Abstract
Background
Influenza vaccination coverage in the United States remains below national targets and racial/ethnic differences persist.
Objectives
To gain insights into potential strategies for improving influenza vaccination by examining reasons given for not receiving an influenza vaccination during the 2011–12 influenza season.
Methods
Data from the National Flu Survey were analyzed for the 2011–12 influenza season.
Tests of association between reasons for non-vaccination and demographic variables were conducted using Wald chi-square tests. Multivariable logistic regression analyses were used to determine variables independently associated with each reason for non-vaccination.
Results
For adults and children, there were no racial/ethnic differences in the overall most frequent reason for non-vaccination: “unlikely to get very sick from the flu”. Regarding adults, there were racial/ethnic differences in seven of the twelve reasons for non-vaccination in bivariate analyses, but only three remained significant in the multivariable models. Most notable of these was that blacks (40.9%) were more likely than Hispanics (27.0%), whites (25.2%), and adults of other/multiple races (21.2%) to report concerns about getting the flu from the vaccination and blacks (39.8%) were more likely than whites (28.4%) and adults of other/multiple races (29.3%) to report concerns about side effects from the vaccine. Regarding children, there were racial/ethnic differences for three of the reasons for non-vaccination, and these remained significant in the multivariable models. The most noteworthy of these was that more black (44.4%) than white (24.0%) and other/multiple race (19.0%) parents had concerns about their child getting the flu from the vaccination. Other demographic variables (age, gender income, MSA for adults and age and income for children) were also associated with reasons for non-vaccination based on the multivariable models.
Conclusions
There are racial/ethnic group differences in reasons for not receiving an influenza vaccination; recognition of these differences should guide the choice of interventions to increase vaccination rates.
Keywords: Adult, Child, Influenza, Human, United States, Vaccination
1. Introduction
Since 2010, the Advisory Committee for Immunization Practices has recommended influenza vaccination for all people ≥6 months of age [1]. Yet, during the 2014–15 influenza season, only 43.6% of adults and 59.3% of children were vaccinated [2]. These rates remain below the national Healthy People 2020 target of 70% influenza vaccination coverage for adults and children [3]. Furthermore, racial/ethnic differences in influenza vaccination coverage have been persistent, with coverage being even lower for some racial/ethnic groups [4,5].
Many evidence-based strategies have been promoted for increasing influenza vaccination coverage, including but not limited to standing orders, provider reminders and recommendations, expanding access to vaccination services by reducing cost, and having vaccinations available at schools and pharmacies and other non-medical sites [6,7]. These strategies do not take into account specific patient attitudes; however, these strategies have been shown to work regardless of patient attitude [8]. Yet attitudes play a role in accepting vaccination as evidenced by a study of pregnant women which found the percentage vaccinated among women recommended and offered vaccine by their physician was 77.2% for those with a positive attitude about vaccine efficacy compared with 15.4% for those with a negative attitude; the percentages vaccinated were 79.2% for those with a positive and 26.1% for those with a negative attitude about vaccine safety [9]. An exploration of reasons for non-vaccination, by quantifying the most common reasons given for non-vaccination, could be useful to healthcare providers and immunization programs so that they are better prepared to address the concerns of patients. This could aid efforts to increase vaccination rates and decrease disparities in influenza vaccination. The objective of this study was to examine the reasons given for not receiving an influenza vaccination for adults and for children overall and by racial/ethnic group.
2. Methods
2.1. Survey description
Data from the National Flu Survey (NFS) were analyzed. The NFS was designed to provide rapid national estimates of influenza vaccination coverage and knowledge, attitudes, and practices during the influenza season and again at the end of the season. The NFS was sponsored by CDC and conducted by NORC at the University of Chicago in November 2010, March and November 2011, and lastly in March 2012 [10]. This study used data from the March 2012 NFS which included interviews conducted during March 1–29, 2012. The sample for the NFS was a list-assisted random digit-dial sample of both landline and cellular telephones. The interviews were conducted in English or Spanish with language line interpretation services used to conduct the survey in other languages as needed. Cellular telephone respondents were screened into the survey if they were a “cell telephone only” household (i.e., they reported that they do not maintain a landline telephone in their household) or a “cell telephone mainly” household (i.e., they maintain a landline but are unlikely to answer it if it rings while an adult is at home), and they were ≥18 years. For the landline sample, the youngest male ≥18 years currently at home was selected to be interviewed; if there were no males at home, the youngest female ≥18 years was selected [11]. For the cell telephone sample, the adult who answered the cell phone was selected to be interviewed. For interviews pertaining to children, the adult respondent was asked the ages of all children in the household younger than 18 years and one child was randomly selected. Then the interviewer stated that for the next section they needed to talk to the parent or guardian living in the household who knows about the health and health care of the selected child. If the respondent was the parent/guardian they continued with the survey; if they were not, the parent/guardian came to the phone or the interview was rescheduled for another time with the parent/guardian. Hereafter in this paper the parent/guardian is referred to as the parent.
