Abstract
Numerous positive properties of glass ionomer cements including biocompatibility, bioactivity, releasing of fluoride and good adhesion to hard dental tissue even under wet conditions and easy of handling are reasons for their wide use in paediatric and restorative dentistry. Their biggest drawbacks are the weaker mechanical properties. An important step forward in improving GIC’s features is thermo-curing with the dental polymerization unit during setting of the material. Due to their slow setting characteristics the GIC is vulnerable to early exposure to moisture. After thermo curing, cements retain all the benefits of GIC with developed better mechanical properties, improved marginal adaptation, increased microhardness and shear bond strength. Adding external energy through thermocuring or ultrasound during the setting of conventional GIC is crucial to achieve faster and better initial mechanical properties. Further clinical studies are needed to confirm these findings.
Keywords: Glass ionomer, mechanical properties, thermo-curing, ultrasound
Introduction
Glass ionomer cements (GICs) are very suitable material for restorations in paediatric dentistry. Many properties like self adhesiveness, fluoride release and hydrophilic behaviour make GICs as a material of choice for restorations of deciduous teeth and young permanent teeth (1, 2). Properties of glass ionomers for restorations like biocompatibility, bioactivity, remineralization of the carious process and prophylactic effect on all teeth in the oral cavity make them very suitable for everyday use in clinical practice (2, 3, 4, 5, 6). In addition to this GIC has the ability of good adhesion to hard dental tissues, even under wet conditions where optimal moisture control is not possible and easy of handling is reasons for their wide application in children. GIC is specially indicated when it is difficult to achieve optimal control of the dry working field due to poor patient cooperative activity (7). The lack of patient co-operation is most common in young children and in mentally or physically compromised patients. Patients with special needs are also classified into a high risk caregiver group and some nano-ionomer material or thermo-cured conventional GIC is also material of choice (7, 8).
Their biggest drawbacks are the weaker mechanical properties. An important step forward in improving GIC’s features is thermo-curing. For this purpose simple dental polymerization unit emitting heat can be used during initial setting of the material (8, 9, 10, 11). Due to their slow setting characteristics the GIC is vulnerable to early exposure to moisture. After thermo-curing, cements retain all the benefits of GIC with developed better initial mechanical properties. Thermo-curing of the GIC during setting also decrease microleakage and improves marginal adaptation (8) as well as increase microhardness and shear bond strength of the restoration (9). Adding external energy through thermo-curing or ultrasound during the setting of conventional GIC is crucial to achieve faster and better initial mechanical properties (8, 9, 10, 11, 12). The use of ultrasonic vibrations to change the setting of glass ionomer cements was reported by Towler et al. (12). It has been described that ultrasound could produce a marked acceleration in setting of GIC and increase adhesion to the hard tooth substances (13, 14). The effect on chemical setting processes has not been reported. Results of different research groups showed that some mechanical properties of GIC could be improved (8, 9, 10, 11, 12, 14, 15). Addition of external energy during setting of GIC is crucial for achievement of better properties. Conventional glass ionomers can be thermo-cured by application of heat from dental polymerization lamps, which causes acceleration in the setting. The acceleration of setting leads to better mechanical properties especially early mechanical properties and decrease marginal leakage. Gorseta et al. (8) have suggested that the use of dental polymerization lamp can be used as a source of heat in order to achieve improved early mechanical properties of GICs. GIC interacts with calcium from the enamel creating an enamel-like structure that is more stable and more resistant to demineralization (so-called pseudo-enamel). In cariogenic conditions, release is suddenly increased and supported by the precipitation phase that stops the progression of the caries (6).
