Abstract
Background and Objectives
Childhood maltreatment is related to alcohol use as well as psychological distress in young adulthood. Few studies have examined whether psychological distress mediates the relationship between child maltreatment and alcohol use. We examined the role of psychological distress in linking child maltreatment subtypes (ie, emotional abuse, physical abuse, sexual abuse, neglect) to four patterns of alcohol use, including frequency of alcohol use, binge drinking, alcohol-related problems, and alcohol dependence.
Methods
We used a community sample of young adults (N=337), who completed an interview assessing exposure to childhood maltreatment, current psychological distress, and drinking behaviors.
Results
Emotional abuse was associated with psychological distress, whereas psychological distress was related to more pathological drinking behaviors such as alcohol-related problems and alcohol dependence. Subsequent analyses indicated significant mediated effects between emotional abuse and alcohol-related problems and alcohol dependence via psychological distress, even after controlling for demographic factors, other maltreatment subtypes, parental alcoholism, and peer alcohol use.
Conclusions and Scientific Significance
Findings suggest that among four types of childhood maltreatment, emotional abuse might be the major driver of pathological drinking among child maltreatment victims. Interventions aimed at negative emotionality may be useful in preventing and treating problematic drinking among the victims of childhood emotional abuse.
INTRODUCTION
Alcohol use and misuse during young adulthood is a significant public health issue. In 2013, the majority (59.6%) of young adults aged 18–25 years consumed at least one drink in the past 30 d, whereas more than a third (37.9%) of young adults drank five or more drinks on the same occasion on at least 1 d in the past 30 d, which is often called binge drinking.1 Alcohol studies in the past two decades have identified a variety of correlates of young adult alcohol use, ranging from genetic, neurobiological, psychological, environmental, and cultural determinants.2–6 For example, emerging evidence points to exposure to adverse childhood experiences, including child abuse and neglect as significant susceptibility factors for alcohol use in later life.7 A large body of studies have shown that childhood maltreatment increases an individual’s risk for alcohol problems in young adulthood.8–11 Nevertheless, the processes linking child maltreatment to later alcohol use and abuse have received scant attention.
A few existing conceptual and empirical studies exploring potential mechanisms that may mediate the relationship between child maltreatment and alcohol use in later stages of life have paid an increasing attention to the role of psychological distress.12 Numerous studies have also found that victims of child maltreatment were more prone to negative emotionality and showed greater difficulties in dealing with psychological distress than non-maltreated individuals.13 For example, from a study of childhood sexual abuse-discordant pairs of twins, Nelson et al. (2002) discovered that the twin who reported sexual abuse was at substantially higher risk for major depression and anxiety than the twin with no history of sexual abuse.14 A meta-analysis of 16 epidemiological studies also found that childhood maltreatment was associated with an increased risk of depressive episodes.15 Existing literature, therefore, suggests that many victims of child maltreatment suffer from psychological distress, which might make them more liable to the development of alcohol use in young adulthood.
Previous research has indicated that psychological distress operates as a risk factor for alcohol use among young adults.16–18 Studies have specifically shown a positive association between internalizing negative emotional states such as depression and anxiety with alcohol use. Part of this association has been explained by both the tension reduction hypothesis and self-medication hypothesis, which states that people consume alcohol to temporarily reduce the intensity of negative emotional and affective states.19,20 Alcohol consumption may temporarily help regulate emotional distress by reducing both tension and negative effect.21 However, excessive alcohol use is likely to further worsen negative emotional states, thereby forming a vicious cycle of alcohol use and negative emotional states. The presence of an alcohol use disorder has been shown to double the risk of developing a major depressive episode.22 Furthermore, individuals with a history of both childhood trauma and alcohol use disorders experience alcohol cravings when exposed to trauma cues, suggesting that trauma cues and subsequent negative affect may reinforce alcohol use.23 There is also growing evidence that negative emotional states and alcohol use disorders share common psychobiological pathways.24 Despite indications that psychological distress might be the core factor underlying the negative effects of child maltreatment on alcohol use in young adulthood, it has received little attention. The present study examined the relative contribution of psychological distress to the development of alcohol use among child maltreatment victims.
Child maltreatment manifests in a variety of forms, including emotional, physical, and sexual abuse, and neglect, which have been all found to influence later alcohol use.8,25,26 For example, Moran et al.26 found that three forms of childhood abuse, including emotional abuse, physical abuse, and sexual abuse, were all associated with adolescent drinking frequency in a sample of 2,164 students in the 10th, 11th, and 12th grades, controlling for age, gender, and family configuration. Previous studies also suggest that the impact of child maltreatment on both psychological and alcohol use outcomes may depend on specific subtypes of maltreatment a child experienced. For example, in a study on 676 young adult victims of child maltreatment, Widom et al.8 found that individuals who experienced physical abuse or co-occurring physical and sexual abuse displayed an increased risk of lifetime depression, whereas those who experienced neglect had a greater risk for current depression. Exposure to sexual abuse in this study did not have an association with elevated risks of depression. Mullings et al.25 also reported that childhood neglect was associated with alcohol dependence, whereas physical or sexual abuse was not related to alcohol dependence. Further, exploring the relationship between child maltreatment and alcohol use, many studies have focused on alcohol use disorders (AUDs), but have neglected to examine the full spectrum of alcohol drinking behavior ranging from normal use to pathological use of alcohol.27,28 As psychological distress might particularly relate to certain stages of alcohol use, it is critical to include the heterogeneity of drinking behaviors, including frequency of alcohol use, binge drinking, alcohol-related problems, and alcohol dependence.
