Abstract
Objectives
Specialty drugs can bring significant benefits to patients, but their prices are very high. Medicare Part D plans charge relatively high cost-sharing for specialty drugs. A provision in the Affordable Care Act (ACA) reduced cost-sharing in the Part D coverage gap phase to mitigate financial burdens of beneficiaries with high drug spending. We examined the early impacts of the Part D in-gap discount on specialty cancer drug use and patients' out-of-pocket spending.
Study Design
Natural experimental design. We compared changes in outcomes before and after the in-gap discount among beneficiaries with and without low-income subsidies. Beneficiaries with low-income subsidies, who were not affected by the in-gap discount, were used as the control group.
Method
A random sample of elderly stand-alone Prescription Drug Plan enrollees with uncommon cancers (leukemia, skin, pancreas, kidney, sarcoma, and non-Hodgkin lymphoma) between 2009 and 2013. We constructed four outcome variables annually: use of any specialty cancer drug, the number of specialty cancer drug fills, total speciatly cancer drug spending and out-of-pocket spending on specialty cancer drugs.
Results
The in-gap discount did not influence specialty cancer drug use but reduced annual out-of-pocket spending on specialty cancer drugs among users without low-income subsidies by $1,114.
Conclusions
Closing the donut hole in Part D decreased patients' financial burdens to some extent but resulted in no change in specialty drug use. As demand for specialty drugs increases, it will be important to ensure patients' access to needed drugs and reduce their financial burdens.
Keywords: Prescription Drug Benefits, Specialty Drugs, Out-of-pocket Spending, Medicare Part D
1. Introduction
Spending on prescription drugs has increased rapidly. In 2014, it grew by 14%, while spending on other medical care increased only by 4.1%-4.6%.1,2 A driver of the growth of prescription drug spending is specialty drugs, whose spending increase has been high for the decade (14%-20% annually between 2006 and 2013 and 30% in 2014).1 Specialty drugs do not have a single definition but often have at least one of the following characteristics: high prices, biologics, treating complex conditions, and requiring special handling and delivery, although not all drugs with any of these features are specialty drugs.3,4 Specialty drugs made up only 1% of prescriptions in 2014; however, they accounted for 30% of total drug spending due to their high prices.1 Facing this cost pressure, payers place higher cost-sharing requirements for specialty drugs than traditional drugs, creating concerns about patients' access to needed specialty drugs and financial burdens of specialty drug users.3,5,6
Consumer cost-sharing is commonly used to manage prescription drug use and spending. Literature indicated that patients were less likely to use traditional prescription drugs when cost-sharing was higher.7 A recent review showed that commercial enrollees' responsiveness to cost-sharing for specialty drugs was relatively small.8 Evidence on the price responsiveness in elderly Medicare beneficiaries is sparse although conditions for which specialty drugs are used are age-related. Part D plans use high cost-sharing for specialty drugs to manage utilization among beneficiaries without low-income subsidies.9 However, high cost-sharing would be counter-productive if specialty drug use is not responsive to price due to potential benefits of specialty drugs or the absence of viable substitutes3,8; it would simply put patients at financial risk. Yet few studies examined the relationship between cost-sharing and specialty drug use among elderly beneficiaries without low-income subsidies.
Studying responses to specialty drug benefits is challenging because Part D plan choice is voluntary, which can lead to biased estimates if specialty drug users enroll in plans with low cost-sharing. We used a natural experimental design, leveraging on an exogenous change in the Part D benefit. The exogenous change, which enables us to avoid selection in plan choice, is filling in the Part D coverage gap introduced by the 2010 Affordable Care Act (ACA). This provision led to a change in benefit generosity that particularly affects specialty drugs because it focuses on a large decrease in cost-sharing for brand-name drugs (and thus specialty drugs).
The presence of a coverage gap in the standard Part D benefit, where beneficiaries were responsible for the full drug spending prior to 2011, had been criticized to have posed financial burdens to enrollees.10,11 In response, a provision in the ACA stipulated that the gap be gradually filled in until it is closed in 2020. It reduced the in-gap coinsurance rate to 50% for brand-name drugs in 2011 and 2012. In-gap cost-sharing for brand-name drugs is gradually decreasing to 47.5% in 2013-2014, 45% in 2015–2016, and a 5% point decline per year thereafter. Coinsurance for generic drugs decreases by 7% points every year. In 2020, beneficiaries will be responsible for 25% of branded or generic drug spending until they reach catastrophic coverage.
