Abstract
Context:
Depressive disorders often start at a young age. There is a need for early identification of depression, anxiety, and stress (DAS) and prevention. The present study was undertaken to find the magnitude of DAS among adolescents.
Aims:
To find the mental health status of school going adolescents in Chandigarh. The objectives were (i) to study the prevalence of DAS among school going adolescents and (ii) to study the correlates of DAS.
Settings and Design:
A Cross-sectional survey of students of four classes from 9th to 12th studying in government schools.
Subjects and Methods:
Ten government schools in Chandigarh were randomly selected through lottery method. In each school, for each of the four classes, a section was randomly selected again by the lottery method. Forty students were selected from each school reaching sample size of 470. DAS scale 21 questionnaires were used.
Statistical Analysis Used:
The data entry was done in MS Office Excel 2007. The analysis was done in the form of frequency tables, charts cross tables. For statistical significance, Chi-square test and correlation was found between various factors.
Results:
The prevalence of DAS was 65.53%, 80.85%, and 47.02%, respectively. Overall, comorbidity between depression and anxiety was 57.65%. Extremely severe depression was very less (3%). The prevalence of DAS was higher in females. For depression and anxiety, the peak age was 18 years.
Conclusions:
The prevalence of DAS was high among school going adolescents in Chandigarh. There is a need for early and effective identification of DAS that can prevent many psychiatric disorders at their nascent stage.
Keywords: Adolescent, Chandigarh, depression, anxiety, stress, India
Introduction
Adolescence is the period of transition. Depressive disorders often start at a young age; they reduce people's functioning and often are recurring. Globally, the reported prevalence rates of mental disorders among children and adolescent range from 1% to 51%. According to the WHO reports, community-based studies revealed an overall prevalence rate for mental disorders around 20% in several national and cultural contexts.[1] Major depression was the fourth most prevalent human disease in 1990 and is expected to rank second by the year 2020 in adolescent age group (Lopez and Murray, 1998).[2] In the USA and Australia, one in five teenagers suffers from mental health problems. In developing countries, the prevalence of mental disorders among adolescents attending primary health-care facilities ranges between 12% and 29%.[3] Several studies indicate that the prevalence rates of the individual disorders: Depression, anxiety, and stress (DAS) are growing among adolescents (Institute for Health Metrics and Evaluation, 2013).[4]
India contributes 21% of adolescent's population in the world. One out of six children affected with mental disorder. Early Indian community-based studies reported the prevalence rate of psychiatric disorders among children ranging from 2.6% to 35.6%.[5] It has been noted that the majority of suicides in India are by those below the age of 30 years.[6] Depressive disorders often start at a young age; they reduce people's functioning and often are recurring.[7,8] Hence, there is need for early and effective identification of DAS that can prevent many psychiatric disorders at their nascent stage. With this thought in mind, the present study was undertaken to find the magnitude of DAS among adolescents and various factors associated with it. The aim of this study was to find the status of the mental health of school going adolescents (13–18 years of age) in Chandigarh. The objectives were (i) to study the prevalence of DAS among school going adolescents (13–18 years of age) and (ii) to find the correlates of DAS among them.
Subjects and Methods
Study design
The cross-sectional survey was conducted in government schools of Chandigarh, India, for 4 months (January 1, 2014–April 30, 2014). The students (aged 13–18 years) of classes 9th, 10th, 11th, and 12th studying in selected schools were included in the study.
Selection of participants
In total, there were 186 recognized schools in Chandigarh, with 107 government schools and 79 private schools. For the representation of true population of these government schools in Chandigarh, ten government schools were randomly selected through lottery method. In each school out of four classes (9–12th), each section was randomly selected again by the lottery method. Further, ten students were selected from each section by systematic random sampling [Figure 1]. Sample size for the study was 470 students. Based on the varied prevalence of psychiatric morbidity from approximately 1–40%,[5,6] the maximum prevalence was taken to be 40% to calculate the sample size and relative error 5%. To check DAS, prepiloted questionnaire DAS scale (DASS) 21 was used. The DASS 21 is a 21 item self-report questionnaire designed to measure the severity of a range of symptoms common to both depression and anxiety. In completing the DASS, the individual is required to indicate the presence of a symptom over the previous week. Each item is scored from 0 to 3. Accordingly, the DASS allows not only a way to measure the severity of a patient's symptoms but also a means by which a patient's response to treatment can also be measured. In addition, a self-structured questionnaire on socioeconomic status was also prepared. Before administering the questionnaire to the students, they were briefed about the study. They were assured about the privacy and confidentiality of their personal information and opinions. The questionnaire was pilot tested on the similar age group students of one school, which was not the part of the study. This was done to validate the questionnaire. Principals, concerned teachers, and students were informed before the visit.
