Abstract
The introduction of cone beam computed tomography (CBCT) devices, changed the way oral and maxillofacial radiology is practiced. CBCT was embraced into the dental settings very rapidly due to its compact size, low cost, low ionizing radiation exposure when compared to medical computed tomography. Alike medical CT, 3 dimensional evaluation of the maxillofacial region with minimal distortion is offered by the CBCT. This article provides an overview of basics of CBCT technology and reviews the specific application of CBCT technology to oral and maxillofacial region with few illustrations.
Keywords: Cone beam computed tomography, dentistry, radiography, x-ray, oral and maxillofacial imaging
Introduction
The discovery of X – rays in 1895 by Sir Wilhelm Conrad Roentgen was an incredible era in the history of medicine. Diagnostic imaging over the last few decades, turned out to be much more refined owing to addition of various imaging technology with complex physical principles. Threedimensional imaging (3D) evolved to meet the demands of advanced technologies in delivering the treatment and at the same time responsible for the evolution of new treatment strategies. Considering the limitations (superimpositions, distortions etc.) of two-dimensional (2D) radiography (Figure 1), which was the backbone of diagnostic imaging for many years, doubt exists that it will continue to contribute in the future. G.N. Hounsfield, in 1972 introduced computerized transverse axial scanning (1) which lead to introduction of Computed Tomography (CT). However the high cost, limited access, and high radiation exposure, were the main drawbacks for under utilization of CT in dentistry. Arai et al. (2) in Japan and Mozzo et al. (3) in Italy working independently, introduced the Cone Beam Computed Tomography (CBCT) for the oral and maxillofacial applications and like CT, offered 3D exploration and more accurate imaging compared to 2D imaging. The cost effective technology of CBCT, led to speedy ingress into the field of dentistry with demand for commitment of dental professionals and dental educators to explore the applications of CBCT technology. The purpose of this review is to provide an insight into 3D imaging with CBCT technology, its basic concepts, advantages, disadvantages and applications in dentistry with few illustrations.
Figure 1.
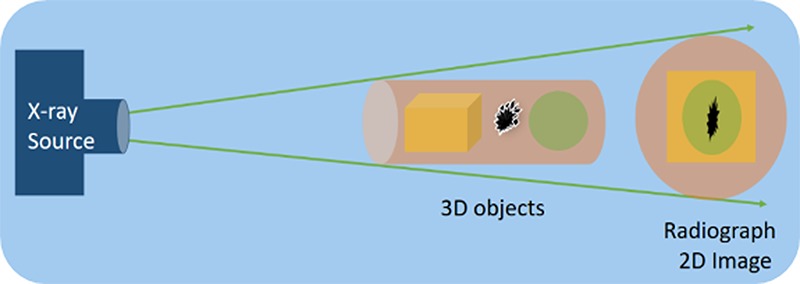
2D Imaging, compression of three-dimensional objects into superimposed, distorted two-dimensional images on the resultant radiograph.
Basic principles
Conventional CT equipment using a fan shaped X ray beam captures a series of axial plane slices or from a continuous spiral motion over the axial plane. A CBCT machine, on the other hand, uses a cone-shaped beam and a reciprocating solidstate flat panel detector, which rotates once around the patient (Figure 2), 180-360 degrees, covering the defined anatomical volume (complete dental/ maxillofacial volume or limited regional area of interest) rather than slice-by-slice imaging found in conventional CT. This single scan (rotation) captures planned data (180-1024 2D images, similar to lateral cephalometric images, each one’s marginally offset), unlike stacked axial slices found in CT, further reducing the absorbed x-ray dose from 6 to 15 times in comparison to CT. Depending upon manufacturers, the scanning time of CBCT equipment varies from nearly 5 to 40 seconds. The X-ray parameters of CBCT is comparable to that of panoramic radiography with a usual operating range of 1-15 mA at 90-120 kVp, while that of CT is considerably higher at 120- 150 mA and 220 kVp. The captured 2D images are instantaneously conveyed to the computer, which reconstructs them, using modified Feldkamp algorithm into the anatomical volume for viewing at 1:1 ratio in axial, coronal, and sagittal planes (orthogonal planes) (Figure 3a,3b,3c,3d) (4). The data is in the Digital Imaging and Communications in Medicine (DICOM) format, which enables ease of telecommunication and usage with other third party imaging software.
Figure 2.
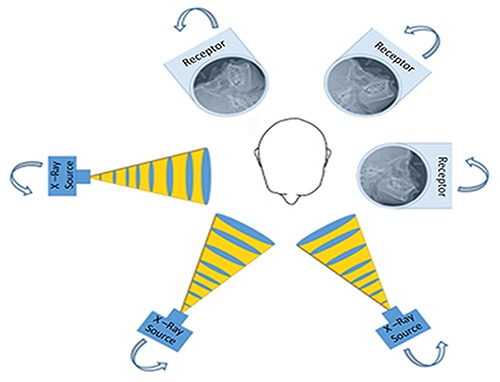
CBCT, Principle of basis image acquisition where in X-ray source and Image receptor reciprocate around patient 180 – 360 degrees to acquire 180 – 1024, 2D cephalometric images (Basis images).
Figure 3.
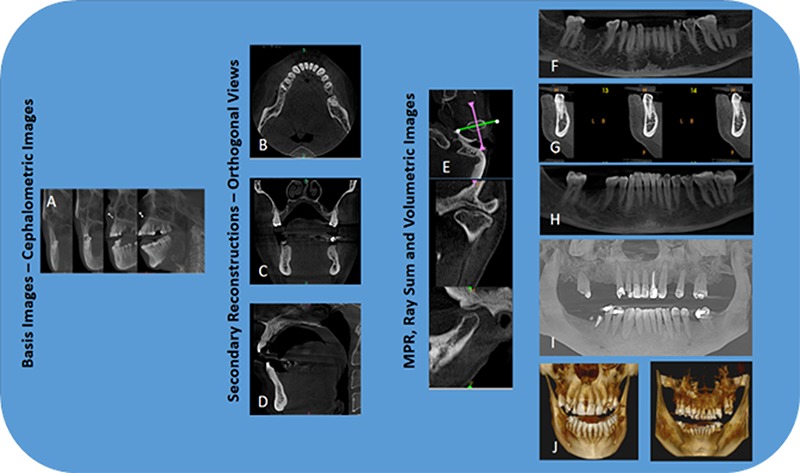
CBCT: Image acquisition and display modes. Acquired 2D Basis images (A) are used for Secondary reconstruction of axial (B), coronal (C) and sagittal (D) views (orthogonal views). Other display modes available in CBCT include (i) multiplanar reformatted (MPR) consisting of Oblique slices (E) Curved slice (F) and Cross sectional views (G); (ii) Ray sum comprising images of increased section thickness (H); and (iii) volumetric images consisting of Direct volume rendering (DVR), the most common of which being maximum intensity projection (MIP) (I) and Indirect volume rendering (IVR) (J).
Most of the CBCT equipment comes with userfriendly viewing software containing basic 3D imaging tools. Third party software are accessible at a wide range of price, which provide extensive tools to analyze and do treatment plans. Besides these, third party software are used to prepare surgical guides, virtual study prototypes, and laser generated resin models, easing the process of diagnosis, treatment plan and delivery of the treatment (5, 6). The utmost hands-on benefit of CBCT in dental imaging is the facilitation to interact with the data and create images imitating those generally employed in clinical settings (for example panoramic, cephalometric, or bilateral multiplanar projections of the temporomandibular joint). These reconstructed views, consecutively interpreted, judged, and measured for diagnostic and treatment-planning purposes (Figure 3). The CBCT provides following display modes apart from basic orthogonal views, as explained below (7, 8, 9,10):
Oblique slicing: Nonorthogonal slicing (Figure 3e) of the CBCT images at any angle is possible because of the isotropic nature of the datasets to provide non-axial 2-D planar images referred to as multiplanar reformations (MPR). This function creates 2D images at any angle by cutting across a set of axial images, which help in evaluating particular structures (Impacted teeth, TMJ).
Curved slicing: This enables to trace the jaw arch to display a trace view, providing acquainted panorama like view (Figure 3f).
Cross-sectional (oblique coronal) view: This function creates a set of successive cross-sectional images (Figure 3g) perpendicular to curved slice with the option of selecting the thickness and spacing. Such images are valuable in the evaluation of morphometric characteristics of alveolar bone for implant placement, the relationship of impacted mandibular third molar with mandibular canal, condylar surface and shape in the symptomatic TMJ or pathological conditions affecting the jaws.