The literature also suggests that there are common risk factors for alcohol use in young adulthood, including age, gender, parental alcoholism, and peer alcohol use, which need to be included in alcohol research to adjust for potential genetic and social influences on alcohol use.5,29 For example, the heritability of alcohol dependence ranges between 30% and 70%.30 In an adult twin study, Kendler and co-workers found that the alcohol dependence risk associated with childhood maltreatment was mostly due to shared environmental factors between twins.11 Similarly, peer drinking has been shown to influence alcohol use.31 Examining data from 134 schools and 1,846 twin and sibling pairs, Cruz et al. found that peer use predicted increased drinking from adolescence into adulthood.31
The present study investigates the potential direct and indirect relationships between different types of childhood maltreatment, psychological distress, and alcohol drinking outcomes, controlling for demographic, environmental, genetic influences as well as other types of childhood maltreatment. The hypothesis of our study is that all maltreatment types and psychological distress will be positively associated with all alcohol-drinking types, and that psychological distress will mediate these associations.
METHODS
Procedures and Participants
Young adults (ages 18–25 years) were recruited to participate in our study through advertisements placed in a Northeastern metropolitan area. The recruitment advertisements entitled “Childhood Experiences and Later Development,” were placed in public areas such as bus stops, bulletin boards, and subway stations. Participants were included in the present study if they were between the ages of 18 and 25 years and did not indicate any major health concerns (eg, cancer, diabetes, other chronic/life-threatening illness) during the screening interview. The total sample included 337 young adults (mean age=21.7; SD=2.1 years; range 18–25). Each participant was provided with a complete description of the study conditions, including potential risks and benefits, after which written informed consent was obtained from all participants. The Institutional Review Board approved all study procedures.
Measures
Childhood Maltreatment
Exposure to maltreatment was evaluated using a computer-assisted self-interviewing (CASI) method of the Childhood Trauma Questionnaire (CTQ).32 The CTQ has 25 items that assesses four subtypes of maltreatment committed by parents, family members, and others: physical, sexual, and emotional abuse, and neglect. It evaluates how often each item is experienced prior to age 18 using a 5-point scale ranging from never true (1) to very often true (5; eg, “I was punished with a belt, a board, a cord, or some other hard object”).
The CASI method has been effective in obtaining accurate responses of previous exposure to child maltreatment and other sensitive behaviors such as substance use in young populations. Previous studies have validated the CTQ’s psychometric properties and demonstrated sufficient validity and reliability.33 For our study, internal consistencies of the CTQ are .89 (Cronbach’s α) for emotional abuse, .86 for physical abuse, .86 for sexual abuse, and .71 for neglect.
Psychological Distress
The Brief Symptom Inventory 18 (BSI-18) was used to assess psychological distress.34 The BSI-18 is a short form version of the BSI, and includes 18 items that evaluates certain features of psychological distress, including, somatization, depression, and anxiety (eg, how much ‘feeling fearful’ has distressed or bothered you during the past 7 days including today?). A higher BSI score indicated a higher level of psychological distress. Internal consistency of the BSI-18 in our sample was .93.
Alcohol Use
Frequency of monthly alcohol use in the past year was evaluated by the question, “In the past 12 months, on how many days did you drink alcohol per month?” In addition, past-year binge drinking was measured by the question, “Over the past 12 months, on how many days did you drink five (for males) or four (for females) or more alcoholic drinks on the same occasion?” Both items had response categories that ranged from 1 (everyday) to 7 (never). These items were reverse coded in the statistical models such that a higher score was indicative of more alcohol drinking. The present study defined binge drinking as consuming five or more drinks in a row for males and four or more drinks in a row for females, at least 2–3 d permonth within the past year (coded as “1”).35 Given the high prevalence of monthly alcohol use in our sample (ie, about 8 d per month on average), we used the binge drinking frequency of at least two to three times per months in defining binge drinking. Alcohol-related problems were assessed using the Rutgers Alcohol Problem Index (RAPI; 23 items; α=0.90), which provides a total negative alcohol-related consequences score, ranging from 0 to 69.36 Internal consistency of the RAPI for the current sample was .90. Next, lifetime alcohol dependence was assessed through the Composite International Diagnostic Interview (CIDI), which is based on the Diagnostic and Statistical Manual (DSM-IV) criteria for alcohol abuse and dependence. The presence of alcohol dependence was coded as “1.”
Peer Alcohol Use and Parental Alcoholism
Peer alcohol use was measured with questions examining the participant’s total number of close friends who currently drink alcohol. Finally, parental alcoholism was assessed using the Children of Alcoholics Screening Test-6 (CAST-6).37 The CAST-6 includes six items measuring offspring’s experiences related to a parent’s alcohol use (eg, have you ever thought that one of your parents had a drinking problem?). Internal consistency of the CAST-6 for our study sample was .91.
Demographic Information
Demographic information, including age, gender, and race/ethnicity, was assessed by using a self-reported structured questionnaire.