Figure 1.
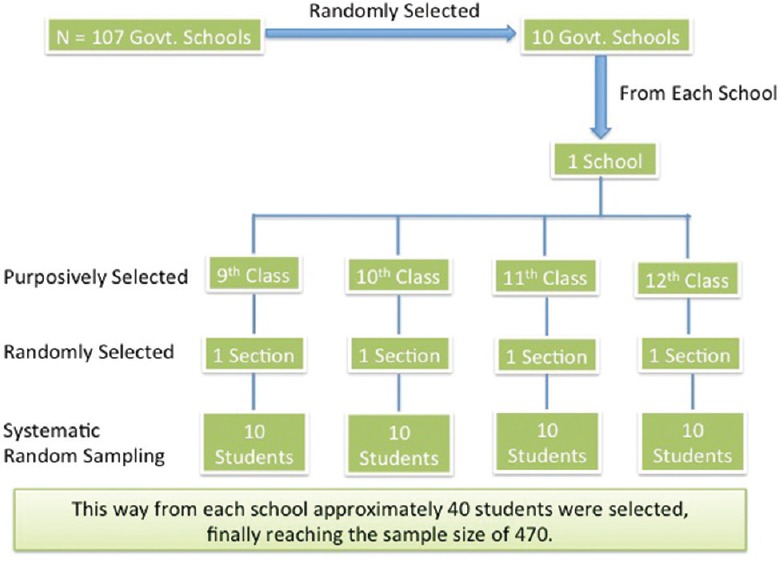
Sampling technique used to select study sample
Inclusion criteria
All government schools present in Chandigarh
Students studying in classes 9th, 10th, 11th, and 12th of both the genders (males and females).
Exclusion criteria
Those students who did not give consent or refuse to participate in the study.
Statistical analysis
The data entry was done in MS Office Excel 2007. The analysis was done in the form of frequency tables, charts cross tabs. For statistical significance, Chi-square test and correlation were found between various factors.
Ethical consideration
The permission from the office of Director Public Instructions, Chandigarh, for undertaking the study in selected schools was obtained. Written permission was also taken from the office of District Education Officer, Chandigarh, for conducting a study in randomly selected ten government schools. Permission was also obtained from the principals of selected schools after explaining them the aim and objectives of the study. In case of minor participants, consent was taken from their parents and the students. Consent was taken from the students, and their confidentiality has been maintained.
Results
Out of 470 students, the maximum number of students participating in study was from 9th class (28.72%), and minimum number of students was from 12th class (22.76%). There were 257 male (54.68%) and 213 female (45.31%) participants in the study. The maximum number of students were from the age group of 16 years, i.e., 180 (38.29%) and minimum from the age group of 19 years, i.e., 3 (0.63%) students. Table 1 shows gender-wise distribution of participants having DAS. Table 2 shows that overall comorbidity between all three disorders, i.e., DAS was 36.1%. Distribution of participants of 9th, 10th, 11th, and 12th class having the DAS is shown in Table 3. On comparison of DAS among participants of 9th, 10th, 11th, 12th classes, it can be seen that depression was higher in 12th class, anxiety was higher in 10th class, and stress was higher in 9th class. While comparing DAS among participant of nonboard (9th + 11th) and board classes (10th + 12th), it was found that it was higher in board classes than in nonboard classes. It was found that all types of depression (75.59%) and stress (53.52%) were higher in board classes than of nonboard classes (57.2% and 41.63%, respectively).
Table 1.
