Abstract
The National Rural Health Mission (NRHM) has been successful in reducing maternal, infant, and child mortality rates in India. In addition, it has tremendously improved the infrastructure of India's public health system. It has also placed at least one Accredited Social Health Activist worker in every village of India. However, the NRHM has not been able to overcome the shortage of specialist doctors at Community Health Centre (CHC) level. During 10 years of NRHM, only 81 gynecologists, 34 physicians, and 290 pediatricians have been added at the CHC level. Family medicine specialist can be a viable alternative to these specialist doctors, fill the existing gap, and drastically improve the quality of health care provided at CHC level.
Keywords: Family medicine, India, National Rural Health Mission
Introduction
Achievements of India's National Rural Health Mission (NRHM) have been remarkable; it is because of this program that India is much closer to achieving health-related Millennium Development Goals. It has accelerated the decline in maternal, neonatal, infant, and child mortality rates.[1] In addition, NRHM has vastly improved the physical infrastructure of India's public health system. But perhaps the most astonishing feat NRHM has achieved is that it has successfully placed more than half a million grass-root community health workers (Accredited Social Health Activist) in villages of India.[2]
Despite all these remarkable achievements, there is one crucial area in which the achievements of NRHM are questionable and, i.e., the availability of specialist doctors at the peripheral level. NRHM has devised strategies to attract specialist doctors to work in rural areas by providing better incentives, handsome salaries, and flexible working conditions but so far these strategies have not met with any considerable and permanent success. From time to time, NRHM has devised a host of strategies to put in place the required workforce for India's health system. These efforts included training plain MBBS doctors in specially designed short courses such as Emergency Obstetric Care and Life Saving Anesthetics skill.[2] These courses were designed for one and only one purpose and, i.e., to reduce maternal death. However, such courses cannot ensure the provision of quality health care for patients as doctors trained in these short courses cannot replace a professionally trained specialist whether it is a gynecologist/obstetrician, pediatrician, surgeon, physician, or anesthetist. To bring this problem of Indian health system into focus, we analyzed the deployment of a specialist doctor at Community Health Centre (CHC) during the first decade of NRHM.
One CHC is designed to cater the health needs of 80,000–120,000 population.[3] CHC is a secondary level facility providing referral services for patients from primary health centers (PHCs) and provides specialized care in four different medical specialties.[3] As per the Indian Public Health Standards (IPHS), there should be one each of surgeons, pediatricians, gynecologists, physicians, and anesthesiologists at each CHC.[3] In the year 2015, one CHC was catering to an average population of 154,512.[4] Data on the rural health-care system are published every year in the form of rural health statistics since the year 2005 by the government of India. Governmental agency publishing rural health statistics does not publish data as per norms of Indian public health standard, but they have their format/questionnaire for collecting information.[4] We analyzed data on the availability of specialists' doctor posted at CHC for the year 2005, 2010, and 2015. We analyzed data for three types of specialist doctors, i.e., pediatricians, obstetricians, and physicians. Data on surgeon are available but not included, and data on anesthetics are not published, hence are not included here.
