Abstract
Many potential causative factors are related to the initiation and progression of osteonecrosis of the femoral head (ONFH). The matrix metalloproteinase/tissue inhibitor of metalloproteinases (MMPs/TIMPs) system was found to play a significant role in the development of ONFH. The aim of this study is to investigate the association between polymorphisms of MMP-3 and ONFH in the Chinese population. We selected 8 single-nucleotide polymorphisms (SNPs) in 2 genes selected from the MMPs/TIMPs system in a case–control study with 585 cases of ONFH and 507 healthy controls. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated using the chi-squared test, genetic model analysis, haplotype analysis, and stratification analysis. We found that the minor allele of rs650108 and rs522616 (p<0.05) was assumed a risk allele compared to the wild-type allele. In the genetic model analysis, We observed two susceptibility SNPs additionally: rs650108, dominant model analyses (with adjustment: OR=0.73; 95%CI 0.56-0.95; p=0.017) and additive model analyses (with adjustment: OR=0.83; 95%CI 0.70-0.99; p=0.044); and rs522616 recessive model analyses (with adjustment: OR=1.52; 95%CI 1.07-2.14; p=0.018) and additive model analyses (with adjustment: OR=1.21; 95% CI 1.02-1.44; p=0.033). Our results verify that genetic variants of MMP3 contribute to ONFH susceptibility in the population of northern China. In addition, we found that gender differences might interact with MMP3 polymorphisms to contribute to the overall susceptibility to ONFH.
Keywords: case-control study, MMP3, single-nucleotide polymorphism, osteonecrosis of the femoral head
INTRODUCTION
Osteonecrosis of the femoral head (ONFH) is a debilitating bone disease in which patients experience the collapse of the joint cartilage and femoral head and a subsequent loss of joint function caused by abnormities in the fibrinolytic system and a disorder in the blood supply [1–3]. Since this stubborn disease may seriously affect the quality of life for patients, a large number of researchers have kept an eye on the identification of risk factors for ONFH. A great deal of ONFH cases develop in association with alcohol intake and steroid therapy are also contributing factors. Though it is well known that ONFH is caused by many factors, genetic factors have been demonstrated to be a strong factor of this disturbance. Many candidate genes have been shown related to ONFH in previous studies [4].
Repair ability and bony remodeling play a significant part in the development and severity of ONFH, nevertheless, little is known about the potential regulatory and repair machine-processed [5, 6]. Matrix metalloproteinases (MMPs), an enzyme family that provides the extracellular matrix (ECW) remodeling, play an important parts in the tissue remodeling process and physiological and pathological repair [7, 8]. MMPs and tissue inhibitor of matrix metalloproteases (TIMPs) expression and activity that may increase the ability to repair damaged bone matrix influencing the equilibrium between bone resorption and de novo bone formation in ONFH.
The ECW host some structural molecules (protein, proteoglycans, polysaccharides) as well as some enzymes, both being secreted by certain cells forming a 3-dimensional macromolecule network specific to different tissues, in a way to create cellular microenvironments or niches. In case the regulation of ECW remodeling is lost, tissue integrity is jeopardized, leading to development of pathological processes including connective tissue disorders, cancer, and metastasis (tumor microenvironment) [9, 10]. Matrix metalloproteinases (MMPs), an enzyme family that provides the ECW remodeling, are responsible for degradation of ECW elements. In biology, MMPs have been linked to ECM degradation and turnover [11, 12]. Though certain MMPs are expressed in bone and cartilage tissue during the normal bone development, MMPs-2,-9,-13,-14, and-16 play an essential part in skeletal development, as shown by knockout mice models and human genetic diseases [13, 14]. MMP-3 is a part of the stromelysin which is expressed in few cell types that contain human articular chondrocytes and synoviocytes [15]. According to reports in the literature, Other MMPs can proteolytically activated by MMP-3, and pathological conditions might ensue by means of the MMP genes overexpression [16].
