Abstract
Cardiovascular disease remains the number one cause of mortality in the United States. There are numerous approaches to treating these diseases, but regardless of the approach, an in vivo model is needed to test each treatment. The pig is one of the most used large animal models for cardiovascular disease. Its heart is very similar in anatomy and function to that of a human. The ameroid placement technique creates an ischemic area of the heart, which has many useful applications in studying myocardial infarction. This model has been used for surgical research, pharmaceutical studies, imaging techniques, and cell therapies.
There are several ways of inducing an ischemic area in the heart. Each has its advantages and disadvantages, but the placement of an ameroid constrictor remains the most widely used technique. The main advantages to using the ameroid are its prevalence in existing research, its availability in various sizes to accommodate the anatomy and size of the vessel to be constricted, the surgery is a relatively simple procedure, and the post-operative monitoring is minimal, since there are no external devices to maintain. This paper provides a detailed overview of the proper technique for the placement of the ameroid constrictor.
Keywords: Medicine, Issue 128, Ameroid, ischemia, cardiac, angiogenesis, swine, coronary
Introduction
Coronary artery disease (CAD), which leads to myocardial ischemia, is the leading cause of disability, death, and health care costs around the world4 and attributable for approximately 1 out of every 3 deaths in the U.S.1,2,3,4,5,6. Although there have been many advances in both percutaneous and surgical treatments, as many as one third of patients suffering from CAD are ineligible for these treatments due to age, poor health, or suboptimal anatomy4,5,6,7. In order to evaluate new methods of diagnostic imaging or treatment, the development of an appropriate animal model is critical.
When developing an animal model for a disease, the induced disorder should closely emulate the anatomical and physiological characteristics of the disorder in humans8,9. One of the most widely used large animals for cardiovascular studies is the pig. The pig heart is most closely analogous to the human heart in terms of size, anatomy, and physiology3,6. Similar to the human heart, the myocardium of the pig's heart does not possess an extensive collateral circulation6. Because of this, the pig heart does not tolerate acute coronary occlusion well, but it can tolerate a gradual coronary occlusion. If a coronary artery is slowly occluded, it can be used as a model for chronic myocardial ischemia, chronic myocardial infarction, and heart failure5,6,9,10,11,12,13. Chronic myocardial ischemia can be induced through stent implantation or the placement of a hydraulic occluder, a fixed stenosis occluder, or an ameroid constrictor. There are advantages and disadvantages for all these methods which are outlined in detail in various publications6,9,13 but the most commonly used method is the ameroid placement5,6,10,11.
The ameroid constrictor consists of casein material encased within a stainless steel, plastic, or titanium ring. Once placed around an artery (usually the left anterior descending coronary artery (LAD) or the left circumflex coronary artery (LCX)), the casein material absorbs the surrounding fluid causing the inner lumen to narrow gradually, mimicking the slow stenosis of an artery and resulting finally in full occlusion9,13,14. This procedure used by itself or in conjunction with other methods results in a region of chronic myocardial ischemia and/or infarction of the left ventricle of the heart that has been useful for developing and evaluating new imaging techniques8,10,15, therapeutic treatments7,16,17,18 and surgical procedures19,20.
Protocol
The procedures described here were approved by the National Heart, Lung, and Blood Institute Animal Care and Use Committee at the National Institutes of Health and conform to the policies outlined in The Public Health Service Policy on Humane Care and Use of Laboratory Animals, The Animal Welfare Act, and the Guide for the Care and Use of Laboratory Animals.
NOTE: The purpose of this surgical procedure is to produce an animal model of chronic myocardial ischemia that can be used to develop treatments that are clinically relevant for patients with severe CAD. This cannot be accomplished using an in vitro model.
1. Animals
Use male Yorkshire swine weighing between 12 and 15 kg.
2. Pre-surgical Procedures
For a prophylactic antibiotic, use amoxicillin and clavulanate potassium (15 mg/kg) orally twice a day beginning 24 h prior to surgery. NOTE: This oral antibiotic is started before surgery to make sure that the pig will swallow it and to also make sure that they will not have an allergic reaction to the medication post-operatively.
Withhold food and water from the pig 12 h prior to surgery.
