Abstract
Objective
This study estimates the expected cost-effectiveness and population impact of alternative outpatient interventions to reduce suicide risk among adults presenting to general hospital emergency departments (EDs), relative to usual care. Several such interventions have been found efficacious, but none is yet widespread, and cost-effectiveness of population-based implementation is unknown.
Methods
Modeled cost-effectiveness analysis comparing three ED-initiated suicide prevention interventions previously found to be efficacious: follow-up via postcards/caring letters, follow-up via telephone outreach, and suicide-focused Cognitive Behavioral Therapy (CBT), relative to usual care. Primary outcomes are treatment costs, suicides, and life-years saved, evaluated over the year after initial ED presentation.
Results
Relative to usual care, adding postcards improved outcomes and reduced costs. Adding telephone outreach and suicide-focused CBT, respectively, improved outcomes at a mean incremental cost of $5,900 and $18,8000 per life-year saved, respectively. Monte Carlo simulation (1,000 repetitions) revealed the chance of incremental cost-effectiveness to be certainty for all the three interventions, assuming societal willingness to pay ≥$50,000 per life year. These main findings were robust to various sensitivity analyses, including conservative assumptions about effect size and incremental costs. Population impact is limited by low sensitivity of detecting ED patients’ suicide risk, and health care delivery inefficiencies
Conclusions
The highly favorable cost-effectiveness found here for each outpatient intervention provides a strong basis for widespread implementation of any or all of these. The estimated population benefits of doing so would be additionally enhanced by increasing the sensitivity of suicide risk detection among individuals presenting to general hospital EDs.
INTRODUCTION
The United States’ Healthy People 2020 goals include a target suicide rate of 10.2 per 100,000 people, representing a 10% reduction from the 2007 rate of 11.3, and a 26% reduction from the 2015 rate of 13.8.1–3 Reaching this goal requires multiple strategies across different populations and settings.4–7 One key setting is hospital Emergency Departments (EDs), where at least 500,000 people present annually with self-injury, and many more with suicidal ideation. These numbers, along with evidence that self-injury and ideation are major suicide predictors, suggest that effective ED-initiated suicidality treatment is likely essential to meeting suicide prevention targets.8–10
This study examines the current evidence regarding ED-initiated interventions to reduce suicide risk in people presenting to general hospital EDs, to assess whether any such interventions are likely cost-effective enough to support widespread implementation. If so, there is a clinical and economic rationale for adopting such interventions as the new standard of practice, even while researchers develop and test additional suicide prevention interventions.
Several ED-initiated interventions to reduce suicide risk have been found to be efficacious in at least one randomized control trial, relative to usual care. These vary in approach and intensity, from the “caring letters” approach, which provides messages of psychosocial support to individuals after discharge; to post-discharge telephone contacts that encourage follow-up treatment; to aftercare involving suicide-focused Cognitive Behavioral Therapy.11–19 However, none is yet in widespread use; and the cost-effectiveness of population-based implementation, as well as the potential impact on suicide rates, is currently unknown.17–19 We therefore use decision analysis to address these questions, drawing on findings from existing efficacy trials, other available data, and expert opinion regarding suicide risk identification among ED patients.20 We also identify key gaps in existing evidence, for future research.
METHODS
A Markov state-transition model was created to evaluate the cost-effectiveness of three interventions designed to reduce post-discharge suicide risk among adults (aged 18+) presenting to general hospital EDs. Patients treated in psychiatric EDs are outside our scope. Our study period is 54 weeks from the initial (index) ED presentation, divided into nine six-week Markov cycles (for expositional convenience, we report annualized results). The model begins with initial ED presentation; each subsequent period, each individual can have a new non-fatal suicide event, die by suicide, die by other manner, or none of these. Our endpoints are case identification; suicide attempts averted; life-years saved; and costs associated with the index and any subsequent ED visit, and with inpatient and outpatient care that follows ED presentation. We used TreeAge Pro 15.2.1.0-v20150831 modeling software.
Triage and Case Identification
For tractability, and absent clear empirical guidance, we assume that each ED patient falls into one of three latent (i.e., unobserved) states of suicide risk: high (2.8%), low (9.6%), and none (87.6%). High-risk patients have high near-term risk of suicidal acts, defined here as the next six weeks. Low-risk patients have somewhat elevated suicidal risk, which we define operationally as half the rate of high risk. By definition, no-risk patients have zero near-term suicide risk. Details for all model parameters are in Table 1; Supplemental eFigure 1 illustrates our understanding of patient flow through the ED for high- and low-risk (eFigure 1a) and no-risk (eFigure 1b) patients.
Table 1.