Ray sum: This function enables to display the thickened MPR slices by adding up adjacent voxels (Figure 3h). The resulting image ‘ray sum’ denotes exact volume of the patient that can be used to generate virtual projections, such as panoramic or cephalometric images identical to conventional radiographs without magnification and parallax distortion. However, they can be negatively affected by the superimposition of multiple structures analogous to 2D imaging.
Volume rendering: This function enables one to selectively display voxels within a data set to visualize volume. Direct volume rendering and indirect volume rendering are the two frequently used tools with this function. Direct volume rendering involves picking an arbitrary threshold of voxel values, below or above which all gray values are excluded. Numerous techniques are available; however, the most commonly used is maximum intensity projection (MIP).MIP displays an image (Figure 3i) with the voxels, which have highest density values within a particular thickness. Voxel values that are below an arbitrary threshold are excluded. MIP images are ideal for locating impacted teeth, for TMJ assessment, for assessment of fractures, for craniofacial analysis, for surgical follow-up, and for visualization of soft tissue calcifications. Indirect volume rendering (IVR) involves selection of the density of the voxels to be displayed within an entire data set (called “segmentation”) resulting in a volumetric surface reconstruction with depth (Figure 3j). Two kinds of views are possible: views that are solid (surface rendering) and views that are transparent (volumetric rendering). IVR is ideal for visualization and analysis of craniofacial conditions and determination of relationships of various anatomic features, such as the inferior alveolar canal to the mandibular third molar.
Advantages of CBCT over CT
High radiation dose, cost, availability, longer scanning time, poor resolution and difficulty in interpretation have led to restricted use of CT in dentistry. Few of these problems can be overcome with CBCT, which provides a number of potential advantages for Oral and Maxillofacial imaging, compared with conventional CT (10).
X-ray beam limitation: The CBCT machines come with capability to collimate (select the Field of View, FOV, Figure 4) the primary X- ray beam to the area of interest, reducing the size of irradiation. This procedure fulfils the individual needs, reduces unnecessary exposure to the patient and minimizes scattered radiation that would degrade image quality. CBCT units are classified according to the maximum FOV incorporated from the scan or scans (10, 11, 12).
Figure 4.
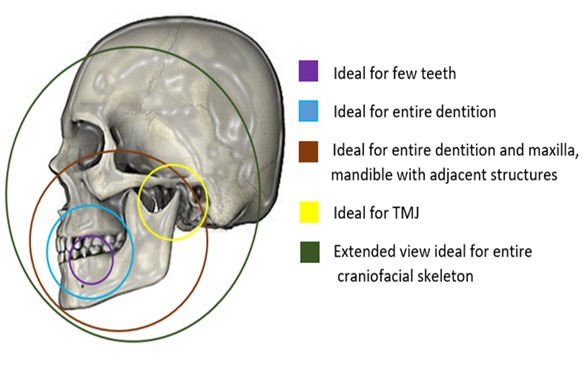
Showing the capability of CBCT machines to collimate (select FOV’s) the X-ray beam to suit the needs of individual clinical situations.
Image accuracy: CBCT machines provide isotropic voxels i.e. equal in all three proportions as compared to anisotropic voxels found in conventional CT. Although CT voxel surfaces can be as small as 0.625 mm square, their depth is usually in the order of 1–2 mm where as CBCT produces sub-millimeter resolution ranging from 0.4 mm to as low as 0.09 mm. This sub-millimeter resolution of CBCT is precise enough for measurements in oral and maxillofacial applications fulfilling the need of exactness required for implant site assessment and orthodontic analysis (9, 13).
Rapid scan time: The single rotation, which is used in CBCT technology to acquire basis images for 3D imaging usually requires scan time ranging from 5 to 40 seconds comparable to panoramic radiography. This short scanning time is advantageous in plummeting the artifacts owing to patient movement (10).
Dose reduction: The effective dose (E) according to the category and model of CBCT equipment and FOV designated ranges from 29-477 μSv (14, 15, 16, 17, 18). Further, up to 40% reduction of the dose can be achieved by varying patient positioning (tilting the chin) and supplementary usage of personal protection (thyroid collar). CBCT delivers an equivalent patient radiation dose of 5 to 74 times that of a panoramic X - ray or 3 to 48 days of background radiation (15, 16). CBCT offers significant dose reductions of between 98.5% and 76.2% in contrast with patient dose reported for oral and maxillofacial imaging by conventional CT (approximately 2000 mSv) (18).
Display modes unique to maxillofacial imaging: Besides providing interrelated images in orthogonal planes CBCT data sets can be segmented nonorthogonally (MPR) to provide oblique, curved planar reformation (distortion free simulated panoramic images) and, serial cross sectional reformation (Figure 3), all of which can be utilized to accentuate precise anatomic structures and diagnostic functions. These features are very essential considering the intricate oral and maxillofacial anatomy. Measurements calculated on the screen are free from distortion and magnification. Furthermore, true 3D visualization of the dataset including ray sum, MIP and 3D computer generated models (Figure 3) are available (10, 19).
Reduced image artifact: Availability of artifact suppression algorithms and increasing number of projections have led to low level of metal artifact, mainly in secondary reconstructions intended for seeing the jaws and teeth (20).
Limitations of CBCT
Although CBCT has made a speedy ingress into the field of dentistry, currently it is not devoid of drawbacks, which may be related to the ‘‘cone-beam’’ projection geometry, detector sensitivity, and contrast resolution. The clarity of CBCT images is affected by artifacts, noise, and poor soft tissue contrast.
An artifact is any distortion or error in the image that is unrelated to the subject being studied. This impairs CBCT image quality and limit adequate visualization of structures in the dento-alveolar region. Artifacts can be due to beam hardening (results in cupping artifact and streaks and dark bands), Patient-related artifacts (Patient motion resulting in unsharpness of the reconstructed image), Scanner-related artifacts (circular or ringshaped) and cone beam–related artifacts (partial volume averaging, undersampling, and cone-beam effect) (21).
Image noise is due to large volume being irradiated during CBCT scanning resulting in heavy interactions with tissues producing scattered radiation, which in turn leads to nonlinear attenuation by the detectors. This additional x-ray detection is called noise and contributes to image degradation (22).
Poor soft tissue contrast: CBCT units have noticeably less soft tissue contrast than conventional CT machines. Three factors limit the contrast resolution of CBCT, which include increased image noise, the divergence of the x-ray beam and numerous inherent flat-panel detector-based artifacts (23, 24).
Various machines available in the market
The first CBCT device (NewTom-9000; Quantitative Radiology, Verona, Italy) was described in 1998 by Mozzo et al. (3). Since then, a number of CBCT machines have been introduced into the market and the information of some of these has been summarized in the Table 1.
Table 1.
Technical characteristics of some commercially available CBCT devices.
