Abstract
Objective:
To replicate an existing electronic consultation (eConsult) service in a new jurisdiction to test its generalizability.
Methods:
We conducted a cross-sectional study of all eConsults submitted by providers in the region of Mississauga Halton, Ontario, between January 5, 2015, and May 31, 2016. We compared our results to those from the original pilot in Eastern Ontario. The RE-AIM model served as our study framework.
Results:
Providers submitted 594 patient cases to 46 different specialty groups during the study period. Specialists responded in a median of 1.1 days, with 75% of cases answered within four days. Providers rated the service as having high or very high value for themselves and their patients in 92% of cases. The service yielded a net program cost of $10,321.56.
Conclusion:
Our findings resembled those of the initial implementation, though with a faster rate of uptake and lower cost because of the avoidance of start-up and administrative costs.
Abstract
Objectif:
Reproduire la mise en place d'un service de consultation en ligne existant dans une nouvelle région et en évaluer la généralisabilité.
Méthode:
Nous avons mené une étude transversale de toutes les consultations en ligne effectuées par les fournisseurs dans la région de Mississauga Halton, en Ontario, entre le 5 janvier 2015 et le 31 mai 2016. Nous avons comparé nos résultats à ceux du projet pilote initial dans l'Est ontarien. Le modèle RE-AIM a servi de cadre de travail pour notre étude.
Résultats:
Les fournisseurs ont présenté 594 cas à 46 groupes de diverses spécialités au cours de la période à l'étude. Le temps médian de réponse des spécialistes est de 1,1 jour, et 75 % des cas ont reçu une réponse en moins de quatre jours. Les fournisseurs ont accordé aux services les cotes « grande utilité » et « très grande utilité » pour eux-mêmes et leurs patients dans 92 % des cas. Le coût net du programme généré par le service s'élève à 10 321,56 $.
Conclusion:
Nos résultats ressemblent à ceux observés lors de la mise en œuvre initiale, quoiqu'avec un taux d'adhésion plus rapide et des coûts moindres en raison d'une diminution des frais de lancement et des frais administratifs.
Background
Scaling up healthcare innovations can be challenging. Many programs fail to realize their potential in “real world” settings as the evidence supporting their effectiveness often does not account for local contexts, which can be crucial to successful replication. This is especially true of eHealth solutions, which are often created without a nuanced understanding of the problems they seek to address (Ammenwerth et al. 2006). Neglecting these factors can result in costly failures. This was seen in the UK, where the National Health Service invested in an initiative providing physicians with a suite of health information technologies. Despite an investment of billions of dollars, 98% of the purported benefits of many programs have not been achieved (National Audit Office 2013). Similar failures have been reported in other health systems (Johnson 2010) including Canada's (Liddy et al. 2015b).
Since 2008, our team has been addressing the issue of excessive wait times for accessing specialist care, which is a significant problem facing many healthcare systems worldwide, including Canada's (CIHI 2017; Globerman et al. 2015; Viberg et al. 2014). A report by the Fraser institute found that patients wait a median of 18.3 weeks between being referred to a specialist and receiving treatment, an increase of 97% from 1993. Median wait times vary widely by region, from 13.6 weeks in Saskatchewan to 43.1 weeks in Prince Edward Island (Barua 2015). These waits exceed the duration deemed reasonable by many clinicians and have serious real-world consequences, resulting in worse health outcomes, proliferation of chronic disease, burdensome costs from missed work and higher mortality rates (Barua 2015; Barua et al. 2014).
To this end, we launched the Champlain BASE™ (Building Access to Specialists through eConsultation) eConsult service in the Champlain Local Health Integration Network (LHIN), a health region situated in the easternmost part of Ontario. The eConsult service is a secure web-based platform that facilitates communication between primary care providers (PCPs) and specialists. PCPs submit a patient-specific question to one of 95 different specialty groups and receive a reply within one week. Two-thirds of cases are resolved without the patient requiring a face-to-face specialist visit. The eConsult service's effectiveness at reducing wait times, high levels of patient and provider satisfaction, and ability to lower costs for care have been described in previous studies using a range of methods, including cross-sectional analyses of usage data and close-out survey responses, thematic analyses and costing evaluations (Keely et al. 2013; Liddy et al. 2013a, 2013b, 2015a, 2016, 2017a).
Having successfully implemented the eConsult service in our health region, our team has begun exploring its implementation in new jurisdictions across Canada. However, prior to a broad expansion to new provinces and territories, it was necessary to explore and verify the service's generalizability on a smaller scale. We thus sought to replicate the eConsult service in the Mississauga Halton LHIN, another Ontario health region situated in the province's southwest.
In this study, we examined the process of implementing eConsult in Mississauga Halton and evaluated its adoption rates, utilization and impact using the RE-AIM model developed by Glasgow and colleagues (1999). By exploring the implementation process in a new jurisdiction, we identified the critical success factors needed to support the successful adoption of eConsult services.
Methods
Setting
The Mississauga Halton LHIN is one of Ontario's 14 health regions. Located to the southwest of Toronto, it covers approximately 900 square kilometres and is home to over 1.2 million residents (Mississauga-Halton LHIN 2016). Two hospital corporations spanning six sites provide many of the specialty services to people living throughout the region.
