Abstract
This article reviews the literature on nasal changes with maxillary orthognathic surgery. Understanding such changes is vital for surgical planning and for obtaining appropriate informed consent, and there are medico-legal implications. During orthognathic surgical planning a prediction of the effects of the different surgical movements is possible and this forms part of the basis of the planning stage. The predicted changes need to be identified and their desirability or not for each individual patient determined. Some techniques for managing undesirable nasal changes are discussed, including adjunct measures to minimize these potential effects (e.g. cinch sutures), and additional surgical procedures to manage the undesired nasal changes once they are produced.
Keywords: Maxillary osteotomy, orthognathic surgery, nasal changes, orthodontics, suture
Introduction
For a successful outcome in facial aesthetic and reconstructive surgery a thorough analysis of the deformity and the tissues being managed is needed. The nose should form part of the assessment of patients for whom we plan orthognathic surgery (1). Altering the position of the maxilla with orthognathic surgery produces changes to the nasal appearance and function. Some of these could be beneficial and should be allowed to happen for a more refined aesthetic result. For instance, where preoperative interalar distance is reduced, the advancement of the maxilla with orthognathic surgery will widen the interalar distance, producing a desired effect. On the other hand anticipated negative features could be eliminated at the planning stage, minimized or controlled with ancillary procedures during surgery or corrected with secondary procedures. It is worth noting that although mandibular orthognathic surgery would not directly change the nasal structure a relative change in appearance to the nose can be brought about by changing the position of the chin and vice-versa, Figure 1. Surgery to the maxilla will undoubtedly have effects on the nasal appearance. This article will concentrate on Le Fort I type surgeries, as this is the most common type of surgery undertaken in isolation or as part of bimaxillary orthognathic surgery and directly affects nasal appearance. The aim is to summarize the literature about changes to nasal function and appearance with Le Fort I maxillary orthognathic surgery and the evidence for ancillary techniques.
Figure 1.

Illusional change in the perception of the position of the chin in profile view following nasal hump removal. (From: Naini FB. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell, 2011; used with permission). (a) Preoperative. (b) Postoperative.
Effects of maxillary orthognathic surgery on nasal function
The nasal cavity anatomy and volume are altered with maxillary osteotomies and as a result nasal airway resistance changes. After impaction and/or advancement of the maxilla a decrease in the nasal airway resistance is observed (2, 3). It has also been reported to decrease with maxillary expansion (4).This is likely to be due to widening of the nares (external nasal valve) and opening of the internal valve. Patients with high initial values for airway resistance have the greatest benefit (5).
Effects of maxillary orthognathic surgery on nasal morphology
Widening of the alar base occurs following almost all maxillary osteotomies, especially with impaction and/or advancement(6) or segmental advancement and widening (7).It is the most consistently reported change in the literature (6, 7, 8, 9, 10). It has also been noted to occur with surgically assisted maxillary expansion (7, 11, 12). The most likely explanation for this is the elevation of the periosteum off the anterior surface of the maxilla, together with the muscles and ligaments stabilizing the alar region (13). A study using CBCT images preoperatively and 12 months postoperatively for a cohort of patients undergoing bimaxillary surgery (involving maxillary advancement and cinch suture) found no significant correlation between the horizontal or vertical movement of A-point or ANS and the widening of the alar base (9). This was supported by another study assessing 3D laser scans (10). Often in skeletal Class III cases, part of the deformity is maxillary hypoplasia and poor support to the alar bases resulting in a narrowed interalar distance, hence a mild widening of the alar base width is welcomed, Figure 2. On the other hand, if the interalar distance is already wide, as is often the case in patients of African-Caribbean ethnicity, avoidance of a further