Recent studies confirmed that adding external energy could promote faster setting of conventional GIC. Some authors have tried to accelerate reaction using ultrasonic excitation, heat curing with warm metal plates or heat application using light-curing dental units. Kleverlaan et al. (10) demonstrated the mechanical properties of some conventional glass ionomers after curing with ultrasound and also after heat curing between warm metal plates. They found a significant increase in mechanical properties comparing with GICs without additional curing methods. Gorseta et al. (9) found increased bond strength of GICs to enamel in thermo-cured groups. Billington and Williams (16) investigated the influence of temperature on compressive strength, showing significant increase at temperature higher than 37°C. Nicholson and Czarnecka (17) suggested that application of heat evaporated part of the unbound water in the cement matrix and accelerated the chemical reaction. In clinical practice the temperature rise during heating might have influence on the pulp tissue. Santini et al. (18) have investigated the pulp temperature rise during composite polymerization. LED units demonstrated higher temperature rise (3- 7.1°C) then halogen units (2.8-4.9°C). According to Zach and Cohen (19) the pulp vitality can be affected when the rise is 5-6°C. In vivo absorption of the heat is possible by gingival tissue and also blood flow through pulp tissue absorbs some amount of heat (18). Generally, GICs has acceptable thermal properties for clinical use such as thermal conductivity. Gavic et al. (20) measured the relative small temperature rises at greatest depths of GICs and showed that the cements transmit a small amount of the thermal energy. Such transmission leads to increases in temperature of 5–6 °C at depths of 3–4 mm within the cement. The heat transmission through the GICs was insufficient to affect the pulp tissue, suggesting that thermo-curing with dental polymerization lights of this type is a safe for clinical use (21). However, accelerating the setting reaction should be avoided when the cements are used as cavity liners close to the pulp tissue and in layers less than 2 mm thick (20).
Marginal leakage
Glass ionomers are also subjected to microleakage that allows oral bacteria to migrate along marginal gap. Decrease of marginal leakage of GIC restorations were demonstrated on enamel margine in cavity with conditioning. GICs are not enough acidic to remove the smear layer. It depends on a number of factors such as type of polyacid matrix, concentration of acid solution and power/liquid ratio (9, 22, 23). There was also a significant difference between capsulated and hand mixed GIC. Gorseta et al. (8) used class V cavities filled with GICs that were heated with dental polymerization unit during setting period. Some groups of samples were cured with ultrasound as a ‘setting on command’. Results showed that both groups cured with ultrasound and heated group had decrease in marginal leakage and showed better marginal adaptation comparing to chemical setting of GIC. Lower porosities were shown inside of GICs in heated and ultrasound cured restorations comparing to standard curing. (Figure 1) Heat cured GIC restorations appeared more homogenous.
Figure 1.
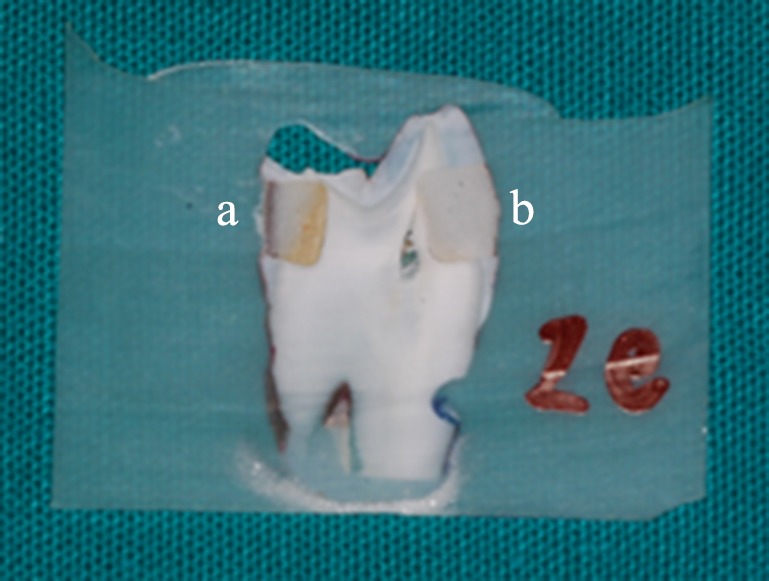
Class V cavities filled with GIC: A- dye penetration inside the material (standard chemical setting) and B- no dye penetration, homogenous material (thermo-cured for 40s).
