With the development of endoscopic ultrasound (EUS), EUS-guided gallbladder drainage (EUS-GBD) has gradually emerged as a viable option for gallbladder disease nonamenable to surgical intervention. Calculous and acalculous cholecystitis, biliary malignancy with the patent cystic duct, and gallbladder hydrops are a few of the indications for this novel technique.[1,2]
Baron and Topazian were first to describe EUS-GBD, which has since improved substantially in terms of technique and results.[3] Currently, EUS-GBD has the tendency to replace percutaneous transhepatic GBD, with some studies indicating similar technical and clinical success rates;[4] and EUS-GBD is clearly an alternative for patients who are not candidates for surgery. Those who undergo EUS-GBD seem to have shorter hospital stays, lower pain scores, and fewer repeated interventions, trending toward fewer adverse events as well.[5] Hence, EUS-GBD is assuming increasingly greater importance.
Early case series investigations of EUS-GBD have shown that plastic biliary stents placed across transmural tracts[3,6,7,8] routinely yielded success rates of 100%. However, plastic stents are prone to bile leakage (in the course of tract dilation), leading to bile peritonitis.[9] Self-expanding metal stents (SEMSs) that have been proven to be highly efficient for drainage of pancreatic fluid collections[10,11,12,13,14,15,16] were thus introduced, given their larger caliber, adjustable deployment, and the immediate sealing of fistulous tracts on stent expansion.[17,18] Partially covered stents or those with end-mounted flanges have also helped prevent migration.[9,19] In a modest number of patients (n = 15) studied by Jang et al.,[9] all procedures were technically successful, with no adverse events (such as stent migration or bile leakage), although self-limiting pneumoperitoneum (n = 2) did occur.
The latest innovation in EUS-GBD is the lumen-apposing metal stent (LAMS), offering a choice of luminal diameter (10 mm or 15 mm) and a dual dumbbell-shaped flange apparatus that hold two lumens in apposition. Such stents reduce the risks of bile leakage, stent migration, and stent occlusion.[20] Combination of metal and plastic stents for tandem deployment are also envisioned to prevent stent displacement and entry of food into the gallbladder. In theory, food or sludge in the gastrointestinal tract may flow into the gallbladder, through the patent cystic duct, and into bile duct, causing biliary obstruction or cholangitis. Takagi et al.[21] have targeted gallbladder neck for a puncture to prevent bile leakage and mechanical stent blockage. Of those patients treated (n = 16), only one instance of self-limiting pneumoperitoneum resulted. There were no other adverse events due to biliary leakage, stenting, recurrent cholecystitis, or cholangitis. Finally, Teoh et al.[22] have formulated a single-step EUS-guided puncture technique using a novel cautery-tipped stent delivery system for LAMS placement and GBD. This strategy may further serve to control bile leakage.
The clinical success rate for LAMS placement cited in some case reports and series and largely equated with clinical improvement and alleviation of pain/symptoms is also impressive (99.6%). Still, the peak technical success rate (97%) of one source[23] must be tempered by the lower rates of others.[1,24,25] According to de la Serna-Higuera et al.,[25] LAMS placement was proved successful in most patients (11/13, 85%), leaving two respective failures due to uncontrolled stent release (deploying fully in gastric lumen) and cobblestone gallbladder (preventing deep insertion and guidewire progression).[23] Likewise, only a single instance of intraperitoneal distal flange migration was encountered by Irani et al.[1] during stent placements. Although Walter et al.[24] logged a 10% (3/30 patients) rate of technical failures in LAMS placements, each failed attempt was remedied by inserting the second stent so that endoscopic GBD nevertheless took place. Their concern was that such remediation may falsely skew data on LAMS placement. In four patients counted as technical successes by de la Serna-Higuera et al.,[25] for example, each required a second fully covered tubular SEMS (inserted via LAMS) to ensure stent patency and stability. Assuming these secondary stentings were deemed technical failures, the stated technical success rate of 85% would instead be 46%.[23] At our endoscopy center, most procedural failures in patients subjected to EUS-GBD were attributable to collapse of the gallbladder. However, seldom do reports mention gallbladder collapse, which can be disastrous for outcomes of EUS-GBD.