Gender-wise distribution of participants having depression, anxiety, and stress (n=470)
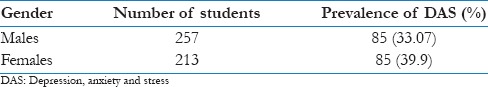
Table 2.
Comorbidity between different disorders (n=470)
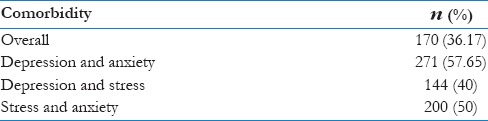
Table 3.
Distribution of participants of 9th, 10th, 11th and 12th class having the depression, anxiety, and stress (n=470)
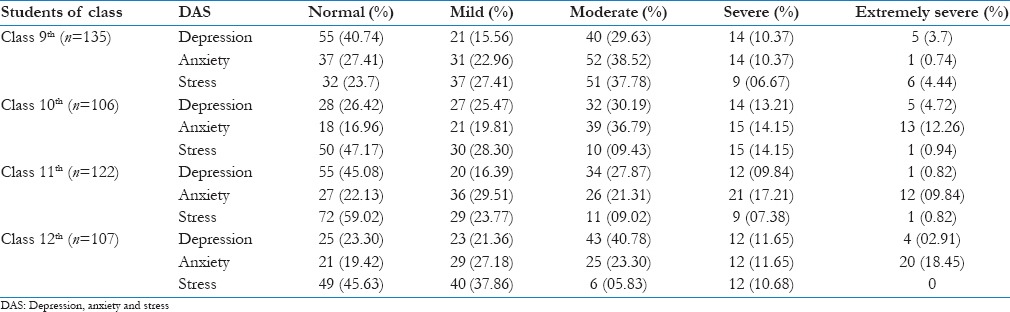
Among students of classes 11th and 12th, according to their stream, it was found that depression and anxiety were maximum in medical students (78.57%), and stress was more in commerce students (48.89%). It was found that extremely severe depression was highest among medical students (03.57%); mild depression was also more in them (28.57%). Moderate depression was more in arts students (43.42%). Extremely severe (17.10%) and moderate anxiety (27.63%) were higher in arts students. Mild anxiety was higher in medical students (42.86%). Severe anxiety was higher in commerce students (16.67%). Extremely severe stress was present only in commerce students (01.11%); severe stress was higher in nonmedical students (60.71%). Mild stress was higher in arts students (35.53%).
Distribution of participants having DAS according to the age showed that half of the student of 13 years of age felt stressed and three-fourth are depressed and anxious. In 14-year-old students 78% of students had anxiety. In 15-year-old students, nearly two-third had depression and more than three-fourth had anxiety. A similar situation was seen in 16-year-old students. In 17-year-old students, three-fourth had anxiety. In 18-year-old students, all students had anxiety, and 91% were depressed. The overall trend shows that the level of stress increased with age. In case of depression and anxiety, the peak age was 18 years.
Self-satisfaction with academic performances in participants with DAS was 67.08%, 86.07%, and 40.5%, respectively whereas the parent's satisfaction with academic performances of their wards with DAS was 66.86%, 80.47%, and 43.19%, respectively. Poor socioeconomic conditions and father's occupation (nonworking) were directly related with higher level of DAS. With increase in the education level of parents, level of DAS in their children decreased. As the parents love decreased, level of depression and stress in the participants increased. DAS was found to be more among students whose mothers were not alive. The level of anxiety was found higher in the participants belonging to the joint families. Students staying away from home in hostels and paying guest accommodations had higher levels of depression and stress. It was found that the prevalence of depression and stress was more in students who were bullied by batch mates. It was also found that the prevalence of DAS was more in students who felt overburdened with test schedules. The level of stress was higher among the participants who were not self-satisfied with their academic performance and whose parents were not satisfied. Participants, who took alcohol and smoked, showed higher prevalence of DAS.