Shear bond test
Bond strength relates to the ability of the materials to interact with the under laying enamel. Conventional GIC is able to penetrate the smear layer through a self-etching process and affect a bond to the under laying enamel. If this smear layer is removed, material has a greater ability to interact with the enamel and the measured bond strength is higher (22). Gorseta et al. (8) demonstrated increased bond strength of GIC to enamel after thermo-curing during setting time. Failure mode analysis for the bond strength specimens are depended on enamel treatments and curing mode of GIC. The most of cohesive mode of failure was observed in thermo-cured and ultrasonic cured groups of GIC. (Figure 2)
Figure 2.
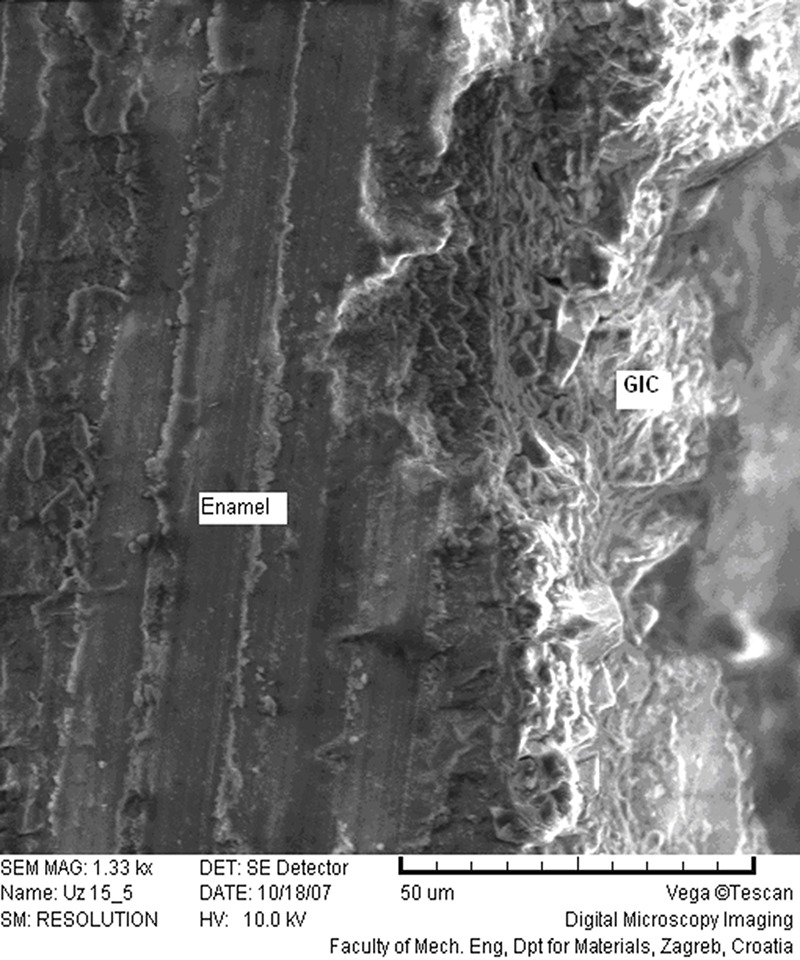
Scanning electron micrographs of fractured GIC on enamel. Failure occured in the material above ion-exchange layer.
Microhardness
GIC are usually weak after setting and still vulnerable to moisture. Microhardness is a very important for the resistance of material during the first hours after placing. Gavic et al. (24) demonstrated that thermo-light curing of GIC increases the microhardness of the GICs at the surface and also at depths of 1, 2, 3 and 4 mm. Surfaces of GICs were thermo-cured with different polymerization units for 60s during setting reaction. In this study it was shown that thermo curing may increase resistance to mastication forces which is important for clinical success of GIC restorations.