increase is important. Minimizing the amount of maxillary movement or avoidance of maxillary surgery if possible may help in this. Other nasal changes also occur with maxillary surgery and generally thought to be dependent on the direction and magnitude of the maxillary move. Maxillary advancement and superior repositioning tends to cause elevation and advancement of the nasal tip, as well as enlargement of the nasal base (6, 8). Rotation of the tip, exaggeration of the supratip break and softening of the dorsal hump may follow maxillary advancements (6). Nasal tip support is provided by various components; nasal septum, lower lateral cartilages, attachment of the medial crura foot plates to the septum, attachment of the upper lateral cartilages to the lower lateral cartilages, and the anterior nasal spine. Therefore dissection and modifications in this region may have an influence on the tip position. Maxillary advancement and impaction led to superior repositioning of the nasal tip in 85% of the cases, nasal tip advancement in 80%, rotation in 80%, and widening of the alar base in 95% (8). The most consistent association reported is the increased projection and rotation of the nasal tip (upturning) with maxillary advancement (7, 8). In under-projected, rotated short noses, this may result in excessive nostril show, Figure 3. Superior repositioning also causes elevation of the nasal tip. With inferior repositioning of the maxilla and the rarely performed posterior repositioning there is a loss of tip support. Studies assessing three-dimensional photogrammetric images pre and post-operatively (7, 14, 15) show maxillary advancement leads to significant increases in alar base, interalar and nostril widths, nasolabial angle (15), soft triangle, nasal tip, columella and upper lip projection (7, 14). Significant decreases in the nasofrontal angle and nostril height were also found 7, 14). During maxillary impaction it is important to trim the cartilage of the septum appropriately to prevent its lateral deflection, which may obstruct the nasal airway and/or cause asymmetrical deviation of the nose, Figure 4. On the other hand, if this is done overzealously in front of the anterior nasal spine, in the postoperative period when scarring is taking place, columellar retraction may occur, leaving the columella in a relatively ‘hanging’ position. Excessive reduction of the anterior nasal spine itself can also cause the same deformity, Figure 5. In predicting the change in the nasolabial angle it is helpful to consider it as being composed of two components; hence, the overall alteration will depend on the changes in the columella angle (i.e. upturning of the nasal tip) and the change in the inclination of the upper lip, Figure 6 (16). For instance, in maxillary advancement procedures the upper lip would be advanced leading to a reduction in the lower component but if there is considerable upturning of the nasal tip there would be an increase in the upper component and the overall resultant effect is most commonly an increase in the nasolabial angle (7, 15). There tends to be a decrease in the nasolabial angle following maxillary impaction, which can also be coupled with deepening and accentuation of the nasolabial groove. On the other hand, inferior and/ or posterior repositioning of the maxilla causes an increase in the nasolabial angle (6). Maxillary Le Fort I osteotomy has minimal direct effects on the nasal dorsum. These changes are often perceptual and relate to the tip position. Nasal tip droop often accentuates a prominent nasal dorsum. When the tip projects and rotates upwards, the hump becomes apparently less visible. Conversely when the dorsal nasal profile is low, advancement of the maxilla may result in further flattening of the dorsum.
Figure 2.
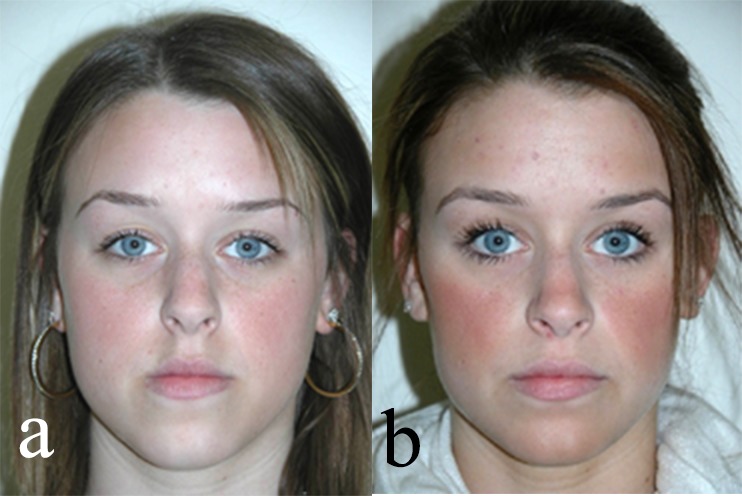
Photographs of a patient with a Class III malocclusion as a result of maxillary retrognathia with associated poor support to the alar base and narrow interalar distance. The latter improved following orthognathic surgery as a result of the expected increase in interalar distance with the maxillary advancement. (From: Naini FB. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell, 2011; used with permission). (a) Preoperative. (b) Postoperative.
Figure 3.
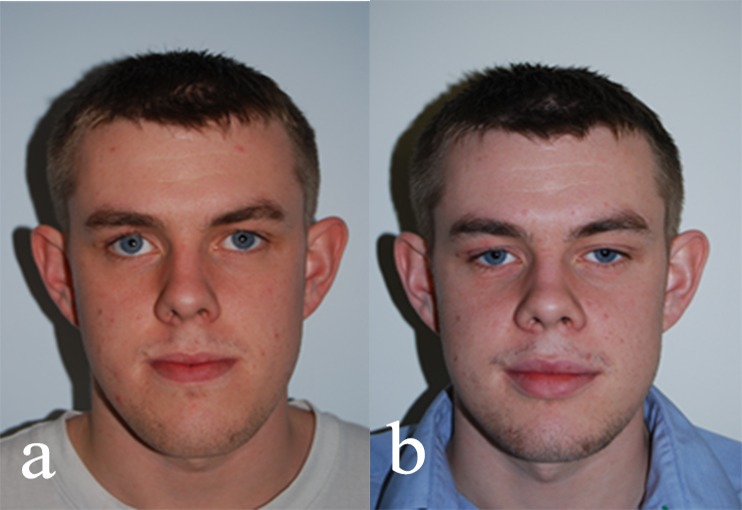
Photographs showing excessive nostril show following a maxillary advancement procedure. (From: Naini FB. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell, 2011; used with permission). (a) Preoperative. (b) Postoperative.
Figure 4.