The March 2012 survey questionnaire included questions about receipt of influenza vaccination, reasons for non-vaccination, and demographic questions. To assess influenza vaccination status, the respondents were asked: “Since July 1st, 2011, have you had a flu vaccination? It could have been a shot or a spray, drop, or mist in the nose.” For those responding that they were unvaccinated, the following questions were asked: “There are many reasons why people do not get flu vaccinations. I am going to read you a list of reasons why people may not get a flu vaccination. Please tell me if each is a reason why you did not get a flu vaccination this flu season. You did not get the flu vaccination this year because…” The list included the following with the respondent reporting if it was a reason of theirs after each was read: you are allergic to the vaccine; you don’t like needles and shots; you never get the flu; you are unlikely to get very sick from the flu; you did not have time to get the vaccination; you were not in a high risk or priority group; you were concerned about getting the flu from the vaccination; you were concerned about side effects from the vaccination other than getting the flu from the vaccine; you have an ongoing health condition that prevents you from getting the vaccination; you believe the flu vaccines do not work very well; you do not trust what the government says about the flu; the vaccine costs too much; you did not want the vaccination for some other reason. For reasons why the child did not receive a vaccination, the parent was asked the reasons for not having the child vaccinated in the same format as previously described. Information on the following demographic characteristics were included in this study: adult’s and child’s age, race/ethnicity, and sex, adult’s education, income/poverty level, and Metropolitan Statistical Area (MSA) category. The income/poverty level variable was defined based on total family income in the past calendar year, and the U.S. Census poverty thresholds for that year specified for the applicable family size and number of children <18 years.
The Council of American Survey Research Organizations (CASRO) response rate for the NFS was 31% for landlines and 18% for cell phones [12]. The CASRO response rate is the product of the percentage of telephone lines identified as residential or nonresidential (landline 76.2%, cell 49.0%), the percentage of known households with a completed screening interview (landline 96.6%, cell 72.6%), and the percentage of eligible respondents who complete the interview (landline 42.6%, cell 51.5%). A total of 15,630 households completed interviews (12,503 landline, 3127 cell); of these, 12,082 households had an interview regarding an adult only and 3548 households had an interview regarding both an adult and a child. Thus, there were completed interviews for 19,178 persons in the sample; of these, 19,017 had a non-missing influenza vaccination status (15,583 regarding adults, 3434 regarding children). Among the 15,583 interviews regarding adults, 45.5% received influenza vaccination in the 2011–12 season; the sample size of unvaccinated adults included in this study was 7398. Among the 3434 interviews regarding children, 55.5% of children were vaccinated; the sample size of unvaccinated children included was 1505. Of these 1505, there were 131 or 8.3%, in which the initial adult respondent was not the parent and the interview switched to the parent for the child questions. This left 1374 (91.7%) of the 1505 unvaccinated children in which the initial adult respondent was the parent of the child. Of these 1374 unvaccinated children, 316 had vaccinated parents leaving 1056 unvaccinated child/parent pairs for which to conduct a sub-analysis to examine agreement between reasons given for non-vaccination by parents for themselves versus their children.
2.2. Statistical methods
Tests of association between reasons for non-vaccination and demographic variables were conducted using Wald chi-square tests followed by post-hoc pair-wise comparison t-tests. Multivariable logistic regression analyses were used to determine variables independently associated with each reason for non-vaccination. Adjusted prevalence ratios (APR) based on predicted marginals from the logistic regression models were computed [13]. In the sub-analysis, agreement between reasons for non-vaccination given by parents for themselves versus for their children was evaluated using both the proportion of agreement and the unweighted kappa statistic, which adjusts for any agreement by chance [14]. Kappa values <0.40 show poor agreement, values between 0.40 and 0.75 show fair to good agreement, and values >0.75 show excellent agreement [14]. A two-sided significance level of 0.05 was adopted for all statistical tests. Reported percentages and corresponding 95% confidence intervals (95% CI) were weighted while sample sizes were unweighted. All analyses were weighted to population totals and to adjust for households having multiple telephone lines, unit non-response, and non-coverage of non-telephone households. Analyses were performed using SAS, release 9.3 (SAS Inc., Cary, NC, USA) and SUDAAN, release 11.0.0 (Research Triangle Institute, Research Triangle Park, NC, USA).