Fissure sealing
Dental surfaces with pits and fissures are particularly susceptible to caries development. As a preventative measure, the fissure sealing with the material which is attached to the adhesive enamel is either micromechanical or through chemical bonding of the material and tooth tissue (25). Anatomical relationships may also make it difficult to isolate the tooth, for example, the crown of the erupting tooth with gingival covering. Then, the advantage of GIC is also evident. Simplicity in the work phases (not mandatory conditioning, does not require the application of the adhesive system), and faster cure mode (dental polymerization lamp produces heat that accelerates the curing process by up to 30%), all these are the advantages of clinically working with GIC much simpler (26, 27). ART sealants using highviscosity glass-ionomer (HVGIC) have a very high dentine carious lesion prevention rate. The survival rate of these sealants is not significantly different from that of sealants produced with resin (28). Glass Carbomer material showed a similar retention rate when compared with a resin-based sealant. Glass Carbomer is a new generation of restorative material developed from glass-ionomer cements with possibility of gradual mineralization into fluorapatite. The retention of Glass Carbomer fissure sealant after 12 months was similar to a commonly used conventional resin-based sealant (29).
Atraumatic restorative treatment
The atraumatic restorative treatment (ART) concept is an example of minimal intervention dentistry (28). For developing countries with a poor dental care system where electricity is not available, GIC is a material of choice for restorative procedures as well as for preventing further caries progression (2). Also, it could be used as behaviuor management procedure in contemporary clinical setting. ART is based on the knowledge that the dentinal layer has the potential for remineralization of calcium phosphate if a soft destroyed dentin is removed. GIC continues to release fluoride after application into the cavity thereby contributing to stopping and preventing caries around the fill (9). The survival rate of ART restorations matches those of amalgam and resin composite in single- and multiple-surface cavities in primary teeth and in single-surface cavities in permanent teeth. The annual dentine carious lesion development in teeth with high-viscosity glassionomer ART sealants over the first three years is 1%. These ART sealants have a high capacity of preventing carious lesion development (30). Hall technique is a non-invasive treatment for decayed primary molar teeth. Decay is sealed under preformed stainless steel crowns (SSC) involving no caries removal, no crown preparation and no use of local anaesthetic before placement of crowns (31). It is biologically orientated approach for managing dental decay. Ludwig et al. (31) showed a similar success rate for SSCs placed with the traditional technique or the Hall technique. Today is available hydroxyapatite enhancing glass ionomer cement. Glass Carbomer cement represents a new generation of dental material, which mineralizes gradually into fluorapatite, demonstrates good toughness and strength of material and better fluoride release than its predecessors. Glass Carbomer is described as a material with less sensitivity to abrasion and wear, stiffness, glazier surface, better adhesion and less moisture sensitivity (29).
Conclusion
Adding external energy through thermo-curing as a ”Command set” method during the setting of conventional GIC is crucial to achieve faster and better initial mechanical properties.
Footnotes
Source of funding: None declared.
Conflict of interest: None declared.
