Abstract
Objectives
To compare emergency hospital use for infants in Ontario (Canada) and England.
Methods
We conducted a population-based data linkage study in infants born ≥34 weeks’ gestation between 2010 and 2013 in Ontario (n=253 930) and England (n=1 361 128). Outcomes within 12 months of postnatal discharge were captured in hospital records. The primary outcome was all-cause unplanned admissions. Secondary outcomes included emergency department (ED) visits, any unplanned hospital contact (either ED or admission) and mortality. Multivariable regression was used to evaluate risk factors for infant admission.
Results
The percentage of infants with ≥1 unplanned admission was substantially lower in Ontario (7.9% vs 19.6% in England) while the percentage attending ED but not admitted was higher (39.8% vs 29.9% in England). The percentage of infants with any unplanned hospital contact was similar between countries (42.9% in Ontario, 41.6% in England) as was mortality (0.05% in Ontario, 0.06% in England). Infants attending ED were less likely to be admitted in Ontario (7.3% vs 26.2%), but those who were admitted were more likely to stay for ≥1 night (94.0% vs 55.2%). The strongest risk factors for admission were completed weeks of gestation (adjusted OR for 34–36 weeks vs 39+ weeks: 2.44; 95% CI 2.29 to 2.61 in Ontario and 1.66; 95% CI 1.62 to 1.70 in England) and young maternal age.
Conclusions
Children attending ED in England were much more likely to be admitted than those in Ontario. The tendency towards more frequent, shorter admissions in England could be due to more pressure to admit within waiting time targets, or less availability of paediatric expertise in ED. Further evaluations should consider where best to focus resources, including in-hospital, primary care and paediatric care in the community.
Keywords: emergency department, health services research, hospital medicine, paediatrics, healthcare quality improvement
Background
Paediatric emergency admissions in England have risen by a third over the past decade and are continuing to rise.1 2 For serious conditions, admissions are necessary and appropriate. However, the majority of unplanned admissions within the first year of life are for minor conditions, particularly minor infections, which could be treated outside hospital.1 3 Responding to infant illness in ways that avoid emergency admission could help reduce inconvenience to families (eg, emotional distress, interruption of work or school) and the risk of iatrogeny (eg, hospital-acquired infection or medical errors). However, there is a lack of evidence on the best approaches to reducing unplanned infant admissions.4
Analyses of trends over time in admission rates have provided important insights into how changes to policy influence paediatric healthcare use (eg, how UK primary care policy reforms aimed at improving working conditions for physicians and outcomes for patients are related to increasing rates of short-stay paediatric admissions).1 5 Comparisons of healthcare use in different settings provide further opportunities to identify determinants of variation in service use.6 Specifically, Ontario (Canada’s largest province) and England have similar cultural and environmental risk factors and similar levels of child poverty.7 Both countries offer universal healthcare systems, with no user fees at the point of care. General practitioners (GPs) also operate similar gatekeeper functions in both countries, referring families to hospital where appropriate. However, important organisational differences between these jurisdictions provide an opportunity to understand how different policies and service provision may contribute to paediatric acute healthcare use.
For example, although most of the Ontario population has a primary care provider, access to a doctor out of hours without attending emergency department (ED) is very low in comparison to other OECD (Organisation for Economic Co-operation and Development) countries.8 Primary care reform in Ontario has attempted to improve access through incentives aimed at general/family practitioners, although children also receive primary care from paediatricians (predominantly in urban centres).9 There are also differences in postnatal support during early infancy: all families in England are supported by home visiting by qualified midwives and health visitors, whereas follow-up is less well established in Ontario, where only 9% of pregnant mothers are cared for by a midwife and less than 35% of low-risk newborns receive the recommended follow-up visit in the first week of life.10–12 While Canada has a well-established history of paediatric emergency medicine (PEM) in tertiary centres and a system of consultant paediatricians in the ED in large community hospitals,13 consultant PEM provision in the UK varies regionally, and is only recommended for emergency care settings seeing more than 16 000 children per year (around half of EDs in the UK).14 Finally, ED wait time targets also differ between countries: in England, 95% of patients attending an ED should be seen, treated, admitted or discharged in under 4 hours (98% prior to 2010), whereas in Ontario, 90% of ED visits for patients with only minor or uncomplicated conditions are expected to be completed within 4 hours.
We performed an in-depth comparison of emergency hospital use during infancy, a time of high need for acute care, within which admissions may be avoidable, and a time when neonatal morbidity and social risk factors may be especially important. We evaluated both inpatient admissions and ED visits in order to gain an overall picture of hospital contact. We aimed to identify differences in patterns of hospital use and maternal and neonatal risk factors, based on standardised birth cohorts of healthy populations, derived from linked administrative hospital data.
Methods
Data sources
We extracted data for Ontario from linked population-based administrative databases at the Institute for Clinical and Evaluative Sciences in Toronto.15 Eligible mothers and infants were identified from the Registered Persons Database, which holds information on all Ontario residents (currently over 13 million) with a provincial health card number. Linked maternal and newborn health records were extracted from the MOMBABY dataset, which provides information on all births in hospitals in Ontario and is linked using a unique health card number. Inpatient admissions and ED visits were extracted for all hospitals providing acute inpatient facilities in Ontario from the Canadian Institute of Health Information Discharge Abstract Database and the National Ambulatory Care Reporting System Database.