Studies have demonstrated association of MMP-3 polymorphism with knee osteoarthritis and osteosarcoma [17, 18]. Nevertheless, previous studies have rarely investigated the association between genetic variants in MMP-3 and the risk of ONFH. We conducted a case-control study to analyze the relevance between 8 single nucleotide polymorphisms (SNPs) in MMP-3 and the risk of ONFH in a Chinese Han population.
RESULTS
A total of 585 cases and 507 controls were included in this study. The demographic in ONFH cases and control are shown in Table 1. As shown in Table 2, the Sequenom MassARRAY Assay Design 3.0 Software was used to design a multiplexed SNP MassEXTEND assay. All 8 single nucleotide polymorphisms were checked for Hardy Weinberg equilibrium in the control group (Table 3). We used chi square test to compare the allelic frequency distributions between cases and controls.
Table 1. Characteristics of cases and controls in this study.
| Variable(s) | Case (n=585) |
Control (n=507) |
p value |
|---|---|---|---|
| Sex N(%) | >0.05a | ||
| Male | 472(80.7) | 396(78.1) | |
| Female | 113(19.3) | 111(21.9) | |
| Age, years (mean ± SD) | 42.61±12.95 | 47.43±9.74 | <0.001b |
p ≤ 0.05 indicates statistical significance.
a Two-sided Chi-squared test.
b Independent samples t test.
Table 2. Primers Used for this Study.
| SNP_ID | 1st-PCRP | 2nd-PCRP | UEP_SEQ |
|---|---|---|---|
| rs639752 | ACGTTGGATGCA GATAAATTCTCCACTTGC |
ACGTTGGATGGGCT GCAATGCAGGGAAAAG |
tGGGAAGAAAGA AATAGGTGAT |
| rs650108 | ACGTTGGATGGTC ACTGTCTCATTGTGTGT |
ACGTTGGATGTCAGG TAGAGGTGACAAGTG |
tAAGTGGGT GAGGTTAGA |
| rs520540 | ACGTTGGATGGCG AAAGGGCTTAACTGTTAT |
ACGTTGGATGCCA GCTCGTACCTCATTTCC |
CTCGTACCT CATTTCCTCTGAT |
| rs646910 | ACGTTGGATGCCA CTGTAAGCTGGTGACTA |
ACGTTGGATGGTTA AGCCCTTTCGCTTTAG |
CGCTTTAGAAA TACACTTTAGCATCT |
| rs602128 | ACGTTGGATGCT TCGGGATGCCAGGAAA |
ACGTTGGATGAAG CTGGACTCCGACACTCT |
CAGGTGTG GAGTTCCTGA |
| rs679620 | ACGTTGGATGAACA GGACCACTGTCCTTTC |
ACGTTGGATGAGA AATATCTAGAAAACTAC |
tcTCTAGAAAAC TACTACGACCTC |
| rs678815 | ACGTTGGATGAATG CAACGTAATTTTAGC |
ACGTTGGATGTGGA GTATTTCTCTAGCTTG |
TCTCTAGCTTG CTGAAATAATG |
| rs522616 | ACGTTGGATGCGTA GCTGCTCCATAAATAG |
ACGTTGGATGACAGAG AGAATTTCAGTCCG |
gaCGGTAAGCAA TGTAATTCATTTCA |
Table 3. Allele frequencies in cases and controls and odds ratio estimates for ONFH.
| SNP ID | Gene | Position | Alleles A/B | MAF | pa value for HWE | ORs | 95% CI | pb | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Case | Control | |||||||||
| rs639752 | MMP3 | 11q22.2 | C/A | 0.32 | 0.35 | 0.116 | 0.88 | 0.74 | 1.06 | 0.177 |
| rs650108 | MMP3 | 11q22.2 | G/A | 0.39 | 0.44 | 0.147 | 0.84 | 0.70 | 0.99 | 0.040* |
| rs520540 | MMP3 | 11q22.2 | A/G | 0.32 | 0.35 | 0.116 | 0.88 | 0.74 | 1.06 | 0.177 |
| rs646910 | MMP3 | 11q22.2 | A/T | 0.07 | 0.09 | 1 | 0.82 | 0.60 | 1.13 | 0.224 |
| rs602128 | MMP3 | 11q22.2 | A/G | 0.32 | 0.34 | 0.235 | 0.90 | 0.75 | 1.07 | 0.234 |
| rs679620 | MMP3 | 11q22.2 | T/C | 0.32 | 0.35 | 0.202 | 0.88 | 0.74 | 1.05 | 0.156 |
| rs678815 | MMP3 | 11q22.2 | G/C | 0.32 | 0.35 | 0.141 | 0.88 | 0.74 | 1.05 | 0.165 |
| rs522616 | MMP3 | 11q22.2 | C/T | 0.40 | 0.35 | 0.923 | 1.20 | 1.00 | 1.42 | 0.044* |
SNP single nucleotide polymorphism, HWE Hardy-Weinberg equilibrium, OR odds ratio, 95% CI 95% confidence interval, MAF minor allele frequency.
