Abstract
Background:
Providing treatment to patients with diabetes mellitus in rural areas at a cost they can afford is a public health challenge.
Aims:
This study aims to measure the rate of compliance to oral hypoglycemic agents among patients with type 2 diabetes mellitus attending peripheral mobile clinics in rural South India. To study factors that impact glycemic control.
Setting and Design:
A cross-sectional study was done among patients attending peripheral mobile clinics in a rural block in Southern India.
Materials and Methods:
Pill counts were done to assess compliance. Participants' dietary intake was measured using a 24 h diet recall and their level of physical activity was measured using the WHO Global Physical Activity Questionnaire. Glycated hemoglobin (HbA1c) was measured for all participants.
Statistical Analyses Used:
Data were entered on EpiData and analyzed using SPSS. The prevalence of good glycemic control and good compliance was measured. A multiple linear regression was done to study factors affecting glycemic control.
Results:
Overall 52% of the participants were compliant to at least one drug and 50% had achieved good glycemic control. Compliance increased by 2.1% with every passing year since the diagnosis of diabetes. HbA1c reduced by 0.09% for every 10% increase in overall compliance.
Conclusions:
Levels of compliance and glycemic control achieved through this primary care team is comparable to those achieved through other systems.
Keywords: Compliance to oral hypoglycemic agents, glycemic control in rural India, primary care in diabetes mellitus
Introduction
Type 2 diabetes mellitus is a public health problem affecting an estimated 65 million Indians with an increasing trend in both urban and rural India.[1,2,3] The Diabetes Control and Complications Trial and UK Prospective Diabetes Study showed good compliance to treatment results in good glycemic control which in turn delays the onset of complications of diabetes.[4,5] However, studies done in India show that the prevalence of complications related to diabetes are high.[6,7] The compliance rates to oral hypoglycemic agents (OHAs) have been found to range from 60% to 75% among patients attending various tertiary care centers from different regions of the India[7,8,9] and compliance has been found to be affected by knowledge and educational status of the patients.[10,11]
In an effort to provide affordable and accessible care to the residents of a rural block in Vellore district a community health program has been successfully implemented by a nonprofit institution in which primary health care is delivered through doctor-run peripheral mobile clinics and secondary care through a base hospital located at the outskirts of the block. Multiple health-care packages are delivered through these peripheral mobile clinics including care for noncommunicable diseases. This study was conducted to assess the compliance and level of glycemic control achieved by diabetics residing in this rural block and utilizing the primary health-care program through these peripheral mobile clinics.
Materials and Methods
Study setting
Kaniyambadi block is a rural block with a population of 110,000 residing in 82 villages and is located in Vellore District of Tamil Nadu in Southern India. Integrated health care has been provided to this population for over three decades.[12] The health-care component of the program involves a team consisting of health aides, public health nurses and doctors that delivers primary health care and a base hospital, which is the referral unit. Each health aide works among a population of 5000; every public health nurse supervises 2–3 health aides and covers a population of 15,000. One doctor is assigned to a population of 40,000. The health aide's role is to provide health education, monitor health-related events and to refer patients to either the doctor run clinic or the base hospital as the situation demands. The public health nurse, apart from providing health education, also treats minor ailments through the nurse-run clinic that occurs once every fortnight. The doctor (post-MBBS) visits each village once a month, and through the doctor, run clinic provides primary care for those with chronic illnesses such as diabetes, hypertension, and many others.[12,13] Annually, more than 10,000 people avail health-care services from the mobile clinic, of which nearly 70% are women and 20% are those with diabetes alone or both diabetes and hypertension.