References
- 1.Khoroushi M, Keshani F. A review of glass-ionomers: from conventional glass-ionomer to bioactive glass-ionomer. Dent Res J (Isfahan). 2013. July;10(4):411–20. [PMC free article] [PubMed] [Google Scholar]
- 2.Lohbauer U. Dental glass ionomer cements as permanent filling material? Properties, limitations and future trends. Materials (Basel). 2010;3(1):76–96. 10.3390/ma3010076 [DOI] [Google Scholar]
- 3.De Witte AM, De Maeyer EA, Verbeeck RM, Martens LC. Fluoride release profiles of mature restorative glass ionomer cements after fluoride application. Biomaterials. 2000. March;21(5):475–82. 10.1016/S0142-9612(99)00188-X [DOI] [PubMed] [Google Scholar]
- 4.Mount GJ. Glass ionomers: a review of their current status. Oper Dent. 1999. Mar-Apr;24(2):115–24. [PubMed] [Google Scholar]
- 5.Segura A, Donly KJ, Stratmann RG. Enamel remineralization on teeth adjacent to Class II glass ionomer restorations. Am J Dent. 1997. October;10(5):247–50. [PubMed] [Google Scholar]
- 6.ten Cate JM, van Duinen RN. Hypermineralization of dentinal lesions adjacent to glass-ionomer cement restorations. J Dent Res. 1995. June;74(6):1266–71. 10.1177/00220345950740060501 [DOI] [PubMed] [Google Scholar]
- 7.Francisconi LF, Scaffa PM, de Barros VR, Coutinho M, Francisconi PA. Glass ionomer cements and their role in the restoration of non-carious cervical lesions. J Appl Oral Sci. 2009. Sep-Oct;17(5):364–9. 10.1590/S1678-77572009000500003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gorseta K, Glavina D, Skrinjaric I. Influence of ultrasonic excitation and heat application on the microleakage of glass ionomer cements. Aust Dent J. 2012. December;57(4):453–7. 10.1111/j.1834-7819.2012.01724.x [DOI] [PubMed] [Google Scholar]
- 9.Gorseta K, Skrinjarić T, Glavina D. The effect of heating and ultrasound on the shear bond strength of glass ionomer cement. Coll Antropol. 2012. December;36(4):1307–12. [PubMed] [Google Scholar]
- 10.Kleverlaan CJ, van Duinen RN, Feilzer AJ. Mechanical properties of glass ionomer cements affected by curing methods. Dent Mater. 2004. January;20(1):45–50. 10.1016/S0109-5641(03)00067-8 [DOI] [PubMed] [Google Scholar]
- 11.O’Brien T, Shoja-Assadi F, Lea SC, Burke FJ, Palin WM. Extrinsic energy sources affect hardness through depth during set of a glass-ionomer cement. J Dent. 2010. June;38(6):490–5. 10.1016/j.jdent.2010.03.004 [DOI] [PubMed] [Google Scholar]
- 12.Towler MR, Bushby AJ, Billington RW, Hill RG. A preliminary comparison of the mechanical properties of chemically cured and ultrasonically cured glass ionomer cements, using nano-indentation techniques. Biomaterials. 2001. June;22(11):1401–6. 10.1016/S0142-9612(00)00297-0 [DOI] [PubMed] [Google Scholar]
- 13.Guglielmi CA, Mohana A, Hesse D, Lenzi TL, Bonini GC, Raggio DP. Influence of ultrasound or halogen light on microleakage and hardness of enamel adjacent to glass ionomer cement. Int J Paediatr Dent. 2012. March;22(2):110–5. 10.1111/j.1365-263X.2011.01173.x [DOI] [PubMed] [Google Scholar]
- 14.Tanner DA, Rushe N, Towler MR. Ultrasonically set glass polyalkenoate cements for orthodontic applications. J Mater Sci Mater Med. 2006. April;17(4):313–8. 10.1007/s10856-006-8229-7 [DOI] [PubMed] [Google Scholar]
- 15.Fagundes TC, Barata TJ, Bresciani E, Cefaly DF, Carvalho CA, Navarro MF. Influence of ultrasonic setting on tensile bond strength of glass-ionomer cements to dentin. J Adhes Dent. 2006. December;8(6):401–7. [PubMed] [Google Scholar]