Discussion
In our study, we found that the prevalence of DAS was more in students who feel overburdened with test schedules. The level of stress was higher among the participants who were not self-satisfied with their academic performance and whose parents not satisfied. Similar results have been reported by other studies, namely, Kaur and Sharma, Moreira and Furegato, Liu and Lu and Gray-Stanley et al.[9,10,11,12] A study done by Deb et al. revealed that 63.5% of the higher secondary students in Kolkata experience academic stress, and the parental pressure for better academic performance was found to be mostly responsible for academic stress as reported by 66.0% of the students.[13] It was found that the prevalence of DAS was higher in females than in males. The study by Kaur and Sharma in Chandigarh also found that girls were more academically frustrated than the boys.[9] The study conducted in Bengaluru by Sharma and Kirmani found that girls had higher scores on beck depression inventory than boys.[14] A comprehensive review of almost all general population studies conducted to date in the United States of America, Puerto Rico, Canada, France, Iceland, Taiwan, Korea, Germany, and Hong Kong reported that young women predominated over men in lifetime prevalence rates of major depression.[15] In India, similar findings were obtained by Verma et al.[16]
Academic stress is a type of stress that arises due to academic factors such as heavy school schedule, unrealistic expectation and demands of parents and teachers, low academic performance, poor study habits, and not having enough time to deal with school's multiple priorities.[17] Academic stress is recognized as a risk factor for depression and suicidal behavior.[18,19] The experience of school-related stress such as poor academic performance, negative feedback from parents and teachers about school work; daily hassles in the school environment, stressful life events, and negative affect states during school work were all leads to increase in depression.[11,12] Poor academic grades generally predict high educational stress; the discrepancy between expected and actual grades may play a more important role in the development of psychological distress and other mental health problems.[20]
In our study, DAS increases as the intake of alcohol increases. Higher DAS was found among those who drink alcohol and those who were occasional smokers. Severe depression and extremely severe stress were more in males as compared to females. A study done in Chennai in 1986 revealed that 23.25% had contemplated suicide earlier and that 91.9% of them were aged 30 years or less. A strong association of suicidal tendency with alcohol was reported in 10.42% of the sample.[20] The suicide rate was more in males as compared to females. It might be due to the reason that males are not emotionally very strong as compared to females and shared less of their problems as compared to female.
The prevalence of DAS increases as the parents love decreases, lack of parental affection takes toil on mental peace of children. In a review done by Zgambo, et al. in 2012, it was seen that children and adolescents who live without parents exhibit higher levels of depressive symptoms than those who live with parents around them.[21] Depression is decreased by higher levels of parental care and lower levels of parental indifference.[22,23] Greenberger et al. stipulate that strong positive family relationships lessen the symptoms of depression.[24] Many other factors, such as loss of loved ones, conflicts with parents, teachers, and peers, and significant physical diseases may have important effects on adolescent suicidality.[25] In our study, as the level of parent's education increases, the level of prevalence DAS among adolescents decreases. There is a direct relation between the parents' mental health and their children's health. A cross-sectional study by Olfson et al. in 2003, on parental depression and child mental health reported that children of parents with depression were approximately twice as likely as children of parents without depression to have a variety of mental health problem.[26] The prevalence of depression and stress was more among the participants who were bullied by their batch mates or seniors. According to the study conducted by Khawaja et al. in 2015 in Pakistan showed that physical abuse (P = 0.05), verbal abuse (P = 0.003), injury (P = 0.02), and bullying (P < 0.001) were significantly associated with psychological stress.[27]
As the age increases, the prevalence of DAS was also found to be increasing. The peak of the prevalence of depression was in the 18th year of age. Tepper et al. argue that depressive symptoms do not differ between boys and girls but intensify with age.[28] This trend of increasing DAS may be due to different social and developmental challenges faced by teens.
In our study, depression and stress were prevalent in participants who belong to poor families. Direct and indirect effects of relative poverty had bad effect on the development of emotional, behavior, and psychiatric problems. Poverty has multidimensional phenomenon, encompassing inability to satisfy basic needs, lack of control over resources, lack of education and poor health.