Through this team people with signs and symptoms of diabetes are referred to the secondary level base hospital. The base hospital is a 150 bedded hospital which has an out-patient department that caters to 90,000 patients annually, provides 24 h emergency services and also has laboratory and pharmacy services. Treatment is initiated at the base hospital if the person has a fasting blood sugar of more than 126 mg/dl or a postprandial sugar of more than 200 mg/dl. Together with the initiation of an OHA, patients are also educated about the need to engage in the regular physical activity and the need for a diet with low calorie and high fiber. Lifestyle modification is tailored to the patient's needs. Treatment is continued through the primary health-care services provided at the villages. All patients are referred once in 3 months for a repeat check of their blood sugars, annually for a check of creatinine and screening for diabetic retinopathy. Through various methods of education such as street plays and pamphlets people are taught about the signs, symptoms, diagnosis, and complications of diabetes, the need for life-long regular treatment, dietary restrictions, and regular physical activity. Patients who are lost to follow-up are identified and visited in their homes by the peripheral workers, counseled and encouraged to continue treatment.
This cross-sectional study was conducted in Kaniyambadi block between March and May in 2012, among people with diabetes attending the peripheral clinics after obtaining necessary permissions of the Institutional Review Board. Permanent residents of this block above the age of 30 years, diagnosed with type 2 diabetes and on OHAs for at least 1 year were included. Bedridden patients and those receiving insulin were not included in the study.
Data from previous studies done in tertiary centers show that compliance to treatment may be close to 50%.[14] Using this estimated prevalence and a precision of 10% a sample size of 100 was estimated. Hundred eligible diabetics were identified from 22 randomly selected villages using the existing health information system of the program.
Data collection
A semi-structured interviewer administered questionnaire was administered to consenting individuals. The first part of the questionnaire was designed to collect data pertaining to the individuals' sociodemographic details. Knowledge about their prescription was scored on 10 based on their ability to identify their drugs in hand and correctly mention the dose and frequency as advised by the doctor, verified using existing prescriptions. Socioeconomic status of each participant was measured using the Modified Kuppusamy Scale for 2012.[15] A 24 h dietary recall using standard sized vessels was used to assess each participant's dietary intake. The food items listed in the dietary recall were converted into kilocalories using the guidelines published by the National Institute of Nutrition, Hyderabad. The WHO Global Physical Activity Questionnaire was administered to measure the level of physical activity the person was engaged in on a daily basis.[16] Compliance to OHAs was measured by doing a pill count in their homes. The actual number of pills taken as a proportion of the number of pills expected to have been taken was calculated. Participants who had taken more than 80% of their prescribed pills were classified as compliant to treatment. In this study, overall compliance was defined as the best compliance to any one drug. Venous blood was collected from the participants using standard techniques and glycated hemoglobin (HbA1c) was measured using the high-performance liquid chromatography method with the Bio-Rad Variant 2 to assess the level of glycemic control achieved by the participant. For the purpose of the study, those with HbA1C levels <7% were considered to have good glycemic control as per the ICMR guidelines published in 2005.[17]
Data entry and analysis
Data were entered on EpiData v3.1 (EpiData Association 2000-2017, Denmark, Europe) and analyzed using SPSS Statistics for Windows, Version 17.0. Chicago, IL, USA: SPSS Inc.[18] The compliance to individual OHAs, the overall compliance, prevalence of good glycemic control, prevalence of sedentary lifestyle, and average dietary intake was calculated. Associations between individual risk factors and compliance were studied. A multiple linear regression analysis was done to assess the impact of each of these variables, after adjusting for confounders, on glycemic control.
Results
A total of 100 participants were selected from 22 villages. The mean age of the participants was 60.3 years (standard deviation [SD] 10.2), and 73% of them were women. Forty-four belonged to the middle class, and 56 belonged to the lower class as defined by the Modified Kuppusamy Scale. Twenty-one were unemployed, 24 were homemakers, and 19 were manual laborers. Twelve were skilled laborers, 16 were petty shop owners, and 8 had either salaried jobs or were receiving a pension.