3. Results
Table 1 shows the sample characteristics of the unvaccinated adults included in this study with regard to age, race/ethnicity, sex, poverty status, education, and MSA. Approximately one-fifth of respondents (17.2%) had only one reason for non-vaccination, with many respondents choosing two to four reasons for non-vaccination (Table 1).
Table 1.
Sample characteristics of unvaccinated adults and children, 2011–12 influenza season, National Flu Survey*, United States.
| Demographic characteristic | Adults
|
Children
|
||
|---|---|---|---|---|
| n | % ± 95% CI† | n | % ± 95% CI | |
| Overall | 7398 | 1505 | ||
| Age group | – | – | – | – |
| ≤4 years | 3728 | – | 244 | 19.2 ± 3.4 |
| 5–12 years | 2279 | – | 616 | 42.4 ± 4.3 |
| 13–17 years | 1391 | – | 645 | 38.4 ± 4.1 |
| 18–49 years | 68.8 ± 1.7 | – | – | |
| 50–64 years | 22.0 ± 1.5 | – | – | |
| 65+ years | 9.2 ± 0.9 | – | – | |
| Race/ethnicity | – | – | – | – |
| Hispanic | 913 | 15.7 ± 1.7 | 248 | 17.2 ± 3.2 |
| Black only, non-Hispanic | 941 | 14.1 ± 1.6 | 198 | 13.3 ± 2.9 |
| White only, non-Hispanic | 4936 | 63.0 ± 2.1 | 886 | 63.1 ± 4.0 |
| Other or multiple race, non-Hispanic | 608 | 7.2 ± 1.1 | 173 | 6.4 ± 1.6 |
| Sex | – | – | – | – |
| Male | 3680 | 51.3 ± 2.1 | 764 | 49.8 ± 4.3 |
| Female | 3718 | 48.7 ± 2.1 | 741 | 50.2 ± 4.3 |
| Poverty status‡ | – | – | – | – |
| Above poverty, >$75,000/year | 2162 | 28.0 ± 1.9 | 643 | 37.9 ± 4.1 |
| Above poverty, ≤$75,000/year | 2064 | 29.6 ± 2.0 | 411 | 29.8 ± 4.1 |
| At or below poverty | 954 | 16.3 ± 1.7 | 191 | 15.7 ± 3.2 |
| Not reported | 2218 | 26.1 ± 1.8 | 260 | 16.6 ± 3.0 |
| Education | – | – | – | – |
| <12 years | 611 | 9.5 ± 1.3 | – | – |
| 12 years | 1331 | 21.4 ± 1.8 | – | – |
| Some college | 1878 | 29.2 ± 2.0 | – | – |
| College graduate | 2763 | 32.1 ± 1.9 | – | – |
| Not reported | 815 | 7.9 ± 1.0 | – | – |
| MSAa | – | – | – | – |
| MSA, principle city | 3280 | 39.6 ± 2.1 | 590 | 33.2 ± 3.8 |
| MSA, not principle city | 3116 | 43.8 ± 2.1 | 733 | 49.3 ± 4.3 |
| Non-MSA | 1002 | 16.6 ± 1.6 | 182 | 17.5 ± 3.5 |
| Number of reasons given | ||||
| 0 | 276 | 2.6 ± 0.6 | 88 | 5.7 ± 1.9 |
| 1 | 1323 | 17.2 ± 1.5 | 312 | 21.4 ± 3.5 |
| 2 | 1705 | 22.7 ± 1.7 | 302 | 19.5 ± 3.3 |
| 3 | 1561 | 23.0 ± 2.0 | 316 | 23.1 ± 3.6 |
| 4 | 1118 | 15.7 ± 1.5 | 216 | 12.6 ± 2.8 |
| 5 | 687 | 8.8 ± 1.2 | 113 | 7.5 ± 2.4 |
| 6 | 407 | 5.8 ± 1.0 | 94 | 5.1 ± 1.6 |
| 7 | 184 | 2.5 ± 0.7 | 35 | 3.4 ± 2.1 |
| 8–12 | 137 | 1.7 ± 0.5 | 29 | 1.8 ± 1.1 |
Sample includes interviews conducted March 1–29, 2012.
Weighted percentage and 95% Confidence Interval half-width.
The income/poverty level variable was defined based on total family income in the past calendar year, and the U.S. Census poverty thresholds for that year specified for the applicable family size and number of children <18 years. Poverty thresholds are available at http://www.census.gov/hhes/www/poverty/data/threshld/index.html.
MSA = Metropolitan statistical area.
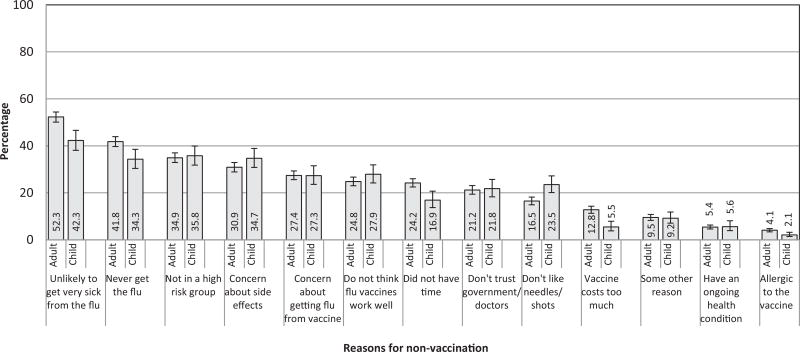
The overall percentages of unvaccinated adults indicating each reason for not receiving an influenza vaccination during the 2011–12 season are included in Fig. 1. The most common were: “unlikely to get very sick from the flu” (52.3%); “never get the flu” (41.8%); “not in a high risk or priority group” (34.9%); and “concerned about side effects from the vaccination other than getting the flu from the vaccine” (30.9%). Seven of the reasons for non-vaccination differed by racial/ethnic group based upon the bivariate analyses; two are highlighted here (Table 2). Blacks (40.9%) were more likely than Hispanics (27.0%), whites (25.2%), and other/multiple race adults (21.2%) to report concerns about getting the flu from the vaccination. Blacks (39.8%) were more likely than whites (28.4%) and other/multiple race adults (29.3%) to report concerns about side effects from the vaccine. Additional differences are noted in Table 2.
Fig. 1.
Percentage of unvaccinated adults reporting each reason for non-vaccination and parents reporting reasons for non-vaccination for their children, 2011–12 influenza season, National Flu Survey (based on interviews conducted March 1–29, 2012), United States.
Table 2.
Reasons for non-vaccination by race/ethnicity, adults and children, 2011–12 influenza season, National Flu Survey*, United States.
