Abstract
A 45-year old man with intermittent dyspnea was found to have a large mediastinal mass on chest radiograph. Computerized tomography scan revealed a 14.7 cm anterior mediastinal mass with cystic and solid components. The patient underwent a thoracoscopic resection of the mass without complication. Techniques utilized during this surgery may be helpful in avoiding pitfalls for other surgeons.
INTRODUCTION
Benign thymic cysts are rare, accounting for ~3% of mediastinal masses, and patients may be asymptomatic for years [1, 2]. As such, the literature regarding large thymic cysts is scarce. The clinical course of mediastinal cysts is unknown and management largely depends on size and presence of symptoms. Infectious complications and compressive symptoms are known effects of untreated thymic cysts [3].
Video-assisted thoracoscopic surgery (VATS) has been reserved for smaller thymic cysts with the use of multiple thoracoscopic ports. In the adult literature, an open thymectomy approach has been preferred for thymomas or thymic cysts that demonstrate vascular invasion or have a diameter greater than 5 cm in most studies [4, 5]. We report the removal of a giant thymic cyst using a one-port approach.
CASE REPORT
A 45-year-old man with dyspnea was referred to our institution after a large mass was discovered on chest radiograph. The patient’s past medical history was significant for asthma and latent tuberculosis [6]. Over the last year he had developed intermittent dyspnea, after participation sports. Otherwise, his physical examination was unremarkable.
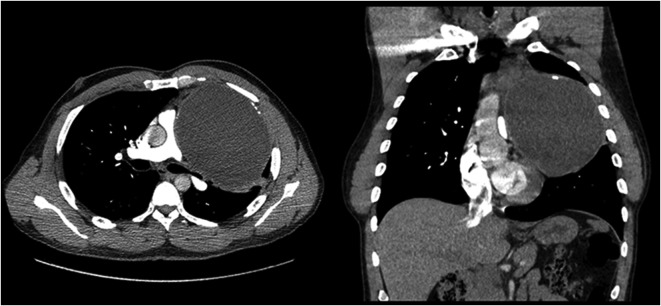
A CT scan of the chest (Fig. 1) revealed a 14 cm anterior mediastinal mass with both cystic and solid components, as well as compression of the pulmonary trunk, right main pulmonary artery and left main bronchus. Serum markers for alpha-fetoprotein and beta-human chorionic gonadotropin, to evaluate for germ cell tumor, were negative.
Figure 1:
Computed tomography of the mediastinal mass. Transverse cross sectional view. The cystic mass is compressing the pulmonary trunk and the left main bronchus.
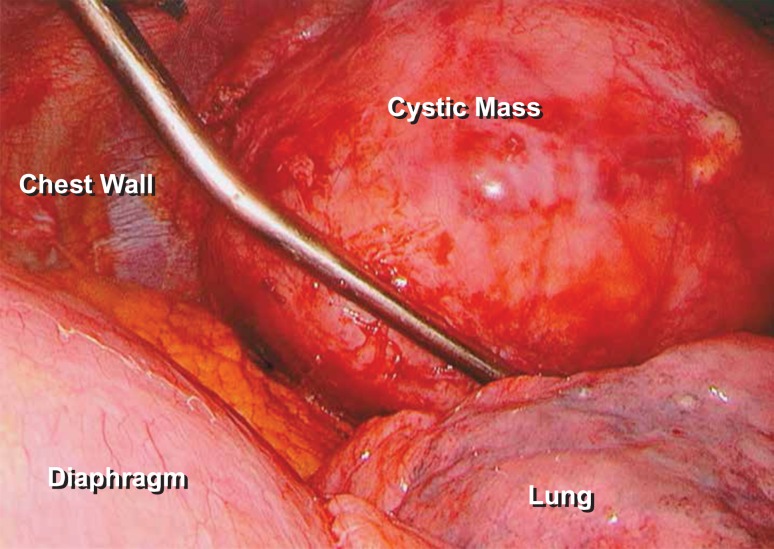
The patient underwent a VATS resection of the mass. To perform the procedure, the patient was placed in right lateral decubitus position. A 4 cm incision was made in the fourth intercostal space anteriorly. A chest tube site was opened in the seventh intercostal space at the mid-axillary line. The camera was placed through this site. The mass was adherent to the chest wall at the level of the apex, but did not invade any intrathoracic structures (Fig. 2). Once the mass was fully mobilized, it was placed in an impermeable bag. The mass was then opened, and the intracystic contents were evacuated. The fluid which was removed was purulent and thick. No intracystic contents spilled outside the bag. The residual mass was then easily removed in the bag through the utility incision. A small wedge resection was also performed to remove an area of bleb disease at the apex of the left lung which had been injured during the dissection.
Figure 2:
Thoracoscopic video-assisted photograph of the thymic cyst. Demonstrates mass abutting the left lung. The pericardial fat is inferior to the mass in this picture.
Postoperatively, the patient had a small but persistent air leak, likely secondary to his significant emphysematous lung disease. He was discharged with a chest tube and Heimlich valve on postoperative Day 7. His chest tube was eventually removed at his outpatient follow-up without difficulty.
Final pathologic review demonstrated a multiloculated thymic cyst (MTC) without signs of malignancy. The mass measured 14.7 cm in maximum diameter.
