Abstract
Context:
Globally, around 16% of under-five children die due to pneumonia. Childhood pneumonia, if identified early is a readily treatable through low-cost antibiotics. Access to timely and appropriate care is a key action to control pneumonia.
Aims:
The aim of the study was to understand the caregiver's care-seeking behavior for the management of childhood pneumonia among rural and urban poor communities in Lucknow.
Settings and Design:
Rural areas and urban slums of Lucknow district, from September 2014 to August 2015.
Subjects and Methods:
A community-based cross-sectional study. Total of 1065 under-five children were selected by multistage random sampling method. Caregivers of children (<5 years of age) were interviewed through pretested, semi-structured interview schedule. Information was gathered on episode of cough, difficult breathing, and or chest indrawing in child within 2 weeks preceding the survey, and caregiver's treatment seeking practices.
Results:
Out of total 1065 children, 52 (%) had pneumonia within 2 weeks preceding the survey. At the onset of illness, difficult/fast breathing was identified by 86.5% caregivers, but majority of them did not perceive it as a serious condition and resort to home remedies. Only 9.6% sought appropriate care at onset of illness. Appearance of chest indrawing in the child was identified by caregivers as a serious condition and sought treatment from outside. The mean time taken from onset of illness to the seeking care from health facility was around 2½ days (2.39 ± 0.75). Qualified private practitioners (70.5%) were the preferred choice and majority (87.0%) of the children received antibiotic for pneumonia. However, even after perception of seriousness of the illness, 26.8% and 11.1% caregivers in urban slums and rural areas, respectively sought inappropriate care at the first consultation.
Conclusions:
Caregivers were unable to perceive the severity of fast breathing leading to the delayed initiation of the appropriate treatment. There is a need of community mobilization through behavior change communication interventions to promote early symptom recognition and appropriate care seeking for pneumonia.
Keywords: Care seeking, caregivers, childhood pneumonia, rural, urban slum
Introduction
Pneumonia and diarrhea are leading killers of under-five children, predominantly concentrated in 15 developing countries.[1] India and Nigeria are the two countries with the largest burden of these two diseases and also have low coverage levels for prevention and treatment interventions.[2] Pneumonia contributes to 15% of infant deaths in India.[3] Since a large proportion of pneumonia cases in children of the developing world, is caused by bacterial pathogens, prompt treatment with a full course of effective antibiotics is key to reducing pneumonia deaths. Early initiation of antibiotic therapy soon after symptoms such as fast breathing with cough, the progression of pneumonia infection can be blunted.[2]
Delay in seeking appropriate care or not seeking any care at all contributes to large number of pneumonia deaths in developing countries.[4] Studies identified symptom recognition as a key barrier for care seeking for pneumonia.[5,6,7,8] Multiple Indicator Cluster Surveys (2000–2006) in 55 countries shows that key pneumonia symptoms (difficult and/or fast breathing) are not widely recognized; only about one in five caregivers recognize these danger signs.[5] Care seeking for pneumonia among children is also very poor in the communities. National Family Health Survey-3, India, shows that only 64.2% children with acute respiratory infection (ARI) or fever were taken to a health facility, care seeking was low in rural areas (59.2%) in comparison to urban areas.[9] Previous studies from different states of India revealed that about one-third families do not seek care for their children suffering from pneumonia. Even when families do seek care, they often do so from informal health providers, especially in the northern states.[10]
Excluding neonatal causes, childhood pneumonia is the leading killer (17%) of children, with high prevalence (27.9%) of ARIs in Uttar Pradesh.[11] Information on care-seeking behavior for childhood pneumonia will help policy maker to set strategies to decrease pneumonia-related morbidity and mortality and also enabling state to achieve its child health-related goals. It is important to understand how caregivers perceive pneumonia, when and where they go for treatment of pneumonia. Therefore, the present study was conducted to understand the care-seeking behavior of caregivers regarding childhood pneumonia in rural and poor urban community of Lucknow district.
Subjects and Methods
Study setting
Lucknow district had a total population of 4589,838 persons with rural population of 15,50,842.[12] As per State Urban Development Agency UP, slum population was 645,000 in 2001.[13] The under-five mortality of Lucknow is 58 with infant mortality rate of 44/1000 live births.[11] Female literacy rate of the district is 71.5%.
