Abstract
Background and Aims:
Hyponatremia is the predominant electrolyte abnormality with an incidence rate of approximately 22%. It is the leading cause of morbidity and mortality with scarce data in Indian intensive care settings. The aim of this study is to evaluate the clinical features and etiology of hyponatremia in patients admitted to an Intensive Care Unit (ICU) of a tertiary care hospital.
Materials and Methods:
A 1-year prospective cross-sectional observational study was conducted, including 100 adult patients with moderate-to-severe hyponatremia admitted to the Medical ICU. Patients underwent investigations such as serum creatinine, blood urea nitrogen, serum osmolality, serum sodium, urine sodium, and urine osmolality, sputum culture, cerebrospinal fluid analysis, and neuroimaging. Data were analyzed using independent sample t-test, Chi-square test, and Fisher's exact test.
Results:
Vomiting (28) followed by confusion (26) was the most common complaint. Syndrome of inappropriate antidiuretic hormone secretion (SIADH) (46) was the most common etiology for hyponatremia, and euvolemic hypoosmolar hyponatremia (50) was the most common type of hyponatremia. Confusion was significantly high in patients with severe hyponatremia as compared to patients with moderate hyponatremia (22 vs. 4, P < 0.001). In majority of the patients (46), SIADH was the main cause of euvolemic type of hyponatremia (P < 0.001). Increased urine sodium levels were observed in patients with SIADH (46), renal dysfunction (12), and drug-induced etiology (8, P < 0.001).
Conclusion:
Patients with hyponatremia secondary to an infectious cause should be meticulously screened for tuberculosis. The timely and effective treatment of hyponatremia is determined by the effective understanding of pathophysiology and associated risk factors of hyponatremia.
Keywords: Hyponatremia, moderate and severe hyponatremia, serum sodium, syndrome of inappropriate antidiuretic hormone secretion, tuberculosis
INTRODUCTION
Sodium-related disorders (both hyponatremia and hypernatremia) are extremely common and are associated with considerable morbidity and mortality.[1] Hyponatremia is the most common electrolyte disorder, reported in up to 6% of hospitalized patients. Mild hyponatremia (plasma sodium 125–135 mmol/l) is found in as many as 15%–30% of hospitalized patients, with an average of about 25% of Intensive Care Unit (ICU) patients experiencing this disorder.[2] Moderate-to-severe hyponatremia, especially which is rapid in onset, is associated with considerable morbidity and mortality. Despite the awareness on hyponatremia since long time, this common disorder remains an enigma due to its association with a plethora of underlying disease states and its multiple etiologies with different pathophysiological mechanisms.[3]
Hyponatremia, which is defined as the plasma sodium concentration of <135 mEq/L, occurs primarily due to imbalance in water homeostasis, antidiuretic hormone (ADH) regulation, and renal handling of filtered sodium. Syndrome of inappropriate ADH secretion (SIADH), a common cause of hyponatremia, is associated with many clinical conditions. These include neoplasia, central nervous system (CNS) disorders, drugs and pulmonary diseases.[3]
Tuberculosis (TB), one of the common illnesses in developing countries like India, can present with various clinical manifestations including nonspecific symptoms of hyponatremia. TB can induce hyponatremia via several mechanisms such as local invasion to the adrenal gland (leading to adrenal insufficiency), local invasion of hypothalamus or pituitary gland, tubercular meningitis, and inappropriate ADH secretion through pulmonary infections.
Timely diagnosis and treatment are the key to improved neurological status and reduced hospital stay. Determining the cause of hyponatremia is challenging in clinical practice. The clinical presentation of severe hyponatremia ranges from mild, nonspecific symptoms, such as nausea, headache, and lethargy, to severe neurological symptoms such as seizure and coma. The data available on clinical presentation and etiology are scarce in ICU settings, especially in those patients who develop moderate-to-severe hyponatremia. Hence, the present study was undertaken to assess the clinical profile and etiology of clinically significant hyponatremia, not only to aid in the treatment of patients but also to prevent further morbidity and mortality.
MATERIALS AND METHODS
Sampling and study design
The present 1-year cross-sectional observational study included 100 adult patients with moderate-to-severe hyponatremia admitted to the Medical ICU (MICU) was conducted at the Department of Medicine from January 2014 to December 2014. Patients aged ≥18 years with moderate-to-severe hyponatremia (≤125 mmol/L) admitted to the MICU were included in the study. The exclusion criteria comprised of cases with hyperglycemia, hyperlipidemia, and paraproteinemia. Ethical clearance was obtained from the Institutional Ethical Committee and after explaining the purpose of the study. Written consent from all the participants was obtained before data collection.
Instrumentation
Demographic data, including age and sex, were obtained from the patients. A history of other comorbid conditions along with presenting complaints was noted. Further, these patients were subjected to a physical examination for evaluating the clinical signs. The patients underwent the investigations including, complete blood count, random blood sugar, liver function tests, renal function tests, serum osmolality, urine osmolality, serum sodium, and urine sodium. Other investigations such as sputum culture, cerebrospinal fluid analysis, and neuroimaging were conducted wherever indicated. Based on the investigations, the type of hyponatremia was determined as euvolemic hypoosmolar, hypervolemia hypoosmolar, and hypovolemic hypoosmolar. Following this categorization, the etiology was determined and evaluated in different types of hyponatremia.
