Abstract
Introduction:
Disease burden estimations based on sound epidemiological research provide the foundation for designing health services. Patients visiting a primary care often present with symptoms and signs. Understanding the burden is crucial for developing countries including India. The project aimed to record the reasons for encounter (RFE) at primary care settings for estimating the burden at the health-care facility.
Methodology:
This cross-sectional study was undertaken at four urban health dispensaries of Bhubaneswar, Odisha, with the aim to explore the prevailing patterns of diseases among patients attending these facilities. Data collection spanned from May to October 2012. At each center, patients' information on age, sex, religion, and presenting illness was extracted from the outpatient records over these time period. Data were entered and analyzed in SPSS version 20, and the International Classification of Primary Care-2 was used for coding the illnesses.
Results:
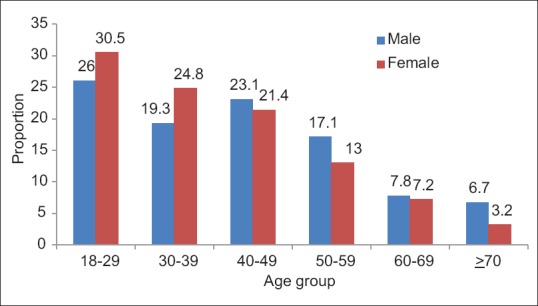
In total, 2249 patient's records were extracted over 12 weeks. Out of them, 1241 (55.2%) were male with mean age of 41.8 (±15.8) years vis-à -vis 38.2 (±14.1) years for females. Around 151 (6.7%) had 2 or more symptoms or conditions. Overall, the most common categories were general and unspecified followed by digestive-related symptoms in both sexes. The most common symptoms among males were fever (11.4%), heart burn (8.1%), and vertigo or dizziness (3.6%). Similar pattern was seen among females. Respiratory (17.0%) and cardiovascular (10.2%) problems were the most common RFEs among males and females. The most common RFEs for acute care among males and females were fever, allergic rhinitis, upper respiratory tract infection, and acute bronchitis. Leading RFEs for chronic care among males were hypertension uncomplicated, heart burn, low back pain, whereas among females, hypertension and heartburn were mostly seen.
Conclusion:
Primary care settings are experiencing both communicable and non-communicable diseases along with injuries. Understanding the distribution of the diseases are essential to design appropriate service package at primary care.
Keywords: International Classification of Primary Care, medical records, primary care
Introduction
Over the last century, successful disease prevention strategies coupled with more effective treatments for many diseases has culminated in a decline in mortality due to infectious diseases. This is accompanied by a shift in the population disease profiles, with chronic noncommunicable diseases slowly replacing infectious diseases as the major cause of mortality and morbidity,[1] particularly in low- and middle-income countries (LMICs), thus affects disproportionately who are still struggling with infectious diseases. Similar to other LMICs, India, the second most populous country in the world, is currently experiencing a rapid demographic transition resulting in increased life expectancy and attendant dual burden of diseases.[2] This undoubtedly would put a heavy strain on the present health-care system that has been traditionally oriented to cater to infectious diseases.[3,4] To design preventive, management, and treatment services to meet the needs of patients, it is first important to understand the morbidity profile of patients availing of public health-care services. The information derived can help the clinicians and health service planners to prioritize diseases and interventions to focus on and contribute toward the formulation of programs to circumvent the impact of morbidity and mortality due to those diseases.
In India, primary care physicians are the first point of contact and the main providers of healthcare for individuals.[5] Therefore, primary care practice constitutes an ideal setting to study the morbidity profile given its continuity of care and coordinating role. The best source of such data is the patient registers that they are easily available and require less resource.[6] The nature of morbidity presentations in primary care guides primary care providers ensuring their competencies to assess common undifferentiated symptoms. The comparison between the expected burden of disease and the actual presentations and diagnoses would indicate, whether primary care is effectively engaging with the burden of disease and the health system's readiness to address it. We undertook a chart review with a view to explore the patterns of diseases among adult patients attending primary care settings. The objectives were two-fold: to examine the reasons of encounter in primary care and second to estimate the prevalence of chronic conditions as well as to identify the most frequently encountered chronic conditions.
Methodology
Study design
A retrospective study of patient encounters in the outpatient department (OPD) of the urban health center (UHC) was done from 15th May to 30th October 2014.
