Abstract
Introduction:
Laparoscopic adjustable gastric banding and laparoscopic sleeve gastrectomy are popular bariatric procedures. Certain complications may necessitate revision. Adverse outcomes are reported after revisional bariatric surgery. We compared patients undergoing revisional versus primary laparoscopic Roux-en-Y gastric bypass (LRYGB).
Materials and Methods
This was retrospective comparative 1:1 case-matched analysis of revisional LRYGB Group A versus primary LRYGB (pLRYGB/Group B). Matching was based on body mass index (BMI) and comorbidities. BMI decrease at 6 and 12 months post-surgery, comorbidity resolution, operative time, morbidity and length of hospital stay (LOS) were compared. Total decrease in BMI, i.e., change from before initial bariatric procedure to 12 months after revision for Group A was also compared.
Results:
Median BMI (inter-quartile range) for Group A decreased to 44.74 (7.09) and 41.49 (6.26) at 6 and 12 months, respectively, for Group B corresponding figures were 38.74 (6.9) and 33.79 (6.64) (P = 0.001 and P = 0.0001, respectively). Total decrease in BMI (Group A) was 9.8, whereas BMI decrease at 12 months for Group B was 15.2 (P = 0.23). Hypertension resolved in 63% (Group A), 70% (Group B) (P = 0.6). Diabetes resolution was 80% (Group A), 63% (Group B) (P = 0.8). Operative time for Groups A, B was 151 ± 17, 137 ± 11 min, respectively (P = 0.004). There was no difference in morbidity and LOS.
Conclusion:
Comorbidity resolution after revisional and pLRYGB are similar. Less weight loss is achieved after revision than after pLRYGB, but total weight loss is comparable. Revisional surgery is safe when performed by experienced surgeons in high-volume centres.
Keywords: Case-matched cohort, revisional bariatric surgery, Roux-en-Y gastric bypass
INTRODUCTION
Bariatric surgery results in effective and sustained weight loss and resolution of comorbidities in the morbidly obese.[1] Common bariatric procedures in current practice include laparoscopic adjustable gastric banding (LAGB), laparoscopic sleeve gastrectomy (LSG), laparoscopic Roux-en-Y Gastric Bypass (LRYGB) and laparoscopic bilio-pancreatic diversion (BPD). LAGB and LSG are popular due to technical ease.
The incidence of revisional surgery is increasing due to inadequate weight loss or weight re-gain. However, certain procedure-specific complications also form indications for revision. Complications such as band erosion and slippage, oesophageal dilatation and dysmotility and tube/port dysfunction may occur after LAGB.[2] Persistent staple-line leak, dysphagia secondary to stricture formation and gastro-oesophageal reflux disease (GERD) are complications specific to LSG.[3]
The requirement for revisional bariatric surgery ranges from 5% to 50%.[4] LRYGB is a popular revisional procedure with several studies showing good weight loss.[5,6,7,8] However, results following revisional LRYGB (rLRYGB) are considered inferior when compared to those following primary LRYGB (pLRYGB). We performed a retrospective study in which patients undergoing rLRYGB at our institute after a previous bariatric procedure (either primary LAGB or primary LSG) were compared with a case-matched cohort undergoing pLRYGB, with the aim of reporting the peri-operative and early outcomes of rLRYGB versus pLRYGB. We also reviewed literature relevant to revisional bariatric surgery.
MATERIALS AND METHODS
Computerised records of patients have been maintained prospectively since the beginning of the bariatric surgery programme at our institution in 2003. Records of all patients undergoing bariatric surgery from the beginning till date were reviewed. Fifty-five LAGB have been performed at this institute, of which ten required revision subsequently. The corresponding figures for LSG are 374 and seven.
Study population
The study period was defined as December 2009 to December 2012. Thirty-eight patients underwent revisional bariatric surgery in this period. The decision of choice of revisional procedure was taken by a well-informed patient.