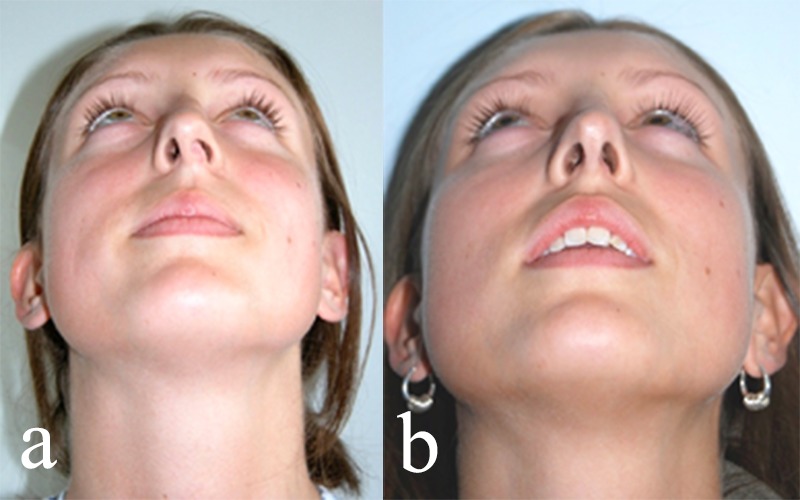
(a) Photograph showing post-orthognathic nasal septum deflection caused by insufficient trimming of the septum during a maxillary impaction. (b) Its management with a secondary procedure. (From: Naini FB. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell, 2011; used with permission).
Figure 5.
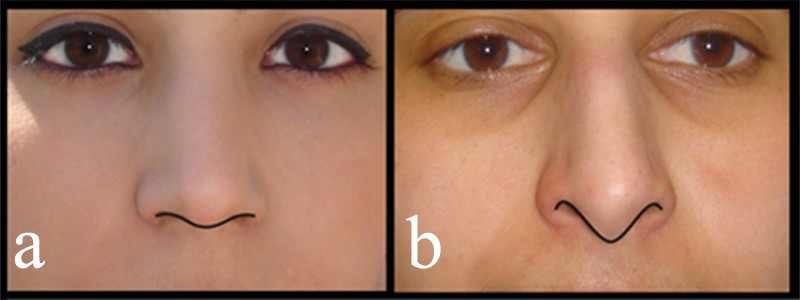
(a) Frontal view showing the ‘gull in flight’ appearance. The columella is observed to hang just inferior to the alar rims. (b) Example of a patient with excessive exposure of the columella (‘hanging columella’) following orthognathic surgery. (From: Naini FB. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell, 2011; used with permission).
Figure 6.
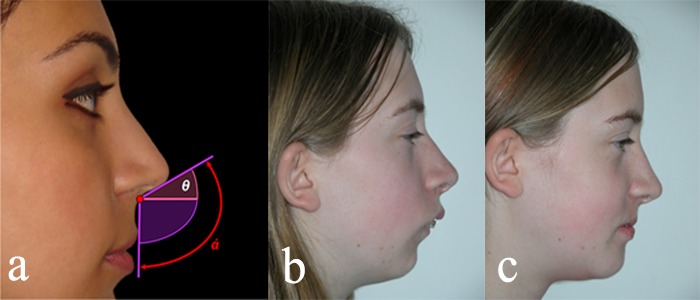
(a) Division of nasolabial angle into upper and lower components. (From: Naini FB. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell, 2011; used with permission). (b) Preoperative profile. (c) Postoperative profile showing increase in nasolabial angle particularly due to changes in the lower component (i.e. upper lip inclination) following a posterior setback of the maxilla.