* p ≤ 0.05 indicates statistical significance.
a p was calculated by exact test.
bp was calculated by Pearson Chi-squared test.
As a result, we discovered that rs650108 and rs522616 were associated with ONFH risk in the MMP3 (rs650108 p = 0.040, OR=0.83; 95 % CI:0.70–0.99 and rs522616 p = 0.044, OR=1.20; 95 % CI:1.01–1.42). A rigorous Bonferroni correction analysis was applied so as to reduce the potential of spurious findings due to multiple testing. Nevertheless, the difference was no longer significant after Bonferroni correction. In contrast to wild-type alleles, the minor allele of each SNP was assumed a risk allele. We have listed the Minor allele frequency (MAF) in cases and controls in Table 3.
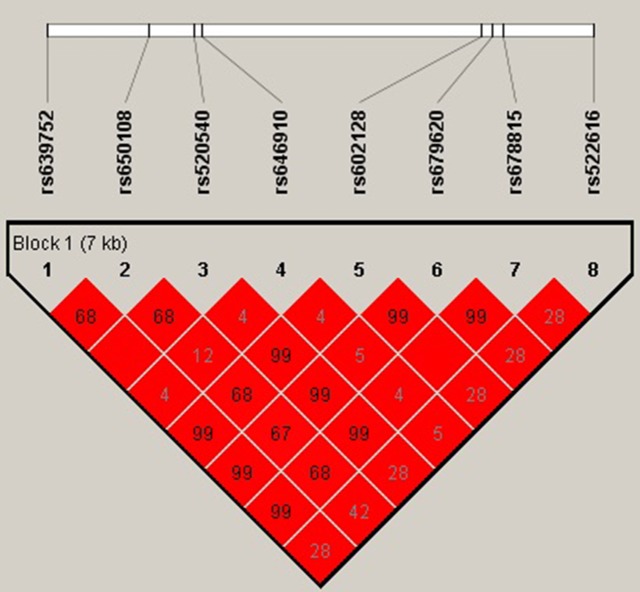
As listed in Table 4, we compared the risk of ONFH and the SNP genotypes. We identified the association between two significant SNP genotypes and the risk of ONFH. We observed two susceptibility SNPs additionally under two models respectively: rs650108, dominant model (with adjustment: OR=0.73; 95% CI:0.56-0.95; p = 0.017) and additive model(with adjustment: OR=0.83; 95% CI:0.70-0.99; p = 0.044); and rs522616 recessive model(with adjustment: OR=1.52; 95% CI:1.07-2.14; p = 0.018) and additive model (with adjustment: OR=1.21; 95% CI:1.02-1.44; p = 0.033). We use linkage disequilibrium (LD) and haplotype analyses to characterize the SNPs in MMP3. We calculated LD between 8 SNPs and the haplotype structure of the MMP3 gene was analyzed (r2). However, the significant difference was not found in haplotypes analysis. LD blocks were detected in the control group (Figure 1).