For England, data were extracted from Hospital Episode Statistics (HES).16 HES is an administrative database holding detailed information for all admissions to National Health Service (NHS) hospitals in England. Maternal and baby birth characteristics were linked using non-identifiable clinical and demographic information available on the main HES record (including admission dates, postcode district and GP practice) and delivery information contained in the ‘baby tail’ (including gestational age, birth weight and mode of delivery). Full details of the linkage have been published elsewhere.17 Inpatient admissions and ED visits were extracted from the Admitted Patient Care dataset and the Accident & Emergency dataset.
For both countries, hospital records are collected for reimbursement purposes, and are encoded, allowing admissions for the same patient to be tracked over time. Admission records allow the entry of multiple fields of clinical diagnoses (24 fields in Ontario, 20 in England) coded using the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10).
Study population
Our study population comprised newborns alive at postnatal discharge. Newborns <34 weeks’ gestation were excluded due to their more complex health needs (1.8% of births in Ontario and 1.7% of births in England). Since we knew that gestational age distributions differed between countries, and expected that gestational age would be strongly predictive of healthcare contact, we stratified results by late-preterm (34–36 weeks), early-term (37–38 weeks) or full-term (39+ weeks) births.
We focused our analysis on data on births from April 2010 onwards, as ED data were not available in England prior to this time. Follow-up data were complete until March 2014 for all births before 1 March 2013. We therefore included births between 1 April 2010 and 1 March 2013. We also plotted trends in admissions from April 2005 onwards.
For mothers with multiple deliveries during the study period, we randomly selected one delivery for inclusion in analyses, to avoid clustering of outcomes by mother. We excluded infants with missing gestation or birth weight or suspected coding errors (birth weight >4 SDs from the average according to published reference values for each country).18 19 For England, the percentage of births excluded due to missing values ranged from 10% in 2010/2011 to 7% in 2012/2013. The level of missing data in the Ontario data was negligible (<1%).
Outcomes
All outcomes were captured in hospital records up to 12 months from postnatal discharge. The primary outcome was the percentage of infants with one or more unplanned admissions. Admissions were defined as unplanned based on the method of admission coded within the hospital record, and were defined as episodes of care starting more than 2 days following the end of a previous admission. Transfers between hospitals were not counted as readmissions.
We also evaluated a number of secondary outcomes. We compared ED visits to any hospital (with or without subsequent admission). For England, ED data were provided for all NHS hospitals included in the study population (n=152), but reliable ED diagnosis data were not available.
To measure overall hospital contact, we compared the percentage of infants with any emergency contact (unplanned admission or ED) and the total number of inpatient days from unplanned admissions (both including and excluding the birth episode). We also compared postdischarge deaths.
A further secondary outcome was overnight admissions, where infants were admitted and discharged on different days (ie, admissions starting and ending on the same day were excluded). Finally, we compared the number of unplanned admissions for different diagnosis groups, based on the 10 most frequently occurring ICD-10 code groups in the main diagnosis fields for admission records in each country.
Risk factors
Gestational age in completed weeks was obtained from the linked maternal-baby data, based on best estimates from menstrual dates or ultrasound. Small or large for gestation (<10th or >90th percentile of birth weight for gestation) was derived from national birth weight percentiles.18 19 Delivery by caesarean section, sex, multiple birth, admission to neonatal intensive care, season of discharge and maternal age were considered as additional covariates. Measures of deprivation were obtained via postal code of residence mapped to neighbourhood income quintile in Ontario, and Index of Multiple Deprivation (IMD) for England.20 Based on code lists used in previous studies, we also derived a number of pregnancy, delivery and neonatal risk factors using ICD-10 codes recorded in any diagnosis field during the birth episode or pregnancy (see table 1 and online supplementary appendix table 1 for code lists).21 22 We explored trends by including a variable for quarterly trend, that is, taking values of 1–12 for each quarter year of postnatal discharge between April 2010 and March 2013. We also plotted outcomes by quarter. Due to the size of the datasets, p values for differences in outcomes between countries were not presented, as all comparisons were statistically significant at the 95% confidence level.
Table 1.
Characteristics of mothers and live births between 2010 and 2013 by country
| Ontario (n=253 930) | England (n=1 361 128) | ||||
| N | % | N | % | ||