Past improvements to EUS-GBD have pertained to stenting, puncture sites, and puncture systems. Because the gallbladder is a relatively soft tissue, electrocautery-enhanced LAMS (ECE-LAMS) delivery readily triggers collapse and positional shift, and the prospect of stent release would be just as formidable. Indeed, this dilemma may well be the Achilles’ heel of EUS-GBD. It has prompted us to devise the first-ever retrievable puncture anchor (Vedkang Inc., Changzhou, China) for gallbladder puncture and drainage that promises to minimize the above by throwing the gallbladder a lifeline. A therapeutic linear array echoendoscope is used in our approach, and under direct EUS visualization, distal gastric antrum, or duodenal bulb is punctured (19-gauge needle) to access gallbladder body. Once the stylet is removed, bile is aspirated and cultured, and contrast medium is injected for cholecystography. The retrievable anchor [Figure 1a and b] is then passed along the needle [Figure 1c and d] and engaged to anchor the gallbladder [Figure 2a]. After needle withdrawal, the gallbladder is pulled with the anchor when the gallbladder is punctured and drained using ECE-LAMS [Figure 2b]. After the procedure, the retrieval cord is pulled with a pair of forceps [Figure 3a and b], so the direction of the anchor is changed and it can be easily removed [Figure 3c].
Figure 1.
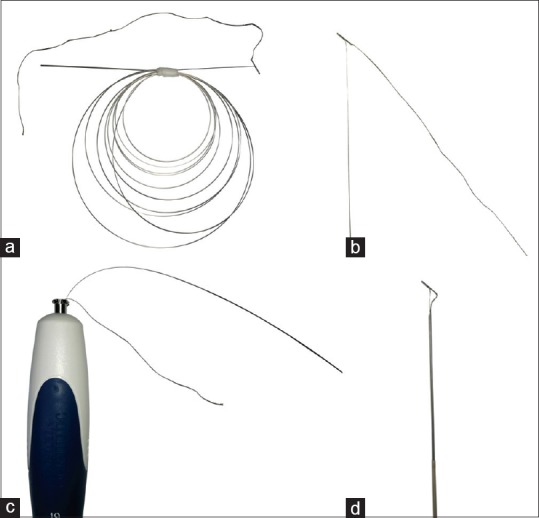
Attributes of retrievable puncture anchor (Vedkang Inc., Changzhou, China): (a) Anchor in its entirety; (b) head of anchor; and (c and d) passage of anchor along shaft of puncture needle
Figure 2.
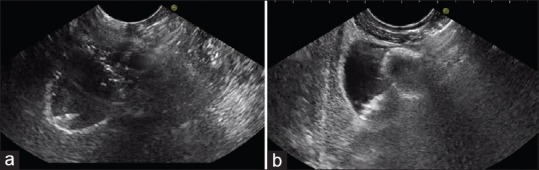
Endoscopic ultrasound images of retrievable puncture anchor: (a) Anchor inserted into gallbladder; and (b) anchor-grasped gallbladder under traction for stent implantation
Figure 3.
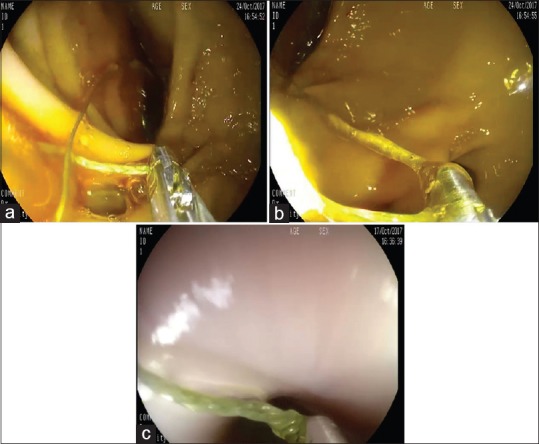
Endoscopic views of retrievable puncture anchor: Use of forceps to (a) clamp cord and (b) pull cord; and (c) anchor removal
Our retrievable puncture anchor traction method can not only reduce the collapse of the gallbladder so that the gallbladder space becomes larger, but also provide a pulling force in the opposite direction with the ECE-LAMS so that the gallbladder closer to the digestive tract. In this case, ECE-LAMS can be easily implanted. In the stent release process, pulling the gallbladder can make the internal space larger, which is more conducive to reduce the probability of stenting failure. Of note, these anchors are nondamaging to the gallbladder, and they are retrievable. This method heightens the probability of success by ensuring a simpler and safer procedure. Operator confidence is boosted as well.