Setting
Four UHCs (out of 17) were randomly selected for data collection. Each UHC provides clinical services to approximately 20,000 people of the urban population.[7] Each health center is supported by a tertiary care hospital for specialist services and referrals to the emergency room. The participating centers were managed by one medical officer, one staff nurse, and one pharmacist. Existing OPD registers were taken for collection of the data of the patients aged 18 years or more.
Data collection
At each UHC, a standard register was used to register the patients, maintained by either the staff nurse or the physician. Data for seven randomly selected weeks in a year were collected from the register. Those 7 weeks constituted of 2 weeks each from rainy season (16 weeks) and winter season (16 weeks) and three weeks from summer season (20 weeks). Patient's information was entered into Excel and later coded by trained research staffs using the International Classification of Primary Care-2 (ICPC-2) system which is widely utilized to classify primary care encounters.[8] ICPC-2 operates a biaxial coding structure: the first axis represents 17 body systems (e.g., alimentary, hematological), and the second represents 7 components, including: (i) complaints and symptoms; (ii) diagnostic, screening, and preventive; (iii) medication, treatment procedures; (iv) test results; (v) administrative; (vi) referrals and other reasons for encounter (RFEs); and (vii) diagnosis/disease. Each component has a list of standardized rubrics that are coded by two digit numeric code.[9] The letter from the corresponding chapter combined with the two digit numeric code gives the final classification. We collected data for: reason for encounter, investigations (if available), treatment, referrals, and the clinician's final diagnosis.
At each facility, the data were maintained through a register by the pharmacist, the nurse, or the physician. The information recorded were age, sex, religion, address, chief complaint, new or repeated case, and date. There was no mentioning of RFEs, disease history, and treatment given. Each patient was prescribed medicine with a slip of paper which he/she has to present at the pharmacy counter to get the free medicines from the facility. On the next visit, the patients often forget to bring the prescription slip.
The coding was done electronically using an open spreadsheet document and saved as softcopy. The data included were the age and sex of each patient and all RFEs and all diagnoses for each consultation from the available record. Attempt was made to record process outcomes such as investigations ordered, outpatient procedures done, medication prescribed, and specialist services requested and referrals made. Repeat cases were excluded from analysis.
Analysis
The combined data set was analyzed using the Statistical Packages for Social Sciences; version 20 (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY, USA: IBM Corp.). In total, 2449 of RFEs were recorded. Descriptive frequency statistics were calculated for age, gender, RFEs, and diagnosis. The RFEs were categorized according to the system involved using ICPC-2 guide. All recorded RFE and diagnoses were classified into either acute or chronic problems by the study team.
Ethical consideration
The study was approved by the Institutional Ethical Committee of the Indian Institute of Public Health, Bhubaneswar. Permission for data collection was obtained from the medical officer of participating dispensaries. Written consent was not required from the patients as the data were extracted from the existing OPD register and processed anonymously.
Results
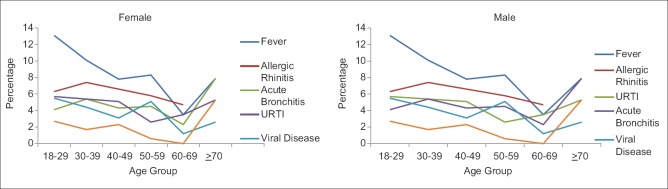
A total of 2449 adult patient encounters (new 2249, repeat 200) were documented over a 7-week period. Out of 2249 new patients, 1241 (55.2%) were male. The mean age of the sample was 40.0 years (standard error [SE]: 0.35) while the mean age of males and females was 41.8 years (SE: 0.45) and 38.2 years (SE: 0.41), respectively. It was found that nearly for 94% patients, one RFE was recorded while for 6% the RFEs was 2 or more. More than 50% of all patients were in the age group 18–39 years [Figure 1]. In this study, repeat consultations were excluded from analysis. Among all RFEs, 78% consultations were due to any disease, 16.6% were for any process outcome (dressing, checkup) and 3.4% had injury or trauma.
Figure 1.