Data Analysis
To examine the measurement structures of psychological distress, we conducted exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). The relationships among each maltreatment subtype, psychological distress, and alcohol use were explored by conducting structural equation modeling (SEM) for each drinking behavior. Finally, we performed SEMs to examine the unique contribution of each maltreatment subtype on psychological distress and drinking behaviors by adjusting for the other types of maltreatment, demographic, parental alcoholism, and peer alcohol use variables. Maltreatment subtypes along with demographic variables, parental alcoholism, and peer alcohol use were specified to directly affect alcohol use variable and to indirectly affect it through the mediating variable, psychological distress. The indirect effect of maltreatment on alcohol use, via psychological distress, was calculated as the product of the coefficients of these relationships,38 and the standard errors of the indirect effects was calculated using the delta method.39 For each level of maltreatment, the percent mediation was determined by dividing the indirect effect by the total effect (the sum of the indirect and direct effects).40
We used the comparative fit index (CFI), root mean square error of approximation (RMSEA), standardized root mean-square residual (SRMR) for continuous outcomes (ie, drinking frequency and alcohol-related problems), and Weighted Root Mean Square Residual (WRMR) for categorical outcomes (ie, binge drinking and alcohol dependence) as standardized indices of model fit.41 Better fitting models will have higher CFI values (.95 or higher) and lower RMSEA (.06 or below), SRMR (.08 or below), and WRMR values (.09 or below).41,42 Demographic information, parental alcoholism, and peer drinking were entered into the models to determine relevant covariates. Mplus 7.0 was used for all analyses using maximum likelihood estimation for continuous outcomes and mean and variance-adjusted weighted least squares (WLSMV) estimator for categorical variables.43
RESULTS
Measurement Structure of Psychological Distress
Sample characteristics are presented in Table 1. Based on previous studies on the BSI-18, a CFA of 3-factor structure was conducted in which somatization, depression, and anxiety loaded onto psychological distress. As the 3-factor solution of psychological distress was not supported, we performed an EFA using the promax for oblique rotations to examine the measurement structure of the BSI-18 for the current sample. As preliminary analyses indicated somatization items had a low loading on the psychological distress (factor loadings from .01 to .39), somatization items were dropped from analysis. In addition, three items (feeling hopeless, nervousness, and suicidal thoughts) were also dropped due to low factor loadings. An EFA compared the fit of a model in which the indicators of psychological distress were specified as measuring two constructs with the fit of a model in which the indicators were all specified as measures of one construct. A 3-factor solution did not converge. Eigenvalues for the correlation matrix were 4.31, 1.06, and .70. The 2-factor solution had a significantly better fit (χ2 (19)=37.34, p<.001, CFI=.98, RMSEA=.05, SRMR=.02) than the 1-factor model (χ2 (27)=194.54, p<.001, CFI=.87, RMSEA=.14, SRMR=.07). Thus, a 2-factor solution with latent constructs representing depression and anxiety was selected. Finally, a CFA model for psychological distress was specified with four indicators of depression and five indicators of anxiety, which showed a satisfactory fit (χ2 (26)=55.10, p<.001, CFI=.98, RMSEA=.06, SRMR=.03).
TABLE 1.
Sample characteristics (N=337)
| Range | Mean (SD) or % (n) | |
|---|---|---|
| Demographics | ||
| Age* | 18–25 | 21.7 (2.1) |
| Gender | ||
| Male | 47.5 (160) | |
| Female | 52.5 (177) | |
| Race/ethnicitya | ||
| White | 55.7 (187) | |
| Black | 17.0 (57) | |
| Hispanic | 8.6 (29) | |
| Asian | 8.0 (27) | |
| Other | 10.7 (36) | |
| Alcohol use | ||
| Monthly frequency* | 0–31 | 7.7 (6.1) |
| Past year binge drinking | 38.9 (131) | |
| Alcohol-related problem* | 0–59 | 9.7 (10.8) |
| Alcohol dependence—lifetime | 48 (162) | |
| Peer alcohol usea | ||
| None | 9.5 (32) | |
| One | 14.8 (50) | |
| Less than half | 12.8 (43) | |
| More than half | 21.4 (72) | |
| Almost all | 41.2 (139) | |
| Parental alcoholism* | 0–6 | 1.3 (2.0) |
| Psychological distress* | 33–80 | 50.9 (10.8) |
| Childhood maltreatment | ||
| Emotional abuse | 5–25 | 9.98 (5.3) |
| Physical abuse | 5–25 | 7.64 (4.2) |
| Sexual abuse | 5–25 | 5.94 (3.1) |
| Neglect | 5–22 | 8.88 (3.7) |
Mean values (standard deviations). All other measures reported in proportion (%).
Valid percentages are reported.
Unique Contribution of Each Maltreatment Subtype on Psychological Distress and Drinking Behaviors
We performed a series of SEM analyses to examine the role of psychological distress in linking maltreatment subtypes to four drinking behaviors. Pathways were specified from child maltreatment to psychological distress and from psychological distress to drinking behaviors. Correlations of study variables are presented in Table 2.
TABLE 2.
Correlations of study variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Emotional abuse | — | ||||||||||
| Physical abuse | .64** | — | |||||||||
| Sexual abuse | .31** | .37** | — | ||||||||
| Neglect | .75** | .53** | .33** | — | |||||||
| Somatization | .33** | .27** | .34** | .29** | — | ||||||
| Depression | .43** | .22** | .11* | .36** | .58** | — | |||||
| Anxiety | .39** | .20** | .18** | .32** | .65** | .71** | — | ||||
| Overall BSI | .45** | .25** | .21** | .38** | .78** | .91** | .91** | — | |||
| Drinking frequency | .02 | *.10 | *.05 | *.02 | .09 | .10 | .07 | .10 | — | ||
| Binge drink | .65 | −.31 | *.58 | .01 | .08 | .11* | .08 | .10 | .54** | — | |
| RAPI | .22** | .20** | .12* | .15** | .27** | .27** | .25** | .30** | .26** | .46** | — |
| Alcohol dependence | .24** | .17** | .109 | .19** | .25** | .26** | .22** | .28** | .24** | .45** | .70** |
N for analysis=336.