This Part D in-gap benefit change is designed to mitigate financial burdens of beneficiaries who reach the coverage gap due to their high drug spending. Among these are specialty drug users without low-income subsidies (LIS). Part D defines specialty drugs as drugs whose monthly price is greater than $600, and allows plans to place those drugs in a separate “specialty” tier in the pre-gap phase. The cost-sharing of a specialty tier in the pre-gap phase is usually 33% coinsurance, which is higher than the standard one (25%). Further, most specialty drugs users pass through the initial coverage and hit the gap with their first fill(s) due to high prices of specialty drugs. The ACA discount is thus likely to lift financial stress of specialty drug users without low-income subsidies. Beneficiaries with LIS do not face financial burdens related to specialty drugs because their drug spending is mostly paid by Medicare. A study showed that LIS enrollees were more likely to initiate specialty cancer drugs than non-LIS patients due to their lack of financial barriers to specialty drug use.12
The 50% in-gap discount for branded drugs can be a sizable reduction in out-of-pocket spending to specialty drug users without subsidies. It implies a decrease of $1,860 in OOP spending for a beneficiary who has the Part D standard benefit (in 2015) and passes through the gap during a given year. Recent data showed that the average OOP spending on specialty drugs decreased from $2,376 to $1,758 (-26%) between 2010 and 2011 among Part D enrollees.13 However, cancer patients may face larger OOP spending due to high prices of specialty cancer drugs: two analyses of Part D plan formulary files suggested that OOP spending of specialty cancer drug users could reach up to $12,000 even with the in-gap discount.6,14
Our study examined how the in-gap discount affected OOP spending on specialty cancer drugs among the elderly during the first three years of its implementation. We focused on specialty cancer drugs, which comprise one-third of total specialty drug spending.15 We also examined how the in-gap discount affected specialty cancer drug use. The reduced in-gap cost-sharing can lead beneficiaries to continue to take medications even when hitting the gap. Beneficiaries may also begin taking specialty drugs if they make consumption decisions based on total OOP spending. However, the ACA provision lowers cost-sharing only in the coverage gap and does not change cost-sharing for the first fill(s). If patients cannot afford cost-sharing in initial coverage, they would not use a specialty drug and the in-gap discount would be irrelevant. We examined this possibility by analyzing whether the in-gap discount changed the probability of using specialty cancer drugs and the number of specialty cancer drug fills among users.
2. Methods
Sample and Data
The study population is randomly selected elderly Medicare beneficiaries with cancer between 2009 and 2013. We focused on six uncommon cancers (leukemia, kidney, pancreatic, skin, sarcoma, and non-Hodgkin lymphoma) for which specialty drugs are used but are understudied. Medicare claims were searched to select a random sample of Fee-for-Service beneficiaries with those cancers based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes – at least one inpatient or skilled nursing facility claim or two outpatient or carrier claims in a given year. We included beneficiaries who had Part A and Part B coverage and stayed in the same stand-alone Prescription Drug Plan (PDP) for the entire year. We excluded beneficiaries in Medicare Advantage Prescription Drug Plans (MA-PDs) because their claims are not available.
The primary data are Part D Prescription Data Event (PDE) Files, which contain records on prescription drug fills, including National Drug Code, days supplied, and spending (beneficiary/plan payment, and subsidy amounts when applicable). All drug spending variables were adjusted to 2013 dollars based on the Consumer Price Index for prescription drugs.
We augmented PDE files with Medicare Master Beneficiary Summary Files, which provided beneficiary information (residence, demographic characteristics, and chronic condition indicators), and Part D Plan Files to get plan benefit attributes. We obtained ZIP-level income/education and county-level healthcare resource information from the 2010 American Community Survey and Area Health Resource Files, respectively. This study was approved by our university's Institutional Review Board.
Identifying Specialty Cancer Drugs
We identified Part D specialty drugs as products placed in a specialty tier at least by one plan based on Plan Formulary Files.13,16 To identify cancer drugs (anti-neoplastic agents including chemotherapy, immunotherapy, and hormone therapy), we used two sources: 1) organizations supporting cancer patients or cancer research (e.g., National Cancer Institute and American Cancer Society); and 2) the Wolters Kluwer Health Medi-Span MED-file v.2,17 which groups drugs by therapeutic class. By cross-walking the lists of Part D specialty drugs and antineoplastic agents, we identified all Part D specialty cancer drugs, which are used in the analysis. Table 1 shows the top 10 frequently used specialty cancer drugs by the study population.
Table 1. Average monthly spending of top 10 specialty cancer drugs frequently used by Part D enrollees with leukemia, kidney, pancreatic, skin, sarcoma or non-Hodgkin lymphoma cancer.