Age and Sex distribution of study sample
Most common reasons for encounter
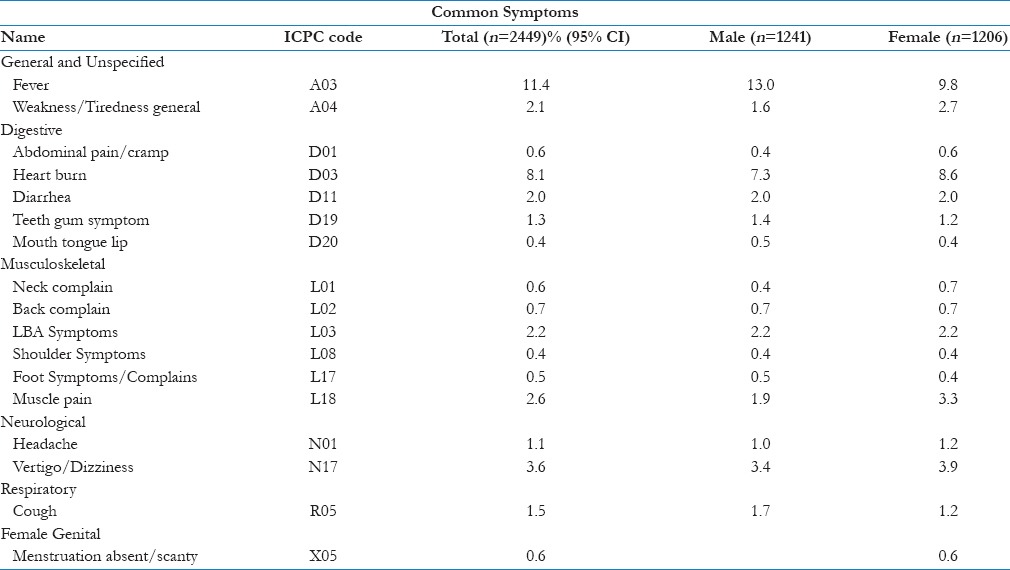
A total of 2603 RFEs were recorded for 2249 patients. The most common RFEs due to symptoms among males were fever (11.4%), heartburn (8.1%), and vertigo or dizziness (3.6%). A similar pattern was seen among females [Table 1].
Table 1.
Most common symptoms across sex
Most common diagnoses
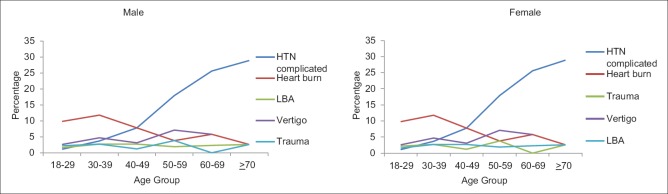
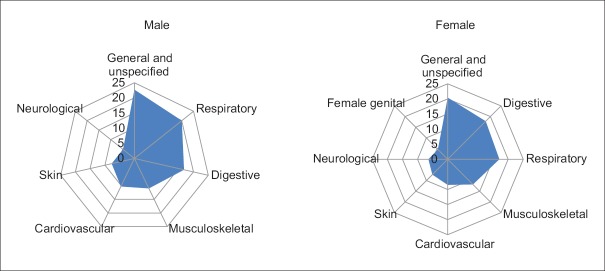
A total of 2023 symptoms and diagnoses were recorded. Respiratory (17%) and cardiovascular (10.2%) problems were the most common symptoms and diagnoses among males and females [Table 2]. The most common RFE for acute care among males and females were fever, allergic rhinitis, upper respiratory tract infection, and acute bronchitis. RFE for acute care were more among young adults 18–39 years, which gradually decreased with age [Figure 2]. Leading RFEs seeking chronic care among males were uncomplicated hypertension, heart burn, low backache among males, whereas among females hypertension and heartburn were mostly seen. Except hypertension and heartburn, the percentages of all other chronic conditions were similar across all age groups [Figure 3]. There was a steep rise in the occurrence of hypertension after the age of 40 years.
Table 2.
Most common diagnosis across sex
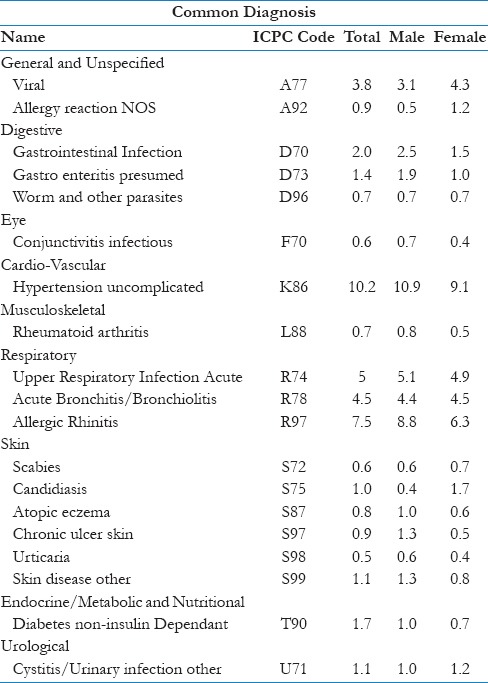
Figure 2.