| CBCT Machine | Availability of Pan and Ceph | FOV available (height x diameter in cm) | Voxel size (mm) | Manufacturer | Exposure time (seconds) |
|---|---|---|---|---|---|
| Veraviewepocs 3D R100 | Yes | 4 x 4, 4 x 8, 8 x 5, 8 x 8, 10 x 5,10 x 8 | 0.125 | J. Morita, Japan | 42834 |
| Galileos comfort plus | Yes | 15.4 cm spherical | 0.25 / 0.125 | Sirona Dental Systems, Germany | 2-5 |
| i-CAT FLX | Yes | 4 x 16, 6 x 16, 8 x 8, 8 x 16, 10 x 16, 11 x16, 13 x 16 Extended Field of View:17 x 23 | 0.125 - 4 | Imaging Sciences Int'l, USA | 4.8, 8.9, 14.7, 17.8 or 26.9 |
| KaVo OP300 Maxio | Yes | 5 x 5, 6.1 x 7.8, 7.8 x 7.8,7.8 x 15, 13 x 15 | 0.085 -0.420 | KaVo, Germany | 1.2 - 9 |
| NewTom 5G | Yes | 6 x 6, 8 x 8, 12 x 8, 15 x 5, 15 x 12, 18 x 16 | 0.075 - 0.250 | QR, Inc. Verona, Italy | 18 to 36 |
| PreXion3D Eclipse 3D | Yes | 8.1 x 7.5, 11.3 x 7.2 | 0.15 | PreXion, Inc. | 43344 |
| Planmeca ProMax 3D s | Yes | 8 x 8, 8 x 5, 5 x 8, 5 x 5 Stitched volume 14 x 10.5 x 8 | 0.075 -0.400 | Planmeca OY, Helsinki, Finland | 7.5-27 |
| 3D CBCT | No | 5 x 5, 6.1 x 7.8, 7.8 x 7.8, 7.8 x 15, 13 x 15 | 0.085- 0.420 | Soredex , Helsinki, Finland | 42979 |
| 9300 3D | Yes | 5 x 5, 8 x 8, 10 x 5, 10 x 10, 17 x 6, 17 x 11, 17 x 13.5 | 0.090 -0.500 | Carestream Health, Rochester, USA | 47088 |
| Gendex GXDP-70 | Yes | 6.1 x 4.1, 6.1 x 7.8 | 0.085 -0.300 | Gendex Dental Systems | 2.3 - 12.6 |
| Papaya 3D Plus | Yes | 4 x 5, 7 x 7, 8 x 8, 14 x 8, 14 x 14 | 0.075 -0.400 | Genoray America Inc | 42923 |
| Hyperion X9 | Yes | 5 x 5, 8 x 5, 8 x 8, 11 x 5, 11 x 8, 11 x 13 | 0.075 | MyRay | 18 |
| PaX-Reve3D | Yes | 5 x 5, 8 x 6, 12 x 8, 15 x 15, 15 x 19 | 0.08 - 0.25 | Vatech Korea | 15 / 24 |
Applications of CBCT in dentistry
Radiographic examination is essential in diagnosis and treatment planning in dentistry. Apart from compressing three-dimensional anatomy of the area being radiographed into a two-dimensional image, 2D imaging possesses unique inherent limitations (including magnification, distortion, and superimposition), together leading to misrepresentation of structures (19). CBCT produces 3D images useful for many oral and maxillofacial situations (Figure 5) that can guide in diagnosis and assessment of disease severity, planning and delivery of treatment, and follow-up.
Figure 5.
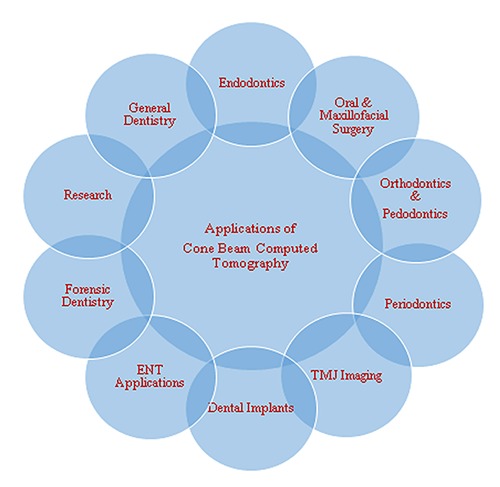
Applications of CBCT in various dental specialties.
Implantology: Missing teeth replacement by dental implants demands accurate assessment of the implant site for the successful implant placement and to avoid injury to contiguous vital structures. Most commonly 2D radiographs and in specific cases, conventional CT were employed for assessment of the implant site. Currently CBCT is the ideal choice (Figure 6), which has brought down implant failures by rendering accurate information about vital structures, height and width of the planned implant site, bone density and profile of the alveolus, while delivering low radiation exposure (25, 26, 27). CBCT can be employed in postsurgical assessments of bone grafts and the implant’s position in the alveolus (28). Furthermore, a surgical guide is prepared which provides accurate guidance for placement of the proposed implants (25, 29). Unlike Hounsfield unit (HU) numbers derived from conventional CT, the bone density numbers from CBCT are not accurate and cannot be correlated with HU units considering the image acquisition methods employed in CBCT machines; as a result, bone density numbers derived from this technology cannot be established over a group of CBCT machines or individuals (28).
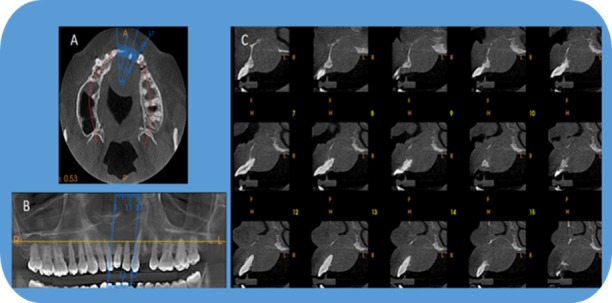
Figure 6.
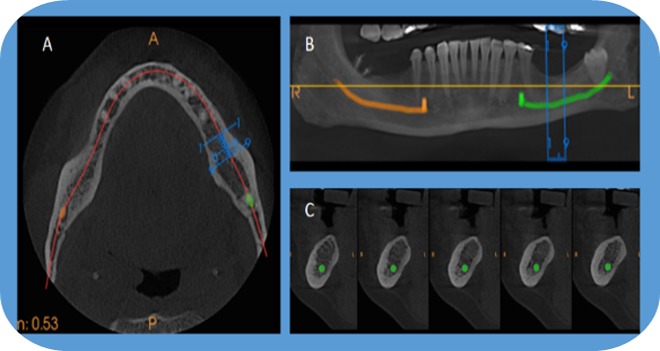
CBCT scan– MPR showing axial view (A) with curved line (red solid line) for “panoramic” view (B) and set of cross-sections, 1-mm-thick images (C) of a potential implant site in the lower left mandible. Blue lines on the axial and panoramic images indicate the location of the cross-sections. Apart from information of bone quality and dimensions, the cross-sections reveal the amount of lingual undercut and location of the inferior alveolar canal (green).
Oral and Maxillofacial Surgery: Because of extensive accessibility of CBCT, more dentists are utilizing these to assess oral and maxillofacial injury (Figure 7). Considering the limitations of 2D images like structural superimpositions, CBCT permits precise measurement of surface distances (30). These advantages of CBCT have made it the choice for exploring and handling midfacial and orbital fractures including dentoalveolar fractures (Figure 8), post fracture evaluation, interoperative visualization of the maxillofacial bones, and intraoperative navigation throughout procedures (31, 32). Intraoperative ability has also been assessed in mandibular fracture fixation (33). CBCT is being used to examine the precise location and extension of pathologies (odontogenic and non-odontogenic tumors, cysts) of the jaws (Figure 9 and Figure 10) as well as osteomyelitis (Figure 11) (34, 35). Pathologic calcifications (e.g., tonsilloliths, lymph nodes, salivary gland stones) can also be recognized in terms of location and distinguished from possibly noteworthy calcifications, such as those occurring in carotid artery (27, 35).The 3D views by CBCT for evaluation of unerupted / impacted or supernumerary teeth and their association with vital structures has been indispensable (Figure 12 and Figure 13) (36, 37).
Figure 7.
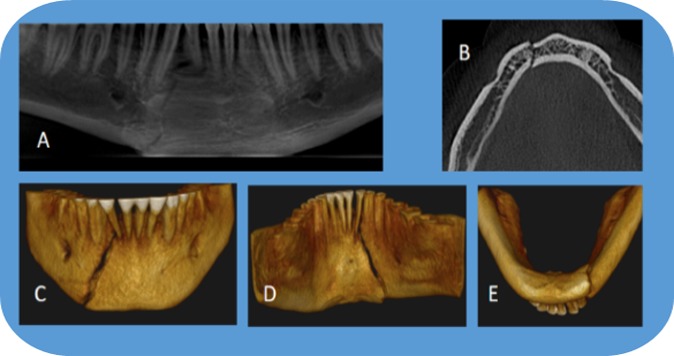
Three Dimensional visualization of right parasymphysis fracture of mandible on CBCT scan – Panoramic view (A), Axial view (B) and IVR (C, D, E).
Figure 8.
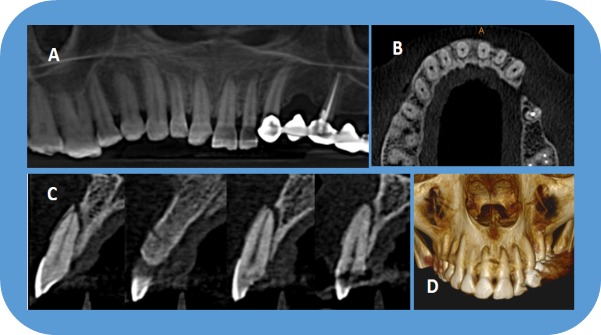
MPR is very useful in evaluating dentoalveolar fractures, which are easily missed on 2D imaging. The present CBCT scan reveals dentoalveolar fracture associated with maxillary anterior teeth in different display modes.