Intervention/eConsult service model
The Champlain BASE™ eConsult service was designed by clinicians as a solution to excessive wait times for specialist care, based on the specific needs determined by patients and their PCPs (Keely et al. 2013; Liddy et al. 2013a, 2013b). The eConsult service was built on an existing web-based platform supported by the Champlain LHIN and hosted within the secure infrastructure of the Winchester District Memorial Hospital, ensuring adherence to provincial privacy policies. Cases begin when the PCP (a family physician or nurse practitioner) sends a question to a selected specialty. Specialists are notified by e-mail and respond to the question within one week with advice for care, a recommendation for referral or a request for more information. PCPs ultimately decide how to apply the specialist's suggestion and when the case can be deemed complete. Upon closing the case, PCPs complete a brief survey assessing the outcome and value of the service. Specialists are generally compensated on a pro-rated hourly basis (Liddy et al. 2013a, 2013b), although some are salaried and do not receive any additional compensation. Funding for the physician compensation is provided through the provincial Ministry of Health. PCPs are not remunerated directly from the service, though family physicians in Ontario are eligible for compensation based on an e-Consult billing code (JCL Medical Systems 2016).
Organization of specialty services
At the time of this study, a comprehensive, multispecialty eConsult service with access to 67 different specialty groups from within the Champlain LHIN was made available to participants from Mississauga Halton. One of the study's goals was to leverage specialists in one jurisdiction to help address the needs of PCPs in another, while simultaneously building a local base of specialists. Specialists from the Mississauga Halton LHIN were added to the service based on requests from the PCPs as well as the specialists' interest and availability. For some specialty groups, the service included specialists located in both the Champlain and Mississauga Halton LHINs. In a few cases, specialty groups in Mississauga Halton not previously available in the Champlain LHIN were formed and began serving the broader community (geriatrics, general surgery and cancer screening).
PCP recruitment
PCPs were recruited into the study via the Ontario Provincial eConsult Initiative developed in partnership between several provincial organizations, including Ontario MD, the Ontario Ministry of Health and Long-Term Care (MOHLTC), the Ontario Telemedicine Network and the Mississauga Halton and Champlain LHINs (Keller 2015). The initiative's goal was to provide access to three different online eConsult technology platforms, one of which was the Champlain BASE™ eConsult service. Mississauga Halton chose to receive the Champlain BASE™ model of care. The official date of the provincial initiative was January 5, 2015, although a small number of users (n = 13) registered for our service prior to the provincial launch, as a result of physician engagement activities during a ramp-up phase. The majority of users were engaged and registered during the first year of the provincial initiative through the Mississauga Halton Primary Care Advisor (PCA) team. PCAs are individuals who promote LHIN-wide programs and initiatives to support the advancement of primary care engagement across all service providers (Burden 2016). In the context of the present study, the recruitment typically consisted of PCAs visiting and/or communicating with the local primary care clinics on various topics, including eConsult, and connecting the eConsult support team with interested PCPs for further instructions and orientation to the service.
Evaluation framework
For this study, we evaluated all cases completed by PCPs in Mississauga Halton between January 5, 2015, and May 31, 2016. We used the RE-AIM framework created by Glasgow et al. (1999) to evaluate the service's implementation. The RE-AIM framework proposes that the translatability and public health impact of an initiative is best evaluated by examining its: (1) reach into the target population; (2) effectiveness or efficacy; (3) adoption by target settings, institutions and staff; (4) implementation, including its consistency and costs of delivery; and (5) maintenance of intervention effects in individuals and settings over time. To assess these dimensions, we examined the data routinely collected by the system. PCPs' responses to the mandatory close-out survey were used to determine (1) whether using eConsult resulted in PCPs choosing a new course of action for treatment and (2) whether a face-to-face consultation was originally contemplated and/or ultimately recommended. We compared our results to those obtained during the pilot phase of the service in the Champlain LHIN (Keely et al. 2013). Given that eConsult is a health system-level innovation, we chose to examine its effectiveness/efficacy on four key dimensions of care outlined by the Quadruple Aim framework developed by Bodenheimer and Sinsky: population health, patient experience, provider experience and cost (Bodenheimer and Sinsky 2014). Since assessing eConsult's impact on population health outcomes in the early pilot stages was not possible due to low case volumes, we focused on quality of care outcomes related to the attainment of timely and appropriate healthcare, which by the Institute of Medicine definitions reflect the degree to which healthcare services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge (Institute of Medicine [US] 2001). Our key outcomes included the timeliness of access to specialist expertise and the effect on PCPs' course of action, including the need for face-to-face visits.
Table 1 provides definitions for the five RE-AIM dimensions and lists the questions we used to guide our assessment of eConsult's implementation in Mississauga Halton.
Table 1.