Table 4. Genotypic model analysis of relationship between SNPs and ONFH risk.
| SNPs | Model | Genotype | Group=control | Group=hormone | Without adjustment | With adjustment | AIC | BIC | ||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | pa-value | OR (95% CI) | pa-value | |||||||
| rs650108 | Codominant | A/A | 153 (30.3%) | 216 (37%) | 1.00 | 0.065 | 1.00 | 0.058 | 1461.8 | 1486.8 |
| A/G | 265 (52.5%) | 279 (47.8%) | 0.75 (0.57-0.97) | 0.73(0.55-0.96) | ||||||
| G/G | 87 (17.2%) | 89 (15.2%) | 0.72 (0.51-1.04) | 0.74 (0.51-1.07) | ||||||
| Dominant | A/A | 153 (30.3%) | 216 (37%) | 1.00 | 0.02* | 1.00 | 0.017* | 1459.8 | 1479.8 | |
| A/G-G/G | 352 (69.7%) | 368 (63%) | 0.74 (0.57-0.95) | 0.73(0.56-0.95) | ||||||
| Recessive | A/A-A/G | 418 (82.8%) | 495 (84.8%) | 1.00 | 0.37 | 1.00 | 0.5 | 1465 | 1485 | |
| G/G | 87 (17.2%) | 89 (15.2%) | 0.86 (0.63-1.19) | 0.89 (0.64-1.24) | ||||||
| Overdominant | A/A-G/G | 240 (47.5%) | 305 (52.2%) | 1.00 | 0.12 | 1.00 | 0.08 | 1462.4 | 1482.4 | |
| A/G | 265 (52.5%) | 279 (47.8%) | 0.83 (0.65-1.05) | 0.80 (0.63-1.03) | ||||||
| Log-additive | — | — | — | 0.83 (0.70-0.99) | 0.037* | 0.83 (0.70-1.00) | 0.044* | 1461.5 | 1481.4 | |
| rs522616 | Codominant | T/T | 212 (41.9%) | 224 (38.3%) | 1 | 1 | 0.052 | 1464.3 | 1489.2 | |
| T/C | 230 (45.5%) | 259 (44.3%) | 1.07 (0.82-1.38) | 0.078 | 1.08 (0.83-1.40) | |||||
| C/C | 64 (12.7%) | 102 (17.4%) | 1.51 (1.05-2.17) | 1.57(1.08-2.29) | ||||||
| Dominant | T/T | 212 (41.9%) | 224 (38.3%) | 1 | 0.23 | 1 | 0.19 | 1466.4 | 1486.4 | |
| T/C-C/C | 294 (58.1%) | 361 (61.7%) | 1.16 (0.91-1.48) | 1.18 (0.92-1.52) | ||||||
| Recessive | T/T-T/C | 442 (87.3%) | 483 (82.6%) | 1 | 0.027* | 1 | 0.018* | 1462.6 | 1482.5 | |
| C/C | 64 (12.7%) | 102 (17.4%) | 1.46 (1.04-2.05) | 1.52(1.07-2.14) | ||||||
| Overdominant | T/T-C/C | 276 (54.5%) | 326 (55.7%) | 1 | 0.7 | 1 | 0.69 | 1468 | 1488 | |
| T/C | 230 (45.5%) | 259 (44.3%) | 0.95 (0.75-1.21) | 0.95 (0.75-1.21) | ||||||
| Log-additive | — | — | — | 1.19 (1.00-1.41) | 0.048* | 1.21(1.02-1.44) | 0.033* | 1463.6 | 1483.6 | |
*p ≤ 0.05 indicates statistical significance.
p values were calculated by Wald test by unconditional logistic regression adjusted for age and gender.
AIC, Akaike’s Information criterion; BIC, Bayesian Information criterion.
Figure 1. Linkage disequilibrium (LD) plots containing 8 SNPs from MMP3.
Red squares display statistically significant associations between a pair of SNPs, as measured by r2; darker shades of red indicate higher r2.
DISCUSSION
We researched the associations between 8 SNPs in the MMP3 gene and the risk of ONFH. In this case-control study, we confirmed for the first time that MMP3 genetic polymorphisms (rs650108 and rs522616) were associated with a risk of ONFH. We can also observed that a protective effect for the dominant model “A/G-G/G” of rs650108 the MMP3 gene was related to a reduction in the risk of developing ONFH. Furthermore, it can be found that a strong effect of the “C/C” recessive model of rs522616 in the MMP3 can increase the risk of developing ONFH.