On the day of surgery, anesthetize the pig with a cocktail of ketamine (33 mg/kg), midazolam (0.5 - 0.75 mg/kg), and glycopyrrolate (0.01 mg/kg) given intramuscular (IM).
Place a 20 G intravenous (IV) catheter in an ear vein and intubate the animal with a 7.0 Fr endotracheal tube. NOTE: Adjust the size of the IV catheter and the endotracheal tube as appropriate for the size of the pig.
Remove the hair (shave) on the left side of the pig from the shoulder to the umbilicus and from the abdominal midline to the vertebral column.
Administer the prophylactic antibiotics (piperacillin and tazobactam: 100 mg/kg IV) and pain medication (buprenorphine sustained release: 0.2 mg/kg subcutaneous (SC) or a fentanyl transdermal patch 25-50 µg/h). NOTE: The IV antibiotic is given because the animals are fasted for 12 h prior to surgery and do not receive the previously mentioned oral antibiotic during this time.
Transport the pig to the operating room and connect the endotracheal tube to the anesthesia machine equipped with a sidestream sensor to monitor the airway gases. Mechanically ventilate the pig using a tidal volume of 10 mL/kg as a starting point and do not exceed an airway pressure of 30 cm H2O. Set the respiratory rate between 10-20 breaths per min (bpm) and adjust as needed to keep the end-tidal CO2 (PetCO2) levels between 28 and 35 mm Hg. Maintain the anesthesia with either isoflurane (1-3%) or sevoflurane (2-5%).
Position the pig right-side down on the operating table. Attach all necessary probes to monitor body temperature (BT), electrocardiogram (ECG), pulse oximetry (SpO2), etc.
Prepare the surgical site via three alternating scrubs with 2% chlorohexidine and 70% alcohol (apply in a circular motion beginning with center and moving outward).
Drape the surgical site using aseptic technique21.
3. Surgical Procedure
- Expose the heart through a left thoracotomy.
- Make a skin incision parallel to the 4th and 5th intercostal space about 8 - 9 cm in length using a no. 10 scalpel blade.
- Cut through the latissimus dorsi and serratus ventralis muscles using a pair of curved Metzenbaum scissors and Brown Adson forceps. Use electrocautery to maintain hemostasis as necessary.
- Enter the pleural cavity through the intercostal muscles between the 4th and 5th ribs with the Metzenbaum scissors cutting along the anterior aspect of the 4th rib. To reduce the chance of accidentally damaging the lung, turn the ventilator off on the exhale just prior to entering the pleural cavity. Once the pleural cavity has been breached, turn the ventilator back on.
- Use a small Finochietto retractor to spread the ribs apart, exposing the heart.
Use Debakey forceps to grasp and lift the pericardium. Use Potts scissors to make a small hole in the pericardium, allowing air to enter the pericardial space. Continue the incision with the Potts scissors over the junction of the LAD and LCX arteries.
Use Babcock forceps to retract the left atrial appendage. Using Debakey and small right angle forceps, dissect the LCX artery from the surrounding tissue prior to or proximal to the 1st obtuse marginal branch.
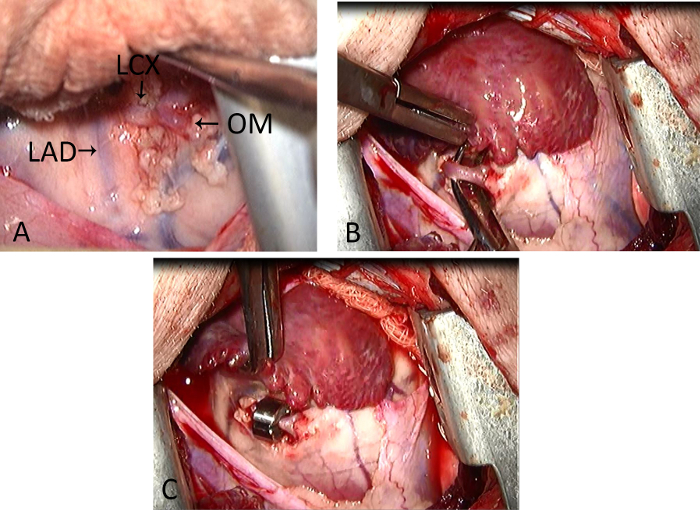
Place two vessel loops under the dissected LCX artery, one at each end. Hold a size 3.0 mm ameroid constrictor with the small right angle forceps and lift the vessel loops to gently guide the LCX artery through the opening of the constrictor. Gently rotate the constrictor so the opening is facing up. Remove the vessel loops. See Figure 1. NOTE: Adequate dissection of the artery is essential to prevent kinking. Select the appropriate sized constrictor for the individual animal. The appropriate sized constrictor will closely encircle the vessel without initially constricting the vessel. Domestic pigs weighing between 12 and 15 kg require ameroid constrictors sized 2.5 - 3.5 mm. The location of the ameroid constrictor on the vessel depends on the desired size of the ischemic area.