Study design
A community-based descriptive cross-sectional study conducted in rural areas and urban slums of from September 2014 to August 2015.
Sample size and sampling technique
Multistage random sampling method was used to select the children in the study. Considering the prevalence (p) of childhood pneumonia in Uttar Pradesh around 8%,[9] absolute permissible error (2%), and 5% level of significance, the sample size was calculated to be 710 under-five children. Multiplying design effect of 1.5, it came to 1065, and taking the nonresponse rate of 5%, final sample size was calculated to be 1118 (~1100) under-five children.
For representation of rural and urban population as per their distribution in the district, 440 (40%) and 660 (60%) children were selected from the rural area and urban slums, respectively. Urban area of Lucknow has six Nagar Nigam zones, and the rural area is divided into eight community blocks. In the first stage, three wards (urban) and two community development blocks (rural) were randomly selected. In the next stage, two slums from each ward and two villages from each community blocks were randomly selected. Total six slums and four villages were selected. In each slum/village, 110 children under 5 years of age were selected. Only those households where children between 2 and 60 months were available were included in the study. In the selected slum/village, first household with an under-five child was selected randomly from the register of the Anganwadi worker and then house adjacent to it was selected. If the under-five child was not available in a household, house next to it was visited. Every child under-5 years of age present in the household was included in the study and their care givers were interviewed. Totally 568 (250 rural and 318 urban) caregivers were interviewed.
Data collections
Pretested, semi-structured, interviewer-administered questionnaire was used for data collection. Informed consent was taken before collection of the data. Information was collected on biosocial profile of parents, under-five children. Caregivers were asked whether the child had cough with fast breathing and/or chest indrawing in the last 2 weeks preceding the survey. Caregivers were also asked about home care practices, the source of the medication, the type of care sought for the illness and if delay in care seeking, the main reasons for delay. Home care practices included any care that was given to the child before being taken to the health facility irrespective of the source or time was asked. A narrative of chain of events that occurred during the course of illness was also recorded. Pneumonia was defined as, a child with cough or difficult breathing who has fast breathing and no general danger signs, no chest indrawing, and no stridor when calm.[14] Care-seeking behavior was defined as (i) recognition of illness in the child, (ii) seeking timely care, and (iii) seeking appropriate care. Qualified practitioner: A registered medical practitioner (Allopathic or AYUSH), least has minimum qualification of MBBS or equivalent.
Data analysis
Information collected on interview schedules was cross checked for completeness and correctness. Descriptive statistics mean and standard deviation for continuous variables and frequencies, proportions for categorical variables were used to arrive at the study results.
Results
Biosocial characteristics of study population
Majority of the children were living in joint family (62.9%), belonged to Hindu religion (79.8%), and from SC/ST community (40.1%). Eight percent of them were from lower socioeconomic class. The mean age of mothers was (26.7 ± 5.2). Majority of mothers were illiterate (60.2%) and housewives (93.0%) by occupation. One-third of the fathers were illiterate (38.0%) and unskilled worker (62.3%). Half of children (44.7%) were in 37–60 months age group, followed by 13–36 months age group (36.2%), and 19.1% were in 2–12 months age group. The mean birth order of children was about 2 and mean preceding birth interval was 20 months. Male children constituted about half (51.6%) of the study subjects. No statistically significant difference in biosocial characteristics of rural and urban slum caregivers was observed.
Prevalence of acute respiratory infection
Out of total 1065 children surveyed, 240 children reported cough/cold within 2 weeks preceding the survey. Among these, 52 children had cough with difficult and/or fast breathing. The prevalence of childhood pneumonia (integrated management of neonatal and childhood illness [IMNCI]) was 4.9%, within 2 weeks preceding the survey.