Correlation is significant at the .05 level (2-tailed);
Correlation is significant at the .01 level (2-tailed).
All SEM analyses found a satisfactory model (Figs. 1 and 2).41 Only significant paths are included in the figures. Exogenous variables specified as freely correlated. Covariances of exogenous variables and of residual terms for endogenous constructs were included in the model but are not all in the figures. Controlling for other types of maltreatment, the current study found that among four types of maltreatment, emotional abuse might be the major driver of drinking behaviors among the victims of child maltreatment. We also found that psychological distress mediated the relationship between emotional abuse and alcohol-related problems, and emotional abuse and alcohol dependence, even after controlling for demographic information, other maltreatment subtypes, parental alcoholism, and peer alcohol use.
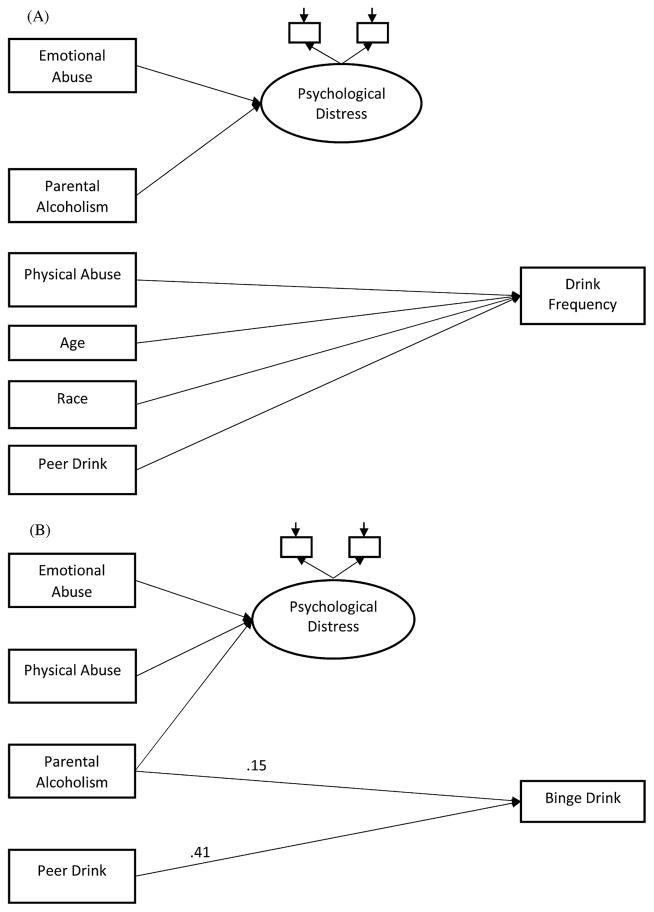
FIGURE 1.
Structural model for emotional abuse, psychological distress, and alcohol use. (A) Frequency of alcohol use. (B) Binge drinking. Only significant paths are included in the figures. Straight single-headed arrows represent path effects, and values are standardized coefficients. Coefficients are significant at p<.05.
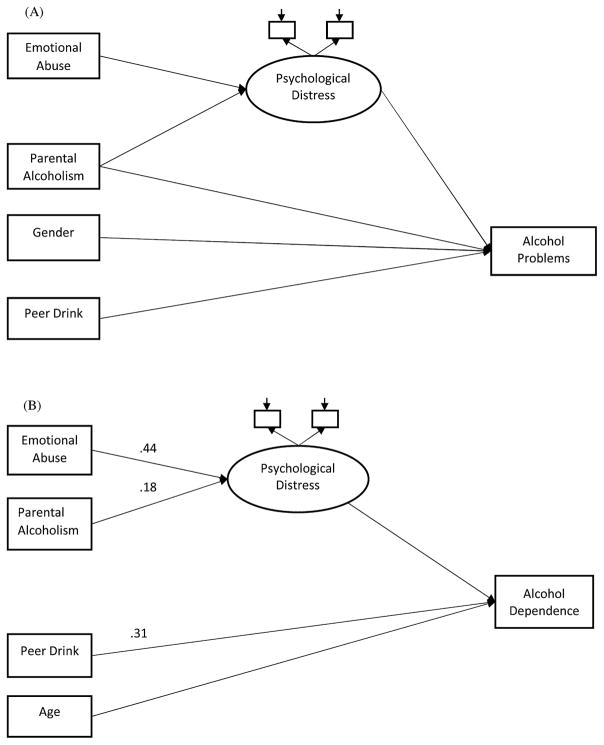
FIGURE 2.
Structural model for emotional abuse, psychological distress, and alcohol use. (A) Alcohol-related problems. (B) Alcohol dependence. Only significant paths are included in the figures. Straight single-headed arrows represent path effects, and values are standardized coefficients. Coefficients are significant at p<.05.