Re-approximate the pericardium and close with 4-0 polypropylene sutures.
Reestablish the negative thoracic pressure by inserting a 12 Fr chest tube or equivalent in the pleural space with the end exiting out between the layers of closure, generally two intercostal spaces posterior to thoracotomy site. NOTE: Observe the lung for atelectasis before closing the ribs. If any signs of underinflation are observed, re-inflate the lungs manually up to a pressure of 30 mm Hg.
Close the chest using 1 polypropylene sutures for the intercostal layer, 0 polypropylene sutures for the serratus and fascial layer, 2-0 polypropylene sutures for the subcutaneous layer, and 3-0 polypropylene sutures for the subcuticular layer. Staple or suture the skin.
Attach a three-way stop cock to the end of the chest tube and evacuate the air in the chest with a 40-60 cc syringe until a negative seal is achieved. Roll the animal onto its sternum or opposite side to facilitate removing all the air. Once the chest maintains negative pressure, remove the chest tube and suture the exit site. If animals are housed singly post-operatively, the incision can be bandaged for several days.
4. Post-operative
Following closure, infiltrate the incision along both sides of the thoracotomy site with 0.25% bupivacaine.
Wean the animal off the ventilator and turn off the anesthesia. Remove the endotracheal tube once the animal is breathing on its own and swallowing.
Monitor the animal until it is fully recovered (awake and sternal). There should be no abnormalities or arrhythmias on the ECG, the BT should be 38.7 - 39.8 °C, the SpO2 should be 95 - 100%, and the respiratory rate should be 32 - 58 bpm.
Administer amiodarone (100 mg, orally twice a day) and clopidogrel bisulfate (75 mg, orally once a day) to prevent thrombosis and arrhythmias. Continue with amoxicillin and clavulanate potassium (15 mg/kg) orally twice a day for 10 days post-operation. Post-operative pain is controlled with buprenorphine SR (sustained release) 0.2 mg/kg. SQ every three days. The buprenorphine SR may be supplemented with carprofen (4.4 mg/kg) once and then (2.2 mg/kg) PO or IM BID.
Keep all bedding and foraging material out of the animal's housing area until the incision is fully healed.
Representative Results
After analyzing the data obtained from ameroid placement surgeries performed in our facility over a two-year period, we found the survival rate to be 80%. The procedure was performed on 25 Yorkshire pigs weighing between 12 - 15 kg. Of the 25 pigs, 20 survived to the follow-up procedure, 2 fibrillated and died shortly after closing, 2 were euthanized for severe heart failure and pulmonary edema, and 1 had an anesthetic death during a follow-up radiograph. Necropsy revealed an infarcted area of the left ventricle in the animals that died within 24 hours of the procedure. It is suspected but could not be confirmed that the artery kinked due to the presence of the ameroid since the lumen of the ameroid was still open. The ameroids obtained from the animals that were euthanized due to heart failure were examined. There was total closure of the lumen at 18 days.
The surviving animals were imaged by Magnetic Resonance Imaging (MRI) at 28 days post-ameroid placement to measure the heart function and size of the ischemic area. Figure 2 and Figure 3 show the MRI images obtained from a pig with a titanium encased ameroid and a pig with a plastic encased ameroid, respectively. After imaging, a second thoracotomy was performed for either a cell injection or sham procedure. Animals were followed out as long as 16 weeks post-ameroid placement.