| Generic name | Description | Average monthly spending ($)a | |
|---|---|---|---|
|
| |||
| 2010 | 2013 | ||
| Imatinib mesylate | Treats certain types of leukemia, bone marrow disorders, and skin cancer, and certain tumors of the stomach and digestive system. | 4,438 | 6,418 |
| Lenalidomide | Promotes immune responses to help slow tumor growth; Treats multiple myeloma, mantle cell lymphoma, and anemia | 8,588 | 8,994 |
| Dasatinib | Treats chronic myeloid leukemia and acute lymphoblastic leukemia | 6,405 | 6,915 |
| Sunitinib malate | Targeted therapy; a receptor protein-tyrosine kinase inhibitor to treat late-stage kidney cancer, gastrointestinal stromal tumor, and metastatic pancreatic cancer | 6,075 | 6,614 |
| Nilotinib hydrochloride | Treats leukemia | 7,027 | 6,934 |
| Erlotinib hydrochloride | Interferes with the growth of cancer cells and slows their spread in the body; Treats non-small cell lung, and metastatic pancreatic cancer. | 4,189 | 5,222 |
| Everolimus | Treats certain types of kidney cancer, breast cancer, or brain tumor. | 6,776 | 8,012 |
| Pazopanib hydrochloride | Treats advanced kidney cancer, and soft tissue sarcoma | 5,609 | 6,069 |
| Sorafenib tosylate | Treats liver cancer, thyroid cancer, and advanced renal cell carcinoma. | 5,707 | 7,764 |
| Bexarotene | Treats cutaneous manifestations of cutaneous T-cell lymphoma. | 4,852 | 8,323 |
Calculated based on the Gross Drug Costs in the Part D Prescription Drug Event records by the study sample, and adjusted to 2013 dollars based on the Consumer Price Index for prescription drugs.
Empirical Approaches
We compared changes in specialty cancer drug use and OOP spending before and after the in-gap discount between non-LIS and LIS beneficiaries. LIS patients, who do not have a coverage gap, were used as the control group because they were not affected by the in-gap discount. This approach is known as a difference-in-differences method, and captures the in-gap discount effect on outcomes in the treatment group (non-LIS beneficiaries) by controlling for secular trends.
We constructed four outcome measures: 1) use of any specialty cancer drugs in a given year (a binary indicator), 2) the number of specialty cancer drug fills during the year, 3) annual total spending on specialty cancer drugs (the sum of patient share, plan payment, and subsidy amounts for LIS enrollees), and 4) annual OOP spending on specialty cancer drugs.
Control variables included patient characteristics (age, gender, race, buy-in status, and chronic condition indicators), plan characteristics (offering enhanced or in-gap coverage), ZIP-level median household income, and other county factors (percent college educated, hospital beds and admissions per capita, MA payment rates, the number of doctors per capita, and region indicators). We also included year dummies to control for time-specific effects that are common to all study samples. Further, we used group-specific (LIS vs. non-LIS) year fixed effects to control for potential differential year effects between the two groups.
Our primary analysis included use of any specialty cancer drugs not limited to those approved to treat the patient's cancer type. This captures off-label drug use, which is common in cancer treatments,18 and allows us to examine the total demand for specialty cancer drugs in the study population. To check whether the results are sensitive to the selection of cancer-type specific drugs, we performed additional analyses: First, we selected patients with chronic myeloid leukemia (CML) and examined use of tyrosine kinase inhibitors (TKI) – imatinib, dasatinib, nilotinib – which are top Part D specialty cancer drugs (Table 1). Second, we limited the sample to patients with pancreatic cancer and examined use of erlotinib or sunitinib. Finally, we performed analyses separately for each cancer type.
We used logit regressions to analyze specialty drug use and calculated marginal effects. For the interaction term between non-LIS and post indicators – the variable of our interest, we obtained the average marginal effects.19 For analyses of fill counts and spending, we limited the analysis to specialty cancer drug users, and thus the dependent variables do not have zero values. Among users, the residuals from the regressions were approximately normally distributed. We thus used linear estimations to analyze those outcomes conditional on use. Error terms were accounted for clustering within a plan in all analyses.
3. Results
Table 2 presents the summary statistics of study variables. The table indicates that non-LIS beneficiaries were likely to be white, have fewer chronic conditions, and live in areas with relatively high income and education levels, compared with LIS enrollees.
Table 2. Descriptive data of the study variables by low-income subsidy (LIS) status.