Revisional LSG was done in eight patients, and they were excluded from the study. Of 38 patients undergoing revisional bariatric surgery, thirty underwent rLRYGB and were included in the study. This group of patients undergoing rLRYGB was labelled Group A. The primary bariatric procedure in Group A was either LAGB or LSG.
A parallel comparable group of patients undergoing pLRYGB (Group B) was identified from our data-base and were matched case-to-case with each patient in group A.
Matching process
The patients in the two groups were matched on the basis of body mass index (BMI) and the presence of comorbidities, i.e., hypertension and diabetes mellitus, at the time of LRYGB.
Surgical procedure
The revision from LAGB to rLRYGB was done in two stages. In the first stage, only the gastric band was removed. The second stage was performed after 3–6 months, to allow resolution of fibrosis and scarring, and included the definitive surgery, i.e., rLRYGB. The revision from LSG to rLRYGB was a single-stage procedure.
Patients in both groups underwent a standardised ante-gastric ante-colic LRYGB, the salient features of which are as follows: the omentum was divided vertically to decrease the tension on the ante-colic Roux limb. The lengths of bilio-pancreatic and alimentary limbs were 75 cm and 100 cm, respectively. The jejuno-jejunostomy (JJ) was done by “triple stapled technique,” i.e., side-to-side anastomoses with application of 60 mm linear endo-stapler (Echelon ENDOPATH™, Ethicon) (white cartridge) in both directions from the enterotomy, and closure of the common enterotomy by a third application of the same stapler. A gastric pouch 20–30 ml size is formed by the serial application of 60 mm linear endo-stapler (blue cartridge). The gastro-jejunostomy was created using 25 mm circular stapler (3.5 mm stapler height, DST Series™ EEA™ OrVil™ 25 mm). Both the Petersen's and JJ mesenteric defect were closed from base to apex using a continuous non-absorbable suture technique.
Discharge criteria
A defined discharge protocol was followed in all patients. Patients were discharged when they achieved an oral liquid intake of >1.5 L, were ambulating well and post-operative pain was well controlled with oral analgesics.
Follow-up protocol
A 24-h emergency number was provided to all patients after discharge. They were advised to actively report symptoms such as severe abdominal pain, vomiting and melena. Follow-up visits were scheduled at 1, 3, 6 and 12 months post-surgery. In case of no-show at scheduled follow-up, an attempt was made to contact them telephonically.
Data collection
For both groups, operative time, early post-operative morbidity and length of hospital stay (LOS) was recorded. BMI of patients in both groups was recorded before surgery, and at 6 and 12 months after surgery. For patients in Group A, BMI before the primary bariatric procedure was also retrieved to determine the total decrease in BMI, i.e., from before initial bariatric procedure to 12 months after revisional surgery. The degree of resolution of co-morbidity was noted at 12 months follow-up visit. No patients were lost to follow-up in either group.
Outcomes
The primary outcome of the study was to compare early decrease in BMI (at 6 and 12 months post-surgery) in patients undergoing rLRYGB (Group A) with those undergoing pLRYGB (Group B). We also compared the resolution of comorbidities between the two groups, and operative duration, LOS and complication rates.
Statistical analysis
The demographic data of the two groups were compared statistically to demonstrate adequate matching. Pre-LRYGB BMI of the patients was found to be normally distributed, and hence has been expressed as mean (standard deviation) in Table 1. The changes in BMI post-LRYGB are skewed in their distribution and hence in subsequent tables, i.e., Tables 2 and 3, median (inter-quartile range) is used and the changes post-LRYGB at 6 and 12 months were analysed using the Mann–Whitney test. Operative time was expressed in mean (standard deviation). The data were analysed using SPSS software version 16 Statistical Package for the Social Sciences (SPSS).
Table 1.
Demographic data of the two groups in the study (n=30)
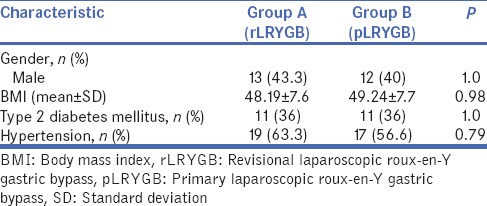
Table 2.