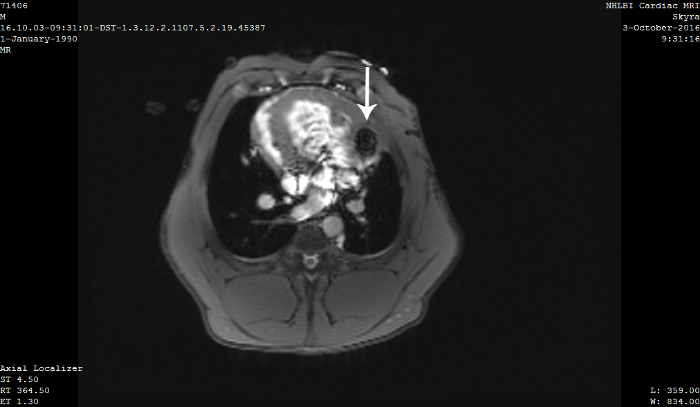

Figure 1: Images of the pig heart during the ameroid placement procedure. (A) Image of the pig heart showing the LAD, LCX, and obtuse marginal artery (OM). (B) Image of the dissected LCX artery before the ameroid placement. (C) Image of the proper placement of the ameroid around the LCX with the opening of the ameroid facing up or away from the heart. Please click here to view a larger version of this figure.
Figure 2: MRI image of pig heart with a titanium encased ameroid. MRI image of a pig heart taken four weeks after the placement of a titanium encased ameroid constrictor on the LCX artery. The arrow points to the artifact created by the titanium. Please click here to view a larger version of this figure.
Figure 3: MRI image of a pig heart with a plastic encased ameroid. MRI image of a pig heart taken four weeks after the placement of a plastic encased ameroid constrictor on the LCX artery. The arrow points to the ameroid constrictor. No artifact is observed. Please click here to view a larger version of this figure.
Discussion
Ameroid constrictors have been used extensively to create animal models of chronic myocardial ischemia, chronic myocardial infarction, and heart failure5,6,7,9,10,11,12,13,15,16,17,18,19,22. Although these models can be created through the use of stents, hydraulic occluders, or fixed stenosis occluders, the prevalence of ameroid use in scientific literature allows researchers to more accurately compare the results of their work with previously published studies5,6,7,9,10,11,12,13,15,16,17,18,19,22. Another advantage of using the ameroid constrictor is that the procedure is relatively straightforward and can be performed successfully by anyone with reasonable surgical skills, and requires no specialized instruments. The other aforementioned methods require greater technical skills and, in the case of the hydraulic occluder, requires intense post-operative monitoring due to the externalized device6,13.
The main limitation of using the ameroid constrictor is the variability in the rate of occlusion9,13. In general, most studies using the ameroid constrictor have found the rate of stenosis to be highest in the first two weeks and then gradually taper off until complete occlusion occurs23,24. Ex vivo studies directly measuring the closure rate of the ameroid lumen have confirmed that the greatest reduction in lumen diameter occurs in the first two weeks and slows thereafter25,26. However, these same studies have also showed that surrounding glucose and protein concentrations can affect the rate and completeness of the ameroid closure, thereby suggesting that in vivo conditions are most likely responsible for the variability in ameroid occlusion rates25,26. Other investigators have suggested that mechanical trauma, inflammation, fibrosis, and thrombus formation caused by the ameroid placement procedure itself may contribute to this variability5,6,25. The latter scenario is most likely the reason for the premature deaths and heart failures observed in this study. It cannot be stressed enough the importance of doing delicate, yet adequate, artery dissection on either side of the ameroid to prevent kinking of the vessel.
Proper placement of the ameroid constrictor is critical to develop an ischemic area of the heart that is large enough to treat but not so large that it results in death. Placing the ameroid constrictor on the LCX before the first obtuse marginal branch appears to work best in Yorkshire pigs. As reported elsewhere, this resulted in an ischemic area of around 25-30% of the left ventricle6. Placing the ameroid any lower resulted in an ischemic area that was inadequate for the specific treatment that was being investigated in this study.
Arrhythmias occurring during the surgical procedure are rare. Administering oral amiodarone post-operation through the end of the study, may prevent arrhythmias during the 2 to 3 weeks post-operation, when the ameroid is closing off. Additionally, caretaking and medical staff should be especially vigilant in noting any coughing during this time, which could be an early sign of pulmonary edema/heart failure.