Intraoperative procedures to manage nasal changes with orthognathic surgery
a. Alar base cinch suture: Originally described by Millard (17) for cleft patients and later introduced into orthognathic surgery as a technique for minimizing alar base widening with maxillary surgery (18). It was postulated that the elevation without re-approximation of the perioral and perinasal musculature was the reason for increased nasal width following Le Fort I type osteotomies (13). Other suggestions for this widening include release of periosteum and muscle attachments adjacent to the nose, oedema and spatial change of the supportive bone to the nasal base (19). The classical cinch suture uses a 3/0 non-absorbable suture passed through the intra-oral incision, anchoring fibro-areolar tissue under both alae and the transverse nasalis muscle. This controlled reorientation of the perinasal muscles is thought to provide a more predictable and stable result than their random reinsertion (20). However, it has been criticized as inaccurate, unpredictable and leading to other possible effects such as upper lip ‘lengthening’, which may not be desirable. The naso-endotracheal tube may distort the nostrils, making intraoperative assessment of alar width and undertaking of the suture difficult and inaccurate (21). Some surgeons have addressed this by using submental intubation (22, 23) whilst others have suggested replacement of the naso-endotracheal tube with an oral endotracheal tube following stabilization of the maxilla and mandible (24, 25). The effectiveness of alar base cinch sutures on minimizing alar widening is controversial, some in support, (23, 25, 26, 27, 28) whilst others stating no significant effect (29, 30).A prospective randomized controlled trial found it provides a small and clinically insignificant decrease in alar width widening (0.5 mm) and concluded it was of ‘little benefit’ (29). On the other hand, a retrospective study found alar widening was statistically significantly reduced with the cinch suture compared to the control group, 1.6 mm and 2.3 mm respectively (28). Another criticism is the unwanted nasal tip rotation (upturning), thought to occur due to ventral pressure of the maxillary bone on the lateral crurae (31). An increase in nasolabial angle has also been identified in individual studies (7, 15, 25, 28, 32, 33), and a systematic review (34).Passing the suture through the nasal septum 10mm posterior to the nasal spine has been suggested as a modification to limit this effect (35). The authors combined this with a VY closure, terming it mACVY and found it limited vertical changes in the nasal tip, to those expected with simple closing sutures (36). There was however a significant increase in nasal tip projection horizontally and increased soft to hard tissue ratios of upper lip movement in mACVY group (36). Two systematic reviews also found the latter trend (34, 37). Generally, it is accepted postoperative oedema can take up to six months if not longer to settle (38), hence stability would be best tested at least a year postoperatively. Studies where samples were followed for at least one year suggest there is good medium term stability (23, 25, 27). Although it has not been compared, it may be that the suture material used i.e. resorbable (28) or non-resorbable (18) could have a bearing on the stability of the procedure. Some modifications to increase stability often by increasing the grasp of tissue (39), for which prospective and mostly randomized trials have been undertaken, include; extra-oral suture insertion (40), extra-oral insertion with partial retraction (41) and transseptal approach (42). A systematic review found the modified versions were more effective than the classical cinch suture at maintaining the preoperative alar and alar base width (43), but a prospective randomized double blind study found no significant difference with their suggested modification (32).
b. Pyriform guttering: In this manoeuvre bone is removed from the pyriform rim to minimize the anterior or superior displacement of alar and perialar soft tissues. Literature assessing the effect of this manoeuvre on nasal soft tissues is lacking.
c. Anterior nasal spine (ANS) recontouring/subspinal osteotomy: Reduction of the ANS can be undertaken when advancing the maxilla in order to control nasal tip rotation, as advancement of the maxilla often leads to nasal tip upturning. It has been reported to lead to a reduced ratio of response of the anterior nasal tip to movement at A-point from 0.33:1 to 0.25:1 (44). It is difficult to quantify the amount and site of bone removal and measurement on lateral cephalometric radiographs is also difficult due to the change in anatomy at the site, hence likely this has led to the little evidence though it is commonly undertaken clinically. Another technique suggested for limiting nasal tip rotation for patients undergoing maxillary advancement and/or impaction is the subspinal osteotomy (45, 46). It is suggested, preservation of the natural muscular insertions of the transverse nasalis and depressor septi muscles can be achieved if the anterior portion of the usual circumvestibular incision is undertaken in a V-shaped full thickness manner and the anterior osteo-musculo-mucosal flap from the nasal septum is preserved (45). Some support this reduces alar base widening and tip rotation though others found no difference in nasal tip elevation and projection (31). The latter, was a retrospective study of two matched groups who received a conventional Le Fort I osteotomy for maxillary advancement and impaction with ANS recontouring, alar base cinch suture and VY closure or subspinal osteotomy. The matching based on amount and direction of skeletal movement allows for a more accurate comparison of the effect of the techniques but it is important to note the comparison is to a Le Fort I with multiple ancillary techniques which have their own effects on the nasal appearance.
d. VY closure: It involves medial advancement of the superior aspect of the vestibular incision to produce the ‘Y’ appearance, to help re-approximate the nasolabial musculature, reducing the tendency for thinning and shortening of the upper lip with Le Fort I osteotomies (13). Studies often include patients receiving cinch sutures as well as VY closures, hence difficult to ascertain which of these techniques produces what effects (36). A trend towards VY closure helping to minimize upper lip shortening is noted in the literature (36, 47, 48), though some studies have also found no statistical significant difference (49). A study found it allowed the upper lip to roll out by approximately 25% more than when no VY closure was used and reduced lip shortening by a factor approaching 2 (47). Furthermore, a randomized prospective trial found a statistically significant increase in upper lip height with an alar cinch suture and VY closure (1.10 mm ± 0.34), which reflected a 23% increase compared to the shortening experienced by the simple closure group with a cinch suture (–0.79 mm ± 0.45) (48).There was also significantly less upper lip thinning with the use of a VY closure (48).
e. Septal trimming and fixation: Instead of or in addition to ANS recontouring, septal trimming can be undertaken to allow for its adaptation to the new anatomical position of the maxilla without it being bent and deviated if lacking space. Additionally, surgeons might use a suture to fix the septum to the surrounding anatomy in the desired position. The fixation of the septum to the anterior nasal spine could be an important stabilization manoeuvre, but one should be careful as the orthognathic surgical procedure would have changed the position of the maxilla and in doing so the anatomical landmarks generally used for positioning the septum may have changed too.