Comparison of decrease in body mass index
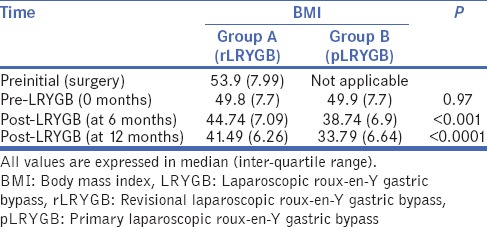
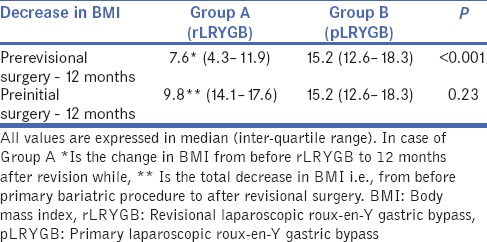
Table 3.
Comparison of decrease in body mass index in Group versus Group B at 12 months
RESULTS
Study population description
During the study, thirty patients underwent rLRYGB (Group A). The primary bariatric procedure was LAGB in 17 patients, and LSG in 13.
Among post-LAGB patients, 7/17 had undergone banding at our institute, whereas 10/17 had been banded at other centres and presented to us for revision. All 13 post-LSG patients had their primary bariatric surgery at our institute.
The post-LSG patients underwent revision due to inadequate weight loss or weight regain, but not for procedure-related or technical complications. The indications for revision after LAGB in this study were inadequate weight loss primarily, or stomach prolapse and band migration, leading to inadequate weight loss or weight regain.
The time between primary bariatric procedure and revisional surgery ranged from 3 to 7 years for Group A.
The demographic data of the two groups are represented in Table 1.
Decrease in body mass index
The decrease in BMI was significantly less in Group A (rLRYGB) than Group B (pLRYGB) at 6 and 12 months follow-up (P < 0.001 and P < 0.0001, respectively). Table 2 shows comparison of decrease in BMI.
We considered total decrease in BMI for Group A, i.e., decrease in BMI from before the primary bariatric procedure to 12 months after revisional surgery. The total decrease in BMI in Group A (rLRYGB) was less than the decrease in BMI at 12 months post-pLRYGB for Group B (pLRYGB), but this was not statistically significant (P = 0.23). Table 3 shows comparison of total decrease in BMI in Group A versus Group B at 12 months.
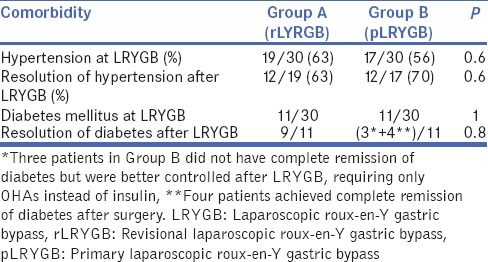
Resolution of co-morbidities
The resolution of comorbidities was similar between the two groups. Table 4 shows comparison of resolution of comorbidities between the two groups.
Table 4.
Comparison of resolution of comorbidities between the two groups
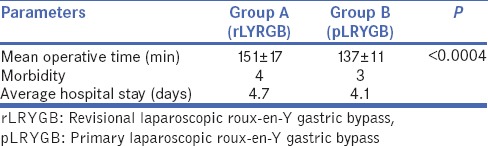
Operative time, morbidity and length of hospital stay
The operative time (expressed as mean ± standard deviation) was 151 ± 17 min for rLRYGB versus 137 ± 11 min for pLRYGB (P < 0.0004).
The only peri-operative complication seen in either group was a significant drop in haemoglobin requiring blood transfusion. This was similar in both groups (13.3%). There were no complications encountered during band removal procedure.