National Rural Health Mission's First 10 Years: More Misses than Hits
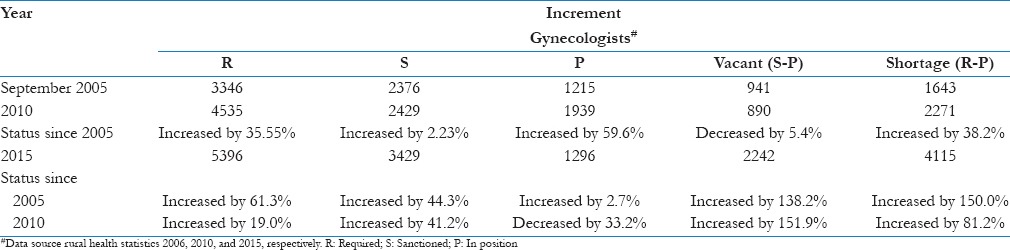
In India, there were a total 3346 CHCs in the year 2005, i.e., during the year, NRHM was launched. Because of increased funding and other factors, the number of CHCs rose to 4535 by 2010 (an increase of 35.55%) and to 5396 by 2015 (an increase of 61.3%).[4,5,6] After the launch of NRHM, many PHCs were upgraded to CHCs without making an arrangement for required workforce, resulting in acute shortage of workforce. During the first 10 years of NRHM, there has been a net increase of only 81 gynecologists at all CHCs across India, which was a mere 2.7% increase as compared to 61.3% increase in the number of CHCs since the inception of NRHM [Table 1]. During the first 5 years of NRHM (from 2005 to 2010), there has been an increase of 724 gynecologists at CHC, but during the second 5 years (from 2010 to 2015), their number decreased and 624 gynecologists who were posted at CHC during 2010 have either been transferred somewhere else or have left their jobs.
Table 1.
Obstetricians and gynecologists at community health centers during 10 years of the National Rural Health Mission
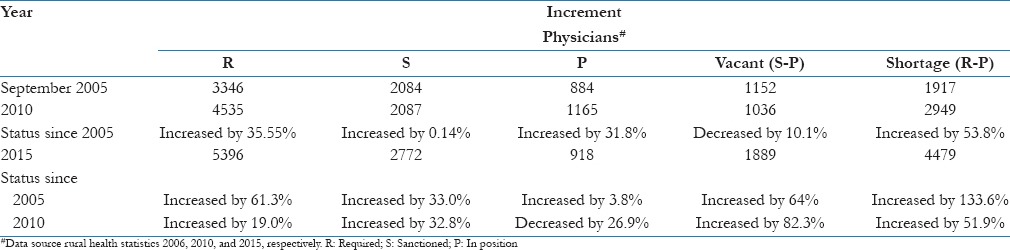
Between the year 2005 and 2015, there was an increase of 290 pediatricians at the CHCs as against an increase of 2050 CHCs [Table 2]. During the first 5 years of NRHM, there was an increase of 633 pediatricians at CHC, but during the second 5 years, the number reduced and 308 pediatricians who were earlier available at CHC during 2010 have been either posted elsewhere or have left their jobs. During the first 5 years of NRHM (from 2005 to 2010), there has been an increase of 281 physicians at CHC but during the second 5 years (2010–2015), number declined by 247 so that the net gain in the decade was only 34 doctors [Table 3].
Table 2.
Pediatricians at community health centers during 10 years of the National Rural Health Mission
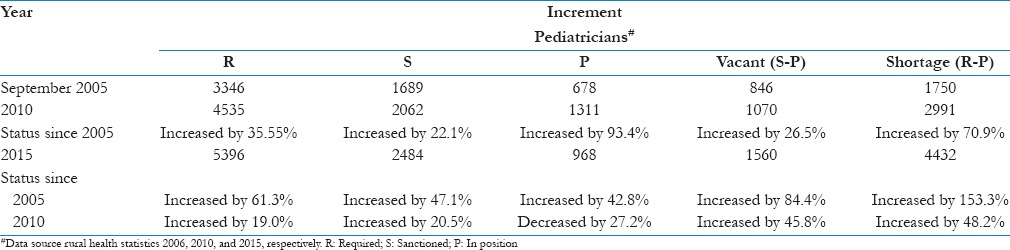
Table 3.
Physicians at community health centers during 10 years of the National Rural Health Mission
How Long will it Take to Fill the Existing Vacancies?