Recognition of illness and initial step taken by the caregivers
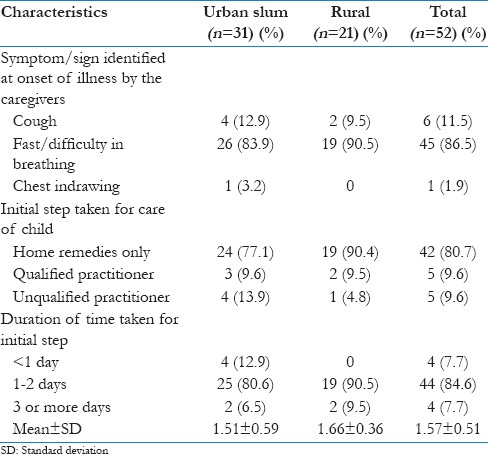
At the onset of illness, fast/difficulty breathing was identified by but rural (90.5%) caregivers and more than 80% urban slums [Table 1]. Majority (80.7%) of the caregivers, both in rural areas (90.4%) and in urban slums (77.7%) opted for the home remedies at the onset of illness. They tried home remedies for 1–2 days. Seven percent of the caregivers tried home remedies for 3 days or more. Very few caregivers in the rural areas (n = 2) and urban slums (n = 3) sought treatment from the qualified health practitioner. None of the caregivers had consulted Accredited Social Health Activists/Auxiliary Nurse Midwives (ASHAs/ANMs) for care of the children. No difference in recognition of signs of illness and initial step taken for care of children was observed between rural and urban slum caregivers.
Table 1.
Recognition of initial sign and symptoms of illness and steps taken by the caregivers for care of children
Home care practices during illness
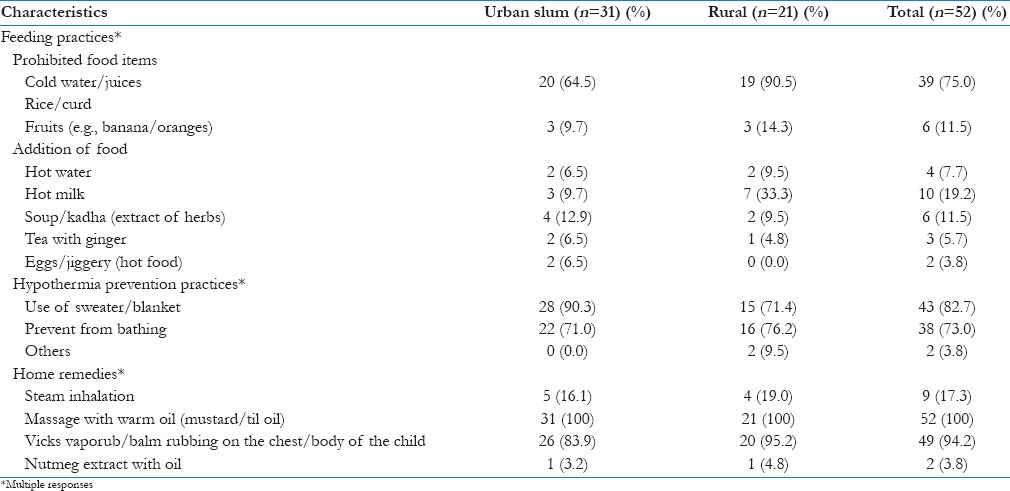
Home remedies have been adopted by all the caregivers for the child illness. The practice of massage with warm oil was universally followed by the application of vicks vaporub/balm on the chest, forehead, palms and soles of the child (94.2%), and steam inhalation (17.3%). Regarding feeding practices, most of the caregivers prohibited intake of cold water/beverages and “cold food” (75.0%) by the children during illnesses [Table 2]. Prohibition of “cold food” was more common practice in rural areas (90.5%) in comparison to urban slum caregivers (64.5). Hot milk (19.2%) was most commonly recommended food item during the illness, followed by soup/kadha (11.5%). More than 80% of the caregivers used sweater/blanket to prevent child from getting cold and 73.0% prevented their children from bathing to prevent hypothermia during illness.
Table 2.