Distribution of top reasons of encounter for acute care
Figure 3.
Distribution of top reasons of encounter for chronic care
Trauma and injury
Over 3.4% sample patients reported trauma and/or injury. Nearly 1.2% patients had sprain or strain and 0.7% had an injury of the musculoskeletal system. This was reported more frequently by males (4.6%) compared to females (2.2%).
Process outcome
Most common process codes recorded were dressing/press/compress/tamponade (code-54) (23%), incise/drain/flush/aspirate (2%) and medical checkup or evaluation (1%). Nearly 20% of the patients were referred to other physician/clinician/hospital/specialists. There was no record of reason for referral. Most common referred cases were found to be injuries and chronic diseases.
Discussion
In our study population, 151 (6.7%) patients had 2 or more symptoms or conditions. Overall, the most common categories were general and unspecified followed by digestive-related symptoms in both male and female. The most common symptoms among males were fever (11.4%), heartburn (8.1%), and vertigo or dizziness (3.6%). Among females, a similar pattern was seen. Respiratory (17%) and cardiovascular (10.2%) were the most common diagnosis among males and females.
The findings illustrate the occurrence of RFE among urban primary care practices and its burden. Age distribution demonstrates that more than 50% of the patients were less than 40 years of age, which reflects the trend in disease burden in the productive age group.[10] In our study, nearly 45% of attendees were women, the proportion is similar to that reported in Sri Lanka.[11] Equivalent figures are reported in developed countries such as Nigeria, Japan, and Australia.[12,13,14]
In our study, 94% of the patients had one RFE and 6% had 2 or more. The increased frequency of consultation represents the complexity of encounters. As there was no record of disease and treatment history, it becomes difficult for the physician to manage the cases. These centers are required to be well equipped for providing services to such patients.
We found that nearly 50% of total symptom/complaint RFE was contributed by seven symptoms. It represents patient's care seeking pattern and symptomatic morbidity which is considered to be an important part of the consultation. Coding of the symptoms using ICPC-2 helped us to quantify patients' illness reported and a variety of patient-reported complaints. Most of the management at the primary care is symptom-based, so this substantiates the concept of RFE (symptoms) as a core element of consultation with a primary care physician.
Among the top 20 diagnoses, RFE due to hypertension was the most common (10%) followed by allergic rhinitis and acute bronchitis. Other diagnoses ranged in frequency from 0.5% to 4.5% individually. A wide variety of diseases was diagnosed at the UHCs [Figure 4]. Contrary to the expectation, a huge number of patients are visiting primary care for medical checkup for chronic conditions such as measuring blood pressure. This necessitates having specific disease burden estimates at the primary care settings for providing tailor made services to the patients. As the primary care facilities are getting more cases of chronic diseases, a robust patient record database is need to be developed for estimating prevalence, complexity and severity of the disease and progress of the disease for designing a patient oriented treatment approach. ICPC-2 can be used as a guide for coding of the symptoms and diseases for preparing a standardized patient record database.
Figure 4.