Secondary surgical procedures to manage nasal changes with orthognathic surgery
To correct unwanted changes to the alar base following orthognathic surgery, alar base surgery may be considered. Ideally, the most lateral aspect of the ala should fall within a perpendicular line dropped from the medial aspect of the medial canthus and infratip lobule width should be approximately 75% of the nasal width (16). The following areas should be assessed when planning the procedure; inter-alar width, amount of nasal sill, presence or absence of alar flaring, nostril shape and thickness of the alar rim. Alar base reduction is best performed in the nasal sill. The excision then can be extended at the alar facial groove to deal with the flare component. Excision may be limited to the alar facial groove if the problem is primarily one of flaring. Extension of incisions to the internal vestibular surface depends on the desire to change the shape of the naris. If the alar rim is thick a further wedge excision of the rim may be carried out to narrow it, Figure 7 (50). Septoplasty can be undertaken for correction of a buckled septum following maxillary impaction to improve the nasal airway and to deal with any resultant asymmetry. Columellar retraction resulting from overzealous removal of caudal septum and ANS can be corrected using septal extension grafts and plumping grafts. Long-term stability is better with a septal extension graft but patients may complain of stiffness of the nose. Finally, following maxillary advancement, in cases where there is already a saddle deformity, improvement in dorsal profile can be achieved by using diced cartilage wrapped in temporalis fascia. This gives a stable result allowing the dorsum to blend well with the neighboring areas.
Figure 7.
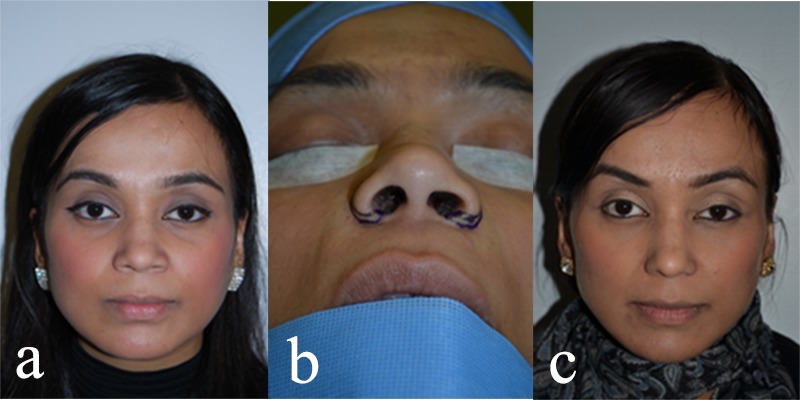
Photographs showing a patient who underwent alar wedge excision as a secondary procedure to manage the alar flare and increased interalar width that resulted from orthognathic surgery. (From: Naini FB. Facial Aesthetics: Concepts and Clinical Diagnosis. Oxford: Wiley-Blackwell, 2011; used with permission). (a) Preoperative. (b) Intraoperative. (c) Postoperative.
Conclusion
Nasal aesthetic and functional analysis should form part of the diagnostic process and treatment planning for orthognathic surgery. Patients should be informed about nasal changes that may occur with orthognathic surgery and the associated strategies for their management. It is an art to allow some changes to occur when these are deemed beneficial but to identify and minimize undesired effects. Although some ancillary manoeuvres are possible, these also lead to nasal changes themselves which should be considered, and in some cases secondary procedures may be required. To be able to carry out a comprehensive septorhinoplasty either planned at the outset or introduced later based on post-orthognathic surgical assessment, provides a powerful tool for the facial surgeon. Whilst there may be attraction to carrying out a rhinoplasty concurrently with a maxillary osteotomy, both in terms of inaccuracy of planning as well as inability to achieve a high quality technical result, this temptation should be avoided in the view of the authors. The nose will change during the maxillary osteotomy and preoperative observations will not be the same, making a finely tuned rhinoplasty plan a challenge. In addition, each procedure may take several hours, making the operation unreasonably long and anaesthetic considerations, such as change of nasal tube to oral, or a submental intubation to be carried out at the outset, may become a necessity. Carrying out rhinoplasty and maxillary osteotomy at the same time is contentious and though advocated by some authors (51), the present authors would recommend instead their sequential undertaking in most cases.
Acknowledgments
The authors are grateful to the patients who kindly allowed for their photographs to be published, the staff they work with and the Editors and publisher of the textbook ‘Orthognathic Surgery: Principles, Planning and Practice’ for allowing part of the published material to be used.
Footnotes
Source of funding: None declared.
Conflict of interest: None declared.