Inputs
| Category | Point estimate | Range | Source |
|---|---|---|---|
|
| |||
| PREVALENCE | |||
|
| |||
| Suicide risk status at time of initial ED presentation | |||
|
| |||
| High risk | 2.8% | * | |
|
| |||
| Low risk | 9.6% | * | |
|
| |||
| No risk | 87.6% | * | |
|
| |||
| Triage | |||
|
| |||
| Medical Branch | 93% | 90% – 97% | * |
|
| |||
| Percentage of the hospitalized patients among the general ED population (i.e., the study cohort) | 13.4% | 12.2%–14.6% | 38,39,** |
|
| |||
| Of these, hospitalized for medical reasons, no sign of suicidality | 7.04%* | * | |
|
| |||
| Of these, no risk | 100% | 100% – 100% | * |
|
| |||
| Of these, hospitalized for medical reasons, apparent self-injury | 4.5% | 2% – 8% | ** |
|
| |||
| Of these, high risk | 20% | 15% – 25% | ** |
| Of these, low risk | 30% | 25% – 35% | ** |
| Of these, no risk | 50%** | * | |
|
| |||
| Of these, medical treatment in ED | 88.46% | * | |
|
| |||
| Of these, high risk | 1.75% | 0.75% – 2.75% | 40,*** |
| Of these, low risk | 8% | 6% – 10% | 27,40,*** |
| Of these, no risk | 90.25% | 87.25% – 93.25% | 30,*** |
|
| |||
| Psych Branch | 7% | 3% – 10% | 41 |
|
| |||
| Of these, high risk | 7.5% | 5% – 10% | 41,*** |
| Of these, low risk | 25% | 20% – 30% | 41,*** |
| Of these, no risk | 67.5% | 60% – 75% | 30,*** |
|
| |||
| SENSITIVITY & SPECIFICITY | |||
|
| |||
| Medical Branch, suicide screening | |||
|
| |||
| Sensitivity, high risk | 30% | 20%–40% | ** |
|
| |||
| Sensitivity, low risk | 3% | 0% – 6% | ** |
|
| |||
| Specificity, no risk | 99% | 95% – 100% | ** |
|
| |||
| Medical Branch, suicide risk assessment among those with positive suicide screening | |||
|
| |||
| Sensitivity, high risk | 95% | 90% – 100% | ** |
|
| |||
| Sensitivity, low risk | 66% | 50% –80% | ** |
|
| |||
| Specificity, no risk | 50% | 40% – 60% | ** |
|
| |||
| Psych Branch, suicide risk assessment (100% assumed to have positive suicide screening) | |||
|
| |||
| Sensitivity, high risk | 95% | 93%–97% | ** |
|
| |||
| Sensitivity, low risk | 66% | 50%–80% | ** |
|
| |||
| Specificity, no risk | 56% | 46% – 66% | 42 |
| Sensitivity & specificity of identifying suicide risk in patients admitted to hospital from ED for medical reasons | |||
|
| |||
| Sensitivity, high risk | 100% | 100% – 100% | ** |
|
| |||
| Sensitivity, low risk | 100% | 100% – 100% | ** |
|
| |||
| Specificity, no risk | 50% | 40% – 60% | ** |
|
| |||
| EVENT PROBABILITIES – PSYCHIATRIC HOSPITALIZATION | |||
|
| |||
| Medical Branch, positive suicide screen & positive suicide assessment | 35%* | 25% – 45% | 24,*** |
|
| |||
| Psych Branch, positive suicide assessment | 80% | 70% – 90% | 24,*** |
|
| |||
| Psych Branch, negative suicide assessment | 10% | 5% – 15% | ** |
|
| |||
| BASE COSTS | |||
|
| |||
| Medical ED visit (no risk; discharged alive) | $675 | $25–$2,850 | 24,*** |
|
| |||
| Medical ED visit (high risk or low risk; discharged alive) | $890 | $25–$3,350 | 24,*** |
|
| |||
| Psych ED visit (discharged alive) | $695 | $25–$2,950 | 24,*** |
|
| |||
| Suicide risk assessment | $150 | $100–$200 | ** |
|
| |||
| Medical hospitalization (no risk; discharged alive) | $8,765 | $1,450–$33,500 | 24,*** |
|
| |||
| Medical hospitalization (no risk; died in the hospital) | $21,740 | $1,650 – $104,000 | 24,*** |
|
| |||
| Medical hospitalization (high risk or low risk; discharged alive) | $11,080 | $1,550–$49,500 | 24,*** |
|
| |||
| Medical hospitalization (high risk or low risk; died in the hospital) | $21,460 | $2,650–$123,000 | 24,*** |
|
| |||
| Psychiatric hospitalization (discharged alive) | $5,875 | $1,050–$20,500 | 24,*** |
|
| |||
| Psychiatric hospitalization (died in the hospital by suicide) | $18,790 | $1,350–$85,000 | 24,*** |
|
| |||
| Inpatient suicide Tx | $2,000 | ** | |
|
| |||
| DEATH AND REATTEMPT RATES | |||
|
| |||
| Death by non-suicide manner (in 6 weeks) – same for all risk categories & treatments: Based on average non-suicide mortality for ages 35–44, US, general population, men & women combined, 2007–2010 | 0.02044% | 43 | |
|
| |||
| Probability for a new suicide attempt (assuming no treatment) | |||
|
| |||
| High risk –1st Markov cycle after the index event | 0.048 | 44,*** | |
|
| |||
| High risk – 2nd – 4th Markov cycle, each | 0.00038 | 44,** | |
|
| |||
| High risk – 5th Markov cycle | 0.00029 | 44,** | |
|
| |||
| High risk – 6th – 9th Markov cycle, each | 0.00020 | 44,** | |
|
| |||
| Low risk – no treatment (false negative) – distributed by 6-week cycles | 50% of high rate | ** | |
|
| |||
| No risk | 0% | ** | |
|
| |||
| Ratio of suicides to suicide attempts | 1:13 | 45,46 | |
|
| |||
| Years of Potential Life Lost per suicide | 24 | 46,*** | |
|
| |||
| INTERVENTIONS - UPTAKE, OUTCOMES and COSTS | |||
|
| |||
| Usual Care (UC; also provided to people who receive inpatient suicide treatment)*** | |||
|
| |||
| Uptake (i.e., this % receive any outpatient suicide treatment) | 35% | 10% – 50% | ** |
|
| |||
| Reduction in (re-)attempt rate, vs. no treatment | 15% | 10% – 20% | ** |
|
| |||
| Cost [based on CPT 90791 (psychiatric diagnostic evaluation) + 2 times CPT 90834 (45 min psychotherapy)] | $340 | 23,** | |
|
| |||
| Postcards (PC)* | |||
|
| |||
| Uptake | 100% | NA | 11 |
|
| |||
| Reduction in (re-)attempt rate, vs. UC | 45% | 35% – 55% | 11,** |
|
| |||
| Additional cost of intervention [based on $10 per person for the postcards per se; plus $135 (1.5 CPT 90834 visits) in additional outpatient treatment as function of receiving the postcards] | $145 | $135 – $500 | 11,** |
|
| |||
| Telephone Outreach (TO) | |||
|
| |||
| Uptake (i.e., this % of those offered TO participate; the rest do UC only) | 70% | 60% – 80% | 12,** |
|
| |||
| Reduction in (re-)attempt rate among those with TO uptake, vs. UC | 34% | 25% – 45% | 12,** |
|
| |||