Figure 9.
CBCT scan - Axial image (A) with oblique curved line (Red solid line) and resultant “panoramic” image (B) and set of cross-sections, 1.1 mm thick images (C) of a left anterior region in the maxilla. The cross-sections revealing expansion and perforation of facial and palatal cortical plates due to radicular cyst.
Figure 10.
CBCT scan - Panoramic view (A), Axial view (B) Cross sections (C) and IVR (D) showing the radiographic features of Stafne bone cavity on the right side of the body of the mandible.
Figure 11.
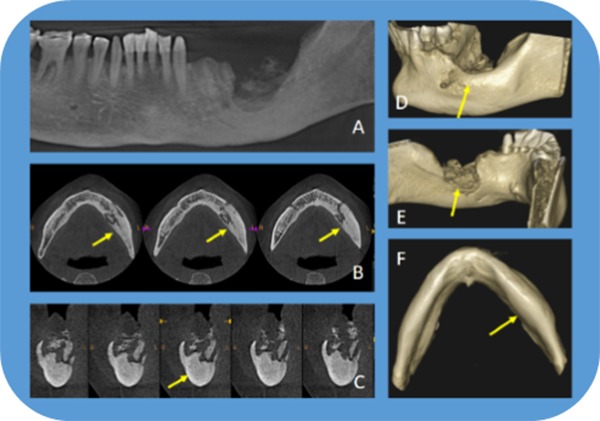
CBCT scan- Panoramic view (A), Axial views (B), crossections (C) and IVR reveal radiographic features (sequestration, altered density of trabecular bone, cortical expansion, compression of the mandibular canal) of a case of chronic osteomyelitis.
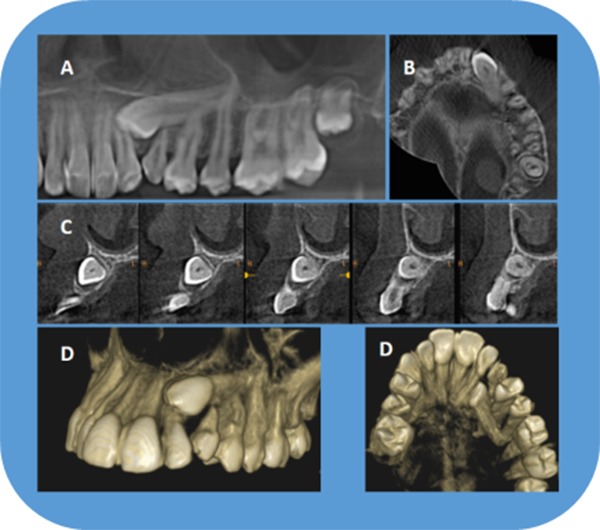
Figure 12.
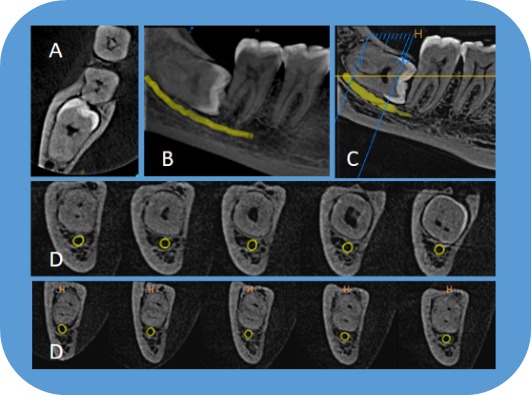
CBCT scan: Axial view (A) showing buccolingual positioning of crown and root of impacted third molar. Panoramic view (B and C) revealing relationship of third molar with mandibular canal and second molar. Set of cross sections (D) revealing the relationship with the mandibular canal.
Figure 13.
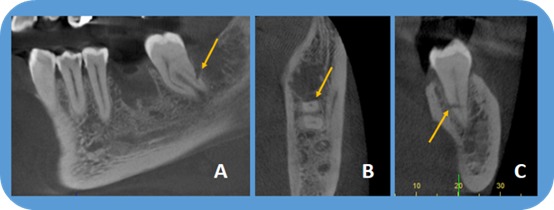
CBCT scan: Panoramic (A), Axial (B) views and (C) crossections reveal iatrogenic injury (accidental sectioning of distal root of second molar, yellow arrow) during third molar removal.
CBCT images are also employed for pre- and post-surgical evaluation of bone graft receiver sites and to assess osteonecrotic changes of the jaws like medication-related osteonecrosis of the jaw (38, 39). The morphologic appearances and degree of lesions in the para nasal air sinuses are predominantly well seen (e.g., retention pseudocyst) (Figure 14), although CBCT imaging does not provide suitable soft tissue contrast (10, 40). CBCT derived images are helpful for pre-treatment assessments of patients with obstructive sleep apnea (Figure 15) and to conclude suitable surgical method (41).
Figure 14.
CBCT (MPR, Panoramic view) revealing retention cyst in the both the maxillary sinuses.
Figure 15.
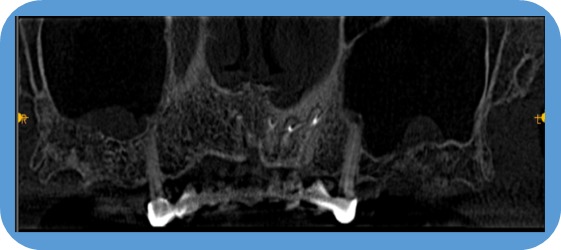
CBCT scans - Extended FOV for Orthodontic and Airway analysis.
Applications in orthodontics CBCT offers superimposition free images that are self-corrected for magnification, with a practical 1:1 measuring ratio, for morphometric analysis of structures and anatomic relationships essential for dealing with various orthodontic demands (Figure 15, Figure 16 and Figure 17). Some of the orthodontic uses include assessment of palatal bone thickness, skeletal growth patterns, dental age estimation, visualization of impacted teeth tooth inclination and torque, determining available alveolar bone width for buccolingual movement of teeth, upper airway assessment, and for planning orthognathic and facial orthomorphic surgeries (42, 43, 44, 45,). The availability of software like Dolphin and In Vivo Dental together with CBCT images for cephalometric analysis has turned out to be the best means for assessing facial growth, age, airway function, and disturbances in tooth eruption. CBCT provides pictorial guides for safe placement of miniimplants, evading accidental and irreparable injury to the vital structures (46, 47).
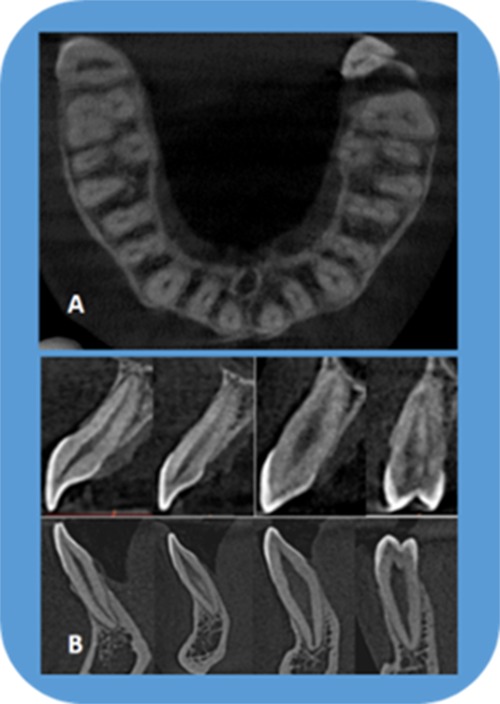
Figure 16.
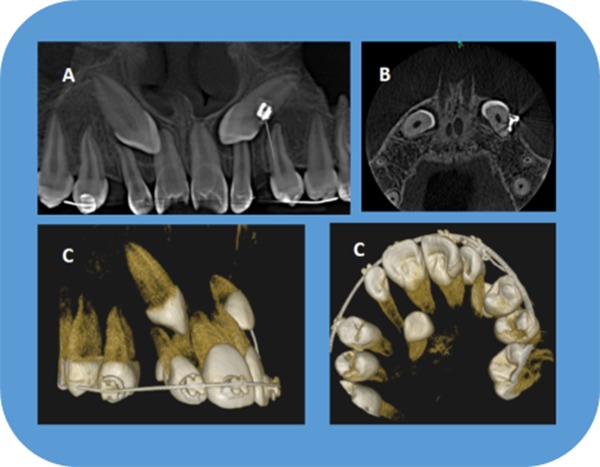
Orthodontic applications revealing evaluation of impacted canine by CBCT.