It is well know that the SNP occurring in MMP gene promoters can affect the expression of MMPs [19]. MMP3, a member of the family of endogenous proteolytic enzymes, is produced by chondrocytes and can degrade many extracellular matrix components except glucose [20]. Previous study has shown that the dynamic equilibrium between the Timp3 and Mmp3 is broken, the inhibition of MMP3 by TIMP3 would be reduced, and the degradation of matrix proteins would be increased in the model rats. It also shows that the development of osteoarthritis can be influenced by the destruction of the balance between MMP3 and TIMP3 [20]. In addition, cartilage degeneration may happen during latestage steroid-induced osteonecrosis of the femoral head, after bone tissue collapse [21].Thus, we postulate that MMP3 is related to ONFH.
In our study, we investigated eight SNPs in MMP3 (in Table 3). Among these SNPs, the rs522616 and rs650108 polymorphisms of MMP-3 have been identified in different diseases, such as chronic periodontitis and sporadic brain arteriovenous malformation [22, 23]. It is not completely determined whether the rs522616 and rs650108 polymorphisms of MMP-3 can influence the susceptibility or severity in patients with ONFH. Therefore, it has been hypothesized that the genetic variations in MMP3 can influence the susceptibility to ONFH. In our study, we only found that the SNPs of the rs522616 and rs650108 are associated with a risk of ONFH. As far as we know, we are the first to report the relation between MMP-3 polymorphisms rs522616, rs650108 and ONFH risk, but the conclusion identified should be proved in further studies.
There are important discoveries revealed in our study, but some limitations of this study should be considered when interpreting these results. First of all, our study does not include an analysis of biological functions, which will be crucial for elucidating the role of MMP3 in ONFH. Secondly, risk factors for ONFH can be classified into different clinical causes for further analysis. Thirdly, the participants in our study were all Han Chinese individuals recruited from the Zhengzhou Traditional Chinese Medicine Traumatology Hospital, which might involve a selection bias. Fourthly, we used a hospital-based case–control design, which may involve selection bias. Finally, the sample size was relatively small after stratification by sex, which might convert the positive findings into negative results. A larger case–control study is expected to circumvent those problems, which could make our conclusions more powerful.
To sum up, we have confirmed for the first time that 2 susceptive SNPs (rs522616 and rs650108) of MMP3 from the MMPs/TIMPs system exhibit a significant association with increased risk of ONFH in the population of northern China. Further functional studies and larger population-based studies are needed to confirm our results.
MATERIALS AND METHODS
Ethics statement
The use of human tissue and the protocol in this study were abided by the principles of the Declaration of Helsinki and were approved by the Ethical Committee of Zhengzhou Traditional Chinese Medicine Traumatology Hospital. All candidate subjects signed informed consent.
Study population
We recruited a total of 585 patients diagnosed with ONFH and 507 control subjects were consecutively enrolled from 2014 to 2015 among Han Chinese. All the subjects were treated by the Affiliated Zhengzhou Traditional Chinese Medicine Traumatology Hospital. All cases were verified, and patients were recruited without age, sex, or disease stage restriction. Moreover, patients did not receive systemic inflammatory treatment including drug control treatment before the blood samples used in this study were obtained.
A number of 507 healthy unrelated individuals were recruited randomly as sample, and the participants were Han Chinese living in Zhengzhou city and nearby. All of the chosen subjects were from the Zhengzhou Traditional Chinese Medicine Traumatology Hospital. To reduce the potential environmental and therapeutic factors impacting the variation of complex human diseases, we performed detailed recruitment and set exclusion criteria to exclude subjects with diseases related to genetic susceptibility, such as tumor.
SNP selection and genotyping
We selected 8 SNPs for investigation in this study. We prioritized SNPs to be studied considering: (a) previous reports of expression in diseased tissues, (b) previous reports of association with ONFH, (c) substrates as recognized molecules in diseased tissues.