| Additional cost of intervention, for those with uptake [based on $30 for the phone calls per se, plus $270 (3 CPT 90834 visits) in additional outpatient Tx as function of receiving the calls] | $300 | $300 – $900 | 12,** |
|
| |||
| Cognitive Behavioral Therapy (CBT) | |||
|
| |||
| Uptake (i.e., this % of those offered CBT participate; the rest do UC only) | 65% | 55% – 75% | 13,** |
|
| |||
| Reduction in (re-)attempt rate among those with uptake, vs. UC | 50% | 40% – 60% | 13,** |
|
| |||
| Additional cost of intervention, for those with uptake [based on 9 times CPT 90834] | $810 | $810 – $2000 | 13,*** |
NOTES:
Calculated by the authors based on available data regarding prevalence of suicide risk within subgroups of the ED population (i.e., the sources cited under “Triage” in Table 1), so that each individual presenting to the ED for the initial (index) visit is counted exactly once
Author opinion
Author opinion, considering information available from the listed source(s)
We assume individuals receive a very brief suicide risk screen by the triage nurse, and are triaged by whether they have acute/emergent medical problems ("medical branch") or not ("psych branch"). Medical patients are hospitalized immediately or treated in the ED; they may be re-screened for suicide risk, based on self-report of suicidality or nurse judgement. Medical patients screening positive for suicide risk, and all psych branch patients, undergo a full clinical suicide risk assessment. Patients who assess positive are hospitalized; or discharged and referred to outpatient treatment, i.e., usual care or one of the alternative interventions. Patients screening or assessing negative are considered non-suicidal, regardless of their “true” risk state. Screening and assessment aims to identify patients with any (high or low) vs. no suicide risk. However, the assumed sensitivity and specificity of screening and assessment, and probabilities of hospitalization vs. discharge, differ for high, low and no risk, respectively (and by the presence and severity of medical conditions).
Outpatient Suicide Interventions
We assume that all patients identified with suicide risk are offered usual care (UC) after ED or hospital discharge. Our operationalized model of aftercare assumes the following: 65% will receive no specific treatment after discharge, 35% will receive an average of one initial diagnostic evaluation plus two 45-minute psychotherapy sessions during the 12 weeks post-discharge (additional details are in Table 1). Our base estimate is that UC reduces the rate of suicide (re-)attempt by 5.25% in the target population over the 12 weeks post-discharge, relative to no treatment, i.e., a 15% reduction among the 35% who receive treatment. After 12 weeks, these effects decline linearly to zero at the end of the study period.
For patients identified with suicide risk and discharged from the ED, we consider three ED-initiated outpatient interventions delivered in addition to UC; these were the only three such interventions that had been tested via randomized control trial when we began this research. For each intervention, we assumed equal effectiveness for persons experiencing suicidal ideation and nonfatal suicidal acts within the respective risk categories. In this study, we assume these interventions are not available to patients hospitalized from the ED:
Postcards – ED or other personnel send patients a total of eight follow-up postcards (PC) as psychosocial support, monthly for four months and then bimonthly.11 We assume that all targeted patients receive this intervention. Per the results of the most relevant trial, conducted in a medical ED among self-poisoning cases, our base estimate is that PC reduces the rate of suicide (re-)attempt by 45% relative to UC alone (and approximately 48% relative to no treatment).11
Telephone outreach – ED or other personnel conduct telephone outreach (TO) as psychosocial support and to encourage engagement in follow-up outpatient treatment, 1–3 months after discharge.12 Per the trial results, 70% of targeted patients receive these calls. Our base estimate is that TO reduces the rate of suicide (re-)attempt by 34% in this 70%, relative to UC alone, across our study period.12
Cognitive Behavior Therapy – ED or other personnel connect patients to a suicide-focused cognitive behavioural therapy (CBT) program.13 We assume that 65% of targeted patients participate, based on the fraction of patients who agreed to participate in the clinical trial. Participants receive an average of nine weekly or biweekly psychotherapy sessions as needed. Our base estimate is that CBT reduces the rate of suicide (re-) attempt by 50% among participants, relative to UC alone, across our study period.13
In each of these, the ED has responsibility for initiating follow-up engagement with the patient. In the respective trials, this was done by ED staff, but in general it could also be done by non-ED staff, e.g., within the same health system.7,21,22
Costs
Interventions can affect costs two ways: the direct cost of delivery, including the intervention per se and any associated health care use; and by altering the incidence of subsequent suicide events. For delivery costs, we use data on health service use reported in the corresponding clinical trial, inferring the relevant CPT codes, and assigning costs based national rates from the 2014 Medicare Physician Fee Schedule.11–13,23 For ED visits and hospitalizations, we calculated average costs based on analysis of corresponding events in the Healthcare Cost and Utilization Project (HCUP) database, for individuals discharged alive and deceased, respectively (Table 1). We use HCUP data from four states (AZ, FL, NE, UT) that either mandate or are known to fully report ICD-9 External Cause of Injury codes.24,25 General medical costs not associated with ED visits and related hospitalizations are outside this study’s scope.