| Gestational age group | Full term (39+ weeks) | 170 445 | 67.1 | 1 047 532 | 77.0 |
| Early term (37–38 weeks) | 69 349 | 27.3 | 250 029 | 18.4 | |
| Late preterm (34–36 weeks) | 14 136 | 5.6 | 63 567 | 4.7 | |
| Birth weight | <1500 | 140 | 0.1 | 1125 | 0.1 |
| 1500–<2500 | 10 817 | 4.3 | 63 319 | 4.7 | |
| 2500–<4000 | 216 777 | 85.4 | 1 141 544 | 83.9 | |
| 4000+ | 26 196 | 10.3 | 155 140 | 11.4 | |
| Size for gestation | Small (<10th percentile) | 25 825 | 10.2 | 120 322 | 8.8 |
| Normal | 204 271 | 80.4 | 1 103 893 | 81.1 | |
| Large (>10th percentile) | 23 834 | 9.4 | 136 913 | 10.1 | |
| Maternal age (years) | <20 | 9439 | 3.7 | 78 659 | 5.8 |
| 20–24 | 31 974 | 12.6 | 255 986 | 18.9 | |
| 25–29 | 70 759 | 27.9 | 375 835 | 27.7 | |
| 30–34 | 85 016 | 33.5 | 385 700 | 28.4 | |
| 35–39 | 45 448 | 17.9 | 207 269 | 15.3 | |
| 40+ | 11 291 | 4.4 | 54 021 | 4.0 | |
| Female infant | 123 937 | 48.8 | 663 798 | 48.8 | |
| Multiple birth | 4618 | 1.8 | 19 973 | 1.5 | |
| Primiparous mother | 133 167 | 52.4 | 661 402 | 48.6 | |
| Income/deprivation quintile | Most deprived: 1 | 55 945 | 22.0 | 266 211 | 19.8 |
| 2 | 50 818 | 20.0 | 269 664 | 20.1 | |
| 3 | 50 472 | 19.9 | 268 799 | 20.0 | |
| 4 | 51 914 | 20.4 | 270 125 | 20.1 | |
| Least deprived: 5 | 39 121 | 15.4 | 267 068 | 19.9 | |
| Newborn length of stay (days) | <2 | 97 728 | 38.5 | 727 461 | 53.5 |
| 2–6 | 147 294 | 58.0 | 577 452 | 42.4 | |
| 7+ | 8908 | 3.5 | 56 215 | 4.1 | |
| Caesarean section | 74 067 | 29.2 | 319 194 | 23.5 | |
| Neonatal ICU | 26 463 | 10.4 | 148 957 | 10.9 | |
| Delivery risk factor (Any) | 33 959 | 13.4 | 37 062 | 10.1 | |
| Hypoxia | 1242 | 0.5 | 78 894 | 5.8 | |
| Amniotic fluid embolism | 14 | 0.0 | 18 | 0.0 | |
| Placental transfusion syndrome | 61 | 0.0 | 203 | 0.0 | |
| Umbilical cord prolapse | 27 780 | 10.9 | 19 374 | 1.4 | |
| Chorioamnionitis | 2270 | 0.9 | 2412 | 0.2 | |
| Fetal haemorrhage | 358 | 0.1 | 5783 | 0.4 | |
| Birth trauma | 1748 | 0.7 | 39 313 | 2.9 | |
| Complications of delivery | 1688 | 0.7 | 18 244 | 1.3 | |
| Umbilical cord problem | 888 | 0.3 | 2871 | 0.2 | |
| Pregnancy risk factor (Any) | 31 103 | 12.2 | 49 687 | 11.0 | |
| Previous intrauterine fetal death | 21 | 0.0 | 139 | 0.0 | |
| Eclampsia | 2858 | 1.1 | 31 084 | 2.3 | |
| Gestational hypertension | 11 911 | 4.7 | 79 576 | 5.9 | |
| Diabetes in pregnancy | 15 405 | 6.1 | 53 170 | 3.9 | |
| Placental abruption or infarction | 3211 | 1.3 | 14 468 | 1.1 | |
| Uterine rupture | 226 | 0.1 | 679 | 0.1 | |
| Neonatal medical condition (Any) | 10 478 | 4.1 | 59 818 | 4.4 | |
| Congenital anomaly | 5884 | 2.3 | 24 763 | 1.8 | |
| Perinatal infection | 1876 | 0.7 | 29 093 | 2.1 | |
| Neonatal abstinence syndrome | 1024 | 0.4 | 2504 | 0.2 | |
| Respiratory distress syndrome | 2924 | 1.2 | 9405 | 0.7 | |
ICU, intensive care unit.
bmjqs-2016-006253supp001.docx (19.9KB, docx)
Statistical analysis
The risk of one or more admissions or ED visits was modelled using multilevel logistic regression, allowing for clustering within healthcare provider at postnatal discharge (hospital for Ontario and NHS Trust for England were included as random effects). In models for admission or ED visits, infants who died within 12 months post discharge were treated as having the outcome. Adjusted ORs (aOR) were used to compare the risk of admission or ED visit according to common risk factors within each country. To allow us to assess the impact of common risk factors on outcomes in each country, all predefined variables were retained in models, irrespective of statistical significance.
Sharing of record-level data outside of each country was not permitted, and we could not incorporate a ‘country’ variable within our models. Instead, we separately modelled data within each country. However, this allowed us to explore the impact of risk factors within each country, without making assumptions about similarity of coding. For example, deprivation was derived from income quintile in Ontario (ie, a direct measure of income) and IMD in England (ie, a measure of material deprivation). Separate models allowed us to compare the impact of being in the lowest versus highest quintile within each country. Analyses were performed in Stata V.14.23
Results
A total of 253 930 (Ontario) and 1 361 128 (England) mother–baby dyads were included in the study (table 1). Characteristics of mothers and infants were broadly similar between countries, with a few exceptions: Ontario had a greater proportion of early-term and late-preterm births, more births by caesarean section and fewer young mothers (table 1).
The percentage of infants with at least one unplanned admission within 12 months of postnatal discharge was substantially lower in Ontario (7.9% vs 19.6% in England, table 2 and figure 1), while the percentage of infants attending ED but not being admitted was much higher (39.8% vs 29.9% in England). ED visits were much less likely to result in an admission in Ontario (7.3% of ED visits resulted in an admission vs 26.2% in England), and were of a slightly longer duration (median 2 hours 5 min vs 1 hour 49 min in England). The percentage of unplanned admissions admitted via ED was similar in both countries (66.1% in Ontario, 67.9% in England), while the percentage recorded as being admitted via a physician or GP was slightly lower in Ontario (23.6% vs 29.1% in England).
Table 2.