| Mean (Standard Deviation) or % | ||
|---|---|---|
|
| ||
| Non-LIS sample (N=117,260) | LIS sample (N=31,005) | |
| Patient characteristics | ||
| Age | 76.54 (7.18) | 77.28 (7.83) |
| Buy-in status (%) | 0.02 | 78.76 |
| Female (%) | 48.60 | 65.20 |
| White (%) | 96.80 | 74.97 |
| Having diabetes (%) | 28.17 | 45.55 |
| Having hypertension (%) | 69.43 | 81.95 |
| Having ischemic heart disease (%) | 40.38 | 51.34 |
| Having hyperlipidemia (%) | 58.92 | 56.63 |
| Having depression (%) | 13.57 | 27.16 |
| Having congestive heart failure (%) | 18.79 | 35.08 |
| Having cataract (%) | 28.73 | 21.61 |
| Having chronic obstructive pulmonary disease (%) | 13.70 | 26.78 |
| Number of chronic conditions | 4.66 (2.60) | 6.08 (2.89) |
| Plan characteristics | ||
| Enhanced (%) | 43.75 | 8.09 |
| Gap coverage (%) | 15.45 | 2.08 |
| Market characteristics | ||
| Zip-level median household income ($) | 61,317 (25,041) | 50,046 (20,285) |
| Zip-level college educated (%) | 27.43 | 20.51 |
| County-level factors | ||
| Medicare Advantage payment ($) | 806.98 (133.51) | 823.32 (136.93) |
| Hospital admission/1,000 | 124.16 (79.09) | 126.27 (78.25) |
| Physician supply/1,000 | 2.94 (2.13) | 2.87 (2.16) |
| Hospital beds/1,000 | 3.26 (2.59) | 3.36 (2.43) |
| Census region | ||
| Midwest (%) | 19.76 | 23.31 |
| South (%) | 37.96 | 40.47 |
| West (%) | 16.54 | 16.98 |
| Northeast (%) | 25.74 | 19.24 |
| Specialty cancer drug use (N, %) | 3,551 (3.03) | 1,769 (5.71) |
| Among specialty cancer drug users | ||
| Reaching coverage gap (%) | 99.21 | 99.72 |
| Reaching catastrophic coverage (%) | 94.40 | 97.06 |
| Annual number of fills | 7.71 (4.63) | 7.67 (4.43) |
| Total annual spending ($) | 44,764 (30,307) | 44,272 (30,201) |
| Total annual out-of-pocket spending ($) | 4,870 (2,099) | 44 (187) |
| In-gap out-of-pocket spending ($) | 2,689 (1,215) | 41 (176) |
About 3% of non-LIS patients used a specialty cancer drug in a year, and each user spent $4,870 out-of-pocket per year on average. The average total annual spending on specialty cancer drugs was $44,764 per user. Most specialty cancer drug users reached the coverage gap (99%) and catastrophic coverage (94%). In contrast, the LIS group had higher specialty drug use rates (5.7%) than the non-LIS group, yet the average OOP spending on specialty cancer drugs among users was only $44. It is likely that subsidies helped to increase LIS beneficiaries' access to specialty cancer drugs. Different characteristics of the LIS patients, such as health status, may also have contributed to the relatively high rate of specialty drug use.
Table 3 describes trends in specialty cancer drug use and OOP spending. The data indicate that the utilization rates of specialty cancer drugs increased over years but to a small degree and that there was no differential increase following the in-gap discount. Among users, the number of specialty cancer drug fills remained stable. Despite little changes in utilization among users, total spending on specialty cancer drugs per user increased substantially over years in both groups – possibly due to rises in drug prices (Table 1). We found that non-LIS beneficiaries' OOP spending on specialty cancer drugs significantly decreased after the in-gap discount. Annual OOP spending on specialty cancer drugs of non-LIS beneficiaries sharply dropped between 2010 and 2011 from $5,752 to $4,277 (-26%). The average annual OOP spending in the post-discount period (2011-2013) was $4,494, which corresponds to a 19% decrease from $5,533 in the pre-discount period (2009-2010).
Table 3. Specialty cancer drug use and spending by year and low-income subsidy (LIS) status.
| Non-LIS sample | LIS sample | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Specialty cancer drug use | ||||||
|
| ||||||
| N | Specialty cancer drug use (N, %) | N | Specialty cancer drug use (N, %) | |||
|
|
||||||
| 2009 | 19,294 | 575 (2.98) | 5,652 | 280 (4.95) | ||
| 2010 | 20,734 | 599 (2.89) | 5,830 | 306 (5.25) | ||
| 2011 | 23,496 | 689 (2.93) | 6,346 | 361 (5.69) | ||
| 2012 | 25,515 | 764 (2.99) | 6,549 | 389 (5.94) | ||
| 2013 | 28,221 | 924 (3.27) | 6,628 | 433 (6.53) | ||
|
| ||||||
| Among specialty cancer drug users (Mean, Standard Deviation) | ||||||
|
| ||||||
| Number of fills | Total spending ($) | Out-of-pocket spending ($) | Number of fills | Total spending ($) | Out-of-pocket spending ($) | |
|
|
||||||
| 2009 | 7.44 (4.95) | 34,327 (23,665) | 5,366 (2,184) | 7.80 (4.80) | 36,358 (24,507) | 53 (200) |
| 2010 | 7.61 (4.67) | 38,479 (26,531) | 5,752 (2,156) | 7.55 (4.39) | 39,247 (26,569) | 59 (222) |
| 2011 | 7.85 (4.49) | 44,308 (28,313) | 4,277 (1,840) | 7.89 (4.55) | 43,931 (28,416) | 41 (181) |
| 2012 | 7.98 (4.55) | 50,044 (31,810) | 4,612 (1,965) | 7.96 (4.37) | 47,964 (31,725) | 34 (159) |
| 2013 | 7.63 (4.58) | 51,309 (33,686) | 4,643 (2,054) | 7.24 (4.12) | 49,910 (34,161) | 39 (180) |
Note: All spending measures are limited to specialty cancer drugs, and they are adjusted to 2013 dollars based on the Consumer Price Index for prescription drugs.