Outcomes
At the end of each Markov cycle, individuals either die by suicide, die by another manner, experience a suicide (re-)attempt, or survive without additional attempt. We assume that one-in-13 suicide attempts result in death; the other 12 enter the next Markov cycle with a new ED presentation. Some hospitalized patients are at risk for suicide and/or death by another manner in the hospital, depending on their medical and suicide-risk state (Supplemental eFigure 1).
We assume that individuals maintain the same suicide-risk state (high, low, none) across the study period, and that risk of a new suicide event declines with each Markov cycle that does not include such an event. After a new (re-)attempt, transition probabilities reset to the same levels as after the index event. We assume that sensitivity and specificity of suicide screening and assessment is the same at the index and any subsequent ED visit.
RESULTS
Cost-Effectiveness
Base-case analysis
Based on eFigure 1 and the base parameter values in Table 1, we computed the mean expected costs and life-years per person during our study period, under each of the four interventions (UC, PC, TO, CBT); and incremental costs and life-years, and cost-effectiveness ratio of PC, TO, and CBT, respectively, relative to UC (Table 2). If there were no deaths in our cohort during the study period, mean life-years would be exactly one.
Table 2.
Expected costs, effectiveness and incremental cost-effectiveness, relative to UC
| Prevention strategy |
Treatment Cost, $ | Life Years | Incremental Cost- Effectiveness ($/LY) |
||
|---|---|---|---|---|---|
| Total (per person) |
Incremental (per person) |
Total (per person) |
Incremental (per person) |
||
| Usual care | 1961.812 | 0 | 0.979321179 | 0 | … |
| Post cards | 1960.454 | −1.36 | 0.979693574 | 0.000372395 | Cost & life saving |
| Telephone outreach | 1962.855 | 1.043 | 0.979565566 | 0.000244387 | 4,300 |
| CBT | 1966.77 | 4.96 | 0.979584921 | 0.000263742 | 18,800 |
LY, life-year; ellipses, not applicable
Mean costs per patient are $1,962 under usual care. Relative to UC, mean costs were 0.07% lower under PC, and 0.05% and 0.25% higher under TO and CBT, respectively. Each enhanced interventions reduced mortality, on average. Relative to UC, PC was “dominant,” in the sense of having both lower costs and better outcomes. The estimated mean incremental cost per life-year was $4,300 for TO and $18,800 for CBT.
Monte Carlo simulation
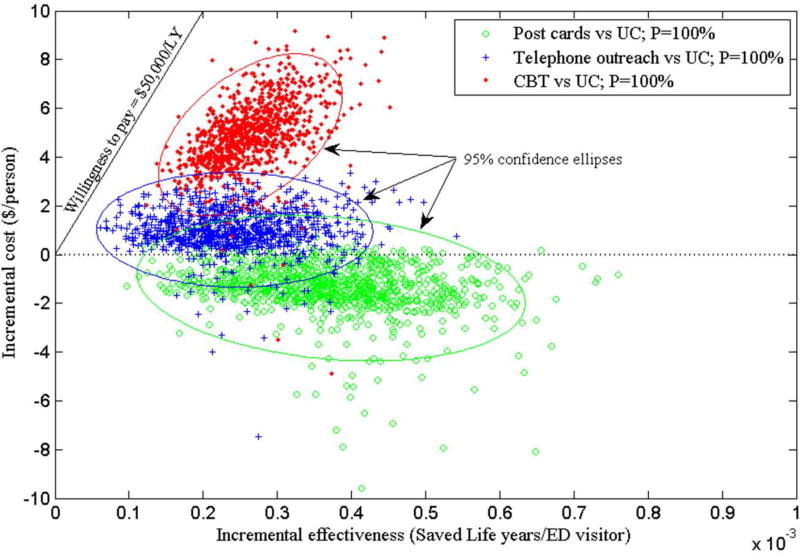
Figure 1 presents incremental costs and outcomes of the enhanced interventions relative to UC, based on Monte Carlo simulation accounting for uncertainty across the model inputs. Table 1 lists ranges for each input, and values are assumed to follow a beta distribution; we drew 1,000 samples and computed the expected values of the respective outcomes for each vector of sampled parameters. While there is no definitive benchmark regarding societal willingness to pay (WTP) to reduce mortality, the sloped line in Figure 1 marks the relatively conservative WTP threshold of $50,000 per life-year.26 Trials to the right of that line represent more favorable incremental cost-effectiveness (ICE). For each comparison, ellipses mark the 95% confidence interval for estimated ICE.