| Adults
|
Children
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hispanic | Black only, non-Hispanic |
White only, non-Hispanic |
Other or multi-race, non-Hispanic |
Hispanic | Black only, non-Hispanic |
White only, non-Hispanic |
Other or multi-race, non-Hispanic |
|||
| Overall, n (unweighted) | 1642 | 1765 | 11051 | 1125 | 644 | 446 | 1876 | 468 | ||
| Unvaccinated % (weighted) | 61.2 | 64.4 | 50.9 | 59.7 | 35.7 | 45.8 | 49.5 | 31.7 | ||
| Unvaccinated, n (unweighted) | 913 | 941 | 4936 | 608 | 248 | 198 | 886 | 173 | ||
| Adults
|
Children
|
|||||||||
| Hispanic | Black only, non-Hispanic | White only, non-Hispanic | Other or multi-race, non-Hispanic | Hispanic | Black only, non-Hispanic | White only, non-Hispanic | Other or multi-race, non-Hispanic | |||
| Reasons | % ± 95% CI† | % ± 95% CI | % ± 95% CI | % ± 95% CI | P‡ | % ± 95% CI | % ± 95% CI | % ± 95% CI | % ± 95% CI | P |
|
| ||||||||||
| Allergic to the vaccine | 2.4 ± 1.1bw | 5.3 ± 2.3h | 4.2 ± 0.8h | 4.3 ± 2.7 | 0.04 | 1.3 ± 1.1 | 3.5 ± 3.7 | 2.1 ± 1.1 | 2.0 ± 3.5 | 0.61 |
| Don’t like needles/shots | 23.1 ± 5.4wo | 19.5 ± 4.9 | 14.3 ± 1.9h | 15.3 ± 4.6h | 0.01 | 18.2 ± 6.8 | 18.6 ± 8.3 | 25.1 ± 4.8 | 31.7 ± 13.0 | 0.17 |
| Concerns about getting the flu from the vaccination | 27.0 ± 5.1b | 40.9 ± 6.3hwo | 25.2 ± 2.2b | 21.2 ± 5.7b | <0.001 | 29.7 ± 9.2 | 44.4 ± 11.7wo | 24.0 ± 5.0b | 19.0 ± 7.5b | 0.01 |
| Concerns about side effects from the vaccine | 33.6 ± 5.6 | 39.8 ± 6.3wo | 28.4 ± 2.3b | 29.3 ± 7.5b | 0.01 | 36.3 ± 9.4 | 43.4 ± 11.4 | 32.7 ± 5.2 | 32.5 ± 10.5 | 0.38 |
| Have an ongoing health condition | 5.7 ± 2.2 | 7.0 ± 2.6 | 4.9 ± 1.0 | 6.2 ± 3.2 | 0.41 | 16.9 ± 8.3wo | 7.3 ± 7.1 | 2.6 ± 1.6h | 1.1 ± 1.7h | <0.004 |
| Never get the flu | 41.3 ± 5.9 | 40.2 ± 6.3 | 42.6 ± 2.5 | 38.7 ± 7.1 | 0.75 | 38.1 ± 10.1 | 29.3 ± 9.7 | 35.1 ± 5.3 | 27.5 ± 10.9 | 0.40 |
| Unlikely to get very sick from the flu | 51.2 ± 5.9 | 49.9 ± 6.4 | 53.1 ± 2.5 | 51.7 ± 8.0 | 0.79 | 44.3 ± 10.2 | 32.9 ± 10.4 | 44.3 ± 5.6 | 36.0 ± 11.5 | 0.21 |
| Not in a high risk group | 27.9 ± 5.3wo | 27.7 ± 5.9wo | 37.4 ± 2.5hb | 42.2 ± 8.0hb | <0.001 | 33.8 ± 9.4 | 22.1 ± 7.9w | 39.4 ± 5.4b | 34.4 ± 11.8 | 0.02 |
| Think flu vaccines do not work very well | 23.2 ± 4.6 | 22.2 ± 5.1 | 25.5 ± 2.5 | 27.5 ± 7.6 | 0.47 | 29.5 ± 9.4 | 29.6 ± 10.4 | 26.6 ± 5.0 | 32.5 ± 11.0 | 0.77 |
| Don’t trust government/doctors | 25.5 ± 5.6 | 20.1 ± 5.4 | 21.1 ± 2.5 | 15.2 ± 5.1 | 0.07 | 22.7 ± 8.2 | 29.2 ± 11.6 | 20.5 ± 4.8 | 16.2 ± 8.5 | 0.37 |
| The vaccine costs too much | 18.4 ± 4.3w | 15.4 ± 5.0 | 10.2 ± 1.7ho | 18.1 ± 6.5w | <0.001 | 8.8 ± 5.4 | 2.6 ± 2.1 | 5.4 ± 2.8 | 3.2 ± 2.3 | 0.12 |
| Didn’t have time | 28.0 ± 5.0w | 22.0 ± 4.9o | 22.5 ± 2.0ho | 34.5 ± 8.0bw | 0.01 | 25.2 ± 10.4 | 17.7 ± 11.0 | 14.7 ± 3.9 | 14.7 ± 6.8 | 0.34 |
| Some other reason | 7.4 ± 2.7 | 10.2 ± 3.9 | 9.6 ± 1.6 | 11.5 ± 4.3 | 0.31 | 10.6 ± 6.2 | 4.4 ± 3.6 | 10.0 ± 3.2 | 7.3 ± 4.4 | 0.12 |
Based on interviews conducted March 1–29, 2012.
Weighted % and 95% Confidence Interval half-width.
The P-value is from the overall chi-square test of racial/ethnic group (4 categories) by reason given, yes versus no (2 categories).
The presence or absence of superscripted letters h, b, w, o (h = Hispanic, b = black, w = white, o = other/multiple race) denotes whether that estimate was statistically significantly different at P < 0.05 from another racial/ethnic group and denotes which group(s) it differed from based on the post-hoc pair-wise comparison t-tests. For example, the percentage of Hispanic adults giving the reason “allergic to the vaccine” (2.4%) was statistically significantly different from the percentage of black adults giving this reason (5.3%) and the percentage of white adults giving this reason (4.2%).
The overall percentage of unvaccinated children whose parents indicated reasons for not getting their child the influenza vaccine are included in Fig. 1. The most common were: “unlikely to get very sick from the flu” (42.3%); “not in a high risk or priority group” (35.8%); “concerned about side effects from the vaccination other than getting the flu from the vaccine” (34.7%); and “never get the flu” (34.3%). Among parents, more blacks (44.4%) than whites (24.0%) and parents of other/multiple race children (19.0%) had concerns about their child getting the flu from the vaccination (Table 2). More Hispanics (16.9%) than whites (2.6%) and parents of other/multiple race children (1.1%) reported the child having an ongoing health condition as the reason for non-vaccination. More whites (39.4%) than blacks (22.1%) reported their child not being in a high risk group as a reason for non-vaccination. There were no other statistically significant racial/ethnic differences other than those described above (Table 2).