There was no significant difference in LOS between the two groups.
(Table 5 Comparison of operative time, morbidity, mean hospital stay).
Table 5.
Comparison of operative time, morbidity, mean hospital stay
DISCUSSION
In this study, we analysed thirty patients who underwent rLRYGB, after primary bariatric procedure that was either LAGB or LSG. We compared these patients with a matched group of patients who underwent pLRYGB. The parameters compared were decrease in BMI at 6 and 12 months post-LRYGB, resolution of comorbidities, operative time, complication rate and LOS for both groups. We found that the decrease in BMI in Group A was significantly less than in Group B at 6 and 12 months post-surgery, at both points of time. However, this difference although persistent, was not statistically significant when total decrease in BMI for Group A was considered. There was a comparable decrease in comorbidities in both primary and revisional groups. The operative time was longer for revisional surgery than for pLRYGB, here were no significant differences in peri-operative morbidity and hospital stay between both groups.
The incidence of surgical revision after a primary bariatric procedure varies widely in published literature and has been reported to range between 5% and 56%.[4,9] The indications for revision are diverse. Following LAGB, they may be classified as either implant-related such as slippage, migration, leakage, breaking and disconnection of band, motility problems leading to band intolerance such as gastric pouch dilatation, oesophageal dysmotility and reflux, or weight-related such as inadequate weight loss/weight regain.[10] Conditions necessitating revision of LSG include inadequate weight loss/weight regain, severe GERD, stricture and persistent leak.[11]
In this study, all patients were morbidly obese at the time of revision. The main indication for revision after primary LSG was inadequate weight loss or weight regain and none were done for technical complications. Patients with primary LAGB underwent revision for a variety of reasons including inadequate weight loss primarily, or stomach prolapse and band migration, leading to inadequate weight loss or weight regain. No patient in Group A had pre-revisional weight loss secondary to complications such as stomach prolapse/band migration.
For the purpose of this study, we defined inadequate weight loss as less than 40% excess weight loss (EWL) at 1 year post-procedure[12] and weight re-gain as more than 15% weight increase from nadir.[13] There is much debate regarding appropriate measures to define success or failure of bariatric procedure. Brolin defined a loss (≥50%) of excess weight as satisfactory, a criterion that has been subsequently used by various investigators.[14] According to the criterion of Reinhold[15] modified by Christou[16] post-operative outcomes are good when BMI ≤35 kg/m2 and excellent when BMI ≤30 kg/m2. The issue is further complicated by the fact that the criteria for failure differs for a purely restrictive procedure like LAGB, and is defined as <5% EWL at 2 years.[12]
The choice of revisional procedure depends on the primary bariatric procedure performed and the indication for revision. Gagner, et al. propose that in case of revision after primary LAGB, this decision should depend on the reason for revision.[17] If the patient has achieved sufficient weight loss but is suffering from band-related complications like slippage, they might benefit from replacement of the band,[18] or conversion to another restrictive procedure in case of pouch dilatation.[17] In case of inadequate weight loss from the very beginning or band intolerance or complications like reflux, conversion to LRYGB or BPD is recommended.[17] On the other hand, Elnahas et al. stated that a key principle of revisional bariatric surgery is that if a purely restrictive procedure requires revision, it should be to one with a malabsorptive component and not merely to another pure restrictive procedure.[2]
The reported outcomes after revisional surgery vary widely. Some studies suggest that morbidity after revisional bariatric surgery can range from 8% to 46%.[18,19,20,21] For rLRYGB, the complication rate can be as high as 32%–62%,[22,23] much greater than those for pLRYGB.[6,23,24,25] This is largely due to technical difficulties encountered during revisional surgery, which is reflected in an increase in operative time. These difficulties include the presence of intra-abdominal adhesions, especially after band infection, adherence of the locking mechanism to the liver/spleen which may cause haemorrhage and obliteration of the lesser sac requiring dissection before each fire of the stapler.[26] An increase in intra-operative time and bleeding may secondarily increase the risk of respiratory or thromboembolic complications.[27] However, there are also several publications which report that laparoscopic revision can be performed safely and without compromising successful weight loss if performed by well-trained and experienced bariatric surgeons in high-volume centres.[8,28,29] In this study, the only complication encountered was a significant drop in haemoglobin requiring blood transfusion, which was similar in both groups (13.3%). The operative time was greater for rLRYGB than pLRYGB (151 ± 17 min for rLRYGB vs. 137 ± 11 min for pLRYGB). There was no increase in duration of hospital stay in the revisional group. There was no mortality encountered in either group.
