Abstract
A 16-year-old girl presented with intermittent left chest pain and breathlessness on exertion for last 4 months with one episode of haemoptysis. There has been loss of appetite and weight loss of 4 kg over a period of 1 month. A chest radiograph revealed a large mass like opacity with pleural effusion in the left lung field. Computerized Tomography scanning (CT scanning) and Positron Emission Tomography/Computerized Tomography scanning (PET/CT scanning) demonstrated a 7 cm round, cystic lesion in the anterior mediastinum. Pleural fluid cytology did not show any malignant cell. The patient was referred to cardiothoracic department for thoracotomy and resection. Surgery was uncomplicated with rapid recovery. Histologic findings suggested mature teratoma components surrounded by oedematous pleura and pericardium with adjacent thymus and lung tissue.
1. Background
Approximately 10% to 12% of primary mediastinal masses are derived from germinal tissue. Mature teratomas are rare and slow growing tumor. Next to sacrococcygeal area in children and the gonads in adults, mediastinum is the most common site for these tumors. Although teratomas are the most common germ cell tumors found in the mediastinum, they form only 8% of all tumors in this area.
There are a number of pathologies to consider when evaluating an anterior mediastinal mass. We present this interesting case as an opportunity to review the differential diagnosis and to discuss in brief the aetiology, presentation, investigation and management of this disease.
2. Case presentation
A 16-year-old non-smoker Caucasian girl presented in Emergency department with intermittent chest pain on left side and left shoulder, breathlessness on exertion for last 4 months and one episode of haemoptysis. There has been loss of appetite and weight loss of 4 kg over a period of 1 month but she denied night sweats and fatigue as well as fever and cough. She was a known case of Asthma, had allergies for grass and dust. As medication, she received Montelukast and oral contraceptive pills. A clinical examination was unremarkable except for decreased breathing sound on lower part of left chest.
3. Investigations
A chest X-Ray showed infiltrative changes on left lower lung and pleural effusion (Fig. 1). Blood testing revealed a C-reactive protein of 30 mg/l, TLC 12.4 and increased D-Dimer 3.22 mg/l. Thoracentesis was performed and pleural fluid cytology did not show any malignant cell. The patient was referred to our Respiratory Department for further evaluation.
Fig. 1.
A chest X-Ray showed infiltrative changes on left lower lung and pleural effusion with suspicion for tumor.
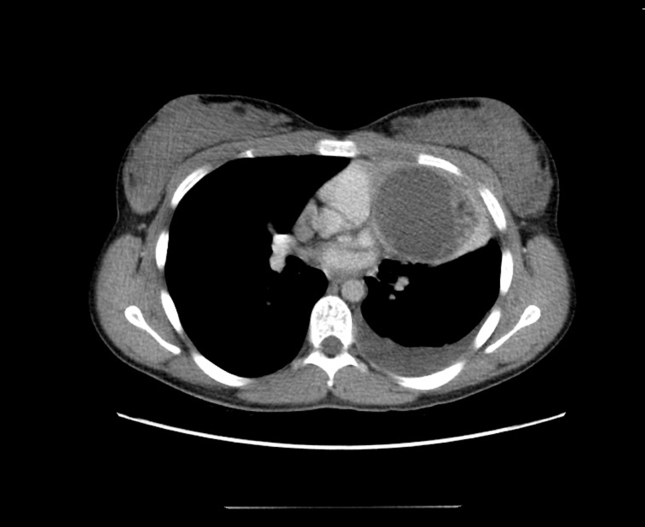
A CT scan of chest and abdomen was arranged. It revealed a 7 cm round, cystic lesion consisting of fat tissue and calcification in the anterior mediastinum, pleural effusion and atelactatic changes in left lung and an enlarged lymph node close to arcus aorta (Fig. 2).
Fig. 2.
A CT scan of chest and abdomen revealing a 7 cm round, cystic lesion consisting of fat tissue and calcification in the anterior mediastinum, pleural effusion and atelactatic changes in left lung, an enlarged lymph node of 1.0 cm close to arcus aorta.
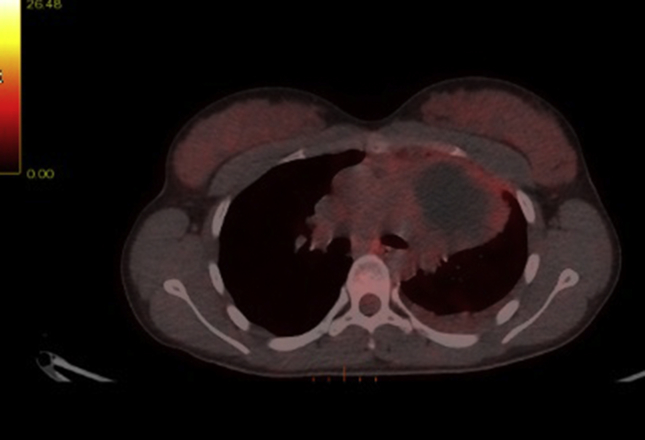
A 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) scanning showed increased FDG uptake in the lateral/caudal area of the cyst with more focal changes in the basal. There was pleural effusion with slightly increased FDG uptake, as well as moderate FDG uptake in an enlarged lymph node in the mediastinum station 6 and slightly FDG uptake in the small lymph node station 1L (Fig. 3).
Fig. 3.
A PET/CT scanning showing a cystic process in the anterior mediastinum left side, with increased FDG uptake.
The further work-up procedure was discussed in Multi-disciplinary team (MDT conference) and the patient was accepted for thoracotomy.