Based on the twelve multivariable logistic regression models for adults, many of the demographic variables were associated with reasons for non-vaccination (Table 3). Adults in the younger age groups were less likely to give the reasons of “allergic to the vaccine”, “have an ongoing health condition”, “never get the flu”, or “don’t trust government/doctors” compared to adults 65 years and older. Conversely these younger age groups were more likely than adults 65 years and older to give the reason “unlikely to get very sick from the flu”, “not in a high risk group”, and “the vaccine costs too much”. Adult females were more likely than males to give the reasons “concerns about getting the flu from the vaccination”, “concerns about side effects from the vaccine”, and “have an ongoing health condition”, but were less likely than males to give the reasons “never get the flu” and “unlikely to get very sick from the flu”. Black adults were more likely than white adults to give the reasons “concerns about getting the flu from the vaccination” and “concerns about side effects from the vaccine”, while blacks and Hispanic adults were less likely than whites to give the reason “not in a high risk group”. Adults with lower income were more likely than those in the highest income group to give the reasons: “don’t like needles shots”, “concerns about getting the flu from the vaccine”, concerns about side effects from the vaccine”, “have an ongoing health condition”, “don’t’ trust government/doctors”, and “the vaccine costs too much”. They were less likely than those in the highest income group to give the reason “not in a high risk group”. Adults living in an MSA were more likely than those in non-MSA areas to give the reason “have an ongoing health condition”.
Table 3.
Demographics associated with reasons for non-vaccination, adults, 2011–12 influenza season, National Flu Survey*, United States.
| Reason for non-vaccination
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | Unvaccinated | Allergic to the vaccine |
Don’t like needles/ shots |
Concerns about getting the flu from the vaccination |
Concerns about side effects from the vaccine |
Have an ongoing health condition |
Never get the flu |
Unlikely to get very sick from the flu |
Not in a high risk group |
Think flu vaccines do not work very well |
Don’t trust government/ doctors |
The vaccine costs too much |
Didn’t have time |
| % | APR† | APR | APR | APR | APR | APR | APR | APR | APR | APR | APR | APR | |
| Age group: | |||||||||||||
| 18–49 years | 64.2 | 0.2 | 1.4 | 0.8 | 0.9 | 0.4 | 1.1 | 1.1 | 1.6 | 0.8 | 0.8 | 1.6 | 1.2 |
| 50–64 years | 49.0 | 0.5 | 1.3 | 0.9 | 0.9 | 1.0 | 0.8 | 0.9 | 1.2 | 0.8 | 1.0 | 1.7 | 1.1 |
| 65+years | 29.2 | Ref [12]b | Ref [12] | Ref [33] | Ref [33] | Ref [10] | Ref [42] | Ref [50] | Ref [24] | Ref [29] | Ref [25] | Ref [8] | Ref [21] |
| Gender: | |||||||||||||
| Male | 56.6 | Ref [4] | Ref [15] | Ref [25] | Ref [28] | Ref [4] | Ref [46] | Ref [58] | Ref [36] | Ref [24] | Ref [23] | Ref [12] | Ref [23] |
| Female | 52.4 | 1.3 | 1.1 | 1.2 | 1.2 | 1.4 | 0.8 | 0.8 | 1.0 | 1.1 | 0.9 | 1.2 | 1.1 |
| Race/ethnicity: | |||||||||||||
| Hispanic | 61.2 | 0.7 | 1.4 | 1.1 | 1.1 | 1.1 | 1.0 | 0.9 | 0.7 | 0.9 | 1.2 | 1.3 | 1.2 |
| Black, non-Hispanic | 64.4 | 1.2 | 1.2 | 1.6 | 1.3 | 1.1 | 1.0 | 0.9 | 0.8 | 0.8 | 0.9 | 1.1 | 1.0 |
| White, non-Hispanic | 50.9 | Ref [4] | Ref [15] | Ref [25] | Ref [29] | Ref [5] | Ref [42] | Ref [53] | Ref [37] | Ref [26] | Ref [21] | Ref [11] | Ref [23] |
| Other, non-Hispanic | 59.7 | 1.3 | 1.0 | 0.9 | 1.0 | 1.3 | 0.9 | 0.9 | 1.1 | 1.1 | 0.7 | 1.5 | 1.5 |
| Income‡: | |||||||||||||
| Above poverty, >$75000/year | 52.0 | Ref [4] | Ref [13] | Ref [22] | Ref [26] | Ref [3] | Ref [43] | Ref [51] | Ref [39] | Ref [21] | Ref [16] | Ref [5] | Ref [27] |
| Above poverty, ≤$75,000/year | 57.6 | 1.3 | 1.2 | 1.3 | 1.1 | 1.6 | 1.0 | 1.0 | 0.9 | 1.2 | 1.4 | 2.5 | 0.9 |
| At or below poverty | 60.2 | 1.4 | 1.5 | 1.4 | 1.4 | 2.6 | 0.8 | 1.0 | 0.7 | 1.3 | 1.8 | 6.0 | 0.9 |
| Not reported | 51.0 | 0.9 | 1.6 | 1.2 | 1.3 | 1.8 | 1.0 | 1.1 | 0.9 | 1.2 | 1.3 | 2.7 | 0.8 |
| MSAa | |||||||||||||
| MSA, principle city | 54.3 | 1.1 | 1.1 | 0.9 | 0.9 | 2.0 | 1.0 | 1.1 | 1.2 | 0.9 | 0.8 | 0.9 | 1.3 |
| MSA, not principle city | 54.5 | 1.1 | 0.9 | 0.9 | 0.9 | 2.4 | 1.0 | 1.0 | 1.2 | 1.0 | 0.8 | 1.1 | 1.2 |
| Non-MSA | 54.8 | Ref [4] | Ref [17] | Ref [30] | Ref [33] | Ref [3] | Ref [41] | Ref [52] | Ref [30] | Ref [25] | Ref [25] | Ref [13] | Ref [20] |
Based on interviews conducted March 1–29, 2012.