The mammoth task of filling the current vacancies may not be impossible, but we will be fooling ourselves if we do not accept that it is one of the most challenging problems currently faced by Indian health system. A total of only 81 gynecologists were added in 10 years at CHCs, i.e., 8.1 per year. Currently, there is a shortage of 4115 gynecologists, and going by an average rate of 8 gynecologists per year, it will take 514 years to fill the current vacancies alone. Even if we take the peak rate of 144 gynecologists per year (724 gynecologists between the years 2005 and 2010), it will take 28 years to fill the present vacancies only. Such pathetic shortage of gynecologist continues to persist despite the fact that medical colleges in India are producing more than 2033 gynecologists every year.[7]
During 10 years of NRHM, an average of 29 pediatricians was added every year. As of now, there is a shortage of 4432 pediatricians, and by going at the average rate of 29 pediatricians per year, it will take 152 years to fill the current vacancies alone. Such is the scenario when medical colleges across India are producing more than 1773 pediatricians per year.[7] Only 34 physicians were added in 10 years, i.e., 3.4 per year. At present, there is a shortage of 4479 physicians at CHC level, and going by the current rate of 3.4 physicians per year, it will take 1317 years (more than a millennium) to fill the current vacancies alone. Such is the condition when more than 2394 medicine postgraduates are passing annually from medical colleges of India.[7]
The Case of Specialist Doctors: Difficult to Hire and Even more Difficult to Retain!
As noted above, there was a considerable improvement during the first 5 years of NRHM. It tells us that problem is not in hiring doctors but in retaining them. The inability to retain the doctors might be due to the hostile environment in which doctors are made to work. There have been countless reports in the newspapers from every corner of the country and strikes by doctors to highlight a range of issues which make it difficult for doctors to work in government hospitals. Most cited reasons include lack of basic amenities, lack of drugs and equipment, poor infrastructure, long working hours, delay in salaries, and being assaulted by patient's relatives. In contrast, the private sector offers better working condition, better salary, and professional working atmosphere, so a considerable number of doctors ultimately leave government jobs and land up in private sector. The problem of specialist workforce becomes more complicated by the fact that a fully functioning CHC requires a pediatrician, obstetrician, surgeon, physician, and an anesthetist to be deployed simultaneously at a single CHC around the clock.[3] Manning a CHC with required workforce has proved to be a very arduous task in itself and to maintain such workforce at one place for the long term will be another cumbersome task to worry about.
The facts and figures mentioned above make one thing crystal clear that India has no shortage of either infrastructure or human resource to fill the existing gap of India's rural health-care system, the only thing lacking is the political leadership to take the tough decisions to overcome the existing deficiencies. Shortage of specialist doctors has been gripping Indian health system for many decades now. The existing gap in terms of a number of specialist doctors required is very broad and very deep. Going by the trends mentioned above, it seems highly dubious that the obstacle of deploying required specialist workforce can be solved in the near future.
Einstein defined insanity as doing something over and over again and expecting different results. To fill the current vaccines, the government should start thinking afresh where and how things went from wrong to terrible to horrible. What Indian government need is a paradigm shift in its thinking and strategy to deal with this problem. One thing that is very obvious from the facts mentioned above is that there exists a total disconnection between the medical education and health system in India.
Family Medicine is not an Out of Box Idea but a Forgotten One!
After trying every trick they can think off, it is high time that government should sincerely focus on developing a cadre of family medicine specialist and deploy them at CHCs. This is the most appropriate solution because, at present, a doctor posted at a CHC has to treat an adult, a mother, newborn, and children in the same outpatient department, thus making a family medicine specialist most suitable candidate for posting at CHC. Even after simultaneous deployment of a pediatrician, obstetrician, and a physician at CHC, we cannot expect these specialists to work around the clock and 365 days a year. When any of these specialists goes on leave or is unavailable due to any reason, the other specialist doctor available in the facility cannot carry out the work of a specialist doctor who is unavailable. In this regard, it would be strategically as well as logically correct to deploy three to four family medicine specialists at a single CHC to provide a full range of services around the clock and throughout the year. In this way, even if one or two doctors are unavailable at CHC, those present can still provide every desired service. To produce such workforce, we need to design a special curriculum for family medicine in accordance with the list of essential and desirable services to be provided at CHC as per IPHS standards. Such an approach can resolve the age old problem of a specialist doctor in the span of just 5–7 years.