Figure 17.
CBCT images used for assessment of orthodontic treatment involving impacted canines.
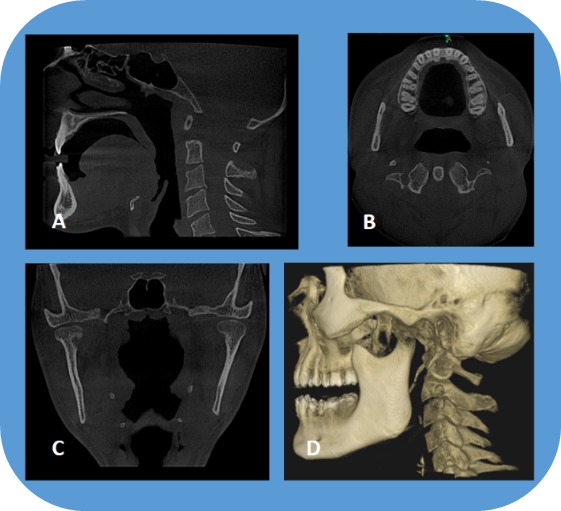
Applications in TMJ disorders: CBCT imaging offers multiplanar and possibly three-dimensional images of the condyle and surrounding structures to enable analysis of TMJ and function (Figure 18). Applicable TMJ imaging practices should comprise reformatted panoramic and axial reference images; corrected parasagittal and paracoronal crosssectional slices; and for cases in which asymmetry is suspected or surgery is a contemplated, volumetric reconstruction. CBCT enables to examine the joint space and the true position of the condyle within the fossa, which is helpful in revealing likely dislocation of the joint disk (48). Additionally CBCT enables to quantify the roof of the glenoid fossa and assists in locating the soft tissue around the TMJ, providing a practicable diagnosis and avoiding the necessity for Magnetic Resonance Imaging (49, 50). These benefits drawn above have made CBCT the best imaging device for cases involving developmental anomalies of the condyle, trauma, fibro-osseous ankylosis, pain, dysfunction, and condylar cortical erosion, rheumatoid arthritis and cysts (51, 52).
Figure 18.
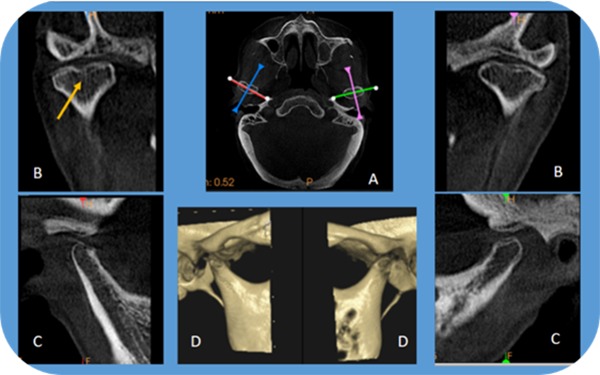
CBCT showing TMJ; Bilateral oblique MPR through lateral and medial poles of the condyle on the axial image showing coronal (B), sagittal view (C) and IVR (D) with right side showing bifid condyle (yellow arrow).
Applications in endodontics: The published literature suggests that CBCT imaging is superior to 2D imaging in the description of periapical lesions (Figure 19), precisely demonstrating lesion juxtaposition to the maxillary sinus, sinus membrane involvement (Figure 20), and lesion location relative to the mandibular canal (53, 54, 55). CBCT can be used to determine the number and morphology of roots and associated canals (both main and accessory) (Figure 21 and Figure 22), establish working lengths, and determine the type and degree of root angulation and as well provides true assessment of present root canal obturations (Figure 20) (53, 54, 55). Furthermore, CBCT has been suggested for classifying the source of the lesion as endodontic or non-endodontic, which may influence treatment plan (53). Detecting vertical root fractures (Figure 23 and Figure 24, measuring the depth of dentin fracture, and detecting horizontal root fractures comes handy due to absence of superimpositions and projection issues of 2D imaging (53, 54, 55, 56 ). CBCT imaging not only allows for early detection of root resorption (external or internal) as compared to 2D imaging, it can also identify the extent of a lesion. Depiction of pulpal extensions in talon cusps and the localization of broken instruments are simplified by CBCT images. Assessment of biomechanical preparation of root canals using various systems by CBCT images is practicable because of its reliability and precision (57, 58).
Figure 19.
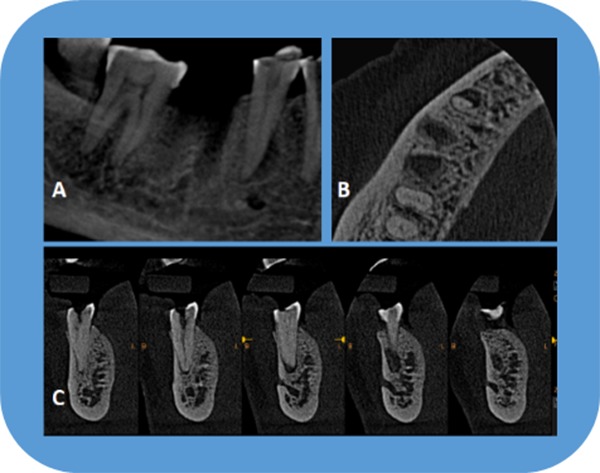
CBCT scans provide a three dimensional evaluation of periapical pathology along with information of the canal morphology. Present scan (a. panoramic view, b. Axial view and C. crossections) shows periapical lesion with right mandibular second premolar.
Figure 20.
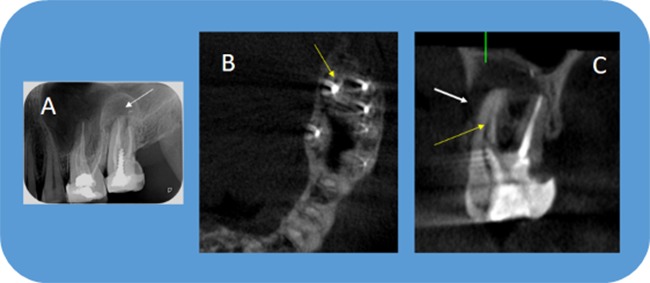
Periapical radiograph (A) shows root canal treated left maxillary second molar with periapical lesion. CBCT scans, axial (B) and coronal (C) view revealing missed distopalatal canal (yellow arrow) with periapical radiolucency and palatal perforation (white arrow) with intact floor of the maxillary sinus in relation to left maxillary second molar.
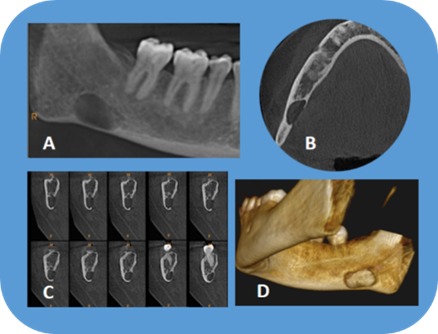
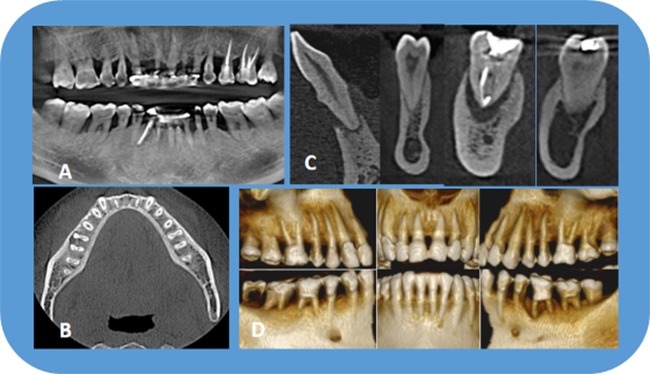
Figure 21.
CBCT images (axial and crossections) are indispensable in endodontics for the evaluation of morphology of the tooth including location and number of canals, pulp chamber size and degree of calcification, root structure, direction and curvature, fractures, iatrogenic defects, and the extent of dental caries. The images also allow measurements free from distortion and magnification.
Figure 22.