Within selected SNPs, 8 polymorphisms were selected based on published reports and/or their locations in the genes, based on their likelihood to have functional consequences (i.e., located in the promoters, exons or near exon/intron boundaries), or if considered tag-SNPs as surrogates for the linkage disequilibrium blocks surrounding the candidate gene. We used information from the NCBI dbSNP (http://www.ncbi.nlm.nih.gov/snp) and the HapMap Project (http://www.hapmap.org) databases.
A total of 8 tSNPs in the MMP3 gene were selected for further genotyping. The phenol–chloroform extraction method was performed to extract genomic DNA from whole blood [24]. DNA concentration was measured by spectrometry (DU530 UV/VIS spectrophotometer, Beckman Instruments, Fullerton, CA, USA). Sequenom MassARRAY Assay Design 3.0 software was used to design multiplexed SNP MassEXTEND assay, and SNP genotyping was performed utilizing the Sequenom MassARRAY RS1000 recommended by the manufacturer [25]. Data management and analyses were performed using the Sequenom Typer 4.0 software as previouslydescribed [25, 26].
Statistical analysis
We used Microsoft Excel and SPSS 16.0 (SPSS, Chicago, IL, USA) to perform statistical analyses. In this study, all p values were two-sided, and p ≤ 0.05 was considered as achieving the threshold of statistical significance. Observed genotype frequencies were compared with expected frequencies to test for deviations from Hardy–Weinberg equilibrium (HWE). Chi-squared test/Fisher’s exact test was used to calculate the allele and genotype frequencies of cases and controls [27]. ORs and 95% CIs were calculated by unconditional logistic regression analyses adjusted for age and sex [28]. The possibility of sex differences as a source of population substructure was evaluated by a genotype test for each SNP in male and female, and the number of significant results at the 5 % level was compared with the number expected by the Chi-squared test [27]. The five genetic models (codominant dominant, recessive overdominant and log-additive) were applied by PLINK software (http://pngu.mgh.harvard.edu/purcell/plink/) to assess the association of single tSNPs with the risk of ONFH. ORs and 95% CIs were calculated by unconditional logistic regression analyses adjusted for age and sex [28, 29] At last, we use the Haploview software package (version 4.2) [30]to evaluate LD patterns and haplotypes.
ACKNOWLEDGMENTS AND FUNDING
This work was supported by the National Natural Science Foundation of China (No. 81160228, 81260284, 81660378). It is our great honor to express heartfelt thanks to all of the patients and controls, the clinicians, and other hospital staff for their participation and contributions to this study.
Abbreviations
- CI
confidence interval
- HWE
Hardy–Weinberg equilibrium
- MMPs
matrix metalloproteinases
- OA
osteoarthritis
- ONFH
osteonecrosis of the femoral head
- OR
odds ratio
- SNPs
single-nucleotide polymorphisms
Footnotes
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
- 1.Kim H, Cho C, Cho Y, Cho S, Yoon K, Kim K. Significant associations of PAI-1 genetic polymorphisms with osteonecrosis of the femoral head. BMC Musculoskelet Disord. 2011;12:160. doi: 10.1186/1471-2474-12-160. https://doi.org/10.1186/1471-2474-12-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Assouline-Dayan Y, Chang C, Greenspan A, Shoenfeld Y, Gershwin ME. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum. 2002;32:94–124. [PubMed] [Google Scholar]