A description of the five dimensions of care outlined by the RE-AIM framework
| RE-AIM dimension | Definition | Questions specific to eConsult evaluation |
|---|---|---|
| Reach into the target population | The absolute number, proportion and representativeness of individuals who are willing to participate in a given initiative, intervention or program. | What was the absolute number and proportion of patients reached and served via eConsult service? Which patients were reached in terms of the breadth of specialties accessed through the eConsult service? |
| Effectiveness or efficacy | The impact of an intervention on important outcomes, including potential negative effects, quality of life and economic outcomes. | What was the impact of eConsult on the key areas to care quality: population health, patient experience, provider experience and cost? |
| Adoption by target settings, institutions and staff | The absolute number, proportion, and representativeness of settings and intervention agents (people who deliver the program) who are willing to initiate a program. | What was the uptake of the eConsult service (absolute number, regional proportion, monthly growth over time) among the PCP population in MH LHIN? What was the uptake/participation among the specialists/specialty groups from the MH LHIN? |
| Implementation consistency, costs and adaptions made during delivery | The consistency and fidelity to the program protocol, the costs and adaptations made during delivery. | What was the fidelity to the essential steps (Liddy et al. 2013b) (including establishing partnerships, addressing privacy issues, physician engagement and payment) previously described as necessary for replication of eConsult platform in other health regions? |
| Maintenance of intervention effects in individuals and settings over time | The extent to which a program or policy becomes institutionalized or part of the routine organizational practices and policies. | What is the ongoing usage of eConsult? What were the reinforcing factors required to maintain the eConsult service? |
MH LHIN = Mississauga Halton Local Health Integration Network; PCP = primary care provider.
Results
Reach
The eConsult service demonstrated greater reach during its implementation in the Mississauga Halton LHIN than it did in the Champlain LHIN during an equivalent period. PCPs in the Mississauga Halton LHIN completed 594 eConsults during the study period compared to 451 in the Champlain LHIN (Figure 1a). The monthly volume of cases also grew more rapidly in the Mississauga Halton LHIN than they had in the Champlain LHIN (Figure 1b). When expressed as population rates, PCPs completed 0.36 eConsults per 1,000 people in the Mississauga Halton LHIN during the first year of implementation compared to 0.16 eConsults per 1,000 people in the Champlain LHIN (Statistics Canada 2011).
Figure 1.

eConsult case volume - Number of cases completed per month and cumulative total in MH LHIN (a) and Champlain LHIN (b)
LHIN = Local Health Integration Network; MH = Mississauga Halton.
The breadth of specialties accessed by patients from the Mississauga Halton LHIN is shown in Figure 2. The most commonly accessed specialties were dermatology (18% of cases), obstetrics/gynecology (OBS/GYN) (9%), hematology (7%), endocrinology (7%) and cardiology (6%).
Figure 2.

Specialty distribution: eConsult cases submitted to all specialties
ENT = ear, nose and throat; OBS/GYN = obstetrics and gynecology. *30 different specialties for a total of 16.3% of all cases submitted.
Effectiveness
We used the Quadruple Aim model as a lens to view the different elements of effectiveness (Bodenheimer and Sinsky 2014).
Population health
Specialists provided an initial response to PCP questions in a median of 1.1 days, with 75% of eConsults answered within 4.2 days. In 5% of cases (29/594), the specialists took longer to respond than the prescribed 7-day response period. PCPs closed eConsult cases (e.g., received and read response and answered close-out survey) in a median of 5.3 days, with 75% of cases completed within 13.2 days.
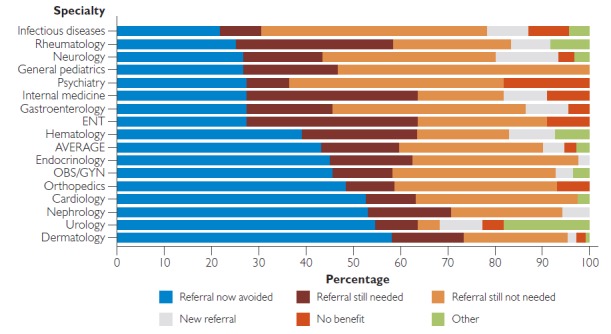
PCPs received advice on a new or additional course of action in 51% of cases, and confirmed their original course of action in 44% (Figure 3). Only 3% of responses were deemed not to be useful. In 40% of cases, a referral was originally contemplated but ultimately avoided. In 32% of cases, a referral was not originally contemplated and was still not needed. Overall, 72% of all completed cases did not require a face-to-face visit.
Figure 3.

Impact of eConsult on the course of action by the PCP by specialty service (for specialty groups with 10 or more completed cases; N = 497)
ENT = ear, nose and throat; PCP = primary care provider; OBS/GYN = obstetrics and gynecology.
These numbers varied across specialty groups. For dermatology, urology, nephrology, and cardiology, over 50% of the cases would have required a face-to-face consultation if eConsult was not available (Figure 4). In 18% of cases, a referral was originally contemplated and was still needed, but the PCP perceived that eConsult would lead to a more effective specialist visit. In 5% of cases, a referral was not originally contemplated, but eConsult process resulted in a referral being initiated (Figure 4). The latter is an example of an unintended consequence of the service with a potential impact on improved patient safety, as delayed referrals can have significant consequences (Liddy et al. 2016, 2017a). This finding was also observed in the Champlain LHIN, albeit to a slightly lower extent (3% of cases). Overall, these results were very similar to those obtained in Champlain LHIN (Keely et al. 2013).