Home care practices followed by caregivers for care of children as initial step
Caregivers' perception of severity of illness
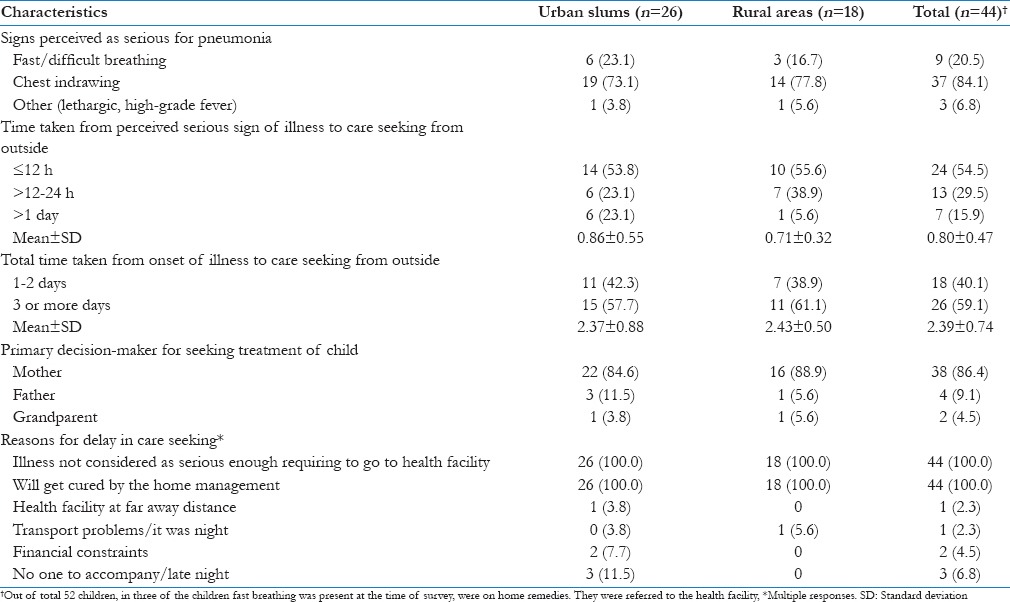
Majority of caregivers (73.1% urban vs. 77.8% rural) sought treatment from outside the on appearance of chest indrawing in the child [Table 3]. Half of the caregivers sought care from outside within 12 h on recognition of chest indrawing in the child. However, 23% caregivers in urban slums waited for more than 1 day. Mean duration of time taken from the appearance of chest to seek treatment was around 0.80 ± 0.47 h. Mean total time taken from the recognition of signs at onset of illness to care seeking from outside was around 2½ days (2.39 ± 0.74). Main reason for delay in seeking treatment cited by almost all the caregivers was, initially not considering that child's illness is serious enough to visit health facility, watching the effect of the home remedies, followed by financial constraints (4.5%). Mother (86.4%) was the main decision-maker for seeking care from outside the home for illness.
Table 3.
Caregiver's perception of severity of illness and reasons for delay in care seeking
Type of treatment provider/treatment
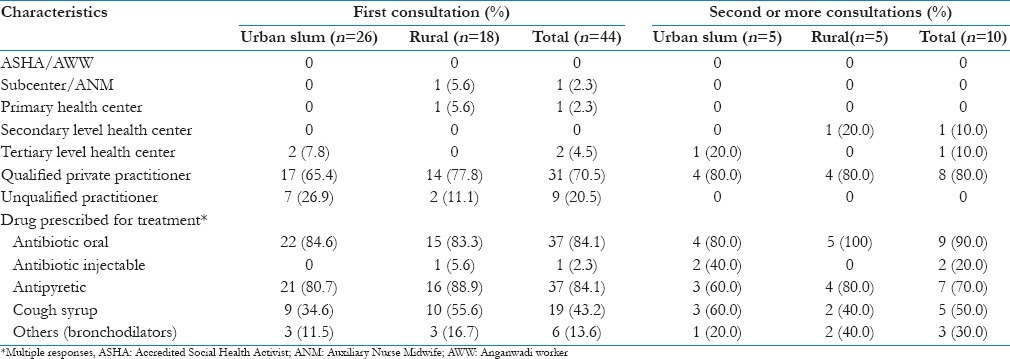
The qualified private practitioners [Table 4] were the preferred choice for first consultation in both rural areas (77.8%) and in urban slums (65.4%). Around one-fifth of the caregivers took first consultation from unqualified practitioners. Oral antibiotics were the most commonly prescribed drugs in both rural areas (88.8%) and urban slums (84.6%). Out of the total 44 caregivers, 10 caregivers (22.7%) also sought second consultation for their child illness. Among these, again the qualified private practitioners were preferred choice for consultation in both rural areas as well as in urban slums (80.0% each). ANM or ASHA was not consulted at any stage of illness in both rural and urban slums. ANM was consulted by one rural caregiver, only after appearance of chest indrawing.
Table 4.