Over the years, the design of the ameroid constrictor has been improved upon. Ameroids are currently available in numerous sizes allowing the surgeon to select an ameroid that matches the diameter of the vessel to be occluded. The outer ring of the ameroid is available in stainless steel, titanium, or plastic. This is especially important when evaluating the affected hearts using MRI. All metal will cause an artifact on the MRI images. Titanium ameroids cause less of an artifact than stainless steel, while plastic leaves none at all. MRI images showing the difference between a titanium ameroid and a plastic ameroid are shown in Figure 2 and Figure 3, respectively. The artifact on the right side of the heart in Figure 2 is caused by the titanium ring encasing the ameroid. Until recently, the containment ring on the plastic ameroid was too bulky to place around a coronary artery without kinking the vessel. The ameroid constrictor used in this study (see Table of Materials) is a much more streamlined version, which has the same outer diameter as the metal ameroids.
Disclosures
The authors have no conflict of interest to disclose.
Acknowledgments
Intramural funding was provided for this project by the Division of Intramural Research, National Heart, Lung and Blood Institute at the National Institutes of Health. We would like to acknowledge Dr. James Hawkins, Dr. Robert Hoyt, The NIH Division of Veterinary Resources and the staff of the Cardiothoracic Surgery Research program at the NIH.
References
- Mozaffarian D, et al. Executive Summary: Heart Disease and Stroke Statistics--2016 Update: A Report From the American Heart Association. Circulation. 2016;133(4):447–454. doi: 10.1161/CIR.0000000000000366. [DOI] [PubMed] [Google Scholar]
- Heron M. National Vital Statistics Reports. 5. Vol. 65. Washington, DC: Public Health Service; 2016. Deaths: Leading causes for 2014. [PubMed] [Google Scholar]
- Tsang HG, Rashdan NA, Whitelaw CBA, Corcoran BM, Summers KM, MacRae VE. Large animal models of cardiovascular disease. Cell Biochem Funct. 2016;34(3):113–132. doi: 10.1002/cbf.3173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassaletta AD, Chu LM, Sellke FW. Therapeutic neovascularization for coronary disease: current state and future prospects. Basic Res Cardiol. 2011;106(6):897–909. doi: 10.1007/s00395-011-0200-1. [DOI] [PubMed] [Google Scholar]
- Tuzun E, et al. Correlation of Ischemic Area and Coronary Flow With Ameroid Size in a Porcine Model. J Surg Res. 2010;164(1):38–42. doi: 10.1016/j.jss.2009.03.024. [DOI] [PubMed] [Google Scholar]
- Hughes GC, Post MJ, Simons M, Annex BH. Translational Physiology: Porcine models of human coronary artery disease: implications for preclinical trials of therapeutic angiogenesis. J Appl Physiol. 2003;94(5):689–701. doi: 10.1152/japplphysiol.00465.2002. [DOI] [PubMed] [Google Scholar]
- Sabe AA, et al. Investigating the effects of resveratrol on chronically ischemic myocardium in a swine model of metabolic syndrome: a proteomics analysis. J Med Food. 2015;18(1):60–66. doi: 10.1089/jmf.2014.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos A, et al. Cardiovascular imaging: what have we learned from animal models? Front Pharmacol. 2015;6:227. doi: 10.3389/fphar.2015.00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klocke R, Tian W, Kuhlmann MT, Nikol S. Surgical animal models of heart failure related to coronary heart disease. Cardiovasc Res. 2007;74(1):29–38. doi: 10.1016/j.cardiores.2006.11.026. [DOI] [PubMed] [Google Scholar]
- Tarkia M, et al. Cardiac remodeling in a new pig model of chronic heart failure: Assessment of left ventricular functional, metabolic, and structural changes using PET, CT, and echocardiography. J Nucl Cardiol. 2015;22(4):655–665. doi: 10.1007/s12350-015-0068-9. [DOI] [PubMed] [Google Scholar]