- 3.Taeho K, Hong JM, Hyunju K, Euikyun P, Shinyoon K. Lack of association of MTHFR gene polymorphisms with the risk of osteonecrosis of the femoral head in a Korean population. Mol Cells. 2010;29:343–8. doi: 10.1007/s10059-010-0054-7. [DOI] [PubMed] [Google Scholar]
- 4.Hadjigeorgiou G, Dardiotis E, Dardioti M, Karantanas A, Dimitroulias A, Malizos K. Genetic association studies in osteonecrosis of the femoral head: mini review of the literature. Skeletal Radiol. 2008;37:1–7. doi: 10.1007/s00256-007-0395-2. https://doi.org/10.1007/s00256-007-0395-2. [DOI] [PubMed] [Google Scholar]
- 5.Jingushi S, Lohmander LS, Shinmei M, Hoerrner LA, Lark MW, Sugioka Y, Iwamoto Y. Markers of joint tissue turnover in joint fluids from hips with osteonecrosis of the femoral head. J Orthop Res. 2000;18:728–33. doi: 10.1002/jor.1100180508. https://doi.org/10.1002/jor.1100180508. [DOI] [PubMed] [Google Scholar]
- 6.Radke S, Battmann A, Jatzke S, Eulert J, Jakob F, Schutze N. Expression of the angiomatrix and angiogenic proteins CYR61, CTGF, and VEGF in osteonecrosis of the femoral head. J Orthop Res. 2006;24:945–52. doi: 10.1002/jor.20097. https://doi.org/10.1002/jor.20097. [DOI] [PubMed] [Google Scholar]
- 7.Murphy G, Docherty AJ. The matrix metalloproteinases and their inhibitors. Am J Respir Cell Mol Biol. 1992;7:120–5. doi: 10.1165/ajrcmb/7.2.120. https://doi.org/10.1165/ajrcmb/7.2.120. [DOI] [PubMed] [Google Scholar]
- 8.Parsons S, Watson S, Brown P, Collins H, Steele R. Matrix metalloproteinases. Br J Surg. 1997;84:160–6. [PubMed] [Google Scholar]
- 9.Noguera R, Nieto OA, Tadeo I, Farinas F, Alvaro T. Extracellular matrix, biotensegrity and tumor microenvironment. An update and overview. Histol Histopathol. 2012;27:693–705. doi: 10.14670/HH-27.693. [DOI] [PubMed] [Google Scholar]
- 10.Rozario T, DeSimone DW. The extracellular matrix in development and morphogenesis: a dynamic view. Dev Biol. 2010;341:126–40. doi: 10.1016/j.ydbio.2009.10.026. https://doi.org/10.1016/j.ydbio.2009.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deryugina EI, Quigley JP. Pleiotropic roles of matrix metalloproteinases in tumor angiogenesis: contrasting, overlapping and compensatory functions. Biochim Biophys Acta. 2010;1803:103–20. doi: 10.1016/j.bbamcr.2009.09.017. https://doi.org/10.1016/j.bbamcr.2009.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Butler GS, Overall CM. Updated biological roles for matrix metalloproteinases and new “intracellular” substrates revealed by degradomics. Biochemistry. 2009;48:10830–45. doi: 10.1021/bi901656f. https://doi.org/10.1021/bi901656f. [DOI] [PubMed] [Google Scholar]
- 13.Page-McCaw A, Ewald AJ, Werb Z. Matrix metalloproteinases and the regulation of tissue remodelling. Nat Rev Mol Cell Biol. 2007;8:221–33. doi: 10.1038/nrm2125. https://doi.org/10.1038/nrm2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paiva KB, Granjeiro JM. Bone tissue remodeling and development: focus on matrix metalloproteinase functions. Arch Biochem Biophys. 2014;561:74–87. doi: 10.1016/j.abb.2014.07.034. https://doi.org/10.1016/j.abb.2014.07.034. [DOI] [PubMed] [Google Scholar]
- 15.Inoue K, Masuko-Hongo K, Okamoto M, Nishioka K. Induction of vascular endothelial growth factor and matrix metalloproteinase-3 (stromelysin) by interleukin-1 in human articular chondrocytes and synoviocytes. Rheumatol Int. 2005;26:93–8. doi: 10.1007/s00296-004-0513-6. https://doi.org/10.1007/s00296-004-0513-6. [DOI] [PubMed] [Google Scholar]
- 16.Nagase H, Suzuki K, Morodomi T, Enghild JJ, Salvesen G. Activation mechanisms of the precursors of matrix metalloproteinases 1, 2 and 3. Matrix Suppl. 1992;1:237–44. [PubMed] [Google Scholar]