Infant outcomes within 12 months post discharge, by gestational age group and country, for births between 2010 and 2013
| N (%) infants with ≥1 event to 12 months postnatal discharge | Mean inpatient days per infant to 12 months postnatal discharge | ||||||||
| All-cause admission | Overnight admission* | ED visit not admitted | Any ED visit | Any contact (admission or ED) | Mortality | From postnatal discharge | From day of birth | ||
| Total | Ontario n=253 930 |
20 016 | 18 954 | 101 060 | 105 661 | 108 903 | 139 | 0.3 | 2.7 |
| (7.9) | (7.5) | (39.8) | (41.6) | (42.9) | (0.05) | ||||
| England n=1 361 128 |
266 771 | 160 690 | 407 331 | 491 991 | 565 896 | 837 | 0.6 | 2.8 | |
| (19.6) | (11.8) | (29.9) | (36.2) | (41.6) | (0.06) | ||||
| Full term (39+ weeks) |
Ontario n=170 445 |
11 178 | 10 524 | 66 634 | 69 351 | 70 910 | 67 | 0.2 | 2.2 |
| (6.6) | (6.2) | (39.1) | (40.7) | (41.6) | (0.04) | ||||
| England n=1 047 532 |
189 921 | 112 235 | 307 362 | 368 752 | 421 097 | 506 | 0.5 | 2.4 | |
| (18.1) | (10.7) | (29.3) | (35.2) | (40.2) | (0.05) | ||||
| Early term (37–38 weeks) | Ontario n=69 349 |
6929 | 6601 | 28 270 | 29 805 | 31 102 | 54 | 0.4 | 2.8 |
| (10.0) | (9.5) | (40.8) | (43.0) | (44.9) | (0.08) | ||||
| England n=250 029 |
58 343 | 36 309 | 79 005 | 96 726 | 113 116 | 215 | 0.7 | 3.3 | |
| (23.3) | (14.5) | (31.6) | (38.7) | (45.3) | (0.09) | ||||
| Late preterm (34–36 weeks) | Ontario n=14 136 |
1909 | 1829 | 6505 | 6891 | 6156 | 18 | 0.6 | 7.7 |
| (13.5) | (12.9) | (46.0) | (48.8) | (43.6) | (0.19) | ||||
| England n=63 567 |
18 507 | 12 146 | 20 964 | 26 513 | 31 683 | 116 | 1.2 | 8.2 | |
| (29.1) | (19.1) | (33.0) | (41.7) | (49.9) | (0.18) | ||||
*All-cause admission excluding those admitted and discharged on the same day.
ED, emergency department.
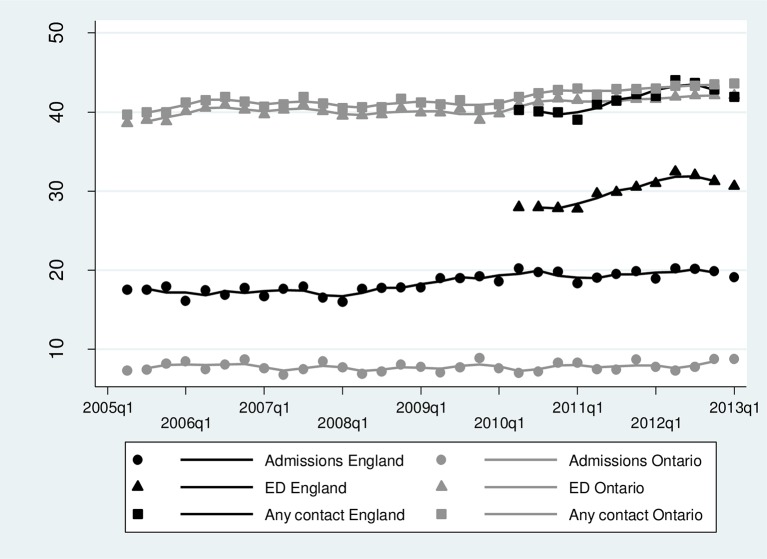
Figure 1.
Trends in the percentage of infants with ≥1 unplanned admission, ED visit or any contact (admission or ED) within 12 months of postnatal discharge. Symbols=observed rates; lines=three-quarter moving average. ED, emergency department.
Overall hospital contact during infancy was similar between countries: the percentage of infants with either unplanned admission or ED attendance was 42.9% in Ontario and 41.6% in England. Mortality was also the same in both countries (0.05% in Ontario, 0.06% in England).
Infants who were admitted were more likely to stay for ≥1 night in Ontario (94.0% vs 55.2% in England) and have longer admissions (median 3.9 days compared with 2.2 days in England). However, due to the greater number of admissions, mean inpatient days per infant post discharge in England were almost double those in Ontario (table 2).
Rates of unplanned admissions and ED visits were increasing over time in both countries, but to a greater extent in England (figure 1, table 3). Other risk factors for infant admission were of similar magnitudes in both countries, with the exception of caesarean section and newborn length of stay (table 3). Gestational age at birth was the most important risk factor for infant admission: aORs for infants born late preterm (34–36 weeks) were 2.44 (95% CI 2.29 to 2.61) in Ontario and 1.66 (95% CI 1.62 to 1.70) in England, compared with full-term babies (39+ weeks) (table 3). Young maternal age (<20 years) was highly predictive of infant admission (aOR 1.36, 95% CI 1.26 to 1.46 in Ontario; 1.49, 95% CI 1.46 to 1.52 in England; table 3) and ED visits (see online supplementary appendix table 2). Deprivation was also an important risk factor in both countries, particularly for ED visits (see online supplementary appendix table 2).
Table 3.