Figure 1.
Incremental costs and outcomes of the enhanced interventions versus usual care, based on Monte Carlo simulation
Relative to UC, PC and CBT improve outcomes with ICE at or below $50,000/LF with certainty, while the probability of TO improving outcomes at or below this threshold is 99.5%. The probability of PC dominating UC is 94%, and PC is cost-effective relative to UC even for WTP = $0/LY. The probability of TC being cost-effective relative to UC is 96% at WTP = $20,000/LY, and 80% at WTP = $10,000/LY (Supplemental eFigure 2); while the probability of CBT being cost-effective relative to UC is 67% at WTP = $20,000/LY, although only 1.6% at WTP = $10,000/LY.
Sensitivity analysis
We conducted one-way sensitivity analyses for all inputs, across at least the full range in Table 1. For nearly all inputs, our primary finding, the cost-effectiveness of each enhanced intervention relative to UC at WTP ≤$50,000/LY, remained intact across this range. The sole exceptions were substantial increases in each intervention’s costs, and the specificity of suicide risk screening among medical branch patients. For CBT vs. UC, incremental cost-effectiveness exceeded $50,000/LY if specificity fell from our base rate of 99% (i.e., 1% false positives among no-risk patients) to 91% or below; for TO vs. UC, ICE went above this WTP benchmark for specificity below 60%. For PC vs. UC, incremental costs were positive for specificity below 79%, but ICE remained below $50,000/LY even at specificity below 40%. Given our other assumptions, even reducing specificity of suicide risk assessment among medical patients who screen positive, and all psych patients, to 30% from our base rate of 50% did not raise ICE above $50,000/LY for any of the three interventions, vs. UC.
Given the obvious relevance of each intervention’s effect size and costs, we conducted two-way sensitivity analyses for these parameters (Table 3 and Supplemental eFigure 3). In Table 3, each row represents an alternative assumption about the cost of the respective interventions; the two columns report the effect size above which the intervention’s ICE vs. UC was below $50,000/LY or $100,000/LY at the specified cost. For instance, if the cost of TO tripled to $900 from the base value of $300, ICE of TO vs. UC would remain below $50,000/LY as long as TO reduced the suicide rate by at least 26% relative to UC, compared to our base value of 34%.
Table 3.
Risk reduction ratios under which the prevention strategies are cost-effective at WTP levels of $50,000 and $100,000 per saved life year
| Intervention | Cost of Delivery | WTP = $50,000 per saved life year |
WTP = $100,000 per saved life year |
|---|---|---|---|
| Risk reduction relative to UC | Risk reduction relative to UC | ||
| Postcards (PC) | $135 (base case) | Cost- and life-saving | Cost- and life-saving |
| $270 | 3% | 2.5% | |
| $500 | 7% | 4.5% | |
| Telephone Outreach (TO) | $300 (base case) | 6% | 3% |
| $600 | 16% | 9% | |
| $900 | 26% | 14% | |
| Cognitive Behavioral Therapy (CBT) | $810 (base case) | 20% | 10% |
| $1,600 | 45% | 23% | |
| $2,000 | 68% | 30% |
Population Impact
Our findings regarding the relative cost-effectiveness of each enhanced intervention are not sensitive to plausible variation in sensitivity of suicide screening or suicide risk assessment. In short, this is because false negatives do not have the opportunity for improved outcomes, but also do not incur additional costs (whereas false positives also have no opportunity for improved outcomes, but incur additional costs). However, sensitivity of screening/assessment is important for a different aspect of this analysis: the extent that enhanced intervention could reduce suicides in the target population.
Per Table 1, we estimate that 12.4% of individuals presenting for the index ED visit are suicidal, 2.8% high- and 9.6% low-risk. Of these, we estimate that approximately 82% of high- and 26% of low-risk patients would be identified, based on our estimates for screening and assessment sensitivity; the rest are false negatives. However, only identified patients who are discharged from the ED are eligible for the enhanced interventions, i.e., approximately 26% of high- and 3% of low-risk patients, following our assumptions about hospitalization – or around 8% of all individuals in the cohort with elevated suicide risk. This represents an upper bound for impact in the target population. Applying additional estimates of each intervention’s relative effect size, the Monte Carlo simulations yield an estimated reduction of suicide deaths in the cohort from the enhanced interventions of around 2.5% [95% CI: 0%–11%]; the differences between PC, TO, and CBT are not statistically significant at conventional levels.
DISCUSSION
Our modeled analysis of ED-initiated suicide prevention interventions found one, Postcards (PC), improved outcomes and reduce costs relative to usual care. Two others, Telephone Outreach (TO) and Cognitive Behavioral Therapy (CBT), improved outcomes at an incremental cost below $50,000/LY, a conservative estimate of societal willingness to pay for reducing mortality.26 These findings were largely insensitive to plausible variation in model inputs. In our view, this provides a compelling rationale for widespread implementation of any of these interventions, most obviously PC.