Several studies comparing revisional and pLRYGB have reported discordant degrees of weight loss. Two previously published case-matched analysis report that patients undergoing revisional RYGB experience less weight loss than those undergoing pLRYGB.[22,27] Our data too suggest a significantly lower weight loss and fall in BMI in the rLRYGB group at 1 year after surgery. This may be because patients requiring revisional surgery for inadequate weight loss may have learned to adjust their eating behaviour, or that they may have poor dietary compliance.[28] Others suggest that the physiology of energy metabolism may be different for a secondary procedure than a primary procedure.[10] In fact, technical factors such as difficulty in creation of an adequately small pouch due to scarring from primary procedure may also contribute to lesser weight loss.[10] On the other hand, there are series which report a similar degree of weight loss between rLRYGB and pLRYGB.[5,28,30] The conflicting results between various studies may be due to significant differences in pre-operative BMI in the two groups. This selection bias was eliminated by our case-control matched study design.
A number of studies on comorbidity resolution after revisional surgery showed that revisional surgery was effective in improving obesity-related comorbidities.[31,32] The study showed similar resolution of comorbidities in both the groups.
The limitation of this study is the small sample size of the revisional group. However, the case-matched study design and the surgical expertise available at a high volume bariatric centre add significant value to this study.
Although the decrease in BMI following rLRYGB is less when compared to the primary procedure, we believe that rLRYGB is associated with reasonable safety and an acceptable rate of complications when performed by experienced surgeons in high-volume centres. Studies with a longer follow-up and larger sample size are required to assess and evaluate the weight loss and late complications in rLRYGB compared to pLRYGB.
CONCLUSION
rLRYGB results in safe and effective weight loss as well as resolution of comorbidities in patients with a failed primary bariatric procedure. Although revisional surgery takes longer and is more technically challenging, inexperienced hands and at high volume centres, there is no significant difference in results, morbidity, mortality or LOS as compared to those undergoing pLRYGB.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: A systematic review and meta-analysis. JAMA. 2004;292:1724–37. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 2.Elnahas A, Graybiel K, Farrokhyar F, Gmora S, Anvari M, Hong D. Revisional surgery after failed laparoscopic adjustable gastric banding: A systematic review. Surg Endosc. 2013;27:740–5. doi: 10.1007/s00464-012-2510-2. [DOI] [PubMed] [Google Scholar]
- 3.Brethauer SA. Sleeve gastrectomy. Surg Clin North Am. 2011;91:1265–79. doi: 10.1016/j.suc.2011.08.012. ix. [DOI] [PubMed] [Google Scholar]
- 4.Kellogg TA. Revisional bariatric surgery. Surg Clin North Am. 2011;91:1353–71. doi: 10.1016/j.suc.2011.08.004. x. [DOI] [PubMed] [Google Scholar]