In specific, Fig. 1A presents the drink frequency model adjusting for the other types of maltreatment, which fits the data well (χ2=157.23, df=88, p<.001, CFI=.95, RMSEA=.05, SRMR=.04). Emotional abuse had a direct path to psychological distress (β=.44). However, psychological distress had no significant direct path to drink frequency. Next, the binge drinking model (Fig. 1B; χ2=119.21, df=88, p<.05, CFI =.96, RMSEA=.03, WRMR=.72) showed that emotional abuse was significantly related to psychological distress (β=.44), yet psychological distress was not significantly related to binge drinking. Figure 2A is the alcohol-related problems model, which fits the data well (χ2=152.52, df=88, p<.001, CFI=.95, RMSEA=.05, SRMR=.04). Emotional abuse was directly related to psychological distress (β=.45), which had a significant path to alcohol-related problems (β=.20). A test of indirect paths found that the mediated effects of emotional abuse on alcohol-related problems via psychological distress was significant (β=.09). Finally, the alcohol-dependence model (Fig. 2B; χ2=121.28, df=88, p<.05, CFI=.96, RMSEA =.03, WRMR=.73) found that emotional abuse had a direct path to psychological distress (β=.44), and psychological distress was related to alcohol dependence (β=.19). Results for indirect effects also showed that psychological distress mediated the relationship between emotional abuse and alcohol dependence (β=.08), and the relationship between parental alcoholism and alcohol dependence (β=.03).
DISCUSSION
We investigated the relationships between childhood maltreatment, psychological distress, and alcohol use in young adulthood. Consistent with previous research, we found that childhood emotional abuse was highly associated with psychological distress. Psychological distress was further associated with more pathological drinking outcomes such as alcohol-related problems and alcohol dependence. We also found that the effect of childhood emotional abuse on alcohol-related problems and alcohol dependence were further mediated by psychological distress, even after controlling for demographic status, other subtypes of child maltreatment, parental alcoholism and peer drink.
The present study showed that exposure to childhood emotional abuse was consistently related to psychological distress. Childhood emotional abuse has been linked specifically with the development of mood disorders in adulthood, such as major depressive disorder and bipolar disorder, which increase the risk of alcohol use disorders.44 Using a sample of 5,378 college freshmen, Gibb et al. (2001) found that among three types of child abuse, including emotional, sexual, and physical abuse, only emotional abuse was related to increased levels of hopelessness and episodes of non-endogenous major depression.45 Further, our findings suggest that emotional abuse may play a prominent role in the development of alcohol-related problems and dependence through mediation of psychological distress. Recent studies indicate that emotional abuse may in fact be more closely associated with alcohol dependence than other abuse forms. A study by Schwandt et al.46 examined the prevalence of five subtypes of childhood maltreatment (ie, emotional abuse, sexual abuse, physical abuse, emotional neglect, and physical neglect) in treatment-seeking alcohol-dependent patients. In comparison to other maltreatment subtypes, alcohol-dependent subjects were more than 10 times as likely to have experienced emotional abuse, which was also the main predictor for alcohol dependence severity. Additionally, the impulsiveness domain of neuroticism mediated the effect of emotional abuse on alcohol dependence severity whereas none of the other subtypes of abuse were mediated by neuroticism.46
Young adults who have been emotionally abused in childhood may be vulnerable to alcohol problems in part because they drink alcohol as a means of regulating the symptoms of psychological distress. Proposing the self-medication hypothesis nearly three decades ago, Khantzian47 argued that individuals are motivated to use alcohol for its pharmacological effects to alleviate distressing psychiatric disturbance. Although there are a few alcohol studies that failed to completely support this hypothesis,48 a number of studies have found that psychological distress, particularly subjective states of distress, has substantial influences on drinking motives in adulthood.49 For example, examining 3,592 current or former drinkers aged 18–39 in a national probability sample, Rothman et al.50 found that emotional abuse was associated with a 2.4-fold increase in risk for drinking to cope with stress, whereas emotional abuse was not related to drinking for pleasure or drinking to be social. To our knowledge, there is only one study examining the pathways from psychological distress to alcohol problems among adult victims of childhood sexual assault, which also suggests the mediating role of psychological distress.49 Future investigation is required for better understanding of the role of drinking motives, such as drinking to cope with negative emotionality, in linking childhood emotional abuse and psychological distress to later alcohol problems.
In our study, we found that emotional abuse and psychological distress were highly associated with more pathological drinking styles such as alcohol dependence and alcohol-related problems. The comorbidity between negative emotional states, such as depression and alcohol use disorders, is pervasive and has been reported to be as high as 11% in young adulthood.51 Although psychological distress has been associated with alcohol-related problems and dependence, we did not find a significant relationship between emotional abuse, psychological distress, and drink frequency or binge drinking. The inconsistent findings regarding the relation between childhood maltreatment, psychological distress, and drinking behaviors may be due to the fact that psychological distress relates to only certain stages of alcohol use or problematic alcohol use among victims of child maltreatment. For example, Camatta et al.52 found that negative emotional states, such as depression, stress and irrational beliefs, were positively associated with alcohol problems but not with alcohol frequency. Overall, studies have not found a significant relationship between frequency of alcohol consumption and depression. On the other hand, studies have been inconclusive about the relationship between psychological distress such as depression and binge drinking.53,54
The development of pathological drinking in young adult victims of emotional abuse is undoubtedly influenced by a large number of individual and contextual factors.27 Research investigating the etiology of hazardous drinking has suggested that impulsive personality traits may play a significant role in promoting problematic drinking among emotional abuse victims.55–57 For example, as emotionally abused children often live in hostile and threatening environments, many forms of functional self-control are difficult to learn.58,59 Therefore, young adults who experienced emotional abuse in childhood may impulsively cope through heavy drinking when they experience negative emotionality, leading to lower self-control and increased alcohol-related problems. Furthermore, they are involved in negative reinforcement such that the individuals act impulsively to escape from negative emotionality. Once they experience the negative reinforcement of temporary relief from their distress by drinking heavily, it increases their likelihood to further become involved in heavy drinking in response to their future distresses, and ultimately to develop pathological drinking habits and alcohol dependence.