Adjusted prevalence ratio (APR); estimates in bold are statistically significantly different from the referent (P < 0.05); one logistic regression model was performed for each reason with all demographic variables listed in the table included in the model; the table shows results from 12 separate models.
The income/poverty level variable was defined based on total family income in the past calendar year, and the U.S. Census poverty thresholds for that year specified for the applicable family size and number of children <18 years. Poverty thresholds are available at http://www.census.gov/hhes/www/poverty/data/threshld/index.html.
MSA = Metropolitan statistical area.
The adjusted prevalence (%) for those in the referent group reporting the reason for non-vaccination is given in parentheses to aid the interpretation of the APRs.
Based on the twelve multivariable logistic regression models for parents of children, various demographic variables were associated with each reason for non-vaccination of children (Table 4). Compared to parents of children in younger age groups, parents of children in older age groups were less likely to give the reason “concern about side effects from the vaccine” and more likely to give the reasons of “never get the flu” and “unlikely to get very sick from the flu”. Compared to parents of white children, parents of Hispanic children were less likely to give the reason “don’t like needles/shots” while more likely to give the reason “have an ongoing health condition.” Parents of black children were more likely than those of white children to give the reason “concerns about getting the flu from the vaccination” but less likely to give the reasons “not in a high risk group”. Parents of children with lower income were more likely than those in the highest income group to give the reasons: “don’t like needles/shots”, “concerns about side effects from the vaccine”, “have an ongoing health condition”, and “the vaccine costs too much”. Sex and MSA were not associated with any of the reasons based on the multivariable models.
Table 4.
Demographics associated with reasons for non-vaccination, children, 2011–12 influenza season, National Flu Survey*, United States.
| Reason for non-vaccination
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographics | Unvaccinated | Allergic to the vaccine |
Don’t like needles/ shots |
Concerns about getting the flu from the vaccination |
Concerns about side effects from the vaccine |
Have an ongoing health condition |
Never get the flu |
Unlikely to get very sick from the flu |
Not in a high risk group |
Think flu vaccines do not work very well |
Don’t trust government/ doctors |
The vaccine costs too much |
Didn’t have time |
| % | APR† | APR | ARP | APR | APR | APR | APR | APR | APR | APR | APR | APR | |
| Age group: | |||||||||||||
| 6m- 4years | 33.4 | Ref [3]b | Ref [21] | Ref [33] | Ref [46] | Ref [3] | Ref [16] | Ref [27] | Ref [31] | Ref [35] | Ref [22] | Ref [2] | Ref [11] |
| 5–12 years | 42.3 | 0.7 | 1.3 | 0.8 | 0.8 | 1.9 | 2.2 | 1.6 | 1.0 | 0.8 | 1.0 | 3.8 | 1.6 |
| 13–17 years | 57.1 | 0.3 | 1.0 | 0.8 | 0.6 | 1.8 | 2.7 | 1.8 | 1.3 | 0.7 | 1.0 | 3.1 | 1.6 |
| Gender: | |||||||||||||
| Male | 44.1 | Ref [3] | Ref [25] | Ref [28] | Ref [37] | Ref [6] | Ref [33] | Ref [42] | Ref [37] | Ref [29] | Ref [24] | Ref [5] | Ref [16] |
| Female | 44.8 | 0.4 | 0.9 | 1.0 | 0.9 | 1.0 | 1.1 | 1.0 | 0.9 | 0.9 | 0.8 | 1.0 | 1.1 |
| Race/ethnicity: | |||||||||||||
| Hispanic | 35.7 | 0.7 | 0.6 | 1.1 | 1.0 | 3.9 | 1.0 | 1.0 | 0.9 | 1.1 | 1.0 | 1.3 | 1.7 |
| Black, non-Hispanic | 45.8 | 1.6 | 0.7 | 1.7 | 1.2 | 1.8 | 0.9 | 0.8 | 0.6 | 1.1 | 1.3 | 0.4 | 1.2 |
| White, non-Hispanic | 49.5 | Ref [2] | Ref [26] | Ref [25] | Ref [34] | Ref [3] | Ref [35] | Ref [44] | Ref [39] | Ref [27] | Ref [21] | Ref [6] | Ref [15] |
| Other, non-Hispanic | 31.7 | 0.9 | 1.2 | 0.8 | 1.0 | 0.4 | 0.8 | 0.8 | 0.9 | 1.2 | 0.8 | 0.6 | 1.0 |
| Income‡: | |||||||||||||
| Above poverty, >$75000/year | 43.6 | Ref [2] | Ref [19] | Ref [23] | Ref [27] | Ref [2] | Ref [36] | Ref [44] | Ref [39] | Ref [24] | Ref [16] | Ref [3] | Ref [17] |
| Above poverty, ≤$75,000/year | 49.0 | 1.0 | 1.1 | 1.4 | 1.3 | 3.0 | 0.9 | 1.0 | 0.8 | 1.3 | 1.7 | 2.3 | 1.0 |
| At or below poverty | 37.6 | 0.8 | 1.8 | 1.6 | 1.6 | 5.6 | 1.0 | 1.0 | 0.9 | 1.3 | 1.8 | 4.0 | 1.1 |
| Not reported | 46.9 | 1.6 | 1.5 | 0.9 | 1.5 | 1.2 | 0.8 | 0.9 | 1.0 | 1.3 | 1.3 | 1.4 | 1.1 |
| MSAa | |||||||||||||
| MSA, principle city | 39.9 | 1.2 | 1.1 | 0.9 | 1.1 | 1.8 | 1.0 | 1.0 | 1.3 | 0.8 | 0.9 | 0.6 | 1.0 |
| MSA, not principle city | 46.4 | 0.6 | 1.2 | 1.1 | 1.2 | 2.0 | 0.9 | 1.0 | 1.2 | 0.9 | 1.1 | 0.6 | 1.2 |
| Non-MSA | 49.4 | Ref [2] | Ref [21] | Ref [27] | Ref [30] | Ref [3] | Ref [37] | Ref [43] | Ref [29] | Ref [31] | Ref [22] | Ref [8] | Ref [16] |
Based on interviews conducted March 1–29, 2012.