DISCUSSION
Thymic cysts account for 1–3% of anterior mediastinal masses. MTCs are usually acquired lesions and have been reported to be associated with an inflammatory process, in comparison to unilocular thymic cysts which have been described as congenital in nature and non-inflammatory. The lesions are thought to arise from cystic transformation of the medullary duct epithelium. The pathological findings in our patient’s mass supported a diagnosis of a MTC, with the colloidal exudate, thickened cyst walls and diffuse calcifications which were seen on histology.
There are three key components to ensure success during VATS for a mediastinal mass. Importantly, the utility incision should be made with the foresight of potential conversion by extending the incision into an anterolateral thoracotomy. Traditionally, a median sternotomy has been used for resection of very large mediastinal masses. A thoracoscopic approach, however, is now used as a first line approach by many surgeons and will have significantly less morbidity than a sternotomy. As thoracic surgeons have gained knowledge and improved upon techniques, there is now the ability to limit the number of additional ports for a VATS. However, one should be aware that outcomes have not been reported to differ based on the number of ports used, although pain scores may be improved [7].
The utility incision should be no greater than 4 cm. This incision length allows for use of multiple instruments easily and should not need to be extended. Large mediastinal masses can quite often be dissected off adjacent structures with minimal difficulty. However, if adequate exposure cannot be obtained then a conversion to an open approach may be necessary. From the senior surgeon’s experience, mass size alone should not be considered an absolute contraindication to a thoracoscopic approach.
When performing VATS resections of giant mediastinal masses, it is imperative for surgeons to be prepared and have a strategy for controlling bleeding. With giant mediastinal masses, the pulmonary artery and the innominate vessels are the most common vessels in close apposition to the mass. Before any very adherent areas are dissected, the proximal and distal aspects of the vessels should be dissected carefully so that vascular clamps can be placed in the case that a major injury occurs. Though we did not have any significant bleeding during our case, we did dissect the proximal pulmonary artery in the aortopulmonary window in case any large injury occurred [8–10].
We were able to limit our incision in this case because we knew from preoperative imaging that this mass was cystic in nature. We did not want to puncture the mass before it was in an impermeable bag, in case it was a cystic malignant mediastinal mass. But once it was safely in the bag, evacuation of the contents of the mass allowed for effortless removal of the mass. The mass should not be punctured prior to placing it within a bag, however, to prevent possible spread of infection and malignancy.
In conclusion, we present a 45-year-old gentleman with a giant thymic cyst removed using a one-port VATS approach. Complete resection of benign mediastinal masses is both diagnostic and curative. We advocate a minimally invasive approach to resection of mediastinal masses, even giant masses, when adequate visualization and exposure can be provided, minimizing postoperative morbidity.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding was provided.
REFERENCES
- 1. Jennings S, Stuklis R, Chan J, Kearney D. Successful giant thymic cyst removal: case report and review of the literature. Heart Lung Circ 2015;24:89–92. [DOI] [PubMed] [Google Scholar]
- 2. Izumi H, Nobukawa B, Takahashi K, Kumasaka T, Miyamoto H, Yamazaki A, et al. . Multilocular thymic cyst associated with follicular hyperplasia: clinicopathologic study of 4 resected cases. Hum Pathol 2005;36:841–4. [DOI] [PubMed] [Google Scholar]
- 3. Nanguzgambo A, Pike M, Page R, Benfield G, McKeon D. Spontaneous infection of a stable mediastinal cystic mass: A case report. Cases J 2008;1:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hess N, Sarkaria I, Pennathur A, Levy R, Christie N, Luketich J. Minimally invasive versus open thymectomy: a systematic review of surgical techniques, patient demographics, and perioperative outcomes. Ann Cardiothorac Surg 2016;5:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gossot D, Izquierdo R, Girard P, Stern JB, Magdeleinat P. Thoracoscopic resection of bulky intrathoracic benign lesions. Eur J Cardiothorac Surg 2007;32:848–51. [DOI] [PubMed] [Google Scholar]
- 6. Esmail H, Barry CE, Young DB, Wilkinson RJ. The ongoing challenge of latent tuberculosis. Philos Trans R Soc B Biol Sci 2014;369:20130437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Akter F, Routledge T, Toufektzian I, Attia R. In minor and major thoracic procedures is uniport superior to multiport video-assisted thoracoscopic surgery? Interact Cardiovasc Thorac Surg 2017;20:550–5. [DOI] [PubMed] [Google Scholar]
- 8. Hirji SA, Balderson SS, Berry MF, D’Amico TA. Troubleshooting thoracoscopic anterior mediastinal surgery: lessons learned from thoracoscopic lobectomy. Ann Cardiothorac Surg 2015;4:545–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kara HV, Balderson SS, D’Amico TA. Modified uniportal video-assisted thoracopsciopic surgery (VATS). Ann Cardiothorac Surg 2016;5:123–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shiono H, Inoue A, Tomiyama N, Shigemura N, Ideguchi K, Inoue M, et al. . Safer video-assisted thoracoscopic thymectomy after location of thymic veins with multidetector computed tomography. Surg Endosc 2006;20:1419–22. [DOI] [PubMed] [Google Scholar]