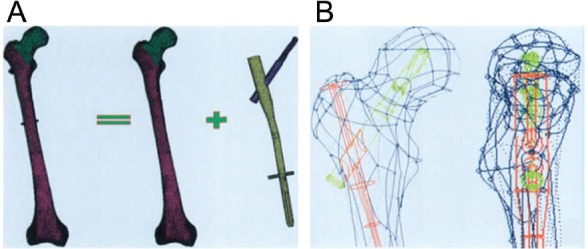
Three-dimensional finite element model. A: Bone was cut according to fracture type, and PFNA fixation with different lengths was assembled, the fixation position followed standard operation method, screw blade was located in the central back medial part of femoral neck for grid partition; B: Positive lateral position after fixation, and main nail was located in the central back medial part of femoral head).
Observation index
Observation index included stress distribution and stress peaks of four zones including medial & lateral for femur and internal fixation.
Statistical methods
SPSS20.0 software was used for statistical analysis, and measurement data were presented as mean ± standard deviation, and single factor ANOVA analysis was used for comparison among groups, and LSD-t test was used for pair-wise comparison; the difference had statistical significance when p<0.05.
Results
Stress distribution, peak and position analysis for femur
The medial stress peaks of 240 mm and 280 mm-long PFNA were significantly reduced in comparison to 200 mm PFNA. However, no statistical significant difference was noticed between 240 mm and 280 mm-long PFNA (Table 2). Also, there were no differences among medial & lateral stress peaks for Evans Type IV and V PFNA with all three-length types (p>0.05).
Table 2.
Stress distribution, peak and position analysis for femur. *p<0.05 Compared with PFNA 200 mm.
| PFNA length | Evans Type IV | Type V | ||
|---|---|---|---|---|
| Medial stress peak (MPa) | Lateral stress peak | Medial stress peak | Lateral stress peak | |
| 200 mm | 23.42±1.26 | 15.62±1.62 | 23.65±1.54 | 14.43±1.35 |
| 240 mm | 19.56±1.32* | 17.85±1.75 | 20.13±1.96 | 16.62±1.48 |
| 280 mm | 19.42±1.45* | 17.96±1.83 | 20.24±1.78 | 16.75±1.62 |
Stress distribution, peak and position analysis for internal fixation
The internal fixation proximal medial stress peaks of 240 mm and 280 mm-long PFNA were reduced significantly when compared with 200 mm-long PFNA. Further, there was no statistical difference between 240 mm and 280 mm-long PFNA. Also, there was no difference between proximal medial & lateral stress peak and distal one for Evans Type IV and V PFNA (Table 3).
Table 3.
Stress distribution, peak and position analysis for internal fixation. *p<0.05 compared with PFNA 200 mm.
| PFNA length | Evans Type IV | Type V | ||||||
|---|---|---|---|---|---|---|---|---|
| Internal fixation proximal medial stress peak (MPa) | Proximal lateral stress peak | Distal medial stress peak | Distal lateral stress peak | Proximal medial stress peak | Proximal lateral stress peak | Distal medial stress peak | Distal lateral stress peak | |
| 200 mm | 156.48±8.52 | 112.62±9.67 | 35.68±4.62 | 15.23±3.63 | 168.95±10.25 | 113.74±14.63 | 38.62±11.52 | 14.47±13.26 |
| 240 mm | 112.36±6.54* | 98.43±7.62 | 52.85±5.23 | 16.37±3.57 | 124.52±12.32 | 106.95±16.25 | 58.93±12.25 | 15.58±13.26 |
| 280 mm | 108.51±6.38* | 93.54±7.84 | 55.43±5.57 | 16.58±3.34 | 119.67±13.54 | 108.52±13.52 | 61.25±14.52 | 16.23±15.63 |
Discussion
The present study showed that the femur medial stress peaks of the 240 mm and 280 mm-long PFNA were reduced significantly in comparison with those of the 200 mm-long PFNA. Lateral stress peak was increased, and the difference had statistical significance. However, there was no difference in femur medial stress peak between 240 mm and 280 mm-long PFNA. Results revealed that femur proximal medial & lateral stress distribution were irrelevant to the fracture type. It was considered that Type IV referred to three-part fractures including the lesser trochanter and small portion of medial cortical defects. On the other hand, Type V referred to three-part fractures containing the lesser trochanter and large portion of medial cortical defects. The two types of fracture positions had the same fracture position and range[7]. The increasing PFNA length reduced the femur medial stress peak leading to decrease in the risk for femur re-fracture. This in turn benefited early weight-bearing exercise and improved hip joint function[8]. It was noted that the femur medial stress peaks of 240 mm and 280 mm-long PFNA were equivalent to lateral stress peak[9]. Further analysis revealed that 240 mm and 280 mm-long PFNA internal fixation proximal medial stress peaks were reduced when compared with 200 mm-long PFNA. It was pointed out that internal fixation proximal as well as distal medial & lateral stress distribution peaks were irrelevant to unstable fracture type. However, they were related to internal fixation implantation position, fracture injury degree and fixation effect. A study in the recent past reported that Type V internal fixation proximal medial stress peak was lower[10]. This observation might be related to more severe injury and fixation effect. It could reduce internal fixation proximal medial stress peak by increasing PFNA length leading to reduction in lateral pain[11]. So, the stress was dispersed in the distal medial part, resulting in better safety with less pain[12]. Therefore, we propose that 240 mm and 280 mm PFNA could reduce femur and internal fixation medial stress peak compared with 200 mm PFNA. Further, the biomechanical stability of 240 mm-long PFNA is similar to that of 280mm-long PFNA.