- Caillaud D, et al. Echocardiographic analysis with a two-dimensional strain of chronic myocardial ischemia induced with ameroid constrictor in the pig. Interact Cardiovasc Thorac Surg. 2010;10(5):689–693. doi: 10.1510/icvts.2010.232819. [DOI] [PubMed] [Google Scholar]
- Unger EF. Experimental evaluation of coronary collateral development. Cardiovasc Res. 2001;49(3):497–506. doi: 10.1016/s0008-6363(00)00285-6. [DOI] [PubMed] [Google Scholar]
- Giordano C, Kuraitis D, Beanlands RS, Suuronen EJ, Ruel M. Cell-based vasculogenic studies in preclinical models of chronic myocardial ischaemia and hibernation. Expert Opin Biol Ther. 2013;13(3):411–428. doi: 10.1517/14712598.2013.748739. [DOI] [PubMed] [Google Scholar]
- St Louis JD, et al. An Experimental Model of Chronic Myocardial Hibernation. Ann Thorac Surg. 2000;69(5):1351–1357. doi: 10.1016/s0003-4975(00)01130-9. [DOI] [PubMed] [Google Scholar]
- Green JD, et al. Comparison of X-ray fluoroscopy and interventional magnetic resonance imaging for the assessment of coronary artery stenoses in swine. Magn Reson Med. 2005;54(5):1094–1099. doi: 10.1002/mrm.20699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu Q, Lin Y, Xiao C, et al. Time-Course of the Effects of QSYQ in Promoting Heart Function in Ameroid Constrictor-Induced Myocardial Ischemia Pigs. Evid Based Complement Alternat Med. 2014. [DOI] [PMC free article] [PubMed]
- Zhou Y, et al. Direct Injection of Autologous Mesenchymal Stromal Cells Improves Myocardial Function. Biochem Biophys Res Commun. 2009;390(3):902–907. doi: 10.1016/j.bbrc.2009.10.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radke PW, et al. Evaluation of the porcine ameroid constrictor model of myocardial ischemia for therapeutic angiogenesis studies. Endothelium. 2006;13(1):25–33. doi: 10.1080/10623320600660128. [DOI] [PubMed] [Google Scholar]
- Estvold SK, et al. Does laser type impact myocardial function following transmyocardial laser revascularization? Lasers Surg Med. 2010;42(10):746–751. doi: 10.1002/lsm.21012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar AH, et al. Intravascular cell delivery device for therapeutic VEGF-induced angiogenesis in chronic vascular occlusion. Biomaterials. 2014;35(32):9012–9022. doi: 10.1016/j.biomaterials.2014.07.016. [DOI] [PubMed] [Google Scholar]
- JoVE Science Education Database. Essentials of Lab Animal Research: Considerations for Rodent Surgery. JoVE, Cambridge, MA: 2017. Available from: https://www.jove.com/science-education/10285/considerations-for-rodent-surgery. [Google Scholar]
- Cao X, et al. Coronary artery vasospasms in a microminipig occurred after placing an ameroid constrictor. J Vet Med Sci. 2016;78(7):1213–1216. doi: 10.1292/jvms.16-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sereda CW, Adin CA. Methods of Gradual Vascular Occlusion and Their Applications in Treatment of Congenital Portosystemic Shunts in Dogs: A Review. Veterinary Surgery. 2005;34:83–91. doi: 10.1111/j.1532-950X.2005.00015.x. [DOI] [PubMed] [Google Scholar]
- Ikonen TS, et al. Ligation of ameroid-stenosed coronary artery leads to reproducible myocardial infarction--a pilot study in a porcine model. J Surg Res. 2007;142(1):195–201. doi: 10.1016/j.jss.2007.01.022. [DOI] [PubMed] [Google Scholar]
- Adin CA, Gregory CR, Kyles AE, Griffey SM, Kendall L. Effect of Petrolatum Coating on the Rate of Occlusion of Ameroid Constrictors in the Peritoneal Cavity. Veterinary Surgery. 2004;33:11–16. doi: 10.1111/j.1532-950x.2004.04001.x. [DOI] [PubMed] [Google Scholar]
- Griffin MA, Hunt GB, Epstein SE. Behavior of plastic and metal ameroid constrictors during in vitro incubation in physiologic solutions of varying glucose concentration. Res Vet Sci. 2016;105:165–170. doi: 10.1016/j.rvsc.2016.02.002. [DOI] [PubMed] [Google Scholar]