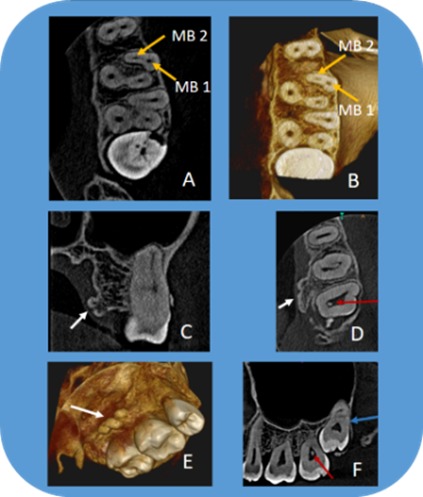
Small FOV, CBCT scan of left posterior maxilla showing MB2 canal in first molar (A, B), exostosis (C,D,E), pulp stone in second molar (D,F), third molar relationship with sinus (F), and the sinus devoid of any pathology.
Figure 23.
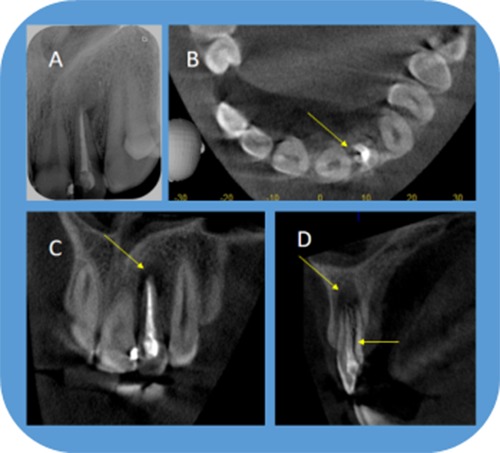
Periapical radiograph (A) showing root canal treated maxillary left lateral incisor without any significant changes. In the CBCT, axial (B), coronal (C) and sagittal (D) view showing periapical lesion with vertical root fracture (Yellow arrow).
Figure 24.
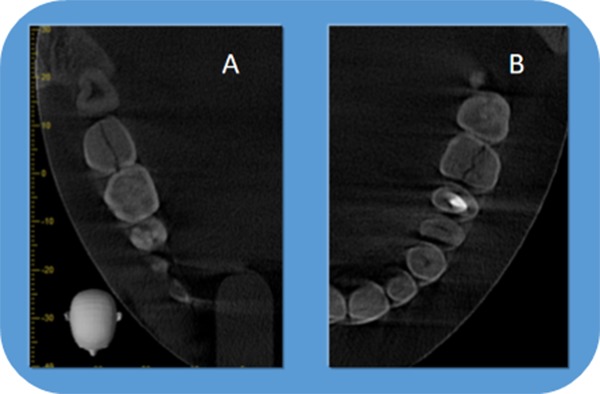
Axial views of two CBCT scans reveal vertical fracture in left lower second molar (A) and left maxillary first molar (B).
Applications in periodontics: For many decades, 2D imaging was the mainstay in periodontal diagnosis, however, their limitations led to under / over estimation of the bone loss (59).The literature has confirmed that morphometric analysis of periodontal diseases by CBCT to be as precise as direct measurement using a periodontal probe (60). In addition, CBCT is far better than 2D radiographs in visualization of buccal and lingual defects due to absence of superimposition of the structures. CBCT offers precise measurement of intrabony defects and lets clinicians to evaluate furcation involvement, dehiscence, fenestration defects, and periodontal cysts and to assess postsurgical consequences of regenerative periodontal treatment (Figure 25) (55, 60, 61).
Figure 25.
CBCT scan: Periodontal evaluation – Panoramic view (A) showing horizontal bone loss with furcation involvement. Axial views (B) are useful for evaluating furcation involvements where as crossections are particularly useful in evaluating buccal and lingual cortical plates as well as defining endo/ perio lesions. IVR (D) showing periodontal situation, which can used as tool for educating the patients.
Applications in forensic dentistry: One of the significant part of forensic dentistry is age estimation. Enamel is generally resistant to alterations beyond normal wear and tear; conversely, the pulpodentinal complex displays physiologic and pathological changes with progressing age. Characteristically, to quantify these changes, extraction and sectioning of teeth is necessary, which is not always a practicable choice. CBCT, however, affords a non-invasive substitute (62).
Virtual treatment planning and simulations: The software (primary or a third party) available with CBCT images allows virtual treatment planning (for e.g. implant planning) which can be transferred to surgical site either directly by the use of imageguided navigation or indirectly via the construction of surgical guides (10, 63, 64). The surgical guides can be a modification of a laboratory imaging stent or created using rapid prototyping. Rapid prototyping is a group of techniques used to quickly fabricate a scale model of a physical part or assembly using three-dimensional computer aided design (CAD) data. Construction of the part or assembly is usually done using 3D printing or “additive layer manufacturing” technology. The applications of rapid prototyping in dentistry include producing an actual size, dimensionally precise model of an anatomic structure. These models are employed for mock surgeries of numerous complex oral and maxillofacial situations, like trauma, tumor resection, distraction osteogenesis, and more commonly, dental implants. The practitioner can be instilled with high level of confidence beforehand and lessen the surgical and anesthetic time with these models (10, 63, 64).
Cone-beam Computed Tomography (CBCT) and stereophotography: Cone-beam Computed Tomography (CBCT) and stereophotography are two of the latest imaging modalities available for three-dimensional (3-D) visualization of craniofacial structures. CBCT image scan be fused with extraoral facial (photographic) or intraoral (impression) optical data for diagnosis of dentofacial deformities, assessment of the interaction of hard tissue base with the soft tissue integument; monitoring and evaluation of changes over time; and planning orthognathic surgery (64, 65). Apart from above discussed applications in dentistry, CBCT have uses in general radiology, mainly in otolaryngological (Figure 14, Figure 15 and Figure 26 ), musculoskeletal, breast, respiratory and cardiac imaging. CBCT has also been used in spinal surgery.
Figure 26.
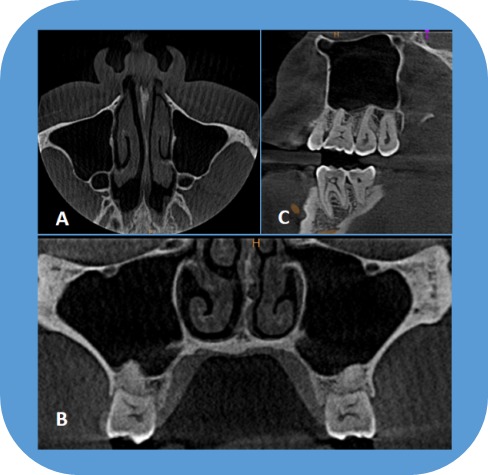
ENT applications of CBCT: MPR can be used for evaluation of paranasal air sinuses. Mild deviation of the nasal septum towards left side can be appreciated in the present scan along with other features of maxillary sinus
Conclusion
This paper stressed upon basics and the prospective uses of CBCT in the assessment of various oral and maxillofacial problems. So far, 2D imaging has assisted dentistry effectively and is bound to do so in the near future. CBCT imaging surpassed the obstacles of 2D imaging, offering practitioners with high quality, sub-millimeter resolution images, with short scanning time and low radiation dose. Since this equipment has become accompaniment of the dentist, dependence upon practice-based guess-estimations will be replaced, benefiting both patient and dentist. Huge scope is available for further applications and needs exploration from diagnosis to image guidance of dental procedures.
Footnotes
Source of funding: None declared.
Conflict of interest: None declared.