Emotional abuse can occur in many forms including bullying, ignoring, coercion, manipulation, isolation, terrorizing, and exploiting. Due to the complexity of emotional abuse, each form of emotional abuse may manifest itself differently in victims and may also be associated with varying alcohol use outcomes. For example, in a study conducted by Allen, terrorizing, as a form of emotional abuse, was associated with anxiety and somatic symptoms; however, ignoring as a form of emotional abuse was associated with the development of depression and Borderline Personality Disorder.60 As such, future studies should consider the complexities of emotional abuse and examine the association between the various forms of emotional abuse with subsequent alcohol use outcomes.
Limitations
The present study has several limitations. Our findings are based on a retrospective self-report of childhood maltreatment. Although numerous studies have used retrospective self-report measures of childhood maltreatment in examining the effects of childhood maltreatment on a variety of developmental outcomes in young adulthood,61 it introduces the potential for recall bias, social desirability, and response acquiescence. Furthermore, as the present study used a convenience sample, it is unknown whether its sample is representative of young adult populations in the United States Next, the cross-sectional design used in the present study provided no insight into temporal directionality among emotional abuse, psychological distress, and pathological drinking behaviors. Although we found that emotional abuse was related to alcohol-related problems and dependence primarily through psychological distress, alcohol use during young adulthood might increase negative emotionality and psychological distress. Therefore, psychological distress might be the negative outcome of alcohol use as well as the predictor of it. Further, the mediating effect of psychological distress on emotional abuse, alcohol-related problems, and alcohol dependence could be attributed to other mediators not included in our study. Finally, child maltreatment has multiple dimensions including subtype, severity, chronicity, and frequency. The present study chose to study maltreatment subtypes and its influences on psychological distress and alcohol use, which did not address the potential effects of other dimensions of maltreatment experience on drinking behaviors in young adulthood. For example, the onset of maltreatment has been associated with varying psychopathology and alcohol use behaviors in adulthood. Kaplow and Widom (2007) found that an earlier onset of maltreatment (ages 0–5 year) predicted anxiety and depression in adulthood, whereas a later onset of maltreatment (ages 6–11 years) predicted alcohol abuse and antisocial behavior in adulthood.62
CONCLUSIONS
Our results are consistent with an internalizing pathway to alcohol-related problems and alcohol dependence. Exposure to emotional abuse was related to psychological distress, which in turn correlated with alcohol-related problems and alcohol dependence. This pathway most likely represents drinking to cope with psychological distress in young adults with a history of childhood emotional abuse. Our results suggest that screening for psychological distress and addressing depressive and anxiety symptoms among emotional abuse victims might be one approach in preventing problematic alcohol use during young adulthood.
Acknowledgments
This research was supported by grants from NIDA DA030884 (Shin) and the AMBRF/The Foundation for Alcohol Research (Shin). The Foundation had no role in the study design, collection, analysis, or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
References
- 1.Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-48, HHS publication no. 14-4863. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. pp. 13–4795. [Google Scholar]
- 2.Lynskey MT, Agrawal A, Heath AC. Genetically informative research on adolescent substance use: Methods, findings, and challenges. J Am Acad Child Adolesc Psychiatry. 2010;49:1202–1214. doi: 10.1016/j.jaac.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wiles NJ, Lingford-Hughes A, Daniel J, et al. Socio-economic status in childhood and later alcohol use: A systematic review. Addiction. 2007;102:1546–1563. doi: 10.1111/j.1360-0443.2007.01930.x. [DOI] [PubMed] [Google Scholar]
- 4.Wagenaar AC, Toomey TL. Effects of minimum drinking age laws: Review and analyses of the literature from 1960 to 2000. J Stud Alcohol Drugs. 2002:206–225. doi: 10.15288/jsas.2002.s14.206. [DOI] [PubMed] [Google Scholar]
- 5.Borsari B, Carey KB. Peer influences on college drinking: A review of the research. J Subst Abuse. 2001;13:391–424. doi: 10.1016/s0899-3289(01)00098-0. [DOI] [PubMed] [Google Scholar]
- 6.Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dube SR, Miller JW, Brown DW, et al. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J Adolesc Health. 2006;38:1–44. doi: 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Widom CS, White HR, Czaja SJ, et al. Long-term effects of child abuse and neglect on alcohol use and excessive drinking in middle adulthood. J Stud Alcohol Drugs. 2007;68:317–326. doi: 10.15288/jsad.2007.68.317. [DOI] [PubMed] [Google Scholar]