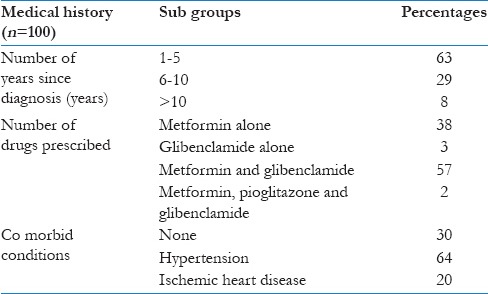
Medical history
The mean duration since the diagnosis of diabetes was 5.4 years (SD 4.1 years, median 4 years) with an interquartile range of 2–7 years. Table 1 shows the medical history of the participants. Comorbid conditions were present in 70% of the participants. More than 2 comorbid conditions were present in 20% of the participants with hypertension being the most common. The OHAs prescribed through the peripheral clinics are metformin, glibenclamide, and pioglitazone. The pill load varied from 2 to 16 pills per day and the average number of pills prescribed was 8 per day (SD 3.2). Since the medications are provided at a subsidized rate by the program, the average patient incurred cost per month was 34/-INR (SD 33.2 INR), and 15% of the participants were receiving free care.
Table 1.
Medical history of the participants
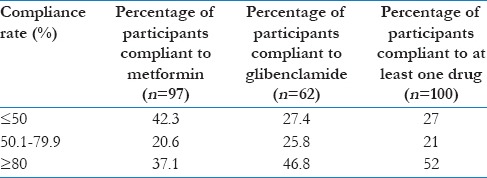
Compliance to oral hypoglycemic agents
Compliance to each drug was calculated separately as given in Table 2. More participants were compliant with glibenclamide. For the purpose of analysis, overall compliance was taken to be the highest compliance to any one of the OHAs. Fifty-two percent of the participants had a compliance rate of more than 80% with at least one drug. Seventeen participants had missed the last clinic and were therefore off medication at the time of the home visit.
Table 2.
Compliance rates to oral hypoglycemic agents
Lifestyle
The mean dietary calorie intake was found to be 1614 kcal/day (SD 601 kcal). Thirty-two percent of them were consuming 1500–1800 kcal/day, 43% were consuming <1500 kcal/day, and 8% were consuming <1000 kcal/day. Thirty-nine were leading a mostly sedentary type of lifestyle, and the others were involved with the moderate physical activity.
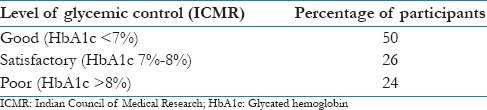
Level of glycemic control
The level of glycemic control achieved by each person was assessed by measuring their HbA1c. It was categorized using the ICMR guidelines and is presented in Table 3. The mean HbA1c was 7.3% (SD 1.4%).
Table 3.
Level of glycemic control achieved
Knowledge of prescription
Participants were awarded one point each for correctly identifying their drugs, stating the required dose and frequency. Their knowledge was then rated on a scale of 1–10. Seventy-two percent scored more than 8, 24 had a score of 5–8 and only 4 scored <5.
Factors affecting compliance
The mean overall compliance among men and women was 71.7% (SD 41.7%) and 70.5% (SD 63.4%), respectively. An independent t-test showed that this difference was not significant (P = 0.651). The mean overall compliance among participants aged <60 years of age was 69% (SD 39.4%) and among those aged more than 60 was 72% (SD 35.6%). The independent t-test showed that this difference was not statistically significant (P = 0.651). Association between age, duration of diabetes, knowledge of prescription and pill load, and the outcome of compliance to OHAs was done using a multiple linear regression. It was found that each passing year since diagnosis of diabetes resulted in a statistically significant 2.1% increase in the level of compliance.