References
- 1.Goldman LW. Principles of CT and CT technology. J Nucl Med Technol. 2007. September;35(3):115–28. 10.2967/jnmt.107.042978 [DOI] [PubMed] [Google Scholar]
- 2.Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol. 1999. July;28(4):245–8. 10.1038/sj.dmfr.4600448 [DOI] [PubMed] [Google Scholar]
- 3.Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998;8(9):1558–64. 10.1007/s003300050586 [DOI] [PubMed] [Google Scholar]
- 4.Feldkamp LA, Davis LC, Kress JW. Practical cone-beam algorithm. J Opt Soc Am. 1984;1(6):612–9. 10.1364/JOSAA.1.000612 [DOI] [Google Scholar]
- 5.Danforth RA, Miles DA. Cone beam volume imaging (cbvi): 3d applications for dentistry. Irish Dent. 2007;10(9):14–8. [Google Scholar]
- 6.Howerton WB Jr, Mora MA. Advancements in digital imaging: what is new and on the horizon? J Am Dent Assoc. 2008. June;139 Suppl:20S–4S. 10.14219/jada.archive.2008.0354 [DOI] [PubMed] [Google Scholar]
- 7.Miracle AC, Mukherji SK. Conebeam CT of the head and neck, part 2: clinical applications. AJNR Am J Neuroradiol. 2009. August;30(7):1285–92. 10.3174/ajnr.A1654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. European Academy of Dental and Maxillofacial Radiology. Basic Principles for Use of Dental Cone Beam CT [Internet]. [Brussels]: European Academy of Dental and Maxillofacial Radiology; 2017. December [revised 2009 Jan; cited 2017 Dec 2]. [about 5 p.] Available from: http://eadmfr.eu/sites/default/files/donwloads/Basic_Principles_for_Use_of_Dental_Cone_Beam_CT.pdf. [Google Scholar]
- 9.Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006. February;72(1):75–80. [PubMed] [Google Scholar]
- 10.White SC, Pharoah M. Oral radiology principles and interpretation. St. Louis: Mosby Elsevier; 2014. pp. 199–212. [Google Scholar]
- 11.Gutierrez D, Monnin P, Valley JF, Verdun FR. A strategy to qualify the performance of radiographic monitors. Radiat Prot Dosimetry. 2005;114(1-3):192–7. 10.1093/rpd/nch565 [DOI] [PubMed] [Google Scholar]
- 12.Palomo L, Palomo JM. Cone beam CT for diagnosis and treatment planning in trauma cases [vi-vii.]. Dent Clin North Am. 2009. October;53(4):717–27. 10.1016/j.cden.2009.07.001 [DOI] [PubMed] [Google Scholar]
- 13.Razavi T, Palmer RM, Davies J, Wilson R, Palmer PJ. Accuracy of measuring the cortical bone thickness adjacent to dental implants using cone beam computed tomography. Clin Oral Implants Res. 2010. July;21(7):718–25. 10.1111/j.1600-0501.2009.01905.x [DOI] [PubMed] [Google Scholar]
- 14.Ludlow JB, Davies-Ludlow LE, Brooks SL. Dosimetry of two extraoral direct digital imaging devices: NewTom cone beam CT and Orthophos Plus DS panoramic unit. Dentomaxillofac Radiol. 2003. July;32(4):229–34. 10.1259/dmfr/26310390 [DOI] [PubMed] [Google Scholar]
- 15.Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006. July;35(4):219–26. 10.1259/dmfr/14340323 [DOI] [PubMed] [Google Scholar]
- 16.Ludlow JB, Davies-Ludlow LL, Mol A. Dosimetry of recently introduced cbct units for oral and maxillofacial radiology. Beijing, China: Proceedings of the 16th International Congress of Dentomaxillofacial Radiology, 26-30 June 2007, 97. [Google Scholar]
- 17.Mah JK, Danforth RA, Bumann A, Hatcher D. Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. October;96(4):508–13. 10.1016/S1079-2104(03)00350-0 [DOI] [PubMed] [Google Scholar]
- 18.Schulze D, Heiland M, Thurmann H, Adam G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofac Radiol. 2004. March;33(2):83–6. 10.1259/dmfr/28403350 [DOI] [PubMed] [Google Scholar]
- 19.Scarfe WC, Farman AG. What is cone-beam CT and how does it work? [v.]. Dent Clin North Am. 2008. October;52(4):707–30. 10.1016/j.cden.2008.05.005 [DOI] [PubMed] [Google Scholar]
- 20.Cohnen M, Kemper J, Möbes O, Pawelzik J, Mödder U. Radiation dose in dental radiology. Eur Radiol. 2002. March;12(3):634–7. 10.1007/s003300100928 [DOI] [PubMed] [Google Scholar]
- 21.Schulze R, Heil U, Gross D, Bruellmann DD, Dranischnikow E, Schwanecke U et al. . Artefacts in CBCT: a review. Dentomaxillofac Radiol. 2011. July;40(5):265–73. 10.1259/dmfr/30642039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Endo M, Tsunoo T, Nakamori N, Yoshida K. Effect of scattered radiation on image noise in cone beam CT. Med Phys. 2001. April;28(4):469–74. 10.1118/1.1357457 [DOI] [PubMed] [Google Scholar]
- 23.Farman AG. Guest editorial—Self-referral: an ethical concern with respect to multidimensional imaging in dentistry? J Appl Oral Sci. 2009. Sep-Oct;17(5):S1678-77572009000500001. 10.1590/S1678-77572009000500001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiegert J, Bertram M, Schafer D et al. . Soft tissue contrast resolution within the head of human cadaver by means of flat detector based cone-beam ct. Proc SPIE. 2004;5368(6):330–7. 10.1117/12.535191 [DOI] [Google Scholar]
- 25.Almog DM, LaMar J, LaMar FR, LaMar F. Cone beam computerized tomography-based dental imaging for implant planning and surgical guidance, Part 1: single implant in the mandibular molar region. J Oral Implantol. 2006;32(2):77–81. 10.1563/789.1 [DOI] [PubMed] [Google Scholar]
- 26.Tyndall DA, Price JB, Tetradis S, Ganz SD, Hildebolt C, Scarfe WC; American Academy of Oral and Maxillofacial Radiology . Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012. June;113(6):817–26. 10.1016/j.oooo.2012.03.005 [DOI] [PubMed] [Google Scholar]
- 27.Yajima A, Otonari-Yamamoto M, Sano T, Hayakawa Y, Otonari T, Tanabe K et al. . Cone-beam CT (CB Throne) applied to dentomaxillofacial region. Bull Tokyo Dent Coll. 2006. August;47(3):133–41. 10.2209/tdcpublication.47.133 [DOI] [PubMed] [Google Scholar]
- 28.Tischler M. In-office cone beam computerized tomography: technology review and clinical examples. Dent Today. 2008. June;27(6):102. [PubMed] [Google Scholar]
- 29.Nickenig HJ, Eitner S. Reliability of implant placement after virtual planning of implant positions using cone beam CT data and surgical (guide) templates. J Craniomaxillofac Surg. 2007. Jun-Jul;35(4-5):207–11. 10.1016/j.jcms.2007.02.004 [DOI] [PubMed] [Google Scholar]
- 30.Cevidanes LH, Bailey LJ, Tucker GR Jr, Styner MA, Mol A, Phillips CL et al. . Superimposition of 3D cone-beam CT models of orthognathic surgery patients. Dentomaxillofac Radiol. 2005. November;34(6):369–75. 10.1259/dmfr/17102411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heiland M, Schulze D, Rother U, Schmelzle R. Postoperative imaging of zygomaticomaxillary complex fractures using digital volume tomography. J Oral Maxillofac Surg. 2004. November;62(11):1387–91. 10.1016/j.joms.2004.05.215 [DOI] [PubMed] [Google Scholar]
- 32.Pohlenz P, Blessmann M, Blake F, Heinrich S, Schmelzle R, Heiland M. Clinical indications and perspectives for intraoperative cone-beam computed tomography in oral and maxillofacial surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007. March;103(3):412–7. 10.1016/j.tripleo.2006.05.008 [DOI] [PubMed] [Google Scholar]
- 33.Pohlenz P, Blessmann M, Blake F, Gbara A, Schmelzle R, Heiland M. Major mandibular surgical procedures as an indication for intraoperative imaging. J Oral Maxillofac Surg. 2008. February;66(2):324–9. 10.1016/j.joms.2007.03.032 [DOI] [PubMed] [Google Scholar]
- 34.Fullmer JM, Scarfe WC, Kushner GM, Alpert B, Farman AG. Cone beam computed tomographic findings in refractory chronic suppurative osteomyelitis of the mandible. Br J Oral Maxillofac Surg. 2007. July;45(5):364–71. 10.1016/j.bjoms.2006.10.009 [DOI] [PubMed] [Google Scholar]
- 35.Tetradis S, Anstey P, Graff-Radford S. Cone beam computed tomography in the diagnosis of dental disease. J Calif Dent Assoc. 2010. January;38(1):27–32. [PubMed] [Google Scholar]