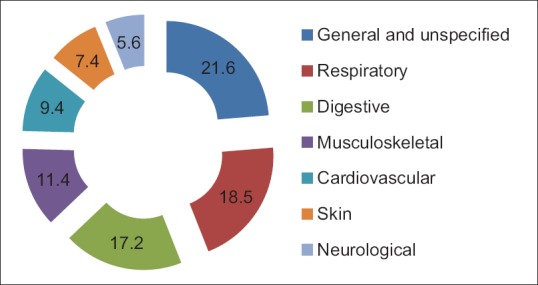
Top leading reasons for encounter system wise among all
For analysis purpose, we segregated the RFEs according to need of the attention and care such as acute or chronic care. In both the sexes common reason seeking immediate care were fever and allergic rhinitis. The pattern of RFE could be due to the seasonal effect or allergic conditions. As fever is the commonly reported symptom to many underlying diseases, further investigation is required to rule out the cause. All the patients at the urban center were referred to other settings for laboratory diagnosis, which consumes a lot of time and money. Primary care settings can be provided with facilities to carry out few basic tests to stop the delay in the diagnosis. The high prevalence of upper respiratory tract infection and acute bronchitis requires further epidemiological studies to find out the risk factors and causes. Among chronic care, most common diseases were hypertension and heart burn. The higher reporting of hypertension diagnosis could be due to the easy diagnostic facility at each center which requires minimum extraskill and human resource. Heart burn is most of the time caused due to acid peptic diseases. The reasons could be due to stress, lifestyle change, and dietary pattern. Further disease specific epidemiological investigation is required to identify specific risk factors. This figure indicates that the primary care still plays a great role in management of chronic diseases. Chronic diseases such as hypertension, diabetes, arthritis, acid peptic diseases, and chronic lung diseases affect the physical and mental health of an individual. Hence, community level of an integrated chronic care model is required to improve the quality of life of these patients, where primary care settings can play a great role.
In our study among 3.4% patients the RFE was trauma and or injury. The most common of them were sprain or strain. Nearly 20% of these patients were referred to other physician/clinician/hospital/specialists. As the settings are in urban area, it received most of the minor injury cases. The presence of trauma database at UHCs can enable us to find the pattern and burden of intentional and unintentional injuries or trauma occurred at household levels [Figure 5].
Figure 5.
Top leading reasons for encounter system wise among all patient
Comparison to literature
ICPC is found to be a comprehensive, simple, and practicable classification guide, which can be used in medical records and in different areas of primary care research. Having such standardized database helps retrieve and analyze the patient reported morbidities at primary care. The ICPC-2 is documented to be an adequate and feasible instrument for routine use in primary care settings of other countries.[14,15]
In our study, coding was done after the data collection. While assigning codes to the symptoms, we came across variety of terminology for similar symptoms were reported. No uniform guideline was followed for maintaining the registers. There is a need of incorporating the coding structure for maintenance of registers, which might help in estimating the burden of diseases with relative ease. In our study, we could not find coded for three symptoms/diseases such as filariasis, abscess, and lymphedema. Furthermore, we could not get any record on psychological problems and social issues. Similar findings were documented in other studies from India and Sri Lanka.[11,16]
In our studies, symptoms such as fever, vertigo/dizziness, heart burn, diarrhea, cough, and low back pain are well represented. Studies from other developing countries have also documented similar pattern in primary care settings.[12,15,17,18] Among chronic diseases, we found high burden of hypertension, heart burn, and low backache like reported in other studies.[11,19,20,21] However, conditions such as tuberculosis, HIV are less noted in our practice. One of the reasons could be due to the presence of dedicated vertical programs in the country for such diseases. Further, mental illnesses and substance abuse are less recognized though 6.5% of Indian population is reported to have a serious mental illness.[22,23] This is suggestive of the poor appreciation of these symptoms in the existing primary and secondary level services in the country. Furthermore, it may reflect the health-seeking behavior of the community for these symptoms that is well limited by the cultural influences.
System-wise analysis of burden of symptoms/diseases depicted that most of the RFEs were because of problems in general and unspecified, respiratory, digestive and musculoskeletal system, similar to other studies.[11,16,20,21,24] However, in developed countries, there appeared to have higher consultations for pregnancy, circulatory, neurological, endocrinological, and psychological problems.[15,17,18,25,26] Various reasons may account for these differences such as demographic profile of patients, health system and awareness, and educational level of the people in those countries.
Interpretation and management of symptoms plays crucial role in primary care. As symptoms are highly frequent in primary care, symptoms without a specific diagnosis constitute a challenge to the physicians, which have been given little priority in research. More attention should be directed to evidence-based management of symptoms to ensure improved outcomes in the future. This study has identified the common RFE, diagnosis, and outcome of urban primary care settings. Existing evidence supports the role of comprehensive coding of episodes of care in strengthening the primary care.[8] As we could not find use of any coding system by the primary care physicians for recoding the presenting illness, improved patient record keeping using ICPC for recording of RFE can be initiated. Comorbidities, social and psychological problems, and follow-up care must be incorporated in the existing registration system. Training on the use of ICPC codes and good record keeping system at primary care settings can help in strengthening the care services. Further studies should be carried out to find the risk factors of specific diseases confined to geographical areas. The study reflects the need for chronic care model at primary care settings as the prevalence of chronic diseases is similar to acute RFEs. Integration of different programs into a common database can help in proper estimation of disease burden and care progress in the community.