However, even widespread implementation would have limited population impact due to low sensitivity of detecting ED patients’ suicide risk, and to health system inefficiencies. While this aspect of our findings should not deter adoption of interventions that are strongly cost-effective even under current circumstances, it suggests additional avenues for increasing intervention benefits, particularly increasing sensitivity of detecting near-term suicide risk in the ED population, and improving coordination and continuity of care across delivery settings after patients leave the ED.27–32 Our findings also highlight the importance of ensuring that evidence-based interventions are economically viable, and that appropriate training and technical assistance are available.
This study has important limitations. EDs vary considerably in staffing, treatment protocols, and other characteristics. Given available information, and the requirements for parsimony inherent in decision analysis, we tried to create a framework reflective of general hospital EDs in the US. In any case, our main findings are quite robust to alternative assumptions about patient flow through an ED, within the parameter ranges in Table 1. This makes our model useful for studying additional improvements in ED practice, such as efforts to improve sensitivity and/or specificity of suicide screening, and from additional efficacy/effectiveness trials.
We relied on author opinion to estimate many inputs, because we could find no corresponding published source, nor any available data for primary estimation. Here, too, we are reassured by the robustness of our findings to alternative parameter values. We consider effects on mortality, but not improvements in quality of life; this is a conservative assumption here.
Only limited evidence exists regarding the effectiveness and costs of these enhanced interventions (and trials have lacked power to assess suicide death).11–19 The trials we reference were conducted under conditions that differ somewhat from our model.11–13 PC and TO were tested outside the US, and CBT in a highly urban US setting. All trials were small, and none explicitly reported effects on costs. The PC trial focused on self-poisoning cases, a subset of ED patients with suicide risk; and it found significant reductions in the number of re-attempts, but not in the fraction of patients who re-attempted.11 A separate PC study focused on all manners of self-harm, with similar results.33 The TO trial also focused on self-poisoning, with null intent-to-treat but positive as-treated findings.12 In the CBT trial, one-third of invited patients declined to participate, while adherence to the therapy protocol approached 100% in the rest.13 These trials found similar effect sizes, across substantially different interventions; this gives us some caution regarding PC’s relative dominance, although not about its cost-effectiveness relative to UC.
Despite the limitations, each of these interventions appears to be strongly cost-effective. Additional research on these and other interventions to reduce suicide risk among individuals presenting to general hospital EDs may further aid decision-makers. For instance, the Emergency Department Safety and Follow Up Evaluation (ED-SAFE) study reported that detection of at-risk individuals can be doubled with universal screening in 8 US EDs.30 ED-SAFE also tested a form of TO aimed at supporting treatment adherence, with back up crisis support provided by a call center that is part of the National Suicide Prevention Lifeline, finding that universal screening and TO resulted in a 27% reduction in the risk of a composite outcome of attempts and deaths compared to UC alone.34–36 The Attempted Suicide Short Intervention Program (ASSIP) trial in Switzerland, which combined elements of CBT and PC, reported an 80% reduction in re-attempts.37 Together, these findings support enhancing the standard of care for suicide risk in general hospital EDs, in service of reaching national suicide prevention targets.
Supplementary Material
Acknowledgments
Support for this research was provided to Drs. W, X, Y, and Z via contract by the National Institute of Mental Health. The authors thank Drs. Annette Beautrais and Gregory Luke Larkin for participating in preliminary discussions on a range of approaches to suicide risk detection and prevention in emergency care settings.
Footnotes
DISCLOSURES: The authors have no conflicts of interest to disclose.
Contributor Information
Peter Denchev, National Institute of Mental Health, Bethesda, Maryland.
Jane Pearson, NIMH - DSIR, Bethesda, Maryland.
Michael H. Allen, University of Colorado Denver School of Medicine - Psychiatry, Aurora, Colorado
Cindy Claassen, University of North Texas Health Science Center - Department of Psychiatry, Fort Worth, Texas.
Glenn W. Currier, Morsani College of Medicine, University of South Florida, Department of Psychiatry and Behavioral Neurosciences, Florida
Douglas Zatzick, UW/Harborview Medical Center - Psychiatry & Behavioral Sciences, Seattle, Washington.
Michael Schoenbaum, National Institute of Mental Health, Epidemiology, and Economics Division of Services and Intervention Research, Bethesda, Maryland.
BIBLIOGRAPHY
- 1.US Department of Health & Human Services. Mental Health and Mental Disorders Objectives - Healthy People 2020. [Accessed April 8, 2016]; http://www.cdc.gov/nchs/healthy_people/hp2020.htm. Published 2015.
- 2.National Center for Health Statistics, Centers for Disease Control and Prevention. [Accessed March 11, 2017];NCHS Data Brief No. 241, April 2016: Increase in Suicide in the United States, 1999–2014. 2016 https://www.cdc.gov/nchs/products/databriefs/db241.htm.
- 3.Drapeau C, McIntosh J for the American Association of Suicidology. [Accessed March 11, 2017];U.S.A. Suicide: 2015 Official Final Data. 2016 http://www.suicidology.org/Portals/14/docs/Resources/FactSheets/2015/2015datapgsv1.pdf?ver=2017-01-02-220151-870.