Our protocol has been successfully tested in all four porcine models, performing EUS-GBD. The gallbladders of pigs are quite membranous without adhesion and even smaller than those of humans, so we are confident that availability is forthcoming. Improvements are naturally expected, but success rates should surpass those of existing practices owing to easier, safer interventions that require less operative time. We consider this a milestone for EUS-GBD and will turn over a new leaf for management of gallbladder diseases. Furthermore, this concept may be similarly applied to a broader range of endoscopic treatments.
REFERENCES
- 1.Irani S, Baron TH, Grimm IS, et al. EUS-guided gallbladder drainage with a lumen-apposing metal stent (with video) Gastrointest Endosc. 2015;82:1110–5. doi: 10.1016/j.gie.2015.05.045. [DOI] [PubMed] [Google Scholar]
- 2.Chaudhary S, Sun S. Endoscopic ultrasound-guided gallbladder drainage: Redefines the boundaries. Endosc Ultrasound. 2016;5:281–3. doi: 10.4103/2303-9027.191605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baron TH, Topazian MD. Endoscopic transduodenal drainage of the gallbladder: Implications for endoluminal treatment of gallbladder disease. Gastrointest Endosc. 2007;65:735–7. doi: 10.1016/j.gie.2006.07.041. [DOI] [PubMed] [Google Scholar]
- 4.Jang JW, Lee SS, Song TJ, et al. Endoscopic ultrasound-guided transmural and percutaneous transhepatic gallbladder drainage are comparable for acute cholecystitis. Gastroenterology. 2012;142:805–11. doi: 10.1053/j.gastro.2011.12.051. [DOI] [PubMed] [Google Scholar]
- 5.Irani S, Ngamruengphong S, Teoh A, et al. Similar efficacies of endoscopic ultrasound gallbladder drainage with a lumen-apposing metal stent versus percutaneous transhepatic gallbladder drainage for acute cholecystitis. Clin Gastroenterol Hepatol. 2017;15:738–45. doi: 10.1016/j.cgh.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 6.Kamata K, Kitano M, Komaki T, et al. Transgastric endoscopic ultrasound (EUS)-guided gallbladder drainage for acute cholecystitis. Endoscopy. 2009;41(Suppl 2):E315–6. doi: 10.1055/s-0029-1215258. [DOI] [PubMed] [Google Scholar]
- 7.Song TJ, Park DH, Eum JB, et al. EUS-guided cholecystoenterostomy with single-step placement of a 7F double-pigtail plastic stent in patients who are unsuitable for cholecystectomy: A pilot study (with video) Gastrointest Endosc. 2010;71:634–40. doi: 10.1016/j.gie.2009.11.024. [DOI] [PubMed] [Google Scholar]
- 8.Itoi T, Itokawa F, Kurihara T. Endoscopic ultrasonography-guided gallbladder drainage: Actual technical presentations and review of the literature (with videos) J Hepatobiliary Pancreat Sci. 2011;18:282–6. doi: 10.1007/s00534-010-0310-4. [DOI] [PubMed] [Google Scholar]
- 9.Jang JW, Lee SS, Park DH, et al. Feasibility and safety of EUS-guided transgastric/transduodenal gallbladder drainage with single-step placement of a modified covered self-expandable metal stent in patients unsuitable for cholecystectomy. Gastrointest Endosc. 2011;74:176–81. doi: 10.1016/j.gie.2011.03.1120. [DOI] [PubMed] [Google Scholar]
- 10.Ge N, Wang S, Wang S, et al. Endoscopic ultrasound-assisted cholecystogastrostomy by a novel fully covered metal stent for the treatment of gallbladder stones. Endosc Ultrasound. 2015;4:152–5. doi: 10.4103/2303-9027.156749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guo J, Liu Z, Sun S, et al. Removal of displaced double flanged metal stent in walled-off necrosis by endoscopic ultrasonography. Endosc Ultrasound. 2016;5:132–3. doi: 10.4103/2303-9027.180479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ang TL, Kongkam P, Kwek AB, et al. Atwo-center comparative study of plastic and lumen-apposing large diameter self-expandable metallic stents in endoscopic ultrasound-guided drainage of pancreatic fluid collections. Endosc Ultrasound. 