4. Differential diagnosis
Anterior mediastinal tumor has numerous diseases as differential diagnoses:
-
-
Thymoma, thymic carcinoma, thymic cyst, thymic hyperplasia
-
-
Thyroid and parathyroid neoplasms
-
-
Lymphoma (Hodgkin, non-Hodgkin)
-
-
Germ cell tumors (mediastinal teratoma, malignant teratoma, mediastinal seminoma, mediastinal embryonal cell carcinoma, mediastinal choriocarcinoma, mediastinal mixed cell type germ cell tumor)
-
-
Thoracic aortenaneurysm
5. Treatment
The patient underwent left anterior thoracotomy with resection of the tumor mass.
6. Outcome and follow-up
The tumor was mature teratoma with elements of skin with mild keratinization and related sebaceous glands and hair follicles. There is an area of adipose tissue. Many surfaces were lined by columnar epithium, as in the areas of gastrointestine with goblet cells but the dominant component is airway epithelium with cilia. In addition to these surfaces there was underlying large tissues areas of seromucinous glands. Macroscopically teratoma surrounded by connective tissue capsule, consists of adjacent lung tissue surrounded by oedematous pleura and oedematous pericardium. Outside the cyst, thymic remnants and fragment of normal lung tissue were identified. Histopathological conclusion was mature teratoma components surrounded by oedematous pleura and pericardium with adjacent thymus and lung tissue.
Patient was discharged and will be follow-up in Oncology department with control CT scanning of thorax in 6 months and 1 year.
7. Discussion
Approximately 15% of primary mediastinal masses are derived from germinal tissue in adults and up to 24% in children [1]. Sporadic cases have been described [[2], [3], [4], [5], [6]]. Most of them present in anterior mediastinum, only up to 8% -in posterior mediastinum [2].
These neoplasms are classified into four main groups: teratoma and teratocarcinoma, seminoma, embryonal cell carcinoma, and choriocarcinoma. They are believed to arise from remnant multipotent germ cells that have migrated abnormally during embryonic development. Next to sacrococcygeal area in children and the gonads in adults, mediastinum is the most common site for these tumors.
Teratoma are the most common germ cell tumors. By definition, they are made up of tissues of foreign to the area in which they occur. Ectodermal derivatives predominate, but structure originating in all three primary germ cell layers may be found. When only the epidermis and its derivatives are present, the term dermoid cyst is appropriate. Teratoma occur most often in young adults but have been reported in all age groups, and men and women are affected with equal frequency. Most (80%) are benign, teratocarcinoma, the malignant counterpart, is an aggressive, rapidly spreading neoplasm with a poor prognosis.
Most patient with teratoma have symptoms caused by the tumor, only about a third are asymptomatic. Usual symptoms are pain, cough and dyspnoea. If the tumor erodes into a bronchus, haemoptysis or even the expectoration of differentiated tissue such as hair(trichoptysis) or sebaceous material may occur. Teratoma may also rupture into the pleural space and produce acute respiratory distress or enter the pericardium, causing pericardial tamponade.
On chest radiograph, teratoma are generally smooth, rounded and well circumscribed if they are cystic and more lobulated and asymmetrical if they are solid. Soft tissue, fat and calcification (occasionally fully formed teeth and bone) can be identified on CT images, rendering this one of few mediastinal tumors that can be diagnosed confidently before operation. On PET/CT scanning teratoma (mostly benign 80%) does not uptake FDG radioactive. CT scanning and PET/CT scanning remain the radiographic modality of choices for evaluate the true extent of a mature mediastinal teratoma. It provides a three dimensional picture, helping to identify the involvement of surrounding structure and to assess the suitability for surgical resection. All teratomas should be resected because of the uncertainty as to whether they are benign and the possibility of further enlargement with impingement on adjacent structure. In malignant teratoma, adjuvant combination chemotherapy may result in improved survival.
8. Learning point
-
#
Mature teratoma is a rare and slow growing tumor, but should be considered for differential diagnosis for any mediastinal mass, particularly with anterior mediastinal lesions.
-
#
Differential diagnosis for anterior mediastinal mass included: thymona, lymphoma, carcinoma and thyroid disease.
-
#
CT or PET/CT scanning allows to identify the tumor and assessment for involvement of surrounding structure.
-
#
Complete surgical resection is recommended for all mature teratoma for histopathological diagnosis with favourable survival rates.
Competing interests
None.
Patient consent
Obtained.
References
- 1.Mulen B., Richardson J.D. Primary anterior mediastinal tumors in children and adults. Ann. Thorac. Surg. 1986;42:338. doi: 10.1016/s0003-4975(10)62751-8. [DOI] [PubMed] [Google Scholar]
- 2.Jaiswal R. Asymptomatic posterior mediatinal teratoma diagnosed incidentally. BMJ Case Rep. 2014 doi: 10.1136/bcr-2013-203228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray J. Mature teratoma of thymus. BMJ Case Rep. 2013 doi: 10.1136/bcr-2013-010127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sawant A.C. Intrapulmonary cystic teratoma mimicking malignant pulmonary neoplasm. BMJ Case Rep. 2012 doi: 10.1136/bcr.02.2012.5770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pattnaik M.K. A rare presentation of huge mature mediastinal teratoma with right lung cavitation. BMJ Case Rep. 2014 doi: 10.1136/bcr-2014-203835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paradies G., Zullino F. Mediastinal teratomas in children, case reports and review of literature. Ann. Ital. Chir. 2013;27:84. [PubMed] [Google Scholar]