Figure 4.
Impact of eConsult on need for face-to-face referral by specialty service (for specialty groups with 10 or more completed cases; N = 497)
ENT = ear, nose and throat; OBS/GYN = obstetrics and gynecology.
Patient and provider experience
The close-out survey includes a question to PCPs on their perceived value of the service for their patients, which we used as a proxy measure of patient satisfaction. On a five-point Likert scale, PCPs rated the eConsult service's value to their patients as four or five (indicating good or excellent) in 92% of cases. Using the same scale, PCPs likewise rated the service's value for themselves as four or five in 92% of cases. In the free-text portion of the survey, PCPs frequently cited the speed of responses, quality of advice, capacity for improving patient care and educational opportunities as its chief benefits. These results mirror those obtained in Champlain LHIN (Keely et al., 2013).
Cost
The delivery costs of the eConsult service in the Mississauga Halton LHIN during the study period amounted to $7,616.33 (Table 2). These included user set-up and registration, user support and variable administration costs. Consultation-specific costs included $27,283.33 for specialist remuneration and $113.85 in assignment costs. The costs of referrals initiated as a result of the eConsult amounted to $3,811.00. The total costs of eConsult service came to $38,824.51, not including the fixed administration costs, which are incurred regardless of the Mississauga Halton LHIN eConsults. A total of 237 specialist visits were avoided due to eConsult, resulting in savings of $28,502.95. The net program costs were $10,321.56.
Table 2.
Total costs and total savings of using eConsult by Mississauga Halton LHIN PCPs during the study period
| Item | Value ($) |
|---|---|
| Costs | |
| Delivery costs | 7,616.33 |
| User set-up/registration/training | 5,002.36 |
| Support | 2,568.43 |
| Administration | 45.54 |
| Consultation-specific costs | 27,397.18 |
| Specialist remuneration | 27,283.33 |
| Assignment | 113.85 |
| Added referrals | 3,811.00 |
| Total | 38,824.51 |
| Savings | |
| Avoided referrals | 28,502.95 |
| Total | 28,502.95 |
| Net costs | 10,321.56 |
Using these costs, we calculated the average cost per eConsult for each specialty that received over 10 cases during the study period (Table 3). Across all of these specialty groups, each eConsult case cost an average of $47.38.
Table 3.
Average specialist self-reported times to complete eConsult and average remuneration costs by specialty (for specialty groups with 10 or more completed cases; N = 497)
| Specialty | n | Average time to complete (minutes) | Average specialist cost per eConsult ($) |
|---|---|---|---|
| Dermatology | 105 | 14.29 | 47.62 |
| Obstetrics and gynecology | 55 | 13.00 | 43.33 |
| Hematology | 41 | 13.78 | 45.93 |
| Endocrinology | 40 | 11.38 | 37.92 |
| Cardiology | 38 | 11.84 | 39.47 |
| General pediatrics | 30 | 12.00 | 40.00 |
| Neurology | 30 | 10.50 | 35.00 |
| Orthopedics | 29 | 19.83 | 66.09 |
| Infectious diseases | 23 | 13.91 | 46.38 |
| Gastroenterology | 22 | 17.95 | 59.85 |
| Urology | 22 | 15.68 | 52.27 |
| Nephrology | 17 | 18.24 | 60.78 |
| Rheumatology | 12 | 14.58 | 48.61 |
| Ear, nose and throat specialist | 11 | 10.45 | 34.85 |
| Internal medicine | 11 | 14.09 | 46.97 |
| Psychiatry | 11 | 15.91 | 53.03 |
Adoption
In the Mississauga Halton LHIN, 133 family doctors and 12 nurse practitioners registered for the eConsult service over the course of the study, representing 13.2% of all family physicians (Gall 2015) and 11% of nurse practitioners (College of Nurses of Ontario 2015) practicing in the region (Figure 5a). The monthly growth rate was more robust than the one observed during the initial pilot phase of the service in the Champlain LHIN (Figure 5b), ultimately leading to greater number of PCPs reached over a time period of the same duration (145 vs. 103). Of the PCPs who registered with the service, 47% (n = 68) submitted at least one eConsult (with a median of four cases). This result is similar to the Champlain LHIN pilot data, where 48% of the PCPs who registered for the service were found to complete at least one eConsult (with a median of five cases) (Keely et al. 2013).
Figure 5.

PCP engagement - Number of new PCPs per month and cumulative total in MH LHIN (a) and Champlain LHIN (b)
LHIN = Local Health Integration Network; MH = Mississauga Halton; PCP = primary care provider.
On a setting level, eConsult was adopted by individual PCPs from 78 clinics in 10 cities/towns across the Mississauga Halton LHIN. The majority of clinics were located in Mississauga (53%), followed by Oakville (14%), Georgetown (13%), Milton (10%) and Etobicoke (4%). Other cities represented by individual clinics included Acton, Brampton, Burlington, Toronto and Woodbridge. All clinics were urban or suburban. Sixty-one (78%) were group physician practices, of which seven were Family Health Teams. There were also individual clinics belonging to the following models: Community Health Centre, Community Care Access Centre, Family Health Organization, Family Health Group and Family Medicine Teaching Unit. Sixty-nine clinics (89%) used electronic medical records.