References
- 1.Warner JP, Chauhan N, Adamson PA. Alar soft-tissue techniques in rhinoplasty: algorithmic approach, quantifiable guidelines, and scar outcomes from a single surgeon experience. Arch Facial Plast Surg. 2010. May-Jun;12(3):149–58. 10.1001/archfacial.2010.30 [DOI] [PubMed] [Google Scholar]
- 2.Guenthner TA, Sather AH, Kern EB. The effect of Le Fort I maxillary impaction on nasal airway resistance. Am J Orthod. 1984. April;85(4):308–15. 10.1016/0002-9416(84)90188-X [DOI] [PubMed] [Google Scholar]
- 3.Turvey TA, Hall DJ, Warren DW. Alterations in nasal airway resistance following superior repositioning of the maxilla. Am J Orthod. 1984. February;85(2):109–14. 10.1016/0002-9416(84)90002-2 [DOI] [PubMed] [Google Scholar]
- 4.Ramires T, Maia RA, Barone JR. Nasal cavity changes and the respiratory standard after maxillary expansion. Rev Bras Otorrinolaringol (Engl Ed). 2008. Sep-Oct;74(5):763–9. 10.1016/S1808-8694(15)31388-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams BJ, Isom A, Laureano Filho JR, O’Ryan FS. Nasal airway function after maxillary surgery: a prospective cohort study using the nasal obstruction symptom evaluation scale. J Oral Maxillofac Surg. 2013. February;71(2):343–50. 10.1016/j.joms.2012.05.010 [DOI] [PubMed] [Google Scholar]
- 6.Mitchell C, Oeltjen J, Panthaki Z, Thaller SR. Nasolabial aesthetics. J Craniofac Surg. 2007. July;18(4):756–65. 10.1097/scs.0b013e3180684360 [DOI] [PubMed] [Google Scholar]
- 7.DeSesa CR, Metzler P, Sawh-Martinez R, Steinbacher DM. Three-dimensional nasolabial morphologic alterations following le fort i. Plast Reconstr Surg Glob Open. 2016. August;4(8):e848. 10.1097/GOX.0000000000000685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dantas WR, Silveira MM, Vasconcelos BC, Porto GG. Evaluation of the nasal shape after orthognathic surgery. Braz J Otorhinolaryngol. 2015. Jan-Feb;81(1):19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeong HI, Lee HS, Jung YS, Park HS, Jung HD. Nasal soft tissue change following bimaxillary orthognathic surgery. J Craniofac Surg. 2017. October;28(7):e605–8. 10.1097/SCS.0000000000003736 [DOI] [PubMed] [Google Scholar]
- 10.Yamada T, Mishima K, Moritani N, Janune D, Matsumura T, Ikeya Y et al. Nasolabial morphologic changes after a Le Fort I osteotomy: a three-dimensional anthropometric study. J Craniofac Surg. 2010. July;21(4):1089–95. 10.1097/SCS.0b013e3181e1e6ff [DOI] [PubMed] [Google Scholar]
- 11.de Assis DS, Duarte MA, Gonçales ES. Clinical evaluation of the alar base width of patients submitted to surgically assisted maxillary expansion. Oral Maxillofac Surg. 2010. September;14(3):149–54. 10.1007/s10006-010-0211-3 [DOI] [PubMed] [Google Scholar]
- 12.Metzler P, Geiger EJ, Chang CC, Steinbacher DM. Surgically assisted maxillary expansion imparts three-dimensional nasal change. J Oral Maxillofac Surg. 2014. October;72(10):2005–14. 10.1016/j.joms.2014.03.004 [DOI] [PubMed] [Google Scholar]
- 13.Schendel SA, Williamson LW. Muscle reorientation following superior repositioning of the maxilla. J Oral Maxillofac Surg. 1983. April;41(4):235–40. 10.1016/0278-2391(83)90265-3 [DOI] [PubMed] [Google Scholar]
- 14.Metzler P, Geiger EJ, Chang CC, Sirisoontorn I, Steinbacher DM. Assessment of three-dimensional nasolabial response to Le Fort I advancement. J Plast Reconstr Aesthet Surg. 2014. June;67(6):756–63. 10.1016/j.bjps.2014.03.023 [DOI] [PubMed] [Google Scholar]
- 15.Worasakwutiphong S, Chuang YF, Chang HW, Lin HH, Lin PJ, Lo LJ. Nasal changes after orthognathic surgery for patients with prognathism and Class III malocclusion: analysis using three-dimensional photogrammetry. J Formos Med Assoc. 2015. February;114(2):112–23. 10.1016/j.jfma.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 16.Naini FB. Regional analysis: The nose. Oxford: Wiley- Blackwell; 2011. pp. 214–37. [Google Scholar]
- 17.Millard DR., Jr The alar cinch in the flat, flaring nose. Plast Reconstr Surg. 1980. May;65(5):669–72. 10.1097/00006534-198005000-00020 [DOI] [PubMed] [Google Scholar]
- 18.Collins PC, Epker BN. The alar base cinch: a technique for prevention of alar base flaring secondary to maxillary surgery. Oral Surg Oral Med Oral Pathol. 1982. June;53(6):549–53. 10.1016/0030-4220(82)90338-3 [DOI] [PubMed] [Google Scholar]