Risk factors for unplanned hospital admission in infants in England and Ontario, 2010–2013
| Ontario | England | ||||
| OR (95% CI) | p Value | OR (95% CI) | p Value | ||
| Gestational age at birth (weeks) | Full term (39+) | 1 | <0.001 | 1 | <0.001 |
| Early term (37-38) | 1.64 (1.59 to 1.70) | 1.39 (1.37 to 1.40) | |||
| Late preterm (34-36) | 2.44 (2.29 to 2.61) | 1.66 (1.62 to 1.70) | |||
| Newborn length of stay (days) | <2 | 1 | 0.024 | 1 | <0.001 |
| 2–6 | 1.02 (0.98 to 1.06) | 1.08 (1.07 to 1.10) | |||
| 7–13 | 0.91 (0.83 to 1.00) | 1.38 (1.34 to 1.41) | |||
| Size for gestation | Small (<10th percentile) | 1.02 (0.98 to 1.03) | <0.001 | 1.07 (1.05 to 1.09) | <0.001 |
| Normal | 1 | 1 | |||
| Large (>90th percentile) | 1.06 (1.01 to 1.12) | 1.00 (0.98 to 1.01) | |||
| Maternal age (years) | ≤19 | 1.36 (1.26 to 1.46) | <0.001 | 1.49 (1.46 to 1.52) | <0.001 |
| 20–24 | 1.18 (1.12 to 1.24) | 1.20 (1.19 to 1.22) | |||
| 25–29 | 1 | 1 | |||
| 30–34 | 0.96 (0.93 to 1.00) | 0.90 (0.89 to 0.91) | |||
| 35–39 | 0.95 (0.91 to 1.00) | 0.83 (0.82 to 0.84) | |||
| ≥40 | 0.95 (0.88 to 1.03) | 0.82 (0.80 to 0.84) | |||
| Female sex | 0.79 (0.76 to 0.81) | <0.001 | 0.80 (0.80 to 0.81) | <0.001 | |
| Primiparous mother | 0.92 (0.89 to 0.95) | <0.001 | 0.89 (0.88 to 0.90) | <0.001 | |
| Multiple birth | 0.66 (0.59 to 0.74) | <0.001 | 0.81 (0.78 to 0.84) | <0.001 | |
| Deprivation quintile | Most deprived | 1.12 (1.06 to 1.17) | <0.001 | 1.03 (1.01 to 1.04) | <0.001 |
| 2 | 1.05 (1.00 to 1.10) | 1.01 (1.00 to 1.03) | |||
| 3 | 1.06 (1.00 to 1.11) | 1.01 (0.99 to 1.02) | |||
| 4 | 1.06 (1.00 to 1.11) | 0.99 (0.98 to 1.00) | |||
| Most affluent | 1 | 1 | |||
| Caesarean section | 0.77 (0.74 to 0.80) | <0.001 | 1.04 (1.02 to 1.05) | <0.001 | |
| Admission to neonatal intensive care | 1.03 (0.98 to 1.09) | 0.232 | 1.03 (1.01 to 1.05) | <0.001 | |
| Season of discharge | January to March | 1 | <0.001 | 1 | <0.001 |
| April to June | 0.89 (0.85 to 0.93) | 1.08 (1.07 to 1.10) | |||
| July to September | 0.91 (0.87 to 0.95) | 1.08 (1.07 to 1.10) | |||
| October to December | 1.06 (1.02 to 1.11) | 1.08 (1.06 to 1.09) | |||
| Quarter year of discharge | 1.01 (1.01 to 1.02) | <0.001 | 1.00 (1.00 to 1.00) | <0.001 | |
| Perinatal infection | 1.09 (0.94 to 1.28) | 0.249 | 1.09 (1.06 to 1.12) | <0.001 | |
| Prematurity related risk factor | 0.87 (0.77 to 0.99) | 0.033 | 1.01 (0.96 to 1.06) | 0.715 | |
| Neonatal medical condition | 1.82 (1.68 to 1.97) | <0.001 | 1.84 (1.79 to 1.89) | <0.001 | |
| Pregnancy risk factor | 1.07 (1.02 to 1.12) | 0.003 | 1.00 (.099 to 1.03) | 0.525 | |
| Delivery risk factor | 1.01 (0.97 to 1.06) | 0.605 | 1.01 (1.00 to 1.03) | 0.112 | |
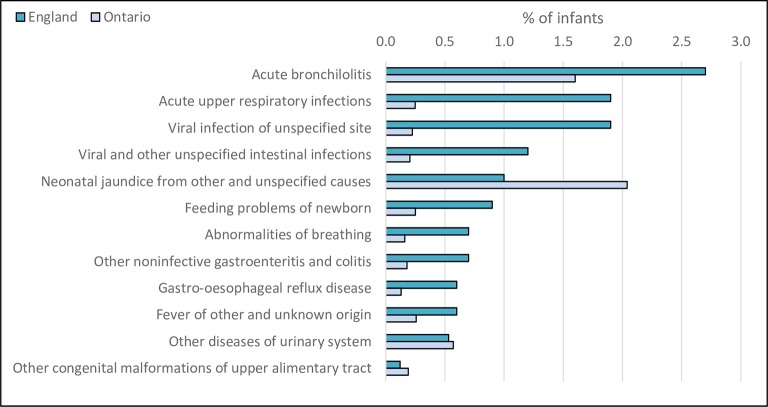
The most frequently occurring admission diagnoses in both countries were acute upper respiratory tract infections, bronchiolitis and viral infections (figure 2). Despite lower admission rates overall, the percentage of infants readmitted with neonatal jaundice was substantially higher in Ontario compared with England.
Figure 2.
Most frequently occurring diagnoses from unplanned admissions within 12 months of postnatal discharge.