- 36.Liu DG, Zhang WL, Zhang ZY, Wu YT, Ma XC. Localization of impacted maxillary canines and observation of adjacent incisor resorption with cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008. January;105(1):91–8. 10.1016/j.tripleo.2007.01.030 [DOI] [PubMed] [Google Scholar]
- 37.Pawelzik J, Cohnen M, Willers R, Becker J. A comparison of conventional panoramic radiographs with volumetric computed tomography images in the preoperative assessment of impacted mandibular third molars. J Oral Maxillofac Surg. 2002. September;60(9):979–84. 10.1053/joms.2002.34399 [DOI] [PubMed] [Google Scholar]
- 38.Hamada Y, Kondoh T, Noguchi K, Iino M, Isono H, Ishii H et al. . Application of limited cone beam computed tomography to clinical assessment of alveolar bone grafting: a preliminary report. Cleft Palate Craniofac J. 2005. March;42(2):128–37. 10.1597/03-035.1 [DOI] [PubMed] [Google Scholar]
- 39.Kumar V, Pass B, Guttenberg SA, Ludlow J, Emery RW, Tyndall DA et al. . Bisphosphonate-related osteonecrosis of the jaws: a report of three cases demonstrating variability in outcomes and morbidity. J Am Dent Assoc. 2007. May;138(5):602–9. 10.14219/jada.archive.2007.0230 [DOI] [PubMed] [Google Scholar]
- 40.American Dental Association Council on Scientific Affairs The use of cone-beam computed tomography in dentistry: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2012. August;143(8):899–902. 10.14219/jada.archive.2012.0295 [DOI] [PubMed] [Google Scholar]
- 41.Ogawa T, Enciso R, Shintaku WH, Clark GT. Evaluation of cross-section airway configuration of obstructive sleep apnea. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007. January;103(1):102–8. 10.1016/j.tripleo.2006.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aboudara CA, Hatcher D, Nielsen IL, Miller A. A three-dimensional evaluation of the upper airway in adolescents. Orthod Craniofac Res. 2003;6(s1 Suppl 1):173–5. 10.1034/j.1600-0544.2003.253.x [DOI] [PubMed] [Google Scholar]
- 43.Harrell WE., Jr Three-dimensional diagnosis and treatment planning: the use of 3d facial imaging and 3d cone beam CT in orthodontics and dentistry. Aust Dent Pract. 2007;18(4):102–13. [Google Scholar]
- 44.Kapila S, Conley RS, Harrell WE Jr. The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac Radiol. 2011. January;40(1):24–34. 10.1259/dmfr/12615645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peck JL, Sameshima GT, Miller A, Worth P, Hatcher DC. Mesiodistal root angulation using panoramic and cone beam CT. Angle Orthod. 2007. March;77(2):206–13. 10.2319/0003-3219(2007)077[0206:MRAUPA]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- 46.Kim SH, Choi YS, Hwang EH, Chung KR, Kook YA, Nelson G. Surgical positioning of orthodontic mini-implants with guides fabricated on models replicated with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2007. April;131(4 Suppl):S82–9. 10.1016/j.ajodo.2006.01.027 [DOI] [PubMed] [Google Scholar]
- 47.Kim SH, Kang JM, Choi B, Nelson G. Clinical application of a stereolithographic surgical guide for simple positioning of orthodontic mini-implants. World J Orthod. 2008;9(4):371–82. [PubMed] [Google Scholar]
- 48.Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol. 2004. May;33(3):196–201. 10.1259/dmfr/27403192 [DOI] [PubMed] [Google Scholar]
- 49.Honda K, Matumoto K, Kashima M, Takano Y, Kawashima S, Arai Y. Single air contrast arthrography for temporomandibular joint disorder using limited cone beam computed tomography for dental use. Dentomaxillofac Radiol. 2004. July;33(4):271–3. 10.1259/dmfr/50972902 [DOI] [PubMed] [Google Scholar]
- 50.Kijima N, Honda K, Kuroki Y, Sakabe J, Ejima K, Nakajima I. Relationship between patient characteristics, mandibular head morphology and thickness of the roof of the glenoid fossa in symptomatic temporomandibular joints. Dentomaxillofac Radiol. 2007. July;36(5):277–81. 10.1259/dmfr/56344782 [DOI] [PubMed] [Google Scholar]
- 51.Honda K, Larheim TA, Johannessen S, Arai Y, Shinoda K, Westesson PL. Ortho cubic super-high resolution computed tomography: a new radiographic technique with application to the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001. February;91(2):239–43. 10.1067/moe.2001.111942 [DOI] [PubMed] [Google Scholar]
- 52.Sakabe R, Sakabe J, Kuroki Y, Nakajima I, Kijima N, Honda K. Evaluation of temporomandibular disorders in children using limited cone-beam computed tomography: a case report. J Clin Pediatr Dent. 2006;31(1):14–6. 10.17796/jcpd.31.1.n1v37664753631r1 [DOI] [PubMed] [Google Scholar]
- 53.Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG. Endodontic applications of cone-beam volumetric tomography. J Endod. 2007. September;33(9):1121–32. 10.1016/j.joen.2007.06.011 [DOI] [PubMed] [Google Scholar]
- 54.Nakata K, Naitoh M, Izumi M, Inamoto K, Ariji E, Nakamura H. Effectiveness of dental computed tomography in diagnostic imaging of periradicular lesion of each root of a multirooted tooth: a case report. J Endod. 2006. June;32(6):583–7. 10.1016/j.joen.2005.09.004 [DOI] [PubMed] [Google Scholar]
- 55.Tyndall DA, Rathore S. Cone-beam CT diagnostic applications: caries, periodontal bone assessment, and endodontic applications [vii.]. Dent Clin North Am. 2008. October;52(4):825–41. 10.1016/j.cden.2008.05.002 [DOI] [PubMed] [Google Scholar]
- 56.Ozer SY. Detection of vertical root fractures of different thicknesses in endodontically enlarged teeth by cone beam computed tomography versus digital radiography. J Endod. 2010. July;36(7):1245–9. 10.1016/j.joen.2010.03.021 [DOI] [PubMed] [Google Scholar]
- 57.Nagaraja S, Sreenivasa Murthy BV. CT evaluation of canal preparation using rotary and hand NI-TI instruments: an in vitro study. J Conserv Dent. 2010. January;13(1):16–22. 10.4103/0972-0707.62636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Siraci E, Cem Gungor H, Taner B, Cehreli ZC. Buccal and palatal talon cusps with pulp extensions on a supernumerary primary tooth. Dentomaxillofac Radiol. 2006. November;35(6):469–72. 10.1259/dmfr/64715224 [DOI] [PubMed] [Google Scholar]
- 59.Vandenberghe B, Jacobs R, Yang J. Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT-images for assessing periodontal breakdown. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007. September;104(3):395–401. 10.1016/j.tripleo.2007.03.012 [DOI] [PubMed] [Google Scholar]
- 60.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006. July;77(7):1261–6. 10.1902/jop.2006.050367 [DOI] [PubMed] [Google Scholar]
- 61.Ito K, Yoshinuma N, Goke E, Arai Y, Shinoda K. Clinical application of a new compact computed tomography system for evaluating the outcome of regenerative therapy: a case report. J Periodontol. 2001. May;72(5):696–702. 10.1902/jop.2001.72.5.696 [DOI] [PubMed] [Google Scholar]
- 62.Yang F, Jacobs R, Willems G. Dental age estimation through volume matching of teeth imaged by cone-beam CT. Forensic Sci Int. 2006. May;159 Suppl 1:S78–83. 10.1016/j.forsciint.2006.02.031 [DOI] [PubMed] [Google Scholar]
- 63.Abou-ElFetouh A, Barakat A, Abdel-Ghany K. Computer-guided rapid-prototyped templates for segmental mandibular osteotomies: a preliminary report. Int J Med Robot. 2011. June;7(2):187–92. 10.1002/rcs.387 [DOI] [PubMed] [Google Scholar]
- 64.Jayaratne YS, Zwahlen RA, Lo J, Tam SC, Cheung LK. Computer-aided maxillofacial surgery: an update. Surg Innov. 2010. September;17(3):217–25. 10.1177/1553350610371626 [DOI] [PubMed] [Google Scholar]
- 65.D’Urso PS, Barker TM, Earwaker WJ, Bruce LJ, Atkinson RL, Lanigan MW et al. . Stereolithographic biomodelling in cranio-maxillofacial surgery: a prospective trial. J Craniomaxillofac Surg. 1999. February;27(1):30–7. 10.1016/S1010-5182(99)80007-9 [DOI] [PubMed] [Google Scholar]