- 9.Schuck AM, Widom CS. Childhood victimization and alcohol symptoms in females: Causal inferences and hypothesized mediators. Child Abuse Negl. 2001;25:1069–1092. doi: 10.1016/s0145-2134(01)00257-5. [DOI] [PubMed] [Google Scholar]
- 10.Shin SH, Edwards E, Heeren T. Child abuse and neglect: Relations to adolescent binge drinking in the national longitudinal study of adolescent health (AddHealth) Study. Addict Behav. 2009;34:277–280. doi: 10.1016/j.addbeh.2008.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Young-Wolff KC, Kendler KS, Ericson ML, et al. Accounting for the association between childhood maltreatment and alcohol-use disorders in males: A twin study. Psychol Med. 2011;41:59–70. doi: 10.1017/S0033291710000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.White HR, Widom CS. Three potential mediators of the effects of child abuse and neglect on adulthood substance use among women. J Stud Alcohol Drugs. 2008;69:337–347. doi: 10.15288/jsad.2008.69.337. [DOI] [PubMed] [Google Scholar]
- 13.Trickett PK, Negriff S, Ji J, et al. Child maltreatment and adolescent development. J Res Adolesc. 2011;21:3–20. [Google Scholar]
- 14.Nelson EC, Heath AC, Madden PAF, et al. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes: Results from a twin study. Arch Gen Psychiatry. 2002;59:139–145. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- 15.Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. Am J Psychiatry. 2012;169:141–151. doi: 10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- 16.Marmorstein NR. Longitudinal associations between depressive symptoms and alcohol problems: The influence of comorbid delinquent behavior. Addict Behav. 2010;35:564–571. doi: 10.1016/j.addbeh.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brady K, Sinha R. Co-occurring mental and substance use disorders: The neurobiological effects of chronic stress. Am J Psychiatry. 2005;162:1483–1493. doi: 10.1176/appi.ajp.162.8.1483. [DOI] [PubMed] [Google Scholar]
- 18.Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105–130. doi: 10.1196/annals.1441.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jackson KM, Sher KJ. Alcohol use disorders and psychological distress: A prospective state-trait analysis. J Abnorm Psychol. 2003;112:599–613. doi: 10.1037/0021-843X.112.4.599. [DOI] [PubMed] [Google Scholar]
- 20.Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Rev Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- 21.Holahan CJ, Moos RH, Holahan CK, et al. Drinking to cope, emotional distress and alcohol use and abuse: A ten-year model. J Stud Alcohol. 2001;62:190–198. doi: 10.15288/jsa.2001.62.190. [DOI] [PubMed] [Google Scholar]
- 22.Boden JM, Fergusson DM. Alcohol and depression. Addiction. 2011;106:906–914. doi: 10.1111/j.1360-0443.2010.03351.x. [DOI] [PubMed] [Google Scholar]
- 23.Vujanovic AA, Bonn-Miller MO, Marlatt GA. Posttraumatic stress and alcohol use coping motives among a trauma-exposed community sample: The mediating role of non-judgmental acceptance. Addict Behav. 2011;36:707–712. doi: 10.1016/j.addbeh.2011.01.033. [DOI] [PubMed] [Google Scholar]
- 24.Young-Wolff KC, Kendler KS, Prescott CA. Interactive effects of childhood maltreatment and recent stressful life events on alcohol consumption in adulthood. J Stud Alcohol Drugs. 2012;73:559–569. doi: 10.15288/jsad.2012.73.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mullings J, Hartley D, Marquart JW. Exploring the relationship between alcohol use, childhood maltreatment, and treatment needs among female prisoners. Subst Use Misuse. 2004;39:277–305. doi: 10.1081/ja-120028491. [DOI] [PubMed] [Google Scholar]
- 26.Moran PB, Vuchinich S, Hall NK. Associations between types of maltreatment and substance use during adolescence. Child Abuse Negl. 2004;28:565–574. doi: 10.1016/j.chiabu.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 27.Widom CS, Hiller-Sturmhofel S. Alcohol abuse as a risk factor for and consequence of child abuse. Alcohol Res Health. 2001;25:52–57. [PMC free article] [PubMed] [Google Scholar]
- 28.Sartor CE, Lynskey MT, Bucholz KK, et al. Childhood sexual abuse and the course of alcohol dependence development: Findings from a female twin sample. Drug Alcohol Depend. 2007;89:139–144. doi: 10.1016/j.drugalcdep.2006.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Enoch M. Genetic and environmental influences on the development of alcoholism: Resilience vs. risk. Ann N Y Acad Sci. 2006;1094:193–201. doi: 10.1196/annals.1376.019. [DOI] [PubMed] [Google Scholar]
- 30.Agrawal A, Lynskey MT. Are there genetic influences on addiction: Evidence from family, adoption and twin studies. Addiction. 2008;103:1069–1081. doi: 10.1111/j.1360-0443.2008.02213.x. [DOI] [PubMed] [Google Scholar]
- 31.Cruz JE, Emery RE, Turkheimer E. Peer network drinking predicts increased alcohol use from adolescence to early adulthood after controlling for genetic and shared environmental selection. Dev Psychol. 2012;48:1390–1402. doi: 10.1037/a0027515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 33.Bernstein DP, Fink L. Childhood trauma questionnaire: A retrospective self-report. San Antonio, TX: Harcourt Brace, Psychological Corporation; 1998. [Google Scholar]
- 34.Derogatis LR. BSI brief symptom inventory. Administration, scoring, and procedures manual. Minneapolis: National Computer Systems; 1993. [Google Scholar]
- 35.Wechsler H, Davenport A, Dowdall G, et al. Health and behavioral consequences of binge drinking in college. JAMA. 1994;272:1672. [PubMed] [Google Scholar]