2016;5:320–7. doi: 10.4103/2303-9027.191659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mukai S, Itoi T, Sofuni A, et al. Clinical evaluation of endoscopic ultrasonography-guided drainage using a novel flared-type biflanged metal stent for pancreatic fluid collection. Endosc Ultrasound. 2015;4:120–5. doi: 10.4103/2303-9027.156738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McVay T, Adler DG. EUS-guided drainage of pancreatic fluid collections: Double pigtails, metal biliary, or dedicated transluminal stents? Endosc Ultrasound. 2015;4:1–3. doi: 10.4103/2303-9027.151295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rana SS, Bhasin DK, Sharma R, et al. Factors determining recurrence of fluid collections following migration of intended long term transmural stents in patients with walled off pancreatic necrosis and disconnected pancreatic duct syndrome. Endosc Ultrasound. 2015;4:208–12. doi: 10.4103/2303-9027.162999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eliason K, Adler DG. Endoscopic ultrasound-guided transmural drainage of infected pancreatic necrosis developing 2 years after acute pancreatitis. Endosc Ultrasound. 2015;4:260–5. doi: 10.4103/2303-9027.163020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peñas-Herrero I, de la Serna-Higuera C, Perez-Miranda M. Endoscopic ultrasound-guided gallbladder drainage for the management of acute cholecystitis (with video) J Hepatobiliary Pancreat Sci. 2015;22:35–43. doi: 10.1002/jhbp.182. [DOI] [PubMed] [Google Scholar]
- 18.Choi JH, Lee SS, Choi JH, et al. Long-term outcomes after endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis. Endoscopy. 2014;46:656–61. doi: 10.1055/s-0034-1365720. [DOI] [PubMed] [Google Scholar]
- 19.Widmer J, Alvarez P, Gaidhane M, et al. Endoscopic ultrasonography-guided cholecystogastrostomy in patients with unresectable pancreatic cancer using anti-migratory metal stents: A new approach. Dig Endosc. 2014;26:599–602. doi: 10.1111/den.12163. [DOI] [PubMed] [Google Scholar]
- 20.Itoi T, Binmoeller KF, Shah J, et al. Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with videos) Gastrointest Endosc. 2012;75:870–6. doi: 10.1016/j.gie.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 21.Takagi W, Ogura T, Sano T, et al. EUS-guided cholecystoduodenostomy for acute cholecystitis with an anti-stent migration and anti-food impaction system; a pilot study. Therap Adv Gastroenterol. 2016;9:19–25. doi: 10.1177/1756283X15609285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Teoh AY, Binmoeller KF, Lau JY. Single-step EUS-guided puncture and delivery of a lumen-apposing stent for gallbladder drainage using a novel cautery-tipped stent delivery system. Gastrointest Endosc. 2014;80:1171. doi: 10.1016/j.gie.2014.03.038. [DOI] [PubMed] [Google Scholar]
- 23.Patil R, Ona MA, Papafragkakis C, et al. Endoscopic ultrasound-guided placement of the lumen-apposing self-expandable metallic stent for gallbladder drainage: A promising technique. Ann Gastroenterol. 2016;29:162–7. doi: 10.20524/aog.2016.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walter D, Teoh AY, Itoi T, et al. EUS-guided gall bladder drainage with a lumen-apposing metal stent: A prospective long-term evaluation. Gut. 2016;65:6–8. doi: 10.1136/gutjnl-2015-309925. [DOI] [PubMed] [Google Scholar]
- 25.de la Serna-Higuera C, Pérez-Miranda M, Gil-Simón P, et al. EUS-guided transenteric gallbladder drainage with a new fistula-forming, lumen-apposing metal stent. Gastrointest Endosc. 2013;77:303–8. doi: 10.1016/j.gie.2012.09.021. [DOI] [PubMed] [Google Scholar]