Adjusted prevalence ratio (APR); estimates in bold are statistically significantly different from the referent (P < 0.05); one logistic regression model was performed for each reason with all demographic variables listed in the table included in the model; the table shows results from 12 separate models.
The income/poverty level variable was defined based on total family income in the past calendar year, and the U.S. Census poverty thresholds for that year specified for the applicable family size and number of children <18 years. Poverty thresholds are available at http://www.census.gov/hhes/www/poverty/data/threshld/index.html
MSA = Metropolitan statistical area.
The adjusted prevalence (%) for those in the referent group reporting the reason for non-vaccination is given in parentheses to aid the interpretation of the APRs.
In the analyses of the subset of unvaccinated parent-child pairs, the observed proportion of agreement between the reasons parents gave for not being vaccinated themselves and for not having their child vaccinated was >75% for ten of the twelve reasons (Table 5). When examining the kappa statistic however there was fair to good agreement for only half of the reasons.
Table 5.
Agreement in reasons for non-vaccination given by parents for themselves versus for their child, sub-analysis of unvaccinated adult/child pairs (n= 1056), 2011–12 influenza season, National Flu Survey*, United States.
| Parent + Child + |
Parent + Child − |
Parent– Child + |
Parent– Child − |
Agreement ++ or- − |
Kappa | |
|---|---|---|---|---|---|---|
| n | n | n | n | % | κ | |
| Reasons‡ | ||||||
| Allergic to the vaccine | 10 | 26 | 18 | 1002 | 96 | .19 |
| Don’t like needles/shots | 58 | 82 | 169 | 747 | 76 | .22 |
| Concerns about getting the flu from the vaccination | 229 | 107 | 85 | 635 | 82 | .59 |
| Concerns about side effects from the vaccine | 292 | 87 | 126 | 551 | 80 | .63 |
| Have an ongoing health condition | 6 | 26 | 48 | 976 | 93 | .01 |
| Never get the flu | 230 | 195 | 141 | 490 | 68 | .35 |
| Unlikely to get very sick from the flu | 336 | 200 | 133 | 387 | 68 | .33 |
| Not in a high risk group | 235 | 186 | 169 | 466 | 66 | .34 |
| Think flu vaccines do not work very well | 278 | 78 | 79 | 621 | 85 | .67 |
| Don’t trust government/doctors | 184 | 52 | 64 | 756 | 89 | .70 |
| The vaccine costs too much | 40 | 41 | 16 | 959 | 95 | .51 |
| Didn’t have time | 106 | 137 | 40 | 773 | 83 | .49 |
Based on interviews conducted March 1–29, 2012.
4. Discussion
This study found that the most common reasons given for not receiving an influenza vaccination during the 2011–12 influenza season were related to not perceiving themselves or their child at risk for influenza or not being at risk for getting very ill if they do get the disease. Concerns about side effects of the influenza vaccine were generally the next most common reasons given. Some previous studies examined reasons for non-vaccination but focused only on older adults and did not test for racial/ethnic group differences. In these studies the most common reasons were related to not perceiving themselves at risk for influenza and concerns about side effects of the influenza vaccine, similar to what our study found for all adults and parents [15–17]. Health professionals should take what opportunities they have available in their interactions with patients to provide objective information about the risks of influenza, the benefits of influenza vaccination, and address concerns that parents have. One resource includes the educational patient brochures, posters, and flyers available at http://www.cdc.gov/flu/freeresources/print-general.htm
This study found some similarities and differences between the racial/ethnic groups in reported reasons for not receiving an influenza vaccination. For example, there were no racial/ethnic differences in the overall most frequently given reason for non-vaccination: “unlikely to get very sick from the flu”. Among the more striking differences was that “concerns about getting the flu from the vaccination” was much more commonly reported as a reason for non-vaccination by black adults (41%) and by parents of black children (44%) compared to the other racial/ethnic groups (30% or less). This was the most frequently reported reason for non-vaccination given by parents of black children, while for all other racial/ethnic groups “unlikely to get very sick from the flu” was the most frequently given reason. This on-going misconception appears to be more prevalent in black communities than other communities and may be a contributing factor to the persistent racial/ethnic differences in influenza vaccination coverage. Research has shown that the mere presentation of facts and statistics in an attempt to persuade people to change their belief may cause them to become more entrenched in the belief [18]. Creative approaches will be needed to dispel this misconception among blacks, as well as among other racial/ethnic groups. Because of the finding that reasons for non-vaccination given by parents for themselves do not highly correspond to reasons they give for not having their child vaccinated, providers should not assume the reasons are the same when talking to parents about their vaccination concerns.
The study is subject to at least four limitations. First, vaccination status was based upon self or parent report and was not verified with medical records [19–21]. Second, the response rate was low however some survey methodologist report that response rates lack validity as a measure for survey bias [22]. Third, the accurate measure of reasons for non-vaccination is complicated because the reasons can vary over time for the same person and by the way the question is asked during a survey; the questions are asked at the time of the interview which is months after the decision was made. Fourth, the profile of reasons for non-vaccination for the 2011–12 season may not apply to the current or future seasons due to variability in the unique circumstances of each influenza season such as reports of early influenza deaths among children or a mismatch of the strains in the vaccine and the circulating virus.