- 16.Williams JA, Billington RW. Changes in compressive strength of glass ionomer restorative materials with respect to time periods of 24 h to 4 months. J Oral Rehabil. 1991. March;18(2):163–8. 10.1111/j.1365-2842.1991.tb00044.x [DOI] [PubMed] [Google Scholar]
- 17.Nicholson JW, Czarnecka B. Kinetic studies of water uptake and loss in glass-ionomer cements. J Mater Sci Mater Med. 2008. April;19(4):1723–7. 10.1007/s10856-007-3244-x [DOI] [PubMed] [Google Scholar]
- 18.Santini A, Watterson C, Miletic V. Temperature rise within the pulp chamber during composite resin polymerisation using three different light sources. Open Dent J 2008;2(137-141. [DOI] [PMC free article] [PubMed]
- 19.Zach L, Cohen G. Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol. 1965. April;19(4):515–30. 10.1016/0030-4220(65)90015-0 [DOI] [PubMed] [Google Scholar]
- 20.Gavic L, Gorseta K, Glavina D, Czarnecka B, Nicholson JW. Heat transfer properties and thermal cure of glass-ionomer dental cements. J Mater Sci Mater Med. 2015. October;26(10):249. 10.1007/s10856-015-5578-0 [DOI] [PubMed] [Google Scholar]
- 21.van Duinen RN, Shahid S, Hill R, Glavina D. In-vitro study on temperature changes in the pulp chamber due to thermo-cure glass ionomer cements. Acta Stomatol Croat. 2016. December;50(4):287–91. 10.15644/asc50/4/1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glasspoole EA, Erickson RL, Davidson CL. Effect of surface treatments on the bond strength of glass ionomers to enamel. Dent Mater. 2002. September;18(6):454–62. 10.1016/S0109-5641(01)00068-9 [DOI] [PubMed] [Google Scholar]
- 23.Yilmaz Y, Gurbuz T, Kocogullari ME. The influence of various conditioner agents on the interdiffusion zone and microleakage of a glass lonomer cement with a high viscosity in primary teeth. Oper Dent. 2005. Jan-Feb;30(1):105–12. [PubMed] [Google Scholar]
- 24.Gavic L, Gorseta K, Borzabadi-Farahani A, Tadin A, Glavina D, van Duinen RN et al. Influence of thermo-light curing with dental light-curing units on the microhardness of glass-ionomer cements. Int J Periodontics Restorative Dent. 2016. May-Jun;36(3):425–30. 10.11607/prd.2405 [DOI] [PubMed] [Google Scholar]
- 25.Wendt LK, Koch G, Birkhed D. Long-term evaluation of a fissure sealing programme in Public Dental Service clinics in Sweden. Swed Dent J. 2001;25(2):61–5. [PubMed] [Google Scholar]
- 26.Herle GP, Joseph T, Varma B, Jayanthi M. Comparative evaluation of glass ionomer and resin based fissure sealant using noninvasive and invasive techniques—a SEM and microleakage study. J Indian Soc Pedod Prev Dent. 2004. June;22(2):56–62. [PubMed] [Google Scholar]
- 27.Skrinjaric K, Vranic DN, Glavina D, Skrinjaric I. Heat-treated glass ionomer cement fissure sealants: retention after 1 year follow-up. Int J Paediatr Dent. 2008. September;18(5):368–73. 10.1111/j.1365-263X.2007.00896.x [DOI] [PubMed] [Google Scholar]
- 28.Frencken JE. Atraumatic restorative treatment and minimal intervention dentistry. Br Dent J. 2017. August;223(3):183–9. 10.1038/sj.bdj.2017.664 [DOI] [PubMed] [Google Scholar]
- 29.Gorseta K, Glavina D, Borzabadi-Farahani A, Van Duinen RN, Skrinjaric I, Hill RG et al. One-year clinical evaluation of a Glass Carbomer fissure sealant, a preliminary study. Eur J Prosthodont Restor Dent. 2014. June;22(2):67–71. [PubMed] [Google Scholar]
- 30.Frencken JE. The state-of-the-art of art sealants. Dent Update 2014;41(2):119-120, 122-114. 10.12968/denu.2014.41.2.119 [DOI] [PubMed]
- 31.Ludwig KH, Fontana M, Vinson LA, Platt JA, Dean JA. The success of stainless steel crowns placed with the Hall technique: a retrospective study. J Am Dent Assoc. 2014. December;145(12):1248–53. 10.14219/jada.2014.89 [DOI] [PubMed] [Google Scholar]