- 17.Honsawek S, Malila S, Yuktanandana P, Tanavalee A, Deepaisarnsakul B, Parvizi J. Association of MMP-3 (-1612 5A/6A) polymorphism with knee osteoarthritis in Thai population. Rheumatol Int. 2013;33:435–9. doi: 10.1007/s00296-012-2371-y. https://doi.org/10.1007/s00296-012-2371-y. [DOI] [PubMed] [Google Scholar]
- 18.Abd-Allah SH, Shalaby SM, Pasha HF, El-Shal AS, Abou El-Saoud AM. Variation of matrix metalloproteinase 1 and 3 haplotypes and their serum levels in patients with rheumatoid arthritis and osteoarthritis. Genet Test Mol Biomarkers. 2012;16:15–20. doi: 10.1089/gtmb.2011.0003. [DOI] [PubMed] [Google Scholar]
- 19.Zhu C, Odeberg J, Hamsten A, Eriksson P. Allele-specific MMP-3 transcription under in vivo conditions. Biochem Biophys Res Commun. 2006;348:1150–6. doi: 10.1016/j.bbrc.2006.07.174. [DOI] [PubMed] [Google Scholar]
- 20.Tong P, Wu C, Jin H, Mao Q, Yu N, Holz JD, Shan L, Liu H, Xiao L. Gene expression profile of steroid-induced necrosis of femoral head of rats. Calcif Tissue Int. 2011;89:271–84. doi: 10.1007/s00223-011-9516-y. [DOI] [PubMed] [Google Scholar]
- 21.Magnussen RA, Guilak F, Vail TP. Articular cartilage degeneration in post-collapse osteonecrosis of the femoral head. J Bone Joint Surg Am. 2005;87:1272–7. doi: 10.2106/JBJS.D.01936. [DOI] [PubMed] [Google Scholar]
- 22.Zhao Y, Li P, Fan W, Chen D, Gu Y, Lu D, Zhao F, Hu J, Fu C, Chen X. The rs522616 polymorphism in the matrix metalloproteinase-3 (MMP-3) gene is associated with sporadic brain arteriovenous malformation in a Chinese population. J Clin Neurosci. 2010;17:1568–72. doi: 10.1016/j.jocn.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 23.Juran BD, Atkinson EJ, Schlicht EM, Larson JJ, Ellinghaus D, Franke A, Lazaridis KN. Genetic polymorphisms of matrix metalloproteinase 3 in primary sclerosing cholangitis. Liver Int. 2011;31:785–91. doi: 10.1111/j.1478-3231.2010.02420.x. https://doi.org/10.1111/j.1478-3231.2010.02420.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kochl S, Niederstatter H, Parson W. DNA extraction and quantitation of forensic samples using the phenol-chloroform method and real-time PCR. Methods Mol Biol. 2005;297:13–30. doi: 10.1385/1-59259-867-6:013. [DOI] [PubMed] [Google Scholar]
- 25.Gabriel S, Ziaugra L, Tabbaa D. SNP genotyping using the Sequenom MassARRAY iPLEX platform. Curr Protoc Hum Genet. 2009 doi: 10.1002/0471142905.hg0212s60. Chapter 2: Unit 2.12. https://doi.org/10.1002/0471142905.hg0212s60. [DOI] [PubMed] [Google Scholar]
- 26.Thomas RK, Baker AC, Debiasi RM, Winckler W, Laframboise T, Lin WM, Wang M, Feng W, Zander T, MacConaill L, Lee JC, Nicoletti R, Hatton C, et al. High-throughput oncogene mutation profiling in human cancer. Nat Genet. 2007;39:347–51. doi: 10.1038/ng1975. https://doi.org/10.1038/ng1975. [DOI] [PubMed] [Google Scholar]
- 27.Adamec C. [Example of the use of the nonparametric test. Test x2 for comparison of 2 independent examples]. [Article in Czech] Cesk Zdrav. 1964;12:613–9. [PubMed] [Google Scholar]
- 28.Bland JM, Altman DG. Statistics notes. The odds ratio. BMJ. 2000;320:1468. doi: 10.1136/bmj.320.7247.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, Sham PC. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81:559–75. doi: 10.1086/519795. https://doi.org/10.1086/519795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shi YY, Lin HE. SHEsis, a powerful software platform for analyses of linkage disequilibrium, haplotype construction, and genetic association at polymorphism loci. Cell Res. 2005;15:97–8. doi: 10.1038/sj.cr.7290272. [DOI] [PubMed] [Google Scholar]