As most of the primary care physicians mention provisional diagnosis in the register but not sign and symptoms or the processes mentioned by the patients, this could be a major limitation of our study. The strength of our study is the urban health center based, allowing comparison with findings from other urban and rural areas of India. As we have not considered data of the whole year, seasonality variation could have been reflected in our study. As we have covered different facilities subjective variation in recording of the registers could not be ruled out.
Implications and recommendations
Strengthening of existing primary care services in India needs a baseline profile of primary care. Morbidity data from our health center are a fragment of such primary care data representing various presentations to primary care. Primary care physicians need skills training for effective, evidence-based approach to these presentations. Significantly, paucity of training in social and psychological aspects of care in existing medical education needs attention.
Conclusion
Primary care settings are experiencing both communicable and non-communicable diseases along with injuries. Understanding the distribution of the diseases are essential to design appropriate service package at primary care.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are thankful to Prof. Marjan Van den Akker, Department of Family Medicine, School Caphri, Maastricht University, Maastricht, The Netherlands and Prof. Job Metsemakers and Prof. J. Andre Knottnerus from Department of General Practice, KU Leuven, Leuven, Belgium, for their guidance and inputs. We would like to express their gratitude to Government of Odisha, all the doctors, and staff of the UHCs for their support and assistance in conducting this study.
References
- 1.NCD Alliance Report 2012-2013. Putting Non-Communicable Diseases on the Global Agenda. 2012. [Last accessed on 2013 May 30]. Available from: http://www.ncdalliance.org/Report2012 .
- 2.Global Status Report on Non-communicable Diseases. World Health Organization. 2010. [Last accessed on 2013 Feb 15]. Available from: http://www.who.int/nmh/publications/ncd_report2010/en/
- 3.Srivastava RK, Bachani D. Burden of NCDs, policies and programme for prevention and control of NCDs in India. Indian J Community Med. 2011;36(Suppl 1):S7–12. doi: 10.4103/0970-0218.94703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Engelgau MM, Karan A, Mahal A. The economic impact of non-communicable diseases on households in India. Global Health. 2012;8:9. doi: 10.1186/1744-8603-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okkes IM, Polderman GO, Fryer GE, Yamada T, Bujak M, Oskam SK, et al. The role of family practice in different health care systems: A comparison of reasons for encounter, diagnoses, and interventions in primary care populations in the Netherlands, Japan, Poland, and the United States. J Fam Pract. 2002;51:72–3. [PubMed] [Google Scholar]
- 6.EHR Standards for India: A Move towards Integrated Indian Healthcare System. [Last accessed on 2014 Mar 29]. Available from: http://www.healthfore.com/blog/2013/10/25/ehr-standards-for-india-a-move-towards-integrated-indian-healthcare-system .
- 7.NUHM – Government of India. [Last accessed on 2016 May 03]. Available from: http://www.nrhm.gov.in/nhm/nuhm.html .