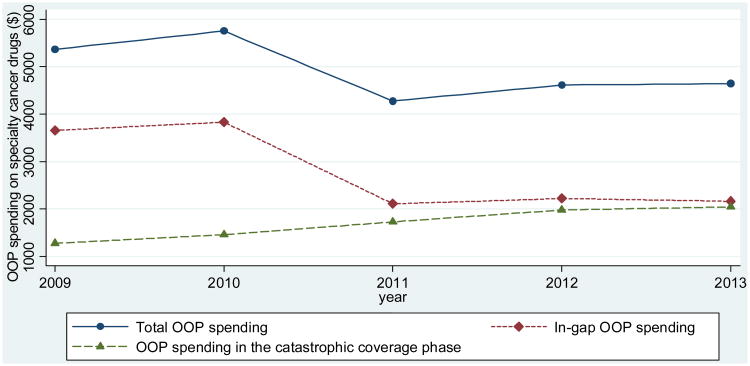
Figure 1 depicts changes in OOP spending on specialty cancer drugs separately for the gap and catastrophic coverage phases in the non-LIS group. A large reduction in OOP spending occurred in the gap phase following the ACA discount: the average in-gap OOP spending decreased by 42% from $3,744 in the pre-discount period to $2,165 in the post-discount periods. However, OOP spending in the catastrophic coverage phase increased from $1,369 to $1,918 between pre- and post-discount periods.
Figure 1.
Out-of-pocket (OOP) spending on specialty cancer drugs by year among beneficiaries with no low-income subsidies (non-LIS)
Table 4 presents results on key variables from regression analyses. We report average marginal effects of the in-gap discount on specialty cancer drug use and OOP spending. The in-gap discount had no significant effect on use of specialty cancer drugs – either any use or the number of fills – among non-LIS beneficiaries. However, it significantly decreased non-LIS patients' annual OOP spending on specialty cancer drugs among users by $1,108. The results on all other covariates are reported in Table A1.
Table 4. Regression results on selected variables.
| Variable | Marginal effect (robust standard error)a | |||
|---|---|---|---|---|
|
| ||||
| Specialty cancer drug use | Among specialty cancer drug users | |||
|
| ||||
| Number of fills | Total spending | Out-of-pocket spending | ||
| All study sample | ||||
| Non-low income subsidy (Non-LIS) | -0.92(0.37)** | -0.63(0.42) | -4,654(2,575)* | 4,988(135)*** |
| Post-discount (POST) | 0.21(0.25) | 0.17(0.35) | 8,144(2,018)*** | 51(51) |
| Non-LIS*POST | -0.05(0.05) | 0.16(0.43) | 1,503(2,462) | -1,114(126)*** |
| N | 148,265 | 5,320 | 5,320 | 5,320 |
|
| ||||
| Sub-group analysis with specific cancer-type agents | ||||
| Patients with chronic myeloid leukemia | ||||
| Non-LIS | -0.70(5.55) | -0.10(0.46) | -3,708(3,582) | 5,657(191)*** |
| POST | 5.48(4.22) | 0.31(0.38) | 10,617(2,782)*** | 34(67) |
| Non-LIS*POST | 0.02(0.18) | 0.56(0.47) | 5,060(3,327) | -970(176)*** |
| N | 3,541 | 2,065 | 2,065 | 2,065 |
|
| ||||
| Patients with pancreatic cancer | ||||
| Non-LIS | 1.30(1.29) | -0.16(1.76) | 779(6,608) | 3,470(442)*** |
| POST | -1.32(1.18) | -0.08(1.74) | 1,033(6,956) | -230(319) |
| Non-LIS*POST | -0.56(0.60) | 0.97(1.87) | 3,920(7,768) | -704(448) |
| N | 8,199 | 246 | 246 | 246 |
Note: All spending measures are limited to specialty cancer drugs, and they are adjusted to 2013 dollars based on the Consumer Price Index for prescription drugs;
All models control for patient, plan, and market characteristics; standard errors are accounted for clustering within a plan;
p < 0.10,
p < 0.05,
p < 0.01.
The results from the sub-group analyses were consistent with the primary analysis. In both CML and pancreatic cancer groups, specialty drug utilization did not change after the in-gap discount. Among non-LIS patients with CML, annual OOP spending on TKI declined by $970 after the in-gap discount. Non-LIS beneficiaries with pancreatic cancer also had a reduction in OOP spending on erlotinib or sunitinib, but this effect was not statistically significant possibly due to the small sample size (N=246). Separate analyses by cancer type also produced similar results to the primary analysis (results not shown).