Since DAS was very high, hence, provision should be made for a natural mentoring program for the children as well as adolescents. Psychological health should be the prime concern of school authorities, and it should be integrated with school health programs. Child-centered activities including individual mental health consultation and specific problem-focused interventions as well as more general classroom programs to improve coping skills, social support, and self-esteem. For relieving stress, yogic exercises, meditation, laughter therapy, and other recreational activities suitable for that group of students should be made part of school curriculum. Although school health program is running in various schools mental, psychological, and emotional dimensions are not given adequate attention, it is recommended that school health program should be strengthened by including above-mentioned aspects. Child psychologists should be recruited on permanent basis in government schools. There should be counseling sessions for students and their parents. Students must be made aware about ill effects of substance abuse through lectures so that do not indulge in such things. Since DAS level was found more among the girls than the boys, the need of hour is that more attention should be paid to girl child under school health program.
The limitations of the study are that, as the data were self-reported, under or over reporting of data may have taken place due to the stigma related to mental disorders. Data were not collected from private school, as it was not permitted.
Conclusions
According to study, the overall prevalence of DAS among school going adolescents in Chandigarh was high. DAS in this population have been shown to be associated with increase risk of suicidal behavior, homicidal ideation, tobacco use, and other substance use. The burden of mental disorder is great as they are prevalent in all societies. They create a substantial burden for affected individuals and their families and produce significant economic and social hardships that affect society as a whole.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors wish to acknowledge their gratitude to all the school authorities for giving permission for data collection and also, to the students who participated in the study and shared their valuable opinions about the issues deserve special appreciation.
References
- 1.Alvi T, Assad F, Ramzan M, Khan FA. Depression, anxiety and their associated factors among medical students. J Coll Physicians Surg Pak. 2010;20:122–6. [PubMed] [Google Scholar]
- 2.Lopez AD, Murray CC. The global burden of disease, 1990-2020. Nat Med. 1998;4:1241–3. doi: 10.1038/3218. [DOI] [PubMed] [Google Scholar]
- 3.Rask K, Astedt-Kurki P, Laippala P. Adolescent subjective well-being and realized values. J Adv Nurs. 2002;38:254–63. doi: 10.1046/j.1365-2648.2002.02175.x. [DOI] [PubMed] [Google Scholar]
- 4.The Global Burden of Disease: Generating Evidence, Guiding Policy. European Union and Free Trade Association Regional Edition. [Last cited on 2015 Oct 31]. Available from: http://www.healthdata.org/policy-report/global-burden-disease-generating-evidenceguiding-policy-european-union-and-free .
- 5.WHO; [Last cited on 2015 Oct 31]. WHO | The World Health Report 2001 – Mental Health: New Understanding, New Hope. Available from: http://www.who.int/whr/2001/en/ [Google Scholar]
- 6.Depression. [Last cited on 2015 Oct 31]. Available from: http://www.nimh.nih.gov/health/publications/depression/index.shtml .
- 7.Williams CA. Empathy and burnout in male and female helping professionals. Res Nurs Health. 1989;12:169–78. doi: 10.1002/nur.4770120307. [DOI] [PubMed] [Google Scholar]
- 8.Farby JJ. Depression. In: Woody RH, editor. Encyclopaedia of Clinical Assessment. San Francisco: Jossey-Bas; 1980. [Google Scholar]
- 9.Kaur S, Sharma V. Depression among adolescents in relation to their academic stress. Indian J Appl Res. 2014;4:183–5. [Google Scholar]
- 10.Moreira DP, Furegato AR. Stress and depression among students of the last semester in two nursing courses. Rev Lat Am Enfermagem. 2013;21:155–62. doi: 10.1590/s0104-11692013000700020. [DOI] [PubMed] [Google Scholar]
- 11.Liu Y, Lu Z. Chinese high school students' academic stress and depressive symptoms: Gender and school climate as moderators. Stress Health. 2012;28:340–6. doi: 10.1002/smi.2418. [DOI] [PubMed] [Google Scholar]
- 12.Gray-Stanley JA, Muramatsu N, Heller T, Hughes S, Johnson TP, Ramirez-Valles J. Work stress and depression among direct support professionals: The role of work support and locus of control. J Intellect Disabil Res. 2010;54:749–61. doi: 10.1111/j.1365-2788.2010.01303.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deb S, Strodl E, Sun J. Academic stress, parental pressure, anxiety and mental health among Indian high school students. Int J Psychol Behav Sci. 2015;5:26–34. [Google Scholar]
- 14.Sharma P, Kirmani MN. Exploring depression & anxiety among college going students. Indian J Sci Res. 2015;4:528–32. [Google Scholar]
- 15.Gomez Homen, Francesca, WHO Nations for Mental Health Initiative, World Health Organization, Division of Mental Health and Prevention of Substance Abuse, Piccinelli M. Gender Differences in the Epidemiology of Affective Disorders and Schizophrenia. 1997. [Last cited on 2015 Oct 31]. Available from: http://www.who.int/iris/handle/10665/63505 .