- 8.Hofmans-Okkes IM, Lamberts H. The International Classification of Primary Care (ICPC): New applications in research and computer-based patient records in family practice. Fam Pract. 1996;13:294–302. doi: 10.1093/fampra/13.3.294. [DOI] [PubMed] [Google Scholar]
- 9.2nd ed. United Kingdom: WHO; 1998. [Last accessed on 2015 Mar 25]. WHO. International Classification of Primary Care, (ICPC-2) Available from: http://www.who.int/ classifications/icd/adaptations/icpc2/en/ [Google Scholar]
- 10.India: National Commission on Macroeconomics and Health; 2005. [Last accessed on 2016 May 03]. Ministry of Health and Family Welfare, Government of India. Burden of Diseases in India. Available from: http://www.who.int/macrohealth/action/NCMH_Burden%20of%20disease_(29%20Sep%202005).pdf . [Google Scholar]
- 11.de Silva N, Mendis K. One-day general practice morbidity survey in Sri Lanka. Fam Pract. 1998;15:323–31. doi: 10.1093/fampra/15.4.323. [DOI] [PubMed] [Google Scholar]
- 12.Takeshima T, Kumada M, Mise J, Ishikawa Y, Yoshizawa H, Nakamura T, et al. Reasons for encounter and diagnoses of new outpatients at a small community hospital in Japan: an observational study. Int J Gen Med. 2014;7:259–69. doi: 10.2147/IJGM.S62384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okkes IM, Veldhuis M, Lamberts H. Severity of episodes of care assessed by family physicians and patients: The DUSOI/WONCA as an extension of the International Classification of Primary Care (ICPC) Fam Pract. 2002;19:350–6. doi: 10.1093/fampra/19.4.350. [DOI] [PubMed] [Google Scholar]
- 14.Ayankogbe OO, Oyediran MA, Oke DA, Arigbabu SO, Osibogun AA. ICPC-2-defined pattern of illnesses in a practice-based research network in an urban region in West Africa. Afr J Prim Health Care Fam Med. 2009;1:3. [Google Scholar]
- 15.Brage S, Bentsen BG, Bjerkedal T, Nygård JF, Tellnes G. ICPC as a standard classification in Norway. Fam Pract. 1996;13:391–6. doi: 10.1093/fampra/13.4.391. [DOI] [PubMed] [Google Scholar]
- 16.Rahman SM, Angeline RP, Cynthia S, David K, Christopher P, Sankarapandian V, et al. International classification of primary care: An Indian experience. J Family Med Prim Care. 2014;3:362–7. doi: 10.4103/2249-4863.148111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soler JK, Okkes I, Oskam S, van Boven K, Zivotic P, Jevtic M, et al. An international comparative family medicine study of the Transition Project data from the Netherlands, Malta and Serbia. Is family medicine an international discipline? Comparing diagnostic odds ratios across populations. Fam Pract. 2012;29:299–314. doi: 10.1093/fampra/cmr099. [DOI] [PubMed] [Google Scholar]
- 18.Al-Shammari SA, Jarallah JS, Olubuyide IO, Bamgboye EA. A prospective study of the morbidity pattern of patients seen at a university primary care clinic. Ann Saudi Med. 1994;14:22–5. doi: 10.5144/0256-4947.1994.22. [DOI] [PubMed] [Google Scholar]
- 19.Islam MM, Valderas JM, Yen L, Dawda P, Jowsey T, McRae IS. Multimorbidity and comorbidity of chronic diseases among the senior Australians: Prevalence and patterns. PLoS One. 2014;9:e83783. doi: 10.1371/journal.pone.0083783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Teng CL, Aljunid SM, Cheah M, Leong KC, Kwa SK. Morbidity and process of care in urban Malaysian general practice: The impact of payment system. Med J Malaysia. 2003;58:365–74. [PubMed] [Google Scholar]
- 21.Adebusoye LA, Ladipo MM, Owoaje ET, Ogunbode AM. Morbidity pattern amongst elderly patients presenting at a primary care clinic in Nigeria. Afr J Prim Health Care Fam Med. 2011;3:211. [Google Scholar]
- 22.Panigrahi A, Panigrahi M, Padhy AP, Das SC. Common mental disorder and its socio-demographic correlates among married women residing in slum areas of Bhubaneswar, India. Women Health. 2016:1–13. doi: 10.1080/03630242.2016.1181137. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 23.Pothen M, Kuruvilla A, Philip K, Joseph A, Jacob KS. Common mental disorders among primary care attenders in Vellore, South India: Nature, prevalence and risk factors. Int J Soc Psychiatry. 2003;49:119–25. doi: 10.1177/0020764003049002005. [DOI] [PubMed] [Google Scholar]
- 24.Mash B, Fairall L, Adejayan O, Ikpefan O, Kumari J, Mathee S, et al. A morbidity survey of South African primary care. PLoS One. 2012;7:e32358. doi: 10.1371/journal.pone.0032358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prazeres F, Santiago L. Prevalence of multimorbidity in the adult population attending primary care in Portugal: A cross-sectional study. BMJ Open. 2015;5:e009287. doi: 10.1136/bmjopen-2015-009287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Caughey GE, Vitry AI, Gilbert AL, Roughead EE. Prevalence of comorbidity of chronic diseases in Australia. BMC Public Health. 2008;8:221. doi: 10.1186/1471-2458-8-221. [DOI] [PMC free article] [PubMed] [Google Scholar]