In this sense, we have reasons to cherish, since the beginning of this decade, considerable thrust has been given by policy-makers and family medicine practitioners to revive the concept of family medicine as a specialty in India. Successful organization of two national level conferences of family medicine in the last 3 years is the results of these efforts. A brainstorming consultation exercise has already been conducted under the aegis of the National Health System Resource Center during which many experts have shared their views and ideas about reviewing family medicine in India.[8] Policy-makers both in the government and outside government have advocated that state governments should start utilizing the already available workforce of this specialty. For the success of this program, it is crucial that family medicine must attract bright medical graduate. To convince a student to choose family medicine as their career, it is essential to introduce family medicine as a separate subject at undergraduate level. Newly established AIIMS under Pradhan Mantri Swasthya Yojana has already taken the first step in this regard by the establishing Department of Community and Family Medicine.[9] Another premier institute such as JIPMER and PGI should follow this initiative. Furthermore, to promote undergraduate students to opt family medicine, the government needs to establish a system in which the desired workforce (family medicine specialist) is given an appropriate post. For this, it is essential to make changes in the current hiring policies of government so as to recognize family medicine as a specialty and make a rule to post a family medicine specialist at the current vacant posts at CHCs. Simultaneously, the complete career pathway of family medicine graduate should be delineated so as to remove any dilemma in the mind of those opting for this specialty. An example of such strategy would be to allow family medicine graduate to appear for DM examinations as a means to advance their career after serving in rural areas for a minimum fixed duration.
Before concluding, we would like to stress that the policy-makers should exercise caution in the due process of reviving family medicine in India. We should not simply copy the western model of family medicine but should take into consideration the existing gap and demand of Indian health system. In this regard, policy-makers should give special emphasis on meeting the demand related to existing gap in pediatric, anesthetic, and obstetric care prevailing in India. We would like to conclude by reminding the policy-makers of India that the world as a whole is moving toward universal health coverage; if India has to keep pace with the world, it must solve the problem of workforce for its rural, peripheral, and backward areas at the earliest.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Annual Health Report 2013-2014 (AHS 2014). Department of Health and Family Welfare, Government of India. 2014 [Google Scholar]
- 2.Five Years of NRHM 2009-2014 (NRHM 2014). Ministry of Health and Family Welfare, Government of India. 2014 [Google Scholar]
- 3.India Public Health Standard 2012 – Community Health Centre (IPHS CHC 2012) Ministry of Health and Family Welfare, Government of India. 2012 [Google Scholar]
- 4.Ministry of Health and Family Welfare. Rural Health Statistics 2015 (RHS 2015) [Last accessed on 2016 Mar 21]. Available from: http://www.nrhm.mis.nic.in/page/RHS2015.aspx .
- 5.Ministry of Health and Family Welfare Rural Health Statistics 2010 (RHS2010) [Last accessed on 2016 Mar 21]. Available from: http://www.nrhm.mis.nic.in/page/RHS2010.aspx .
- 6.Ministry of Health and Family Welfare Rural Health Statistics 2006 (RHS 2006) [Last accessed on 2016 Mar 25]. Available from: http://www.nrhm.mis.nic.in/page/RHS2006.aspx .
- 7.List of Post Graduate Seats in Different Specialties in Medical Colleges in of India (MCI 2016) [Last cited on 2016 Mar 10]. Available from: http://www.mciindia.org/informationdesk/forstudents/listofcollegesteachingPost graduatecourses.aspx .
- 8.National Consultation on Family Medicine Programme; Report and Recommendations. [Last accessed on 2016 Mar 25]. Available from: http://www.nhsrcindia.org . [DOI] [PMC free article] [PubMed]
- 9.Kumar R. Academic Community Medicine in 21st Century: Challenges and Opportunities. Indian J Community Med. 2009;34:1–2. doi: 10.4103/0970-0218.45367. [DOI] [PMC free article] [PubMed] [Google Scholar]