In conclusion, the most common reasons for non-vaccination were related to not perceiving the risks of influenza and concerns about side effects of the influenza vaccine and there were racial/ethnic differences in reasons. Knowledge of these findings can guide the choice of interventions to decrease racial/ethnic differences in influenza vaccination rates. Healthcare providers, as well as immunization programs and their partners, should be made aware of the many reasons for non-vaccination and utilize strategies to help address these barriers.
Footnotes
The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of CDC.
References
- 1.CDC. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices - United States, 2013–14. MMWR Recomm Rep Sep. 2013;62(RR07):1–43. [PubMed] [Google Scholar]
- 2.CDC. [cited 07.04.16];FluVaxView: flu vaccination coverage. United States, 2014–15 influenza season. 2016 Jan 28; Available from: http://www.cdc.gov/flu/fluvaxview/coverage-estimates.htm.
- 3.U.S. Department of Health and Human Services. Healthy People 2020. [cited 26.07.13];Topics & objectives-immunization and infectious diseases. 2013 Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicid=23.
- 4.Lu PJ, O’Halloran A, Bryan L, Kennedy ED, Ding H, Graitcer SB, et al. Trends in racial/ethnic disparities in influenza vaccination coverage among adults during the 2007–08 through 2011–12 seasons. AmJ Infect Control. 2014;42:763–9. doi: 10.1016/j.ajic.2014.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Santibanez TA, Grohskopf LA, Zhai Y, Kahn KE. Complete influenza vaccination trends for children six to twenty-three months. Pediatrics. 2016;137(3):e20153280. doi: 10.1542/peds.2015-3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guide to Community Preventive Services. [cited 30.07.13];Increasing appropriate vaccination. 2013 Jul 20; Available from: www.thecommunityguide.org/vaccines/index.html.
- 7.CDC. [cited 09.03.15];FluVaxView: flu vaccination coverage, United States, 2013–14 influenza season. 2014 Sep 18; Available from: http://www.cdc.gov/flu/fluvaxview/coverage-1314estimates.htm.
- 8.CDC. Adult immunization: knowledge, attitudes, and practices - DeKalb and Fulton counties, Georgia, 1988. MMWR Morb Mortal Wkly Rep. 1988 Nov;37:657–61. (43) [PubMed] [Google Scholar]
- 9.Ding H, Black CL, Ball S, Donahue S, Izrael D, Williams WW, et al. Influenza vaccination coverage among pregnant women- United States, 2013–14 influenza season. MMWR. 2014 Nov;(37):816–21. (63) [PMC free article] [PubMed] [Google Scholar]
- 10.CDC. Flu vaccination coverage. [cited 12.06.15];National Flu Survey, March 2012. 2012 May 16; Available from: http://www.cdc.gov/flu/fluvaxview/nfs-survey-march2012.htm.
- 11.Gaziano C. Comparative analysis of within-household respondent selection techniques. Public Opin Q. 2005;69(1):124–57. [Google Scholar]
- 12.Frankel LR. The report of the CASRO Task Force on Response Rates. In: Wiseman F, editor. Improving data quality in sample surveys. Cambridge, MA: Marketing Science Institute; 1983. [Google Scholar]
- 13.Korn EL, Graubard BI. Analysis of health surveys. New York: John Wiley & Sons, Inc; 1999. Predictive marginals; pp. 126–40. [Google Scholar]
- 14.Fleiss JL. Statistical methods for rates and proportions. John Wiley & Sons, Inc; 1981. [Google Scholar]
- 15.Zimmerman RK, Santibanez TA, Janosky JE, Fine MJ, Raymund M, Wilson SA, et al. What affects influenza vaccination rates among older patients? An analysis from inner-city, suburban, rural, and veterans affairs practices. AmJ Med. 2003;114(1):31–8. doi: 10.1016/s0002-9343(02)01421-3. [DOI] [PubMed] [Google Scholar]
- 16.Singleton JA, Santibanez TA, Wortley PM. Influenza and pneumococcal vaccination of adults aged >65 racial/ethnic differences. Am J Prev Med. 2005 Dec;29:412–20. doi: 10.1016/j.amepre.2005.08.012. (5) [DOI] [PubMed] [Google Scholar]
- 17.Santibanez TA, Mootrey GT, Euler GL, Janssen AP. Behavior and beliefs about influenza vaccine among adults aged 50–64 years. Am J Health Behav. 2010;34(1):77–89. doi: 10.5993/ajhb.34.1.10. [DOI] [PubMed] [Google Scholar]
- 18.Nyhan B, Reifler J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine. 2015;33:459–64. doi: 10.1016/j.vaccine.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 19.Brown C, Clayton-Boswell H, Chaves SS, Prill MM, Iwane MK, Szilagyi PG, et al. Validity of parental report of influenza vaccination in young children seeking medical care. Vaccine. 2011;29:9488–92. doi: 10.1016/j.vaccine.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 20.Donald RM, Baken L, Nelson A, Nichol KL. Validation of self-report of influenza and pneumococcal vaccination status in elderly outpatients. Am J Prev Med. 1999;16(3):173–7. doi: 10.1016/s0749-3797(98)00159-7. [DOI] [PubMed] [Google Scholar]
- 21.Mangtani P, Shah A, Roberts JA. Validation of influenza and pneumococcal vaccine status in adults based on self-report. Epidemiol Infect. 2007;135(1):139–43. doi: 10.1017/S0950268806006479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davern M. Nonresponse rates are a problematic indicator of nonresponse bias in survey research. Health Serv Res. 2013;48(3):905–12. doi: 10.1111/1475-6773.12070. [DOI] [PMC free article] [PubMed] [Google Scholar]