Type of treatment provider and treatment given for childhood pneumonia after perception of serious illness
Discussion
One of the key strategies of IMNCI is the education of the mothers/caregivers on the signs of severe illness for which the child should be immediately taken to the health facility. Prompt recognition and treatment with an effective drug have a crucial role in childhood pneumonia, as the case fatality rate in untreated children is high (sometimes exceeding 20%) and death can occur after 3 days of illness.[15] The timings of the mother's decision to seek medical care depend on her and how family understands of the severity of the child condition.[16]
At the onset of the illness, most of the caregivers in the study had identified the fast/difficult breathing, an early sign of pneumonia in their child. However, even after recognition of this sign of pneumonia in the children, majority of the caregivers did not sought treatment from qualified practitioner. They first tried traditional remedies on their own at home. Only on appearance of the chest indrawing, a late sign of pneumonia, they decided to seek care from a health facility. This suggests that caregivers do not perceive fast/difficult breathing to be a severe enough sign to sought treatment from a health facility for the child. Main reason cited by almost all the caregivers for delay in seeking treatment also was, initially (on difficulty in breathing) they do not consider that child's illness is serious. From the narratives of the events by the caregivers also it was emerged out that for caregivers, “some difficulty in breathing” is a common occurrence in a child having complaint of cough and cold. More severe caregivers perceived child illness to be; the more they go for treatment from outside. In the present study, 11.3% of the urban slum and 6.8% rural caregivers perceived “fast breathing” as a danger sign of childhood pneumonia while about 70% caregivers identified chest indrawing as one of the danger sign. In different countries, researchers observed that caregivers brought their child to the hospital, only when the child developed late danger signs (pasli chalna/refusal to feed) with severe form of pneumonia, associated complications or on worsening of the condition of the child.[4,16,17,18] Awasthi et al. expressed that caregivers missed the identification of early stage of pneumonia when only fast breathing is present; they acknowledge fast breathing only when accompanied with chest indrawing.[19]
In the present study, majority (80.7%) of caregivers first tried home medication on their own at the onset of illness in the child. Similar to this community-based study in Lahore also found 71.2% of mother initiated the home-based treatment on their own to treat pneumonia in children.[20] Self-administration of medication was reported by a 24% of mothers by Memon et al.[21] Studies in Bangladesh, India, show that home remedies; massaging the child chest with different types of oils to expel mucus, herbal preparations, and avoidance of “cold foods” and preference of, “hot foods” are common in ARIs in children. Rashid et al. opined that even if none of the home practices was harmful but it may inadvertently lead to delay in care seeking from health facility.[16] Most of the carers' in the our study also waited for more than 2 days, trying home remedies, after recognition of illness, before seeking any health care from the outside. Mean time taken from the onset of illness to the seeking care from health facility was around 2½ days (2.39 ± 0.75) in the study. Researchers in different countries had reported delay in seeking of more than 2–4 by the caregivers. Mishra et al. reported mean delay of 3.4 ± 2.1 days from the onset of first symptoms to the time of seeking care from any health facility.[17] In Uganda, median time taken to seek care from outside the home was 2 days after onset of illness.[4] Possible explanation for delay in attending health facility was, may be mother waited to see the effects of self-prescribed treatment.[15] Another study from Nepal reported that the mean duration of illness before hospital presentation for males and females were 4.40 and 4.16 days, respectively.[22] In Memon et al. study majority of mothers sought health facility services after 2 days of self-medication while there was delay of up to 3 days in 33.9% of the mothers.[21] Awasthi et al. opined that caregivers' chose either to wait and watch or visit traditional healer or visit a registered medical practitioner for a child perceived as “less sick.”[19] This delay in seeking care could be detrimental for the health of the sick children.
One of the key interventions Global Action Plan for Pneumonia and Diarrhoea has proposed to fight with pneumonia is 90% treatment access for the children with pneumonia, including care by an appropriate health provider and antibiotics.[1] In the study, on recognition of fast/difficult breathing in child, 19.2% of caregivers sought care from outside. Of them, only 9.6% sought services of appropriate care provider. Only, when the caregivers perceived that child is “more sick,” on the appearance of chest indrawing, most of them sought care from outside. Even at this stage of illness, about 20% had first consulted an unqualified practitioner. Another study from Lucknow also reported caregivers of sick neonates sought care from unqualified provider for pneumonia.[19] For the first consultation of illness, the private qualified health practitioners (70.4%) were the preferred choice and only about 10% caregivers went to the government health facilities. Similar preference for type of provider was also observed in urban Karachi where mothers who sought appropriate care, 69.4% had taken their child to private health-care providers, and only 11.7% to public care providers.[23] Another study from the Philippines reported that three-fourth of caregivers brought their child to a private health facility when they had pneumonia.[24] One of the caregiver sought care from the ANM, and none of them consult ASHA at any stage of illness.