During the study period, 15 specialists working in the Mississauga Halton LHIN registered with the eConsult service, one of whom withdrew due to a heavy workload. The remaining 14 specialists represented 13 specialty groups, which were gradually established over the study period. A similar number of specialty groups (n = 16) were established in the Champlain LHIN during the equivalent time period (Keely et al. 2013).
Three groups represented by Mississauga Halton specialists (geriatrics, general surgery and cancer screening) constituted new specialty groups previously not available via the eConsult service. This is an example of reciprocal leveraging of specialty expertise between jurisdictions to meet specific needs and gaps in specialty care. All Mississauga Halton specialists made themselves available to answer queries from PCPs outside of their LHIN. In cases where a particular specialty group already existed in the Champlain BASE™ service, the Mississauga Halton LHIN specialists were available to answer local eConsult cases for Mississauga Halton as well as cover for the other specialists from Champlain LHIN as necessary (e.g., during vacations).
Implementation
When planning implementation in Mississauga Halton, we consulted the 10 steps that we established in a previous paper based on our experiences in the Champlain LHIN: (1) identify your partners, (2) choose your platform, (3) start as a pilot project, (4) design your product, (5) ensure patient privacy, (6) think through the process, (7) foster relationships with your participants, (8) be prepared to provide physician payment, (9) provide feedback and (10) plan the transition from pilot to permanency (Liddy et al. 2013b). Many of these steps (e.g., choosing a platform, designing a product, ensuring patient privacy) required little additional work, as we were able to build on our existing eConsult platform. Others (e.g., identifying partners, planning for transition from pilot to permanency) required consideration to adjust to this new context.
The eConsult service was implemented in the Mississauga Halton LHIN under the context of a focused LHIN-wide and MOHLTC-led provincial eConsult initiative. This enabled greater support associated with planning, launching and maintaining an eConsult platform (e.g., Primary Care Advisor staffing and assistance in the recruitment of users) and helped to keep the focus on innovation and continued development of the service based on regional needs. The key adaptation was the fact that as a region, the Mississauga Halton LHIN was not required to set up its own platform but could instead leverage the existing service available in the Champlain LHIN. This adaptation came with several advantages, including immediate access to a wide group of specialty groups (67 at the start and 86 by the end of the study period) and avoidance of the start-up costs and certain fixed administration costs necessary to support the service. Finally, since the Champlain and Mississauga Halton LHINs are located in Ontario, provincial policies related to privacy requirements, sources and levels of payment for users of the service and rules regarding interjurisdictional collaboration that could potentially impact the service's ability to support the provision of care were the same in both jurisdictions.
Maintenance
The Ontario MOHLTC continues to support the eConsult service in Mississauga Halton, while the provincial adoption of eConsult is being planned with the partners involved in this provincial initiative. The province has specifically identified greater access to specialist care as a main objective in recent health planning with the Patients First Act emphasizing the need to improve access and continuity of care (MOHLTC 2016). Operations, governance, sustainable payment models and quality assurance are key aspects that are under discussion. These actions demonstrate an understanding of the importance of wait times as a determinant of care outcomes, and speak to ongoing support for eConsult. In the meantime, the service continues to grow, and the data we collect directly from users (PCPs and specialists) reflect its consistently high levels of efficacy and satisfaction (Liddy et al. 2015a; Keely et al. 2015). Recent efforts at expansion include partnership with the Canadian Foundation for Healthcare Improvement, who selected Champlain BASE™ as one of two innovative services to implement among 10 improvement teams across Canada (CFHI 2017). Furthermore, the Government of Ontario has announced a plan to expand the eConsult service across Ontario and allocated $10 million in their 2017 budget for this and other innovations targeting wait times for specialist care (Government of Ontario 2017).