- 4.U.S. Surgeon General, National Action Alliance for Suicide Prevention. 2012 National Strategy for Suicide Prevention: GOALS AND OBJECTIVES FOR ACTION. [Accessed March 11, 2017];2012 https://www.surgeongeneral.gov/library/reports/national-strategy-suicide-prevention/full_report-rev.pdf.
- 5.Pringle B, Colpe LJ, Heinssen RK, et al. A strategic approach for prioritizing research and action to prevent suicide. Psychiatr Serv. 2013;64(1):71–75. doi: 10.1176/appi.ps.201100512. [DOI] [PubMed] [Google Scholar]
- 6.Joint Commission. Sentinel Event Alert #56: Detecting and treating suicide ideation in all settings | Joint Commission. [Accessed May 19, 2016]; https://www.jointcommission.org/sea_issue_56/. Published 2016. [PubMed]
- 7.Zero Suicide in Health and Behavioral Health Care. About Zero Suicide | Zero Suicide. [Accessed March 11, 2017]; http://zerosuicide.sprc.org/about.
- 8.Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention. Crisis. 2010;31(1):1–6. doi: 10.1027/0227-5910/a000001. [DOI] [PubMed] [Google Scholar]
- 9.Carroll R, Metcalfe C, Gunnell D. Hospital presenting self-harm and risk of fatal and non-fatal repetition: systematic review and meta-analysis. PLoS One. 2014;9(2):e89944. doi: 10.1371/journal.pone.0089944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmedani BK, Simon GE, Stewart C, et al. Health care contacts in the year before suicide death. J Gen Intern Med. 2014;29(6):870–877. doi: 10.1007/s11606-014-2767-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carter GL, Clover K, Whyte IM, Dawson AH, D’Este C. Postcards from the EDge: 5-year outcomes of a randomised controlled trial for hospital-treated self-poisoning. Br J Psychiatry. 2013;202(5):372–380. doi: 10.1192/bjp.bp.112.112664. [DOI] [PubMed] [Google Scholar]
- 12.Vaiva G, Ducrocq F, Meyer P, et al. Effect of telephone contact on further suicide attempts in patients discharged from an emergency department: randomised controlled study. BMJ. 2006;332(7552):1241–1245. doi: 10.1136/bmj.332.7552.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294(5):563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- 14.Luxton DD, June JD, Comtois KA. Can postdischarge follow-up contacts prevent suicide and suicidal behavior? A review of the evidence. Crisis. 2013;34(1):32–41. doi: 10.1027/0227-5910/a000158. [DOI] [PubMed] [Google Scholar]
- 15.Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52(6):828–833. doi: 10.1176/appi.ps.52.6.828. [DOI] [PubMed] [Google Scholar]
- 16.Hassanian-Moghaddam H, Sarjami S, Kolahi A-A, Lewin T, Carter G. Postcards in Persia: A Twelve to Twenty-four Month Follow-up of a Randomized Controlled Trial for Hospital-Treated Deliberate Self-Poisoning. Arch Suicide Res. 2015 Mar;:1–17. doi: 10.1080/13811118.2015.1004473. [DOI] [PubMed] [Google Scholar]
- 17.Hawton K, Witt KG, Taylor Salisbury TL, et al. Psychosocial interventions for self-harm in adults. Cochrane database Syst Rev. 2016;5:CD012189. doi: 10.1002/14651858.CD012189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawton K, Witt KG, Taylor Salisbury TL, et al. Psychosocial interventions following self-harm in adults: a systematic review and meta-analysis. Lancet Psychiatry. 2016 doi: 10.1016/S22150366(16)300700. Epub ahed of print. [DOI] [PubMed] [Google Scholar]
- 19.Zalsman G, Hawton K, Wasserman D, et al. Suicide prevention strategies revisited: 10-year systematic review. The Lancet Psychiatry. 2015;3(7):63–72. doi: 10.1016/S2215-0366(16)30030-X. [DOI] [PubMed] [Google Scholar]
- 20.National Academies of Sciences. [Accessed May 4, 2016];How Modeling Can Inform Strategies to Improve Population Health: Workshop Summary : Health and Medicine Division. 2015 http://www.nationalacademies.org/hmd/Reports/2015/How-Can-Modeling-Inform-Strategies-to-Inform-Population-Health.aspx. [PubMed]
- 21.Vaze M for the National Suicide Prevention Lifeline. [Accessed March 11, 2017];Crisis Center Guidance: Follow-up with Callers and Those Discharged from Emergency Department and Inpatient Settings. 2012 http://suicidepreventionlifeline.org/wp-content/uploads/2016/09/Lifeline-Follow-Up-Guidance1214.pdf.
- 22.National Institute of Mental Health. RFA-MH-16-800: Applied Research Toward Zero Suicide Healthcare Systems (R01) [Accessed March 11, 2017]; https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-16-800.html.
- 23.Centers for Medicare and Medicaid Services. Physician Fee Schedule Search. [Accessed April 14, 2016]; https://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.
- 24.Agency for Healthcare Research and Quality. HCUP-US Home Page. [Accessed April 14, 2016]; http://www.hcupus.ahrq.gov/
- 25.Claassen C. Self Harm In the United States: What We Can Learn from National and State-Level Medical Datasets. [Accessed April 14, 2016];presented at National Center for Health Statistics 2012 Data Conference. http://www.cdc.gov/nchs/ppt/nchs2012/ss-32_claassen.pdf. Published 2012.