- 16.Verma N, Jain M, Roy P. Assessment of magnitude and grades of depression among adolescents in Raipur city, India. Int Res J Med Sci. 2014;2:10–3. [Google Scholar]
- 17.Banerjee S. Chandigarh, India: Punjab University; 2011. Effect of Various Counseling Strategies on Academic Stress of Secondary Level Students [Ph.D.] [Google Scholar]
- 18.Ang RP, Huan VS. Relationship between academic stress and suicidal ideation: Testing for depression as a mediator using multiple regression. Child Psychiatry Hum Dev. 2006;37:133–43. doi: 10.1007/s10578-006-0023-8. [DOI] [PubMed] [Google Scholar]
- 19.Bjorkman SM. Illinois, U.S.A: Northern Illinois University, DeKalb; 2007. Relationships Among Academic Stress, Social Support, and Internalizing and Externalizing Behavior in Adolescence [Ph.D.] [Google Scholar]
- 20.Lin HC, Tang TC, Yen JY, Ko CH, Huang CF, Liu SC, et al. Depression and its association with self-esteem, family, peer and school factors in a population of 9586 adolescents in Southern Taiwan. Psychiatry Clin Neurosci. 2008;62:412–20. doi: 10.1111/j.1440-1819.2008.01820.x. [DOI] [PubMed] [Google Scholar]
- 21.Zgambo M, Kalembo F, Guoping H, Honghong W. Depression among chinese children and adolescents: A review of the literature. Int J Child Youth Family Stud. 2012;3:442–57. [Google Scholar]
- 22.Zhang Y, Li H, Zou S. Association between cognitive distortion, type D personality, family environment, and depression in Chinese adolescents. Depress Res Treat. 2011;2011:143045. doi: 10.1155/2011/143045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu YL. Parent-child interaction and children's depression: The relationships between parent-child interaction and children's depressive symptoms in Taiwan. J Adolesc. 2003;26:447–57. doi: 10.1016/s0140-1971(03)00029-0. [DOI] [PubMed] [Google Scholar]
- 24.Greenberger E, Chen C, Tally SR, Qi D. Family, peer, and individual correlates of depressive symptomatology among U.S. and Chinese adolescents. J Consult Clin Psychol. 2000;68:209–19. doi: 10.1037//0022-006x.68.2.209. [DOI] [PubMed] [Google Scholar]
- 25.Liu X, Tein JY, Sandler IN, Zhao Z. Psychopathology associated with suicide attempts among rural adolescents of China. Suicide Life Threat Behav. 2005;35:265–76. doi: 10.1521/suli.2005.35.3.265. [DOI] [PubMed] [Google Scholar]
- 26.Olfson M, Marcus SC, Druss B, Alan Pincus H, Weissman MM. Parental depression, child mental health problems, and health care utilization. Med Care. 2003;41:716–21. doi: 10.1097/01.MLR.0000064642.41278.48. [DOI] [PubMed] [Google Scholar]
- 27.Khawaja S, Khoja AA, Motwani K. Abuse among school going adolescents in three major cities of Pakistan: Is it associated with school performances and mood disorders? J Pak Med Assoc. 2015;65:142–7. [PubMed] [Google Scholar]
- 28.Tepper P, Liu X, Guo C, Zhai J, Liu T, Li C. Depressive symptoms in Chinese children and adolescents: Parent, teacher, and self reports. J Affect Disord. 2008;111:291–8. doi: 10.1016/j.jad.2008.03.013. [DOI] [PubMed] [Google Scholar]