Discussion
Our study illustrates the complexities of international comparisons of hospital use. Despite similar health service provision and standardised cohorts of healthy babies in our study populations, focusing solely on the inpatient setting would have revealed substantially higher levels of emergency hospital use in England compared with Ontario. However, by considering both inpatient admissions and ED visits, we showed that overall hospital contact (either ED or admission) and total inpatient days from birth to 12 months were similar across countries. We found different patterns of hospital use that suggest variation in admission thresholds between countries: in Ontario, infants seen in EDs were much less likely to be admitted compared with those in England, while infants admitted in England were more often discharged on the same day as admission.
Infant admission rates observed in our study were low for Ontario (7.9%) and relatively high for England (19.6%) compared with those reported in Australia (15%–20%) and the USA (8%–12%).24–27 There are various contributing factors that might explain the differences in hospitalisation patterns between the two countries in our study, including differences in primary or secondary care practice, or in the underlying population.28 Although we could not directly assess the role of primary care in either country, data suggested that the percentage of infants admitted via a physician or GP was slightly higher in England (29.1% vs 23.6%). Our study populations reflect official statistics published in each jurisdiction and demonstrate some important differences between populations: Ontario has fewer young mothers,29 30 more births by caesarean section31 32 and a greater proportion of early-term births.33 34 Although the greater number of infants born early in Ontario was not reflected in an overall higher admission rate during infancy, jaundice (an early outcome associated with early-term birth) appeared to be a greater problem in Ontario.24 35
Another possible explanation for differences in admission rates between countries is the availability of trained emergency paediatricians in ED. Although we could not directly measure this in our study, consultant PEM is better established in Canada than England.13 14 Only one study has evaluated the effectiveness of PEM provision, finding that increased consultant provision was associated with lower admission rates.36 Further research is needed to determine whether increasing emergency paediatrician provision in EDs in England could reduce the numbers of infants admitted for short-stay emergency admissions, or whether this could better be achieved through more efficient management of children with acute illnesses within the community.2 5 28
Differences in ED wait time targets between countries may also have contributed to differences in admission rates. Implementation of ED waiting time targets in the NHS has resulted in increased pressure to admit, and a marked increase in admissions just before the 4-hour cut-off.37 Targets may also have altered health-seeking behaviours, motivating families to seek ED review rather than wait for an appointment with a GP.38 This was reflected in increasing ED attendance rates over time in both countries. In our study, ‘zero-day’ admissions were much more common in England (45% of admissions were admitted and discharged on the same day compared with 6% in Ontario). Pressure to admit from ED explains some but not all of this difference: in England, 50% of admissions with a preceding ED visit were discharged on the same day, compared with 38% of admissions without a preceding ED visit. Greater travel distances in Ontario may also have a role in explaining the greater proportion of overnight admissions. For example, clinicians in Ontario may choose to admit an infant overnight rather than send them on a long late-night journey. Data were not available to test this within our study.
Further research is needed to determine whether service provision is more effective in Ontario or England. Hospital admission increases exposure to nosocomial infection, medical error and adverse drug reactions, and can contribute to psychological distress, disruption, or economic loss for children and/or their families.39–41 Reducing unplanned admissions has the potential to improve quality of life for children and their families, as well as alleviating pressure on hospital resources, and is recognised as an important indicator of quality by the NHS Outcomes Framework.42 However, there is a complex relationship between relevant outcomes for children and their families, and primary care access, ED attendances and short-stay admissions, and it is unclear where best to focus investment.38 43 44
As with all studies based on data collected for purposes other than research, careful interpretation of observed differences is required, taking into account the implications of any variation in data quality or coding practices.45 A limitation of this study was the level of missing data on gestational age or birth weight in the English data, which led to the exclusion of some records. However, the representativeness of the study population that did have complete data, means that missing data are unlikely to have led to substantial biases. A lack of validation of risk-factor codes could have led to some misclassification, for example, on capturing congenital anomalies or admission to neonatal intensive care. Although gestational age should be recorded in the same way in both countries (estimated from either ultrasound or last menstrual period), there may be differences in derivation between countries that could have led to misclassification. Since measures of socioeconomic status were different in each country, adjustments within countries were made assuming that differences between quintiles (of either income or multiple deprivation) were similar. However, recording of admission and ED patterns, based on event data, is likely to be accurate. A further limitation of our study was a lack of information on general practice and out-of-hospital care. Health-seeking behaviour appeared similar between countries, with the proportion of families visiting EDs being slightly higher in Ontario. We were unable to assess staffing provision or supply of hospital beds.
Administrative data provide a powerful tool for determining how service use varies between countries with similar cultural and environmental risk factors, identifying policy areas that could be compared, and generating hypotheses about how organisational-level factors and service provision contribute to outcomes.6 46 Our study in particular demonstrates the importance of incorporating detailed information on both maternal and baby characteristics and complete healthcare trajectories for exploring variation in emergency care.17 In Ontario, linkage was facilitated by a population spine (the Registered Person database). No such spine currently exists for England, although linkage of prospective maternity data is being developed by NHS Digital for the Maternity and Children’s Dataset.17 47 Further research on the burden of recurrent admissions in both countries would support policymakers to consider the comparative effectiveness and cost-effectiveness of focusing paediatric expertise in ED versus inpatient settings and primary care.
Footnotes
Contributors: KH performed the analysis and wrote the first draft of the manuscript. All authors contributed to interpretation of results and critically revising the manuscript.
Funding: This study is funded by Wellcome Trust [103975/Z/14/Z] and supported by the Economic and Social Research Council through the Administrative Data Research Centre for England, University of Southampton (ES/L007617/1).
Competing interests: None declared.