Discussion
We have successfully implemented the Champlain BASE™ eConsult service in another health region in Ontario, thus demonstrating the model's generalizability. Using the RE-AIM framework, we compared specific aspects of the implementation process between the two regions. Compared to the original site, implementation in the Mississauga Halton LHIN demonstrated more rapid adoption by PCPs and a greater reach as reflected by monthly eConsult case volumes. Enrolment reached an initial peak in the Mississauga Halton LHIN at month nine (September 2015), whereas the Champlain LHIN exhibited a similar trend later in the process, during months 14–15 (May and June, 2012). This most likely reflects the different recruitment approaches in both regions, with a focused LHIN-wide and MOHLTC-led provincial eConsult initiative in the Mississauga Halton LHIN versus a slower and more organic implementation in the Champlain LHIN initially supported only by limited research funding. The early service also provided access to a smaller menu of specialty services during its initial implementation, which could contribute to the smaller number of cases processed. In both LHINs, 40% cases had PCPs originally contemplating referrals, but ultimately avoiding them based on specialists' advice. Participating PCPs considered the service to have high value for themselves and their patients in nearly all cases—an important finding, given that provider experience has been shown to have a substantial impact on adoption of new technologies (Bodenheimer and Sinsky 2014). While PCPs in the Mississauga Halton LHIN had access to specialists in the Champlain LHIN, specialists from within the region ultimately joined the service as well. This uptake demonstrates that although it is beneficial to leverage specialists from the local region, doing so is not required for a successful service. The potential system level impact is significant with eConsult not only from an improved patient access perspective where specialist advice is available in days instead of months of waiting, but also from an efficiency and cost savings lens (Wasfy et al. 2016; Liddy et al. 2016, 2017a). In terms of cost-effectiveness, the service was shown to cost a weighted average of $47.35 per case across specialty groups, versus $133.60 per case for traditional referrals. Additional savings were evident when accounting for societal costs, such as patient travel, lost wages/productivity associated with face-to-face specialist visits, avoided tests and potential improved health outcomes associated with shorter wait times (Liddy et al. 2016, 2017a). Recent work has also shown that cost savings per case of $1,100.93 for patients from remote communities when considering indirect costs such as travel and time off work saved with an avoided face-to-face visit because of eConsult access (Liddy et al. 2017b).
An extensive body of literature stemming from the seminal work by Rogers and colleagues has identified the following five attributes as critical to facilitating adoption of innovations: relative advantage, low complexity, compatibility, observability and trialability (Rogers 2003). Innovations that have a clear, unambiguous advantage in either impact or cost-effectiveness are more easily adopted and implemented. The starting point for our eConsult service was (and remains) the tremendous problem of excessive wait times and the associated burden that falls onto the PCP, which the traditional model of referral-consultation often fails to address. Synchronous telemedicine systems (e.g., video conferencing) can link providers in real time, but face a number of challenges in terms of infrastructure requirements and scheduling. Video conferencing services require high-speed broadband connectivity in order to function, limiting their effectiveness in many rural communities (where internet access remains limited even today), despite the fact that these communities are often most in need of improved access to care (Linkous et al. 2012). By embracing a low-complexity solution, eConsult greatly reduces the minimum technology required for use—requiring minimal bandwidth and running on any device with an internet browser—and removes the challenges associated with coordinating PCPs and specialists to meet remotely. Furthermore, innovations that are compatible with the intended users' values, norms and perceived needs are more readily adopted. The eConsult service demonstrates this compatibility, as evidenced by interviews with providers (Liddy et al. 2015a; Keely et al. 2015). For instance, a survey of participating specialists found that 94% believe eConsult improves their communication with PCPs (Keely et al. 2015), whereas a review of PCP survey comments revealed high satisfaction with eConsult's impact on access, care quality and continuity of care (Liddy et al. 2015a). Lastly, the eConsult service's benefits have a high degree of observability, meaning they can be quickly and easily perceived by adopters. As PCPs who use eConsult are directly involved with the cases they submit, they are immediately aware of response times and whether a referral they had originally planned to make could now be avoided based on the advice they received from the specialist—an outcome that occurs in over 40% of cases (Keely et al. 2013). This high level of observability is reflected in the close-out surveys, which have repeatedly shown that PCPs rank eConsult as having high/very high value in over 90% of cases (Keely et al. 2013; Liddy et al. 2015a)
In addition to the attributes identified by Rogers, Greenhalgh et al. (2004) argued that a receptive context facilitates adoption of innovations. The MOHLTC-led provincial eConsult initiative played a significant role in setting a receptive structural and organizational context for adoption of the eConsult service in the Mississauga Halton LHIN. Furthermore, other studies have emphasized that the ease with which technological innovations integrate into existing workflows plays a key role in determining their success (Bates et al. 2003; Gagnon et al. 2009). The eConsult service was designed to accommodate different workflows and can be adopted by new users with only a minimal amount of training.
We have previously identified the following 10 essential steps for replication of eConsult in a new region: partners, platform, piloting, product, privacy, process, participants, payment, providing feedback and planning for sustainability (Liddy et al. 2013b). We successfully aligned with local priorities through collaborative partnerships with regional stakeholders, and obtained support for local staffing through MOHLTC and a strong focus on physician end-user engagement throughout the process. We capitalized on existing technology infrastructure by using platforms hosted jointly by the Champlain LHIN and Winchester District Memorial Hospital, while leveraging a multitude of specialty services from the Champlain LHIN and integrating new local ones from the Mississauga Halton LHIN.
Limitations
The Mississauga Halton and Champlain LHINs are both in Ontario, which limits generalizability to within the province. The sample of providers from the Mississauga Halton LHIN was small and the policy context was the same in both regions, limiting implications for replication in other Canadian provinces or territories. The Ontario Provincial eConsult Initiative supported the service's implementation, but also allowed participants to choose other competing eConsult alternatives. It is not known if the population of users who picked Champlain BASE™ over the other eConsult options available through the provincial initiative differed from the rest of the population. Costing data were limited to case costs handled directly by the service and did not include in-kind services or costs shouldered by our partner organizations (e.g., PCAdvisors/marketing), and are thus not intended as a comprehensive list of costs associated with replicating an established service.