4. Conclusions
We found that the ACA in-gap discount decreased patients' OOP spending on specialty cancer drugs but did not increase specialty cancer drug use. It is encouraging that the ACA's initiative to close the coverage gap in Part D mitigated the patients' financial burdens, to some extent. A $1,108 decrease in annual OOP spending on specialty anti-neoplastic drugs (-19%) is not a small reduction; however, some cancer patients without subsidies face a large financial burden even with the in-gap discount. The average annual budget of Medicare beneficiaries was reported to be $33,000 in 2012.20 Thus, the mean OOP spending of $4,511 implies that cancer patients who use a specialty drug covered by Part D spent 15% of their budget on specialty cancer drugs. Further, about 14% of (non-LIS) cancer patients spent more than $6,600 – 20% of their budget – on specialty cancer drugs. This suggests that the in-gap discount does not offer sufficient financial protection to certain specialty cancer drug users.
Our finding of no impact of the in-gap discount on specialty cancer drug use might be because patients are not responsive to cost-sharing in specialty drug use. Alternatively, it may be because the cost-sharing reduction kicks in after relatively high cost-sharing for specialty drugs in the pre-gap phase.12 Beneficiaries would not use specialty drugs regardless of the in-gap discount if they cannot afford cost-sharing in initial coverage. Or, some patients may not begin specialty drug treatments due to high annual OOP spending required to complete a course of treatment. To these patients, the in-gap discount is irrelevant and unlikely to lead them to use specialty drugs.
In Part D, catastrophic coverage is a stop-loss mechanism. However, because of high prices of specialty drugs, even the 5% coinsurance in catastrophic coverage can bring a financial pressure on patients. Our data showed that the average OOP spending on specialty cancer drugs in catastrophic coverage increased from $1,277 to $2,046. This change reflects increases in drug prices given no change in drug fills among users. This high level of OOP spending even in the catastrophic coverage phase may have deterred patients from starting a specialty drug.
Demand for specialty drugs is expected to increase as more drugs become available.4,21 Because specialty drugs do not usually have substitutes,3 high cost-sharing for specialty drugs can create financial difficulties to patients, limiting access to needed drugs. Some patients may use specialty drugs despite high cost-sharing; however, high cost-sharing puts these patients at financial risk. It will thus be critical to identify high-value specialty drugs and to ensure patients' access to those medications. Reducing financial stress on beneficiaries who need expensive but effective drugs can help improve patients' access to needed drugs. Expanding eligibility for low-income cost-sharing subsidies for certain costly yet effective specialty drugs might be an option to explore.
This study has several limitations. First, we do not have detailed clinical information, such as cancer stage, which may predict patterns of specialty drug use. However, this would result in any bias only if temporal changes in the distribution of cancer stage systematically differed by LIS status, which is unlikely. Second, Medicare data lack beneficiary-level income information. Our use of ZIP-level median household income may not perfectly capture income of elderly beneficiaries. Third, we focused on the impact of the in-gap benefit change. Our finding may not apply to patients' responsiveness to changes in overall or initial cost-sharing in specialty cancer drug use.. Fourth, we examined costly specialty drugs only. Potential differences in the responsiveness to the in-gap discount by drug price are a topic to pursue in future research. Finally, our study is limited to PDP enrollees with six uncommon cancers, and the results may not be generalizable to MA-PD enrollees or patients with other conditions.
In summary, the Part D in-gap discount patients' OOP spending on specialty cancer drugs; however, even with the in-gap discount, financial burdens of specialty cancer drug users without subsidies remain high. Approaches to reduce financial burdens for high-value specialty drugs may improve patients' access to needed drugs.
Take-Away Points.
A provision in the Affordable Care Act (ACA) provided discounts for prescription drug spending in the coverage gap in Medicare Part D. The impacts of this in-gap discount among specialty cancer drug users were:
The in-gap discount did not increase the likelihood of using a specialty cancer drug.
The in-gap discount did not change the number of specialty cancer drug fills among users.
Specialty cancer drug users' annual out-of-pocket spending on specialty cancer drugs decreased from $5,533 to $4,494 (-19%) after the in-gap discount.
Some cancer patients' financial burdens remain high even with the in-gap discount.
Acknowledgments
Funding Sources: This work was supported by NIH/NIA grant number 1R01AG047934-01, and NIH grant number R24 HD041025. No conflicts of interest exist.