- 19.Wolford LM. Lip-nasal aesthetics following Le Fort I osteotomy-discussion. Plast Reconstr Surg. 1988;81(2):180–2. 10.1097/00006534-198802000-00006 [DOI] [PubMed] [Google Scholar]
- 20.Carlotti AE Jr, Aschaffenburg PH, Schendel SA. Facial changes associated with surgical advancement of the lip and maxilla. J Oral Maxillofac Surg. 1986. August;44(8):593–6. 10.1016/S0278-2391(86)80068-4 [DOI] [PubMed] [Google Scholar]
- 21.Rosen HM. Lip-nasal aesthetics following Le Fort I osteotomy. Plast Reconstr Surg. 1988. February;81(2):171–82. 10.1097/00006534-198802000-00005 [DOI] [PubMed] [Google Scholar]
- 22.Chandu A, Witherow H, Stewart A. Submental intubation in orthognathic surgery: initial experience. Br J Oral Maxillofac Surg. 2008. October;46(7):561–3. 10.1016/j.bjoms.2008.02.021 [DOI] [PubMed] [Google Scholar]
- 23.Raithatha R, Naini FB, Patel S, Sherriff M, Witherow H. Long-term stability of limiting nasal alar base width changes with a cinch suture following Le Fort I osteotomy with submental intubation. Int J Oral Maxillofac Surg. 2017. November;46(11):1372–9. 10.1016/j.ijom.2017.04.027 [DOI] [PubMed] [Google Scholar]
- 24.Kattimani VS, Sridhar M, Shaik TN. Simplified technique to change the endotracheal tube from nasal to oral cavity. J Maxillofac Oral Surg. 2017. September;16(3):392–4. 10.1007/s12663-016-0908-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shoji T, Muto T, Takahashi M, Akizuki K, Tsuchida Y. The stability of an alar cinch suture after Le Fort I and mandibular osteotomies in Japanese patients with Class III malocclusions. Br J Oral Maxillofac Surg. 2012. June;50(4):361–4. 10.1016/j.bjoms.2011.04.073 [DOI] [PubMed] [Google Scholar]
- 26.Mustafa K, Shehzana F, Bhat HH. Assessment of alar flare and efficacy of alar cinch suture in the management of alar flare following Le Fort I superior repositioning: A comparative study. J Maxillofac Oral Surg. 2016. December;15(4):528–34. 10.1007/s12663-015-0866-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stewart A, Edler RJ. Efficacy and stability of the alar base cinch suture. Br J Oral Maxillofac Surg. 2011. December;49(8):623–6. 10.1016/j.bjoms.2010.11.023 [DOI] [PubMed] [Google Scholar]
- 28.Westermark AH, Bystedt H, Von Konow L, Sällström KO. Nasolabial morphology after Le Fort I osteotomies. Effect of alar base suture. Int J Oral Maxillofac Surg. 1991. February;20(1):25–30. 10.1016/S0901-5027(05)80690-3 [DOI] [PubMed] [Google Scholar]
- 29.Howley C, Ali N, Lee R, Cox S. Use of the alar base cinch suture in Le Fort I osteotomy: is it effective? Br J Oral Maxillofac Surg. 2011. March;49(2):127–30. 10.1016/j.bjoms.2010.02.009 [DOI] [PubMed] [Google Scholar]
- 30.van Loon B, Verhamme L, Xi T, de Koning MJ, Bergé SJ, Maal TJ. Three-dimensional evaluation of the alar cinch suture after Le Fort I osteotomy. Int J Oral Maxillofac Surg. 2016. October;45(10):1309–14. 10.1016/j.ijom.2016.05.013 [DOI] [PubMed] [Google Scholar]
- 31.Mommaerts MY, Lippens F, Abeloos JV, Neyt LF. Nasal profile changes after maxillary impaction and advancement surgery. J Oral Maxillofac Surg. 2000. May;58(5):470–5. 10.1016/S0278-2391(00)90002-8 [DOI] [PubMed] [Google Scholar]
- 32.Chen CY, Lin CC, Ko EW. Effects of two alar base suture techniques suture techniques on nasolabial changes after bimaxillary orthognathic surgery in Taiwanese patients with class III malocclusions. Int J Oral Maxillofac Surg. 2015. July;44(7):816–22. 10.1016/j.ijom.2015.03.003 [DOI] [PubMed] [Google Scholar]
- 33.Khamashta-Ledezma L, Naini FB. Prospective assessment of maxillary advancement effects: maxillary incisor exposure, and upper lip and nasal changes. Am J Orthod Dentofacial Orthop. 2015. April;147(4):454–64. 10.1016/j.ajodo.2014.11.028 [DOI] [PubMed] [Google Scholar]
- 34.Khamashta-Ledezma L, Naini FB. Systematic review of changes in maxillary incisor exposure and upper lip position with Le Fort I type osteotomies with or without cinch sutures and/or VY closures. Int J Oral Maxillofac Surg. 2014. January;43(1):46–61. 10.1016/j.ijom.2013.08.005 [DOI] [PubMed] [Google Scholar]