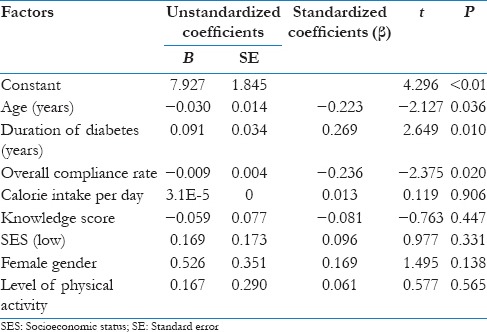
Impact on glycemic control
Fifty percent of the participants had good glycemic control as defined by the ICMR criteria. Association between selected exposure variables and the main outcome variable namely glycemic control as measured by HbA1c was carried out using multiple linear regression. Exposure variables chosen were an age in years, female gender, level of knowledge regarding the drugs prescribed, socioeconomic status, physical activity, calorie intake, overall compliance to OHA's and number of years since diagnosis of diabetes. For every 10% increase in compliance there is almost a 0.1% decrease in HbA1c and for every year increase in age, the HbA1c decreases by 0.03%. For every year that passes since the diagnosis of diabetes, there is an increase in HbA1c by 0.09%. Results of the multiple linear regression are given in Table 4.
Table 4.
Results of the multiple linear regression for factors affecting glycemic control
Discussion
This study was done among residents of the rural area who are receiving care for diabetes through doctor-run peripheral mobile clinics. Patients using insulin are referred to the base hospital and were therefore not included in the study.
The average age of the participants was 60.4 (SD 10.2) with a majority of women participants. This was the case as the majority of the users of these clinics are women as corroborated by the Department's Annual Report of 2015, which showed that 68.4% of the users of the mobile clinic were women. This may be because mobile clinics are conducted during the day when many men are away in their workplaces.
In this study, compliance was defined as consuming more than 80% of the prescribed pills. Overall, 52% of the participants were compliant with at least one OHA. Comparing these results with other studies is difficult as different methods have been used to measure compliance. For example, self-reported compliance was used in studies done in coastal south India and rural Maharashtra where compliance was found to be 83.9% and 76.2%, respectively.[10,19] Compliance, as elicited by the Morisky Medication Adherence Scale, was used in a Tertiary Care Centre in Kerala where the compliance was found to be 64.8%.[11]
Studies show that compliance drops after the first 6 months of diagnosis of any chronic condition. Not much literature is available on what happens thereafter. This study shows that with every passing year since the time of diagnosis compliance increases by 2.1%. Cross-sectional studies inevitably select people who have not dropped out of treatment and who have survived longer. The impact of time since diagnosis of diabetes on compliance may have resulted from this selection bias that occurs in cross-sectional studies. However, it reinforces the point that those who have engaged with this system for a longer period have better levels of compliance.
Among the participants of this study, 50% had achieved the required target of HbA1c, and an additional 26% had satisfactory glycemic control as defined by ICMR. Multiple other studies in different settings have shown that <50% of the people on treatment achieve the recommended target. The average HbA1c of participants of this study was 7.3% which is better than the mean HbA1c of the urban population which was found to be 8.9%.[7] However, this may be explained by the fact that the urban group was a more heterogeneous group including patients on treatment with insulin. The ICMR-INDIAB study among individuals with self-reported diabetes showed that there was no difference in glycemic control between urban and rural participants and overall only 31% had good glycemic control (HbA1c <7%).[20] Results from other public health programs and primary health-care teams in outcomes of management of noncommunicable diseases were not available for comparison.
This study shows also that 10% increase in compliance was associated with a significant decrease of 0.09% in HbA1C levels which is very similar to another study testing this association.[21]
These results are important to physicians who provide care in primary care settings because consecutive surveys, among residents over the age of 30, in the rural area have shown a three-fold rise in the prevalence of diabetes over the last two decades.[2] The latest survey done in this rural block showed that the prevalence of diabetes was 11.4% among men and 9.6% among women.[2] The high burden among those of the lower socioeconomic status puts the onus on the public health delivery system to ensure adequate care of noncommunicable diseases.[22] However, in 2015 a survey of primary heath care centers and community health centers in central India, in 2015, revealed that most centers were ill-equipped to manage noncommunicable diseases.[23] The National Health Mission has the vision of ensuring universal access to equitable, affordable and quality health-care services. Through the National Rural Health Mission, launched by the Government of India in 2005 Mobile Medical Units were deployed to ensure that a range of health-care services was available for people in remote and inaccessible areas and those from vulnerable populations.[24] The medical mobile units are designed to provide preventive, promotive, and curative services in the periphery. Peripheral mobile services have been provided to residents of Kaniyambadi block for many years, and this study shows that it is possible to achieve 52% compliance rates and at least satisfactory glycemic control among 76% of the population. This study also highlights the importance of assessing compliance to pharmaceutical interventions along with regular services. By ensuring good compliance to at least one drug, good glycemic control can be achieved even in a low-resource setting such as a mobile medical unit.