- 5.Topart P, Becouarn G, Ritz P. Biliopancreatic diversion with duodenal switch or gastric bypass for failed gastric banding: Retrospective study from two institutions with preliminary results. Surg Obes Relat Dis. 2007;3:521–5. doi: 10.1016/j.soard.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez R, Gallagher SF, Haines K, Murr MM. Operative technique for converting a failed vertical banded gastroplasty to Roux-en-Y gastric bypass. J Am Coll Surg. 2005;201:366–74. doi: 10.1016/j.jamcollsurg.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 7.Khaitan L, Van Sickle K, Gonzalez R, Lin E, Ramshaw B, Smith CD. Laparoscopic revision of bariatric procedures: Is it feasible? Am Surg. 2005;71:6–10. [PubMed] [Google Scholar]
- 8.Deylgat B, D’Hondt M, Pottel H, Vansteenkiste F, Van Rooy F, Devriendt D. Indications, safety, and feasibility of conversion of failed bariatric surgery to Roux-en-Y gastric bypass: A retrospective comparative study with primary laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2012;26:1997–2002. doi: 10.1007/s00464-011-2140-0. [DOI] [PubMed] [Google Scholar]
- 9.Shimizu H, Annaberdyev S, Motamarry I, Kroh M, Schauer PR, Brethauer SA. Revisional bariatric surgery for unsuccessful weight loss and complications. Obes Surg. 2013;23:1766–73. doi: 10.1007/s11695-013-1012-1. [DOI] [PubMed] [Google Scholar]
- 10.Delko T, Köstler T, Peev M, Esterman A, Oertli D, Zingg U. Revisional versus primary Roux-en-Y gastric bypass: A case-matched analysis. Surg Endosc. 2014;28:552–8. doi: 10.1007/s00464-013-3204-0. [DOI] [PubMed] [Google Scholar]
- 11.van Rutte PW, Smulders JF, de Zoete JP, Nienhuijs SW. Indications and short-term outcomes of revisional surgery after failed or complicated sleeve gastrectomy. Obes Surg. 2012;22:1903–8. doi: 10.1007/s11695-012-0774-1. [DOI] [PubMed] [Google Scholar]
- 12.Menzo EL, Szomstein S, Rosenthal RJ. Reoperative bariatric surgery. In: Nguyen NT, Blackstone RP, Morton JM, Ponce J, Rosenthal RJ, editors. The ASMBS Textbook of Bariatric Surgery. Vol. 1. New York: Springer; 2015. [Google Scholar]
- 13.Odom J, Zalesin KC, Washington TL, Miller WW, Hakmeh B, Zaremba DL, et al. Behavioral predictors of weight regain after bariatric surgery. Obes Surg. 2010;20:349–56. doi: 10.1007/s11695-009-9895-6. [DOI] [PubMed] [Google Scholar]
- 14.Brolin RE, Kenler HA, Gorman RC, Cody RP. The dilemma of outcome assessment after operations for morbid obesity. Surgery. 1989;105:337–46. [PubMed] [Google Scholar]
- 15.Reinhold RB. Critical analysis of long term weight loss following gastric bypass. Surg Gynecol Obstet. 1982;155:385–94. [PubMed] [Google Scholar]
- 16.Christou NV, Look D, Maclean LD. Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 2006;244:734–40. doi: 10.1097/01.sla.0000217592.04061.d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gagner M, Gumbs AA. Gastric banding: Conversion to sleeve, bypass, or DS. Surg Endosc. 2007;21:1931–5. doi: 10.1007/s00464-007-9539-7. [DOI] [PubMed] [Google Scholar]
- 18.Slegtenhorst BR, van der Harst E, Demirkiran A, de Korte J, Schelfhout LJ, Klaassen RA. Effect of primary versus revisional Roux-en-Y gastric bypass: Inferior weight loss of revisional surgery after gastric banding. Surg Obes Relat Dis. 2013;9:253–8. doi: 10.1016/j.soard.2012.01.022. [DOI] [PubMed] [Google Scholar]
- 19.Mor A, Keenan E, Portenier D, Torquati A. Case-matched analysis comparing outcomes of revisional versus primary laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2013;27:548–52. doi: 10.1007/s00464-012-2477-z. [DOI] [PubMed] [Google Scholar]