The innovation of the present study is the use of three-dimensional finite element model analysis, and the biomechanical stability of PFNA with different lengths. The present study objectively and quantitatively evaluated the stress distribution and stress peak of different sites with better precision. Other studies took in-vitro femur specimens, and built fracture injury artificially, displayed digitally strain value of detector, which had great variability in operation[13]. In addition, some studies made analysis on stress distribution of stable and unstable intertrochanteric fracture for PFNA, Asian PFNA (PFNA-II), InterTan and Gamma provided important reference for proximal femoral fractures and apply reasonable internal fixation[14,15].
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Chang JD, Kim IS, Lee SS, Yoo JH, Hwang JH. Unstable intertrochanteric versus displaced femoral neck fractures treated with cementless bipolar hemiarthroplasty in elderly patients;a comparison of 80 matched patients. Orthop Traumatol Surg Res. 2016;24:123–124. doi: 10.1016/j.otsr.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Yu W, Zhang X, Zhu X, Yu Z, Xu Y, Zha G, Hu J, Yi J, Liu Y. Proximal femoral nails anti-rotation versus dynamic hip screws for treatment of stable intertrochanteric femur fractures: an outcome analyses with a minimum 4 years of follow-up. BMC Musculoskelet Disord. 2016;17:222–7. doi: 10.1186/s12891-016-1079-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xie H, Chen S, Zhou B. Comparison of proximal femoral nail antirotation-II and proximal femoral nail antirotation in fixation of femoral intertrochanteric fracture. Zhonghua Yi Xue Za Zhi. 2015;95:2346–2350. [PubMed] [Google Scholar]
- 4.Ma JX, Wang J, Xu WG, Yu JT, Yang Y, Ma XL. Biomechanical outcome of proximal femoral nail antirotation is superior to proximal femoral locking compression plate for reverse oblique intertrochanteric fractures: a biomechanical study of intertrochanteric fractures. Acta Orthop Traumatol Turc. 2015;49:426–32. doi: 10.3944/AOTT.2015.14.0306. [DOI] [PubMed] [Google Scholar]
- 5.Wei J, Qin DA, Guo XS. Curative effect analysis on proximal frmora nail antirotation for the treatment of femoralintertrochanteric fracture and integrity of lateral trochanteric wall. Zhongguo Gu Shang. 2015;28:572–5. [PubMed] [Google Scholar]
- 6.Hélin M, Pelissier A, Boyer P, Delory T, Estellat C, Massin P. Does the PFNA™ nail limit impaction in unstable intertrochanteric femoral fracture? A 115 case-control series. Orthop Traumatol Surg Res. 2015;101:45–49. doi: 10.1016/j.otsr.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Zhang Y, He W, Liu YW, Feng LZ. Comparison of the efftec between eccentric fixation and intramedullary fixation for treatment of intertrochanteric fractures. Zhongguo Gu Shang. 2015;28:117–121. [PubMed] [Google Scholar]
- 8.Liu JJ, Shan LC, Deng BY, Wang JG, Zhu W, Cai ZD. Reason and treatment of failure of proximal femoral nail antirotation internal fixation for femoral intertrochanteric fractures of senile patients. Genet Mol Res. 2014;13:5949–5956. doi: 10.4238/2014.August.7.10. [DOI] [PubMed] [Google Scholar]
- 9.Wang H, Wang Y, Yan B, Zhong L, Jiang J. Measuring method of tip-apex distance in treatment of femoral intertrochanteric fracture with proximal femoral nail antirotation. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014;28:53–55. [PubMed] [Google Scholar]
- 10.Huang Y, Zhang C, Luo Y. A comparative biomechanical study of proximal femoral nail (InterTAN) and proximal femoral nail antirotation for intertrochanteric fractures. Int Orthop. 2013;37:2465–2473. doi: 10.1007/s00264-013-2120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee PY, Lin KJ, Wei HW, Hu JJ, Chen WC, Tsai CL, Lin KP. Biomechanical effect of different femoral neck blade position on the fixation of intertrochanteric fracture: a finite element analysis. Biomed Tech (Berl) 2016;61:331–336. doi: 10.1515/bmt-2015-0091. [DOI] [PubMed] [Google Scholar]
- 12.Yuan GX, Shen YH, Chen B, Zhang WB. Biomechanical comparison of internal fixations in osteoporotic intertrochanteric fracture. A finite element analysis. Saudi Med J. 2012;33:732–739. [PubMed] [Google Scholar]
- 13.Wu X, Yang M, Wu L, Niu W. A Biomechanical Comparison of Two Intramedullary Implants for Subtrochanteric Fracture in Two Healing Stages: A Finite Element Analysis. Appl Bionics Biomech. 2015:475261. doi: 10.1155/2015/475261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goffin JM, Pankaj P, Simpson AH, Seil R, Gerich TG. Does bone compaction around the helical blade of a proximal femoral nail anti-rotation (PFNA) decrease the risk of cut-out?: A subject-specific computational study. Bone Joint Res. 2013;2:79–83. doi: 10.1302/2046-3758.25.2000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karaarslan AA, Aycan H, Mayda A, Ertem F, Sesli E. Biomechanical comparision of femoral intramedullary nails for interfragmentary rotational stability. Eklem Hastalik Cerrahisi. 2015;26:131–136. doi: 10.5606/ehc.2015.28. [DOI] [PubMed] [Google Scholar]