Conclusions
Overall 52% of the rural adult diabetic population attending the peripheral clinics was compliant to at least one OHA with half of the diabetics having good glycemic control. Neither sedentary lifestyle nor high caloric intake was found to be associated with poor glycemic control. An increase in the duration of diabetes resulted in an increase of compliance and increasing compliance was significantly associated with better glycemic control. Doctor-run peripheral clinics coupled with a mechanism to ensure regularity of patient visit may be a useful strategy to ensure good glycemic control and prevent complications among patients with diabetes in rural areas.
Financial support and sponsorship
This study was funded through the Fluid research grant provided by the Christian Medical College, Vellore.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
I would like to thank all the field workers and the faculty of the Department of Community Health of Christian Medical College Vellore, for all their help and guidance. Mrs. Vanitha, from the Department of Clinical Biochemistry in Christian Medical College Vellore, for processing the blood samples. Mrs. Shanti, a software programmer in the Department of Community Health for assistance with analysis of the findings of the WHO Global Physical Activity Questionnaire.
References
- 1.Shrivastava SR, Ghorpade AG. High prevalence of type 2 diabetes melitus and its risk factors among the rural population of Pondicherry, South India. J Res Health Sci. 2014;14:258–63. [PubMed] [Google Scholar]
- 2.Oommen AM, Abraham VJ, George K, Jose VJ. Rising trend of cardiovascular risk factors between 1991-1994 and 2010-2012: A repeat cross sectional survey in urban and rural Vellore. Indian Heart J. 2016;68:263–9. doi: 10.1016/j.ihj.2015.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yesudian CA, Grepstad M, Visintin E, Ferrario A. The economic burden of diabetes in India: A review of the literature. Global Health. 2014;10:80. doi: 10.1186/s12992-014-0080-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nathan DM DCCT/EDIC Research Group. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: Overview. Diabetes Care. 2014;37:9–16. doi: 10.2337/dc13-2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UK Prospective Diabetes Study: Overview. [Last accessed on 2016 Jun 23]. Available from: https://www.dtu.ox.ac.uk/ukpds/
- 6.MohanV, Shah S, Saboo B. Current Glycemic Status and Diabetes Related Complications among Type 2 Diabetes Patients in India: Data from the A1 Chieve Study. [Last accessed on 2016 Jun 20]. Available from: http://www.japi.org/january_special_issue_2013_a1chieve/04_oa_current_glycemic_status_and.pdf . [PubMed]
- 7.Mohan V, Shah SN, Joshi SR, Seshiah V, Sahay BK, Banerjee S, et al. Current status of management, control, complications and psychosocial aspects of patients with diabetes in India: Results from the DiabCare India 2011 Study. Indian J Endocrinol Metab. 2014;18:370–8. doi: 10.4103/2230-8210.129715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma K, Santra S, Bhattacharya A, Agrawal D, Kumar S, Mishra S. Study of utilization pattern and patient compliance of oral anti-hyperglycemic drugs in a tertiary care teaching hospital in Eastern India. J Obes Metab Res. 2015;2:221. [Google Scholar]
- 9.Allam MS, Aqil M, Qadry SA, Kapur P, Pillai KK. Utilization Pattern of Oral Hypoglycemic Agents for Diabetes Mellitus Type 2 Patients Attending Out-Patient Department at a University Hospital in New Delhi. [Last accessed on 2016 Jun 20]. Available from: http://www.file.scirp.org/pdf/PP_2014061314132274.pdf .