In the study, overall 84.9% of children, in rural areas (83.3%) and 88.8% in urban slums received antibiotics for the treatment of childhood pneumonia. A study from Lebanon found similar results; 83.4% of children with pneumonia had received antibiotics.[25] Another study from Nigeria reported that 53% children with cough alone and 60% children with cough and difficult/fast breathing received antibiotics.[4] In the households, drug prescription was not available with the caregivers and also the caregivers were not able to recall the name of prescribed drugs. However, in about thirty cases where the information was available, the most commonly prescribed drug was syrup amoxiclav, cefixime followed by cotrimoxazole.
Mother of the child was the primary care giver in all the surveyed households. In more than 80% rural and urban slum households, she was also the primary decision-maker for seeking care outside the home followed by fathers (9.6%). In another study in Uttar Pradesh and Bihar, mothers were not the primary decision-maker. Fathers during the focus group discussions, they recognized mother as the primary identifier of illness in children, who usually tries out home remedies and approached family members for seeking health care from outside when she perceived that home treatment is ineffective. Ferdous et al. also reported that mothers were unable to detect the severity of illness and brought the matter to the attention of adult family members/household heads to get the permission to take the child to health facility.[18]
Conclusions
Recognition of chest indrawing as a sign of pneumonia by caregivers was universal. They did not identify fast/difficult breathing as a serious sign of childhood pneumonia. Qualified practitioner was not an initial choice for seeking care and administration of home remedies was a common practice in the child with difficult breathing, in the both rural and urban slums communities. This resulted in delay in seeking treatment for the illness. Challenge is to increase the ability of caregivers to recognize when to seek care, to facilitate appropriate care behavior for pneumonia. Empowerment of community, especially of the mothers (primary caregivers) is necessary in recognition of early signs of childhood pneumonia for seeking timely appropriate care. There is need to develop locally adapted behavior change communication interventions for childhood pneumonia. Training of community health workers in prompt identification and first-hand appropriate management with the strengthening of public health facilities will be a key action in evidence-based management of childhood pneumonia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Dr. Rudra P. Das, Dr. Rahul Katiyar, Dr. S. Prasad, Dr. Prashant Bajpai.
References
- 1.Ending Preventable Child Deaths from Pneumonia and Diarrhoea by 2025: Global Action Plan for Prevention and Control of Pneumonia and Diarrhoea. World Health Organization/The United Nations Children's Fund (UNICEF) 2013. [Last cited on 2016 Feb 21]. Available from: http://www.who.int/maternal_child_adolescent/documents/global_action_plan_pneuonia_diarrhoea/en/
- 2.Wardlaw T, Johansson EW, Hodge M. Geneva: The United Nations Children's Fund (UNICEF)/World Health Organization (WHO); 2006. Pneumonia: The Forgotten Killer of Children. [Google Scholar]
- 3.World Health Organization. Pneumonia. Fact Sheet. 2015. [Last cited on 2016 Feb 21]. Available from: http://www.who.int/mediacentre/factsheets/fs331/en/
- 4.Ukwaja KN, Talabi AA, Aina OB. Pre-hospital care seeking behaviour for childhood acute respiratory infections in South-Western Nigeria. Int Health. 2012;4:289–94. doi: 10.1016/j.inhe.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 5.New York: UNICEF; 2007. [Last cited on 2016 Feb 21]. UNICEF. Child Survival and Health – Pneumonia Progress. Available from: http://www.childinfo.org/pneumonia_progress.html . [Google Scholar]
- 6.Zaman K, Zeitlyn S, Chakraborty J, de Francisco A, Yunus M. Acute lower respiratory infections in rural Bangladeshi children: Patterns of treatment and identification of barriers. Southeast Asian J Trop Med Public Health. 1997;28:99–106. [PubMed] [Google Scholar]
- 7.Nichter M, Nichter M. Acute respiratory illness: Popular health culture and mother's knowledge in the Philippines. Med Anthropol. 1994;15:353–75. doi: 10.1080/01459740.1994.9966099. [DOI] [PubMed] [Google Scholar]
- 8.Hildenwall H, Rutebemberwa E, Nsabagasani X, Pariyo G, Tomson G, Peterson S. Local illness concepts – Implications for management of childhood pneumonia in Eastern Uganda. Acta Trop. 2007;101:217–24. doi: 10.1016/j.actatropica.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 9.Mumbai: IIPS; 2008. International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005-2006: India. [Google Scholar]
- 10.Mathew JL, Patwari AK, Gupta P, Shah D, Gera T, Gogia S, et al. Acute respiratory infection and pneumonia in India: A systematic review of literature for advocacy and action: UNICEF-PHFI series on newborn and child health, India. Indian Pediatr. 2011;48:191–218. doi: 10.1007/s13312-011-0051-8. [DOI] [PubMed] [Google Scholar]
- 11.Annual Health Survey 2012-2013. [Last cited on 2016 Feb 21]. Available from: http://www.censusindia.gov.in/vital_statistics/AHSBulletins/AHS_Factsheets_2012_13.html .