- 36.White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J Stud Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- 37.Hodgins DC, Maticka-Tyndale E, el-Guebaly N, et al. Alternative cut-point scores for the CAST-6. Addict Behav. 1995;20:267–270. doi: 10.1016/0306-4603(94)00063-8. [DOI] [PubMed] [Google Scholar]
- 38.MacKinnon DP, Lockwood CM, Hoffman JM, et al. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mackinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17:144–158. [Google Scholar]
- 40.MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- 41.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 42.Yu CY, Muthén BO. Evaluation of model fit indices for latent variable models with categorical and continuous outcomes (Technical report) Los Angeles: University of California, Los Angeles Graduate School of Education and Information Studies; 2001. [Google Scholar]
- 43.Brown T. Confirmatory factor analysis for applied research. New York: Guilford Press; 2006. [Google Scholar]
- 44.Etain B, Mathieu F, Henry C, et al. Preferential association between childhood emotional abuse and bipolar disorder. J Trauma Stress. 2010;23:376–383. doi: 10.1002/jts.20532. [DOI] [PubMed] [Google Scholar]
- 45.Gibb BE, Alloy LB, Abramson LY, et al. History of childhood maltreatment, negative cognitive styles, and episodes of depression in adulthood. Cognitive Ther Res. 2001;25:425–446. [Google Scholar]
- 46.Schwandt ML, Heilig M, Hommer DW, et al. Childhood trauma exposure and alcohol dependence severity in adulthood: Mediation by emotional abuse severity and neuroticism. Alcohol Clin Exp Res. 2013;37:984–992. doi: 10.1111/acer.12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Khantzian EJ. The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. Am J Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- 48.Breese GR, Overstreet DH, Knapp DJ. Conceptual framework for the etiology of alcoholism: A “kindling”/stress hypothesis. Psychopharmacology. 2005;178:367–380. doi: 10.1007/s00213-004-2016-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Grayson CE, Nolen-Hoeksema S. Motives to drink as mediators between childhood sexual assault and alcohol problems in adult women. J Trauma Stress. 2005;18:137–145. doi: 10.1002/jts.20021. [DOI] [PubMed] [Google Scholar]
- 50.Rothman EF, Edwards EM, Heeren T, et al. Adverse childhood experiences predict earlier age of drinking onset: Results from a representative US sample of current or former drinkers. Pediatrics. 2008;122:e298–e304. doi: 10.1542/peds.2007-3412. [DOI] [PubMed] [Google Scholar]
- 51.Briere FN, Rohde P, Seeley JR, et al. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Compr Psychiatry. 2014;55:526–533. doi: 10.1016/j.comppsych.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Camatta CD, Nagoshi CT. Stress, depression, irrational beliefs, and alcohol use and problems in a college student sample. Alcohol Clin Exp Res. 1995;19:142–146. doi: 10.1111/j.1530-0277.1995.tb01482.x. [DOI] [PubMed] [Google Scholar]
- 53.Graham K, Massak A, Demers A, et al. Does the association between alcohol consumption and depression depend on how they are measured? Alcohol Clin Exp Res. 2007;31:78–88. doi: 10.1111/j.1530-0277.2006.00274.x. [DOI] [PubMed] [Google Scholar]
- 54.Graham K, Schmidt G. Alcohol use and psychosocial well-being among older adults. J Stud Alcohol. 1999;60:345–351. doi: 10.15288/jsa.1999.60.345. [DOI] [PubMed] [Google Scholar]
- 55.Simons JS, Carey KB, Gaher RM. Lability and impulsivity synergistically increase risk for alcohol-related problems. Am J Drug Alcohol Abuse. 2004;30:685–694. doi: 10.1081/ada-200032338. [DOI] [PubMed] [Google Scholar]
- 56.Lejuez CW, Magidson JF, Mitchell SH, et al. Behavioral and biological indicators of impulsivity in the development of alcohol use, problems, and disorders. Alcohol Clin Exp Res. 2010;34:1334–1345. doi: 10.1111/j.1530-0277.2010.01217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dick DM, Smith G, Olausson P, et al. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addict Biol. 2010;15:217–226. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pears KC, Fisher P. Developmental, cognitive, and neuropsychological functioning in preschool-aged foster children: Associations with prior maltreatment and placement history. J Dev Behav Pediatr. 2005;26:112–122. doi: 10.1097/00004703-200504000-00006. [DOI] [PubMed] [Google Scholar]
- 59.Shields A, Cicchetti D. Parental maltreatment and emotion dysregulation as risk factors for bullying and victmization in middle childhood. J Clin Child Psychol. 2001;30:349–363. doi: 10.1207/S15374424JCCP3003_7. [DOI] [PubMed] [Google Scholar]
- 60.Allen B. An analysis of the impact of diverse forms of childhood psychological maltreatment on emotional adjustment in early adulthood. Child Maltreat. 2008;13:307–312. doi: 10.1177/1077559508318394. [DOI] [PubMed] [Google Scholar]
- 61.Teicher MH, Samson JA, Polcari A, et al. Sticks, stones, and hurtful words: Relative effects of various forms of childhood maltreatment. Am J Psychiatry. 2006;163:993–1000. doi: 10.1176/ajp.2006.163.6.993. [DOI] [PubMed] [Google Scholar]
- 62.Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. J Abnorm Psychol. 2007;116:176–187. doi: 10.1037/0021-843X.116.1.176. [DOI] [PubMed] [Google Scholar]