Ethics approval: Approvals for the use of HES data were obtained as part of the standard Hospitals Episode Statistics approval process. Hospital Episode Statistics were made available by NHS Digital (Copyright © 2012, Re-used with the permission of NHS Digital. All rights reserved.) The study is exempt from UK NREC approval because it involved the analysis of an existing dataset of anonymous data for service evaluation. ICES datasets were linked using unique encoded identifiers and analysed at the Institute for Clinical Evaluative Sciences (ICES). Parts of this material are based on data and information compiled and provided by CIHI. However, the analyses, conclusions, opinions and statements expressed herein are those of the author, and not necessarily those of CIHI. Use of ICES data for this study was approved by the Institutional Review Board at Sunnybrook Health Sciences Centre, Toronto, Canada.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: HES data are available on application to the NHS Digital (https://digital.nhs.uk/). Publicly funded, not- for-profit researchers, students, policymakers or knowledge users can apply to use ICES data (www.ices.on.ca/Data-Services/Data-Process).
Correction notice: This paper has been amended since it was published Online First. Owing to a scripting error, some of the publisher names in the references were replaced with ’BMJ Publishing Group'. This only affected the full text version, not the PDF. We have since corrected these errors and the correct publishers have been inserted into the references.
References
- 1. Saxena S, Bottle A, Gilbert R, et al. Increasing short-stay unplanned hospital admissions among children in England; time trends analysis '97-'06. PLoS One 2009;4:e7484 10.1371/journal.pone.0007484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gill PJ, Goldacre MJ, Mant D, et al. Increase in emergency admissions to hospital for children aged under 15 in England, 1999-2010: national database analysis. Arch Dis Child 2013;98:328–34. 10.1136/archdischild-2012-302383 [DOI] [PubMed] [Google Scholar]
- 3. Wijlaars LP, Hardelid P, Woodman J, et al. Who comes back with what: a retrospective database study on reasons for emergency readmission to hospital in children and young people in England. Arch Dis Child 2016;101:714–8. 10.1136/archdischild-2015-309290 [DOI] [PubMed] [Google Scholar]
- 4. Coon JT, Martin A, Abdul-Rahman AK, et al. Interventions to reduce acute paediatric hospital admissions: a systematic review. Arch Dis Child 2012;97:304–11. 10.1136/archdischild-2011-301214 [DOI] [PubMed] [Google Scholar]
- 5. Cecil E, Bottle A, Sharland M, et al. Impact of UK primary care policy reforms on short-stay unplanned hospital admissions for children with primary care-sensitive conditions. Ann Fam Med 2015;13:214–20. 10.1370/afm.1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Australian Institute of Health and Welfare. A working guide to international comparisons of health. Canberra: AIHW, 2012. PHE 159. [Google Scholar]
- 7. Menchini L, Chzhen Y, Main G, et al. Relative income poverty among children in rich countries. 2012.
- 8. Osborn R, Moulds D, Schneider EC, et al. Primary care physicians in ten countries report challenges caring for patients with complex health needs. Health Aff 2015;34:2104–12. 10.1377/hlthaff.2015.1018 [DOI] [PubMed] [Google Scholar]
- 9. Guttmann A, Gandhi S, Hanvey P, et al. Section 3: primary Health Care Services for Children and Youth in Canada: access, Quality and structure: In The Health of Canada’s Children and Youth: A CICH Profile, 2017. [Google Scholar]
- 10. Society CP, detection G. Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants (35 or more weeks' gestation) - summary. Paediatr Child Health 2007;12:401–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Darling EK, Ramsay T, Manuel D, et al. Association of universal bilirubin screening with socioeconomic disparities in newborn follow-up. Acad Pediatr 2017;17:135–43. 10.1016/j.acap.2016.07.009 [DOI] [PubMed] [Google Scholar]
- 12. Kurtz Landy C, Sword W, Ciliska D. Urban women’s socioeconomic status, health service needs and utilization in the four weeks after postpartum hospital discharge: findings of a Canadian cross-sectional survey. BMC Health Serv Res 2008;8:1–9. 10.1186/1472-6963-8-203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McGillivray D, Jarvis A. A history of paediatric emergency medicine in Canada. Paediatr Child Health 2007;12:453–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Davies FC, Newton T. Paediatric emergency medicine consultant provision in the UK: are we there yet? Arch Dis Child 2015;100:1016–7. 10.1136/archdischild-2015-308952 [DOI] [PubMed] [Google Scholar]
- 15. Williams TA, Dobb GJ, Finn JC, et al. Data linkage enables evaluation of long-term survival after intensive care. Anaesth Intensive Care 2006;34:307–15. [DOI] [PubMed] [Google Scholar]
- 16. Herbert A, Wijlaars L, Zylbersztejn A, et al. Data Resource Profile: Hospital Episode Statistics Admitted Patient Care (HES APC). Int J Epidemiol. In Press 2017. 10.1093/ije/dyx015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harron K, Gilbert R, Cromwell D, et al. Linking data for mothers and babies in de-identified electronic health data. PLoS One 2016;11:e0164667 10.1371/journal.pone.0164667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kramer MS, Platt RW, Wen SW, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics 2001;108:e35 10.1542/peds.108.2.e35 [DOI] [PubMed] [Google Scholar]