- 10.Chavan GM, Waghachavare VB, Gore AD, Chavan VM, Dhobale RV, Dhumale GB. Knowledge about diabetes and relationship between compliance to the management among the diabetic patients from Rural Area of Sangli District, Maharashtra, India. J Family Med Prim Care. 2015;4:439–43. doi: 10.4103/2249-4863.161349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaimol T, Biju CR, Anilasree BP, Jayakrishnan SS, Babu G. Medication Adherence to Oral Hypoglycemic Agents in Type 2 Diabetic Patients. [Last accessed on 2016 Jun 20]. Available from: http://www.rroij.com/open-access/medication-adherence-to-oral-hypoglycemic-agents-in-type-2-diabetic-patients.pdf .
- 12.Mohan VR, Muliyil J. Mortality patterns and the effect of socioeconomic factors on mortality in rural Tamil Nadu, South India: A community-based cohort study. Trans R Soc Trop Med Hyg. 2009;103:801–6. doi: 10.1016/j.trstmh.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Francis MR, Rakesh PS, Mohan VR, Balraj V, George K. Examining spatial patterns in the distribution of low birth weight babies in Southern India – The role of maternal, socio-economic and environmental factors. Int J Biol Med Res. 2012;3:1255–9. [Google Scholar]
- 14.Bosworth HB, Granger BB, Mendys P, Brindis R, Burkholder R, Czajkowski SM, et al. Medication adherence: A call for action. Am Heart J. 2011;162:412–24. doi: 10.1016/j.ahj.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oberoi SS. Updating income ranges for Kuppuswamy's socio-economic status scale for the year 2014. Indian J Public Health. 2015;59:156–7. doi: 10.4103/0019-557X.157540. [DOI] [PubMed] [Google Scholar]
- 16.Cleland CL, Hunter RF, Kee F, Cupples ME, Sallis JF, Tully MA. Validity of the global physical activity questionnaire (GPAQ) in assessing levels and change in moderate-vigorous physical activity and sedentary behaviour. BMC Public Health. 2014;14:1255. doi: 10.1186/1471-2458-14-1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Indian Council for Medical Research. Guidelines for the Management of Type 2 Diabetes. ICMR. 2005 [Google Scholar]
- 18.EpiData Software. [Last accessed on 2016 Jun 24]. Available from: http://www.epidata.dk/
- 19.Rao CR, Kamath VG, Shetty A, Kamath A. Treatment compliance among patients with hypertension and type 2 diabetes mellitus in a coastal population of Southern India. Int J Prev Med. 2014;5:992–8. [PMC free article] [PubMed] [Google Scholar]
- 20.Unnikrishnan R, Anjana RM, Deepa M, Pradeepa R, Joshi SR, Bhansali A, et al. Glycemic control among individuals with self-reported diabetes in India – The ICMR-INDIAB study. Diabetes Technol Ther. 2014;16:596–603. doi: 10.1089/dia.2014.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.García-Pérez LE, Alvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. 2013;4:175–94. doi: 10.1007/s13300-013-0034-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Checkley W, Ghannem H, Irazola V, Kimaiyo S, Levitt NS, Miranda JJ, et al. Management of NCD in low- and middle-income countries. Glob Heart. 2014;9:431–43. doi: 10.1016/j.gheart.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pakhare A, Kumar S, Goyal S, Joshi R. Assessment of primary care facilities for cardiovascular disease preparedness in Madhya Pradesh, India. BMC Health Serv Res. 2015;15:408. doi: 10.1186/s12913-015-1075-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Operational Guidelines for Mobile Medical Units, National Health Mission. [Last accessed on 2016 Jun 23]. Available from: http://www.nrhm.gov.in/images/pdf/programmes/mmu/Mobile_Medical_Units.pdf .