- 26.Braithwaite RS, Meltzer DO, King JT, Leslie D, Roberts MS. What does the value of modern medicine say about the $50,000 per quality-adjusted life-year decision rule? Med Care. 2008;46(4):349–356. doi: 10.1097/MLR.0b013e31815c31a7. [DOI] [PubMed] [Google Scholar]
- 27.Claassen CA, Larkin GL. Occult suicidality in an emergency department population. Br J Psychiatry. 2005;186:352–353. doi: 10.1192/bjp.186.4.352. [DOI] [PubMed] [Google Scholar]
- 28.King CA. Emergency Department Screen for Teens at Risk for Suicide (ED-STARS) [Accessed May 8, 2016];NIH RePORTER. https://projectreporter.nih.gov/project_info_description.cfm?aid=8755416&icde=21651658&ddparam=&ddvalue=&ddsub=&cr=3&csb=default&cs=ASC. Published 2014.
- 29.Horowitz LM, Bridge JA, Teach SJ, et al. Ask Suicide-Screening Questions (ASQ): a brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med. 2012;166(12):1170–1176. doi: 10.1001/archpediatrics.2012.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boudreaux ED, Camargo CA, Arias SA, et al. Improving Suicide Risk Screening and Detection in the Emergency Department. Am J Prev Med. 2016;50(4):445–453. doi: 10.1016/j.amepre.2015.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Betz ME, Arias SA, Segal DL, Miller I, Camargo CA, Boudreaux ED. Screening for Suicidal Thoughts and Behaviors in Older Adults in the Emergency Department. J Am Geriatr Soc. 2016;64(10):e72–e77. doi: 10.1111/jgs.14529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang BP, Tan TM. Suicide screening tools and their association with near-term adverse events in the ED. Am J Emerg Med. 2015;33(11):1680–1683. doi: 10.1016/j.ajem.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 33.Beautrais AL, Gibb SJ, Faulkner A, Fergusson DM, Mulder RT. Postcard intervention for repeat self-harm: randomised controlled trial. Br J Psychiatry. 2010;197(1):55–60. doi: 10.1192/bjp.bp.109.075754. [DOI] [PubMed] [Google Scholar]
- 34.National Suicide Prevention Lifeline. Crisis Center Guidance: Follow-up with Callers and Those Discharged from Emergency Department and Inpatient Settings. 2014 http://www.suicidepreventionlifeline.org/media/13576/Lifeline-Follow-Up-Guidance1214.pdf.
- 35.Miller IW, Camargo CA, Arias S, et al. International Summit on Suicide Research. New York, NY: 2016. ED-SAFE Intervention Outcomes Evaluation. [Google Scholar]
- 36.Miller IW, Camargo CA, Arias SA, et al. Suicide Prevention in an Emergency Department Population. JAMA Psychiatry. 2017 Apr; doi: 10.1001/jamapsychiatry.2017.0678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gysin-Maillart A, Schwab S, Soravia L, Megert M, Michel K. A Novel Brief Therapy for Patients Who Attempt Suicide: A 24-months Follow-Up Randomized Controlled Study of the Attempted Suicide Short Intervention Program (ASSIP) PLoS Med. 2016;13(3):e1001968. doi: 10.1371/journal.pmed.1001968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. [Accessed May 19, 2016];National Hospital Ambulatory Medical Care Survey: 2008 Emergency Department Summary Tables. 2008 http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2008_ed_web_tables.pdf.
- 39.Centers for Disease Control and Prevention. [Accessed May 19, 2016];National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. 2011 http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf.
- 40.Parkland Hospital. Parkland News and Updates: More than 150,000 patients screened for suicide risk at Parkland this year. [Accessed March 10, 2017]; http://www.parklandhospital.com/phhs/news-and-updates/more-than-150000-patients-screened-for-suicide-ris-464.aspx.
- 41.Claassen CA. Personal Communication Based on Parkland Hospital Administrative Records, Dallas, TX for June 7–July 24, 2003. 2016 [Google Scholar]
- 42.Pokorny AD. Prediction of suicide in psychiatric patients. Report of a prospective study. [Accessed April 13, 2016];Arch Gen Psychiatry. 1983 40(3):249–257. doi: 10.1001/archpsyc.1983.01790030019002. http://www.ncbi.nlm.nih.gov/pubmed/6830404. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. CDC WONDER. [Accessed November 29, 2015]; http://wonder.cdc.gov/
- 44.Qin P, Nordentoft M. Suicide risk in relation to psychiatric hospitalization: evidence based on longitudinal registers. Arch Gen Psychiatry. 2005;62(4):427–432. doi: 10.1001/archpsyc.62.4.427. [DOI] [PubMed] [Google Scholar]
- 45.American Foundation for Suicide Prevention. Suicide Facts and Figures. [Accessed May 19, 2016]; http://afsp.donordrive.com/index.cfm?fuseaction=cms.page&id=1226&cmsContentSetID=D5C4DC12-C299-258B-B0B6FCF9EF015CE0. Published 2013.
- 46.Centers for Disease Control and Prevention. WISQARS Fatal Injury Reports. [Accessed April 8, 2016];2014 http://webappa.cdc.gov/sasweb/ncipc/mortrate10_us.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.