- 19. Cole TJ, Statnikov Y, Santhakumaran S, et al. Birth weight and longitudinal growth in infants born below 32 weeks' gestation: a UK population study. Arch Dis Child Fetal Neonatal Ed 2014;99:F34–40. 10.1136/archdischild-2012-303536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Office of the Deputy Prime Minister The English Indices of Deprivation 2004, 2003. [Google Scholar]
- 21. Unterscheider J, Daly S, Geary MP, et al. Optimizing the definition of intrauterine growth restriction: the multicenter prospective PORTO Study. Am J Obstet Gynecol 2013;208:290 e1-90.e6 10.1016/j.ajog.2013.02.007 [DOI] [PubMed] [Google Scholar]
- 22. Ray JG, Vermeulen MJ, Schull MJ, et al. Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet 2005;366:1797–803. 10.1016/S0140-6736(05)67726-4 [DOI] [PubMed] [Google Scholar]
- 23. Stata Statistical Software: release 14[program]. College Station, TX: StataCorp LP 2015. [Google Scholar]
- 24. Lain SJ, Nassar N, Bowen JR, et al. Risk factors and costs of hospital admissions in first year of life: a population-based study. J Pediatr 2013;163:1014–9. 10.1016/j.jpeds.2013.04.051 [DOI] [PubMed] [Google Scholar]
- 25. Bird TM, Bronstein JM, Hall RW, et al. Late preterm infants: birth outcomes and health care utilization in the first year. Pediatrics 2010;126:e311–19. 10.1542/peds.2009-2869 [DOI] [PubMed] [Google Scholar]
- 26. McLaurin KK, Hall CB, Jackson EA, et al. Persistence of morbidity and cost differences between late-preterm and term infants during the first year of life. Pediatrics 2009;123:653–9. 10.1542/peds.2008-1439 [DOI] [PubMed] [Google Scholar]
- 27. Colvin L, Bower C. A retrospective population-based study of childhood hospital admissions with record linkage to a birth defects registry. BMC Pediatr 2009;9:1–13. 10.1186/1471-2431-9-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ogilvie D. Hospital based alternatives to acute paediatric admission: a systematic review. Arch Dis Child 2005;90:138–42. 10.1136/adc.2003.035543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Office for National Statistics Birth Summary Tables - England and Wales. [Google Scholar]
- 30. Statistics Canada. CANSIM Table 102-4503 - Live births, by age of mother, Canada, provinces and territories, Annual.
- 31. The Information Centre. Hospital Episode Statistics: nhs Maternity Statistics, 2010-2011, 2011. [Google Scholar]
- 32. Public Health Agency of Canada. perinatal health indicators for Canada A report from the Canadian Perinatal Surveillance System, 2013. [Google Scholar]
- 33. Office for National Statistics Gestation-specific Infant Mortality, 2012, 2014. [Google Scholar]
- 34. Statistics Canada. CANSIM Table 102-4512 - Live births, by weeks of gestation and sex, Canada, provinces and territories, Annual.
- 35. Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 2008;371:261–9. 10.1016/S0140-6736(08)60136-1 [DOI] [PubMed] [Google Scholar]
- 36. Geelhoed GC, Geelhoed EA. Positive impact of increased number of emergency consultants. Arch Dis Child 2008;93:62–4. 10.1136/adc.2007.122531 [DOI] [PubMed] [Google Scholar]
- 37. Mooney H. Admissions from emergency departments rise as four hour target approaches. BMJ 2009;339:b4931 10.1136/bmj.b4931 [DOI] [Google Scholar]
- 38. Cowling TE, Soljak MA, Bell D, et al. Emergency hospital admissions via accident and emergency departments in England: time trend, conceptual framework and policy implications. J R Soc Med 2014;107:432–8. 10.1177/0141076814542669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rennick JE, Johnston CC, Dougherty G, et al. Children’s psychological responses after critical illness and exposure to invasive technology. J Dev Behav Pediatr 2002;23:133–44. 10.1097/00004703-200206000-00002 [DOI] [PubMed] [Google Scholar]
- 40. Forgey M, Bursch B. Assessment and management of pediatric iatrogenic medical trauma. Curr Psychiatry Rep 2013;15:340 10.1007/s11920-012-0340-5 [DOI] [PubMed] [Google Scholar]
- 41. Flores G. Preventing hospitalisations for children. Lancet 2005;365:201–2. 10.1016/S0140-6736(05)70130-6 [DOI] [PubMed] [Google Scholar]
- 42. Clinical Indicators Team NHS Digital NHS Outcomes Framework: Quarterly Publication 2017, 2017. [Google Scholar]
- 43. Cecil E, Bottle A, Cowling TE, et al. Primary Care access, Emergency Department Visits, and Unplanned Short Hospitalizations in the UK. Pediatrics 2016;137:e20151492 10.1542/peds.2015-1492 [DOI] [PubMed] [Google Scholar]
- 44. Guttmann A. International perspectives on primary care access, equity, and outcomes for children. Pediatrics 2016;137:e20154163 10.1542/peds.2015-4163 [DOI] [PubMed] [Google Scholar]
- 45. Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected Health Data (RECORD) Statement. PLoS Med 2015;12:e1001885 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Saigal S, den Ouden L, Wolke D, et al. School-age outcomes in children who were extremely low birth weight from four international population-based cohorts. Pediatrics 2003;112:943–50. 10.1542/peds.112.4.943 [DOI] [PubMed] [Google Scholar]
- 47. Health and Social Care Information Centre. Maternity Services Data Set (MSDS) Data Model v1.5. Secondary Maternity Services Data set (MSDS) Data Model v1.5. 2015. http://www.hscic.gov.uk/media/11885/Maternity-Data-Model-v15/pdf/Maternity_Services_Data_Set_Data_Model_v1.5.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjqs-2016-006253supp001.docx (19.9KB, docx)