- 20.Hii MW, Lake AC, Kenfield C, Hopkins GH. Laparoscopic conversion of failed gastric banding to Roux-en-Y gastric bypass: Short-term follow-up and technical considerations. Obes Surg. 2012;22:1022–8. doi: 10.1007/s11695-012-0594-3. [DOI] [PubMed] [Google Scholar]
- 21.Hamdi A, Julien C, Brown P, Woods I, Hamdi A, Ortega G, et al. Midterm outcomes of revisional surgery for gastric pouch and gastrojejunal anastomotic enlargement in patients with weight regain after gastric bypass for morbid obesity. Obes Surg. 2014;24:1386–90. doi: 10.1007/s11695-014-1216-z. [DOI] [PubMed] [Google Scholar]
- 22.Zingg U, McQuinn A, DiValentino D, Kinsey-Trotman S, Game P, Watson D. Revisional vs.primary Roux-en-Y gastric bypass – A case-matched analysis: Less weight loss in revisions. Obes Surg. 2010;20:1627–32. doi: 10.1007/s11695-010-0214-z. [DOI] [PubMed] [Google Scholar]
- 23.Westling A, Ohrvall M, Gustavsson S. Roux-en-Y gastric bypass after previous unsuccessful gastric restrictive surgery. J Gastrointest Surg. 2002;6:206–11. doi: 10.1016/s1091-255x(01)00035-x. [DOI] [PubMed] [Google Scholar]
- 24.de Csepel J, Nahouraii R, Gagner M. Laparoscopic gastric bypass as a reoperative bariatric surgery for failed open restrictive procedures. Surg Endosc. 2001;15:393–7. doi: 10.1007/s004640000347. [DOI] [PubMed] [Google Scholar]
- 25.Hallowell PT, Stellato TA, Yao DA, Robinson A, Schuster MM, Graf KN. Should bariatric revisional surgery be avoided secondary to increased morbidity and mortality? Am J Surg. 2009;197:391–6. doi: 10.1016/j.amjsurg.2008.11.011. [DOI] [PubMed] [Google Scholar]
- 26.Jennings NA, Boyle M, Mahawar K, Balupuri S, Small PK. Revisional laparoscopic Roux-en-Y gastric bypass following failed laparoscopic adjustable gastric banding. Obes Surg. 2013;23:947–52. doi: 10.1007/s11695-013-0888-0. [DOI] [PubMed] [Google Scholar]
- 27.Martin MJ, Mullenix PS, Steele SR, See CS, Cuadrado DG, Carter PL. A case-matched analysis of failed prior bariatric procedures converted to resectional gastric by-pass. Am J Surg. 2004;187:666–70. doi: 10.1016/j.amjsurg.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 28.te Riele WW, Sze YK, Wiezer MJ, van Ramshorst B. Conversion of failed laparoscopic gastric banding to gastric bypass as safe and effective as primary gastric bypass in morbidly obese patients. Surg Obes Relat Dis. 2008;4:735–9. doi: 10.1016/j.soard.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Zhang L, Tan WH, Chang R, Eagon JC. Perioperative risk and complications of revisional bariatric surgery compared to primary Roux-en-Y gastric bypass. Surg Endosc. 2015;29:1316–20. doi: 10.1007/s00464-014-3848-4. [DOI] [PubMed] [Google Scholar]
- 30.Owens BM, Owens ML, Hill CW. Effect of revisional bariatric surgery on weight loss and frequency of complications. Obes Surg. 1996;6:479–84. doi: 10.1381/096089296765556377. [DOI] [PubMed] [Google Scholar]
- 31.Brolin RE, Cody RP. Weight loss outcome of revisional bariatric operations varies according to the primary procedure. Ann Surg. 2008;248:227–32. doi: 10.1097/SLA.0b013e3181820cdf. [DOI] [PubMed] [Google Scholar]
- 32.Brethauer SA, Kothari S, Sudan R, Williams B, English WJ, Brengman M, et al. Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg Obes Relat Dis. 2014;10:952–72. doi: 10.1016/j.soard.2014.02.014. [DOI] [PubMed] [Google Scholar]