Appendix
Table A1. Full regression results.
| Variables | Specialty cancer drug use (Marginal effects, SEa) | Among specialty cancer drug users (Coefficients, SEa) | ||
|---|---|---|---|---|
|
| ||||
| Number of fills | Total spending | Out-of-pocket spending | ||
| Non-low income subsidy (Non-LIS) | -0.92(0.37)** | -0.63(0.42) | -4,654(2,575)* | 4,988(135)*** |
| Post-discount (POST) | 0.21(0.25) | 0.17(0.35) | 8,144(2,018)*** | 51(51) |
| Non-LIS*POST | -0.05(0.05) | 0.16(0.43) | 1,503(2,462) | -1,114(126)*** |
| Age | -0.16(0.01)*** | 0.01(0.01) | -260(73)*** | -11.5(4.8)** |
| Buy-in status | 0.15(0.30) | 0.09(0.37) | 381(2,626) | -162(47)*** |
| Female | -0.319(0.15)** | 0.08(0.16) | -2,236(1,123)** | -105(64) |
| White | -1.66(0.21)*** | -0.21(0.23) | 1,685(1,591) | -13(72) |
| Having diabetes | -0.35(0.14)** | 0.03(0.18) | 737(1,223) | -19(64) |
| Having hypertension | -0.14(0.19) | 0.06(0.20) | 483(1,326) | 1.2(76.7) |
| Having heart disease | -0.18(0.16) | 0.52(0.19)*** | 1,038(1,156) | 51(61) |
| Having hyperlipidemia | -1.77(0.13)*** | 0.23(0.16) | 241(1,081) | 5.6(55.2) |
| Having depression | -0.93(0.16)*** | -0.08(0.20) | 182(1,369) | -119(68)* |
| Having congestive heart failure | 0.09(0.17) | 0.28(0.22) | 833(1,272) | 47(68) |
| Having cataract | -0.63(0.14)*** | 0.63(0.18)*** | 3,393(1,001)*** | 209(63)*** |
| Having chronic obstructive pulmonary disease | -0.91(0.18)*** | -0.54(0.20)*** | -3,274(1,318)** | -166(75)** |
| Number of chronic conditions | 0.52(0.05)*** | -0.30(0.06)*** | -1,251(348)*** | -55(19)*** |
| Enhanced (%) | -0.09(0.16) | -0.09(0.20) | -570(1,241) | 107(84) |
| Gap coverage (%) | 0.99(0.24)*** | 0.67(0.24)*** | 4,978(1,757)*** | 230(109)** |
| Median household income ($1,000) | 0.01(0.01) | -0.00(0.01) | 16.6(37.6) | 0.54(2.32) |
| College educated (%) | -0.02(0.01)** | 0.00(0.01) | 1.4(54.5) | 0.18(3.34) |
| Medicare Advantage payment ($) | 0.00(0.00)*** | -0.00(0.00) | -4.4(5.6) | -0.59(0.33)* |
| Midwest | -0.48(0.23)** | -0.07(0.27) | 458(1,941) | -522(132)*** |
| South | -0.09(0.19) | -0.14(0.21) | -507(1,519) | -0.45(77.30) |
| West | -0.37(0.22)* | -0.54(0.23)** | -1,802(1,734) | -39(92) |
| Hospital admission/1,000 | -0.00(0.00) | -0.00(0.00) | 4.3(9.8) | -0.43(0.60) |
| Physician supply/1,000 | 0.00(0.05) | 0.00(0.6) | -331(371) | 6.7(19.2) |
| Hospital beds/1,000 | 0.09(0.04)** | 0.05(0.02)** | 157(211) | 7.8(11.9) |
| 2010 | 0.09(0.22) | -0.28(0.32) | 2,928(1,622)* | 32(33) |
| 2012 | 0.08(0.18) | 0.06(0.27) | 4,352(1,781)** | 31(28) |
| 2013 | 0.44(0.25)* | -0.65(0.28)** | 6,629(2,006)*** | 29(39) |
| Non-LIS*2010 | -0.02(0.05) | 0.43(0.40) | 1,347(1,983) | 365(109)*** |
| Non-LIS*2012 | -0.02(0.05) | 0.20(0.33) | 2,404(2,259) | 363(90)*** |
| Non-LIS*2013 | -0.11(0.08) | 0.62(0.34)* | 1,744(2,446) | 371(91)*** |
| N | 148,265 | 5,320 | 5,320 | 5,320 |
Standard error terms are accounted for clustering within a plan;
p < 0.10,
p < 0.05,
p < 0.01
Footnotes
Precise: This study examines the early impacts of closing the donut hole in Medicare Part D.
Contributor Information
Jeah Jung, Department of Health Policy and Administration, College of Health and Human Development, The Pennsylvania State University.
Wendy Yi Xu, Division of Health Services Management and Policy, Ohio State University.
Chelim Cheong, Department of Health Policy and Administration, The Pennsylvania State University.
References
- 1.Express Scripts. 2014 drug trend report. [Accessed April 18, 2016]; http://lab.express-scripts.com/drug-trend-report. Published March 2015.
- 2.Centers for Medicare and Medicaid Services. National health expenditures 2014 highlights. [Accessed April 18, 2016]; https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/downloads/highlights.pdf. Published 2015.