Conclusion
The Champlain BASE™ eConsult service was successfully replicated in the Mississauga Halton LHIN, demonstrating its generalizability. The specialist response times, referral avoidance, PCP satisfaction and costs associated with implementation were largely comparable to those seen in the Champlain LHIN during the service's initial rollout. We demonstrated that specialists could be effectively leveraged across jurisdictions to help address regional gaps in care, while supporting the development of a local base of specialists. The successful implementation was enabled by cultivating a receptive context and establishing key partnerships, building a service grounded in patient needs that offered an improvement over current referral processes, and leveraging a low cost simple technology solution.
Contributor Information
Clare Liddy, Clinician Investigator, C.T. Lamont Primary Health Care Research Centre, Bruyère Research Institute, Ottawa, ON.
Isabella Moroz, Research Associate, C.T. Lamont Primary Health Care Research Centre, Bruyère Research Institute, Ottawa, ON.
Amir Afkham, Senior Project Manager – Enabling Technologies, The Champlain Local Health Integration Network, Ottawa, ON.
Erin Keely, Chief, Division of Endocrinology and Metabolism, The Ottawa Hospital, Ottawa, ON.
References
- Ammenwerth E., Talmon J., Ash J., Bates D., Beuscart-Zephir M., Duhamel A. et al. 2006. “Impact of CPOE on Mortality Rates–Contradictory Findings, Important Messages.” Methods of Information in Medicine 45(6): 586–94. [PubMed] [Google Scholar]
- Barua B. 2015. Waiting Your Turn: Wait Times for Health Care in Canada. Vancouver, BC: Fraser Institute; Retrieved July 5, 2017. <https://www.fraserinstitute.org/sites/default/files/waiting-your-turn-2015.pdf>. [Google Scholar]
- Barua B., Esmail N., Jackson T. 2014. The Effect of Wait Times on Mortality in Canada. Vancouver, BC: Fraser Institute; Retrieved July 5, 2017. <https://www.fraserinstitute.org/sites/default/files/effect-of-wait-times-on-mortality-in-canada.pdf>. [Google Scholar]
- Bates D.W., Kuperman G.J., Wang S., Gandhi T., Kittler A., Volk L. et al. 2003. “Ten Commandments for Effective Clinical Decision Support: Making the Practice of Evidence-Based Medicine a Reality.” Journal of the American Medical Informatics Association 10(6): 523–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenheimer T., Sinsky C. 2014. “From Triple to Quadruple Aim: Care of the Patient Requires Care of the Provider.” Annals of Family Medicine 12(6): 573–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burden A. 2016. Primary Care Integration: Strategic Directions 2015–2020. Retrieved November 7, 2016. <http://healthcareathome.ca/mh/en/performance/Documents/MH CCAC overview of primary care integration in partnership with PCN and LHIN_2015_2016.pdf>.
- Canadian Foundation for Healthcare Improvement (CFHI). 2017. Connected Medicine: Enhancing Access to Specialist Consult e-Collaborative (Access to Specialist Consult). Retrieved July 12, 2017. <http://www.cfhi-fcass.ca/WhatWeDo/access>.
- Canadian Institute for Health Information (CIHI). 2017. How Canada Compares: Results from the Commonwealth Fund's 2016 International Health Policy Survey of Adults in 11 Countries. Retrieved July 7, 2016. <https://www.cihi.ca/sites/default/files/document/text-alternative-version-2016-cmwf-en-web.pdf>.
- College of Nurses of Ontario. 2015. LHIN Regional Summaries 2015: Mississauga Halton. Retrieved November 7, 2016. <http://www.cno.org/globalassets/2-howweprotectthepublic/statistical-reports/mississauga-halton-region-report-2015.pdf>.
- Gagnon M.-P., Légaré F., Labrecque M., Frémont P., Pluye P., Gagnon J. et al. 2009. “Interventions for Promoting Information and Communication Technologies Adoption in Healthcare Professionals.” Cochrane Library (1): CD006093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gall C. 2015. Strengthening Access, Performance and Accountability of Primary Health Care within the Mississauga Halton LHIN: Implementation Framework. Retrieved November 7, 2016. <https://www.oma.org/Resources/Documents/MHLHINImplementationPlan.pdf>.
- Glasgow R.E., Vogt T.M., Boles S.M. 1999. “Evaluating the Public Health Impact of Health Promotion Interventions: The RE-AIM Framework.” American Journal of Public Health 89(9): 1322–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Globerman S., Esmail N., Day B., Henderson D.R. 2015. Reducing Wait Times for Health Care – What Canada Can Learn from Theory and International Experience. Vancouver, BC: Fraser Institute; Retrieved July 5, 2017. <https://www.fraserinstitute.org/sites/default/files/reducing-wait-times-for-health-care.pdf>. [Google Scholar]
- Government of Ontario. 2017. Section A: Strengthening Health Care. Retrieved July 12, 2017. <http://www.fin.gov.on.ca/en/budget/ontariobudgets/2017/ch4a.html>.