- 12.Directorate of Census Operations, Uttar Pradesh. District Census Handbook, Lucknow. Census of India. 2011:11. [Google Scholar]
- 13.District Urban Development Agency (DUDA), Nagar Nigam Lucknow. [Last cited on 2016 Feb 20]. Available from: http://www.sudaup.org/hlink/18nov20141.pdf .
- 14.Geneva, Switzerland: World Health Organization; 2005. World Health Organization. Handbook of IMCI: Integrated Management of Childhood Illness; p. 22. [Google Scholar]
- 15.Källander K, Hildenwall H, Waiswa P, Galiwango E, Peterson S, Pariyo G. Delayed care seeking for fatal pneumonia in children aged under five years in Uganda: A case-series study. Bull World Health Organ. 2008;86:332–8. doi: 10.2471/BLT.07.049353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rashid SF, Hadi A, Afsana K, Begum SA. Acute respiratory infections in rural Bangladesh: Cultural understandings, practices and the role of mothers and community health volunteers. Trop Med Int Health. 2001;6:249–55. doi: 10.1046/j.1365-3156.2001.00702.x. [DOI] [PubMed] [Google Scholar]
- 17.Mishra S, Kumar H, Sharma D. How do mothers recognize and treat pneumonia at home? Indian Pediatr. 1994;31:15–8. [PubMed] [Google Scholar]
- 18.Ferdous F, Dil Farzana F, Ahmed S, Das SK, Malek MA, Das J, et al. Mothers' perception and healthcare seeking behavior of pneumonia children in rural bangladesh. ISRN Family Med. 2014;2014:690315. doi: 10.1155/2014/690315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Awasthi S, Srivastava NM, Pant S. Symptom-specific care-seeking behavior for sick neonates among urban poor in Lucknow, Northern India. J Perinatol. 2008;28(Suppl 2):S69–75. doi: 10.1038/jp.2008.169. [DOI] [PubMed] [Google Scholar]
- 20.Iqbal I, Malik AY, Anwar M, Khan SP. Community perceptions about acute respiratory infections (ari) in Multan, Pakistan. Nishtar Med J. 2010;2:2–9. [Google Scholar]
- 21.Memon KN, Shaikh K, Pandhiani BS, Usman G. How do mothers recognize and treat pneumonia in their children at home. A study in Union Council Jhudo, district Mirpurkhas? J Liaquat Univ Med Health Sci. 2013;12:208–13. [Google Scholar]
- 22.Pandey KR, Jha AK, Dhungana R, Lamsal R. Health seeking behaviour of parents for children with pneumonia. JNMA J Nepal Med Assoc. 2009;48:131–4. [PubMed] [Google Scholar]
- 23.Durrani HM, Kumar R, Durrani SM. Recognizing the danger signs and health seeking behaviour of mothers in childhood illness in Karachi, Pakistan. Univers J Public Health. 2015;3:49–54. [Google Scholar]
- 24.Kim SA, Capeding MR, Kilgore PE. Factors influencing healthcare utilization among children with pneumonia in Muntinlupa City, the Philippines. Southeast Asian J Trop Med Public Health. 2014;45:727–35. [PubMed] [Google Scholar]
- 25.Yousif T. Epidemiology of acute respiratory infections among children under five years old attending Tikrit General Teaching Hospital. Middle East J Fam Med. 2006;4:148–52. [Google Scholar]