- 3.Tu HT, Samuel DR. Limited options to manage specialty drug spending. [Accessed April 18, 2016]; http://www.hschange.com/CONTENT/1286/1286.pdf. Published April 2012. [PubMed]
- 4.America's Health Insurance Plan. Specialty drugs: Issues and challenges. [Accessed April 18, 2016]; http://www.ahip.org/wp-content/uploads/2015/07/IssueBrief_SpecialtyDrugs_7.9.15.pdf. Published July 2015.
- 5.Hoadley J. Assessing Medicare Part D ten years after enactment. [Accessed April 18, 2016]; http://www.aging.senate.gov/imo/media/doc/02_Hoadley_5_22_13.pdf. Published May 22, 2013.
- 6.Kaiser Family Foundation. Although a small share of Medicare Part D enrollees take specialty drugs, a new analysis finds those who do can face thousands of dollars in out-of-pocket drug costs despite plan limits on catastrophic expenses. [Accessed April 18, 2016]; http://kff.org/medicare/press-release/although-a-small-share-of-medicare-part-d-enrollees-take-specialty-drugs-a-new-analysis-finds-those-who-do-can-face-thousands-of-dollars-in-out-of-pocket-drug-costs-despite-plan-limits-on-catastrophi. Published December 2, 2015.
- 7.Goldman DP, Joyce GF, Zheng Y. Prescription drug spending: associations with medication and medical utilization and spending and health. JAMA. 2007;298(1):61–69. doi: 10.1001/jama.298.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doshi JA, Li P, Ladage VP, et al. Impact of cost sharing on specialty drug utilization and outcomes: A review of the evidence and future directions. Am J Manag Care. 2016;22(3):188–197. [PubMed] [Google Scholar]
- 9.Hoadley J, Hargrave E, Cubanski J, et al. Medicare Part D 2009 data spotlight: Specialty tiers. [Accessed April 18, 2015]; https://kaiserfamilyfoundation.files.wordpress.com/2013/01/7919.pdf. Published June 2009.
- 10.Zhang Y, Donohue JM, Newhouse JP, Neuman T. The effects of the coverage gap on drug spending: A closer look at Medicare Part D. Health Aff (Millwood) 2009;28(2):w317–w325. doi: 10.1377/hlthaff.28.2.w317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fung V, Mangione CM, Huang J, et al. Falling into the coverage gap: Part D drug costs and adherence for Medicare Advantage Prescription Drug Plan beneficiaries with diabetes. Health Serv Res. 2010;45(2):355–375. doi: 10.1111/j.1475-6773.2009.01071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doshi JA, Li P, Huo H, et al. High cost sharing and specialty drug initiation under Medicare Part D: A case study in patients with newly diagnosed chronic myeloid leukemia. Am J Manag Care. 2016;22(4 Suppl):S78–S86. [PubMed] [Google Scholar]
- 13.Trish E, Joyce G, Goldman DP. Specialty drug spending trends among Medicare and Medicare Advantage enrollees, 2007-11. Health Aff (Millwood) 2014;33(11):2018–2024. doi: 10.1377/hlthaff.2014.0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dusetzina SB, Keating NL. Mind the gap: Why closing the donut hole is insufficient for increasing Medicare beneficiary access to oral chemotherapy. J Clin Oncol. 2015;33:1–6. doi: 10.1200/JCO.2015.63.7736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herrick DM. National center for policy analysis: Specialty drugs and pharmacies. [Accessed April 18, 2016]; www.ncpa.org/pdfs/st355.pdf. Published May 22, 2014.
- 16.Government Accountability Office. Medicare Part D: Spending, beneficiary cost sharing, and cost-containment efforts for high-cost drugs eligible for a specialty tier. [Accessed April 18, 2016]; http://www.gao.gov/new.items/d10242.pdf. Published January 2010.
- 17.Medi-Span Electronic Drug File (MED-File) v 2. Indianapolis, IN: Wolters Kluwer; [Accessed April 18, 2016]. http://www.wolterskluwercdi.com/drug-data/medispan-electronic-drug-file/ [Google Scholar]
- 18.Pfister DG. Off-label use of oncology drugs: The need for more data and then some. J Clin Oncol. 2012;30(6):584–586. doi: 10.1200/JCO.2011.38.5567. [DOI] [PubMed] [Google Scholar]
- 19.Ai C, Norton E. Interaction terms in logit and probit models. Econ Lett. 2003;80:123–129. [Google Scholar]
- 20.Cubanski J, Swoope C, Damico A, Neuman T. Health care on a budget: The financial burden of health spending by Medicare households. [Accessed April 18, 2016]; http://kff.org/medicare/issue-brief/health-care-on-a-budget-the-financial-burden-of-health-spending-by-medicare-households. Published January 9, 2014.
- 21.Payer Perspectives. The growing cost of specialty pharmacy-Is it sustainable? [Accessed April 18, 2016]; http://www.ajmc.com/payer-perspectives/0213/The-Growing-Cost-of-Specialty-PharmacyIs-it-Sustainable. Published February 18, 2013.