- Greenhalgh T., Robert G., MacFarlane F., Bate P., Kyriakidou O. 2004. “Diffusion of Innovations in Service Organizations: Systematic Review and Recommendations.” Milbank Quarterly 82(4): 581–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (US). 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press. [PubMed] [Google Scholar]
- JCL Medical Systems. 2016. “E-Consultations: K738 and K739.” Retrieved November 10, 2017. <https://jclmedicalbilling.ca/ohip-billing-codes/e-consultations-k738-and-k739/>.
- Johnson C.W. 2010. Case Studies in the Failure of Healthcare Information Systems. Retrieved November 7, 2016. <http://www.dcs.gla.ac.uk/~johnson/papers/AHRQ/case_study.pdf>.
- Keely E., Liddy C., Afkham A. 2013. “Utilization, Benefits, and Impact of an e-Consultation Service across Diverse Specialties and Primary Care Providers.” Telemedicine Journal and E-Health 19(10): 733–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keely E., Drosinis P., Afkham A., Liddy C. 2015. “Perspectives of Champlain BASE Specialist Physicians: Their Motivation, Experiences and Recommendations for Providing eConsultations to Primary Care Providers.” Studies in Health Technology and Informatics 209: 38–45. [PubMed] [Google Scholar]
- Keller E. 2015. Show Me the Benefits: Clinicians Informing the eConsult Service for Ontario. Retrieved November 7, 2016. <https://infocentral.infoway-inforoute.ca/@api/deki/files/9268/=Elizabeth_Keller.pdf>.
- Liddy C., Afkham A., Drosinis P., Joschko J., Keely E. 2015a. “Impact and Satisfaction with a New eConsult Service: A Mixed Methods Study of Primary Care Providers.” Journal of the American Board of Family Medicine 28(3): 394–403. [DOI] [PubMed] [Google Scholar]
- Liddy C., Drosinis P., Deri Armstrong C., McKellips F., Afkham A., Keely E. 2016. “What Are the Cost Savings Associated with Providing Access to Specialist Care through the Champlain BASE eConsult Service? A Costing Evaluation.” BMJ Open 6(6): e010920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddy C., Drosinis P., Fogel A., Keely E. 2017a. “Prevention of Delayed Referrals through the Champlain BASE eConsult Service.” Canadian Family Physician 63(8): e381–86. [PMC free article] [PubMed] [Google Scholar]
- Liddy C., Hogel M., Blazhko V., Keely E. 2015b. “The Current State of Electronic Consultation & Electronic Referral Systems in Canada: An Environmental Scan.” Studies in Health Technology and Informatics 209: 75–83. [PubMed] [Google Scholar]
- Liddy C., Rowan M., Afkham A., Maranger J., Keely E. 2013a. “Building Access to Specialist Care through e-Consultation.” Open Medicine 7(1): e1–e8. [PMC free article] [PubMed] [Google Scholar]
- Liddy C., Maranger J., Afkham A., Keely E. 2013b. “Ten Steps to Establishing an e-Consultation Service to Improve Access to Specialist Care.” Telemedicine Journal and E-Health 19(12): 982–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddy C., McKellips F., Deri Armstrong C., Afkham A., Fraser-Roberts L., Keely E. 2017b. “Improving Access to Specialists in Remote Communities: A Cross-Sectional Study and Cost Analysis of the Use of eConsult in Nunavut.” Journal of Circumpolar Health 76(1): 1323493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linkous J., Capistrant G., Alverson D., Hirsch S., Manson S. 2012. “Challenges in Telehealth.” In Lustig T., ed., The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary (pp. 17–30). Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Ministry of Health and Long-Term Care (MOHLTC). 2016. Ontario Introduces Legislation to Further Improve Patient Access and Experience. Retrieved November 7, 2016. <https://news.ontario.ca/mohltc/en/2016/06/ontario-introduces-legislation-to-further-improve-patient-access-and-experience.html>.
- Mississauga-Halton LHIN. 2016. Mississauga-Halton LHIN Profile – Quick Facts 2016–2017. Retrieved November 7, 2016. <http://www.mississaugahaltonlhin.on.ca/resources/reportsandpublications.aspx>.
- National Audit Office. 2013. Review of the Final Benefits Statement for Programs Previously Managed under the National Programme for IT in the NHS. London, UK: NAO. [Google Scholar]
- Rogers E. 2003. Diffusion of Innovations. New York, NY: Free Press. [Google Scholar]
- Statistics Canada. 2011. NHS Profile, 2011. Retrieved November 7, 2016. <https://www12.statcan.gc.ca/nhs-enm/2011/dp-pd/prof/index.cfm?Lang=E>.
- Viberg N., Forsberg B., Borowitz M., Molin R. 2014. “International Comparisons of Waiting Times in Health Care–Limitations and Prospects.” Health Policy 112(1–2): 53–61. [DOI] [PubMed] [Google Scholar]
- Wasfy J.H., Rao S.K., Kalwani N., Chittle M.D., Richardson C.A., Gallen K.M. et al. 2016. “Longer-Term Impact of Cardiology e-Consults.” American Heart Journal 173: 86–93. [DOI] [PubMed] [Google Scholar]