- 35.Muradin MS, Rosenberg A. Controlling nasolabial aesthetics after le fort i osteotomies: A retrospective study. J Craniomaxillofac Surg. 2000;28:209. [Google Scholar]
- 36.Muradin MS, Seubring K, Stoelinga PJ. vd Bilt A, Koole R, Rosenberg AJ. A prospective study on the effect of modified alar cinch sutures and v-y closure versus simple closing sutures on nasolabial changes after Le Fort I intrusion and advancement osteotomies. J Oral Maxillofac Surg. 2011;69(3):870–6. 10.1016/j.joms.2010.03.008 [DOI] [PubMed] [Google Scholar]
- 37.San Miguel Moragas J, Van Cauteren W, Mommaerts MY. A systematic review on soft-to-hard tissue ratios in orthognathic surgery part I: maxillary repositioning osteotomy. J Craniomaxillofac Surg. 2014. October;42(7):1341–51. 10.1016/j.jcms.2014.03.024 [DOI] [PubMed] [Google Scholar]
- 38.Stella JP, Streater MR, Epker BN, Sinn DP. Predictability of upper lip soft tissue changes with maxillary advancement. J Oral Maxillofac Surg. 1989. July;47(7):697–703. 10.1016/S0278-2391(89)80008-4 [DOI] [PubMed] [Google Scholar]
- 39.Peacock ZS, Susarla SM. Is the pyriform ligament important for alar width maintenance after Le Fort I osteotomy? J Oral Maxillofac Surg. 2015. December;73(12 Suppl):S57–66. 10.1016/j.joms.2015.04.015 [DOI] [PubMed] [Google Scholar]
- 40.Ritto FG, Medeiros PJ, de Moraes M, Ribeiro DP. Comparative analysis of two different alar base sutures after Le Fort I osteotomy: randomized double-blind controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011. February;111(2):181–9. 10.1016/j.tripleo.2010.04.019 [DOI] [PubMed] [Google Scholar]
- 41.Rauso R, Tartaro G, Tozzi U, Colella G, Santagata M. Nasolabial changes after maxillary advancement. J Craniofac Surg. 2011. May;22(3):809–12. 10.1097/SCS.0b013e31820f3663 [DOI] [PubMed] [Google Scholar]
- 42.Nirvikalpa N, Narayanan V, Wahab A, Ramadorai A. Comparison between the classical and a modified trans-septal technique of alar cinching for Le Fort I osteotomies: a prospective randomized controlled trial. Int J Oral Maxillofac Surg. 2013. January;42(1):49–54. 10.1016/j.ijom.2012.05.027 [DOI] [PubMed] [Google Scholar]
- 43.Liu X, Zhu S, Hu J. Modified versus classic alar base sutures after LeFort I osteotomy: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014. January;117(1):37–44. 10.1016/j.oooo.2013.09.002 [DOI] [PubMed] [Google Scholar]
- 44.Freihofer HP., Jr Changes in nasal profile after maxillary advancement in cleft and non-cleft patients. J Maxillofac Surg. 1977. February;5(1):20–7. 10.1016/S0301-0503(77)80071-4 [DOI] [PubMed] [Google Scholar]
- 45.Becelli R, De Ponte FS, Fadda MT, Govoni FA, Iannetti G. Subnasal modified Le Fort I for nasolabial aesthetics improvement. J Craniofac Surg. 1996. September;7(5):399–402. 10.1097/00001665-199609000-00015 [DOI] [PubMed] [Google Scholar]
- 46.Mommaerts MY, Abeloos JV, De Clercq CA, Neyt LF. The effect of the subspinal Le Fort I-type osteotomy on interalar rim width. Int J Adult Orthodon Orthognath Surg. 1997;12(2):95–100. [PubMed] [Google Scholar]
- 47.McCollum AG, Dancaster JT, Evans WG, Becker PJ. Sagittal soft tissue changes related to the surgical corrections of maxillary deficient class III malocclusions. Semin Orthod. 2009;15(3):172–84. 10.1053/j.sodo.2009.03.003 [DOI] [Google Scholar]
- 48.Peled M, Ardekian L, Krausz AA, Aizenbud D. Comparing the effects of V-Y advancement versus simple closure on upper lip aesthetics after Le Fort I advancement. J Oral Maxillofac Surg. 2004. March;62(3):315–9. 10.1016/j.joms.2003.08.015 [DOI] [PubMed] [Google Scholar]
- 49.Talebzadeh N, Pogrel MA. Upper lip length after V-Y versus continuous closure for Le Fort I level maxillary osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000. August;90(2):144–6. 10.1067/moe.2000.107836 [DOI] [PubMed] [Google Scholar]
- 50.Manisali M, Khamashta-Ledezma L. Rhinoplasty and nasal changes in relation to orthognathic surgery. Oxford: Wiley- Blackwell; 2017. pp. 724–38. [Google Scholar]
- 51.Seah TE, Bellis H, Ilankovan V. Orthognathic patients with nasal deformities: case for simultaneous orthognathic surgery and rhinoplasty. Br J Oral Maxillofac Surg. 2012. January;50(1):55–9. 10.1016/j.bjoms.2010.12.009 [DOI] [PubMed] [Google Scholar]