Statistics and data analysis
Before commencement of the study, ethical clearance was obtained from the Institutional Ethical Committee. After explaining the purpose of the study, written consent was obtained from the patients before data collection. Data were recorded in a predesigned and pretested pro forma. The data were coded and entered into Microsoft Excel Worksheet. The categorical data were expressed as rates, ratios, and proportions and the continuous data were expressed as mean ± standard deviation. The comparison of categorical data was performed using Chi-square test and Fisher's exact test and the comparison of continuous data was done using independent sample t-test. P ≤ 0.05 at 95% confidence interval was considered as statistically significant.
RESULTS
In the present study of 100 patients with hyponatremia, 59% were men and 41% were women. The male to female ratio was 1.43:1, of which most of the patients were aged between 61 and 70 years (29%) with a mean age of 58.94 ± 16.10 years. The most frequent presenting complaint was vomiting (28%) followed by confusion (26%), seizure (9%), and coma (4%) as depicted in Figure 1.
Figure 1.
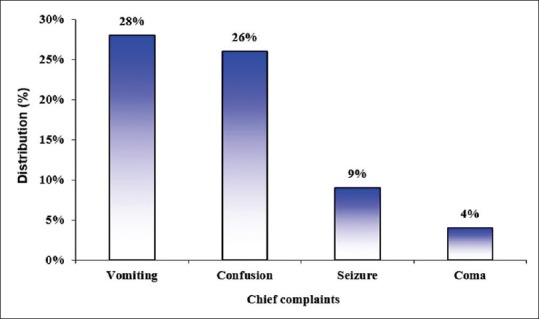
Chief complaints
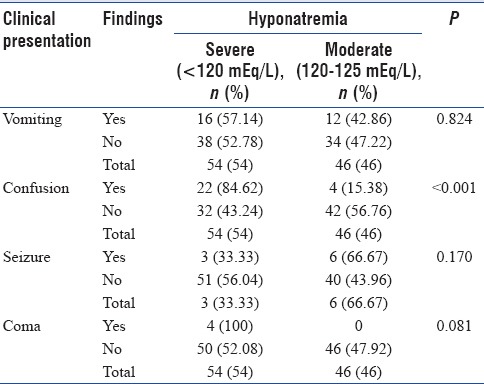
The serum sodium levels were <120 mEq/L (severe hyponatremia) in 54% of the patients and 46% of the patients had serum sodium levels (moderate hyponatremia) between 120 and 125 mEq/L as shown in Figure 2. On the basis of hydration status, 50% of the patients were euvolemic while 33% and 17% of the patients were hypervolemic and hypovolemic, respectively. Further, 50% of the patients had euvolemic hypoosmolar hyponatremia, 31% had hypervolemic hypoosmolar hyponatremia, 17% had hypovolemic hypoosmolar hyponatremia, and 2% had hypervolemic isoosmolar hyponatremia. When symptoms were correlated with severity, confusion was significantly high in patients with severe hyponatremia as compared to moderate hyponatremia (84.62 vs. 15.38%; P < 0.001). Other symptoms were correlated as shown in Table 1.
Figure 2.
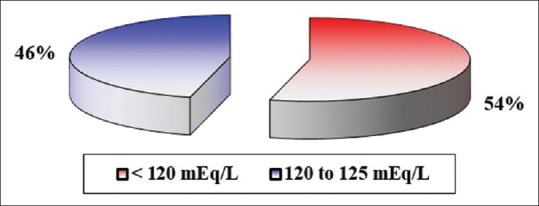
Distribution of patients as per serum sodium levels
Table 1.
Association of clinical presentation with severe and moderate hyponatremia
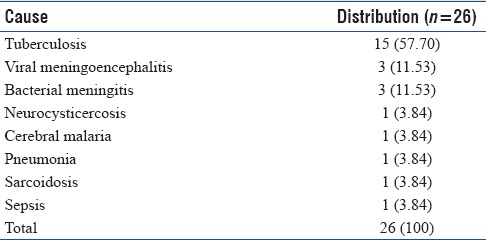
In our study of moderate-to-severe hyponatremia, CNS symptoms were predominant and were present among 61% of the patients. Of the 100 patients evaluated, 52% of the patients were conscious while 48% of the patients presented with altered sensorium. Among comorbid conditions, history of hypertension was present in 49% of the patients, whereas diabetes mellitus was noted among 29%. The most common system involved was CNS (43%) followed by abdominal (21%), renal (15%), cardiovascular (12%), and respiratory (9%) systems. While analyzing the cause of hyponatremia, SIADH was found to be the most frequent cause of hyponatremia observed among 46% of the patients. The other causes are as depicted in Figure 3. Further, on evaluating the cause of SIADH, infections (56.52%) were the predominant cause followed by disorders of CNS (26.08%) and neoplasm (6.52%). However, the cause could not be determined in 10.8% of the patients.
Figure 3.
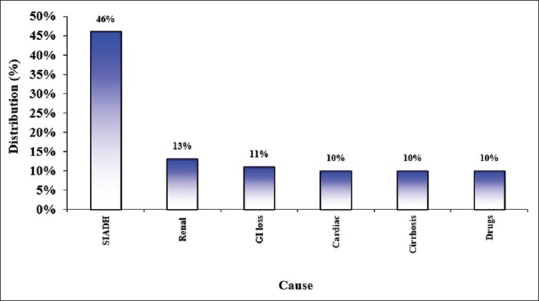
Causes of hyponatremia
The most common infectious etiology of SIADH was observed to be TB (57.7%) followed by viral meningoencephalitis (11.53%) and bacterial meningitis (11.53%). The most common form of TB among patients with SIADH was tubercular meningitis (46.67%). Tables 2–4 depict the various etiologies of SIADH. In the present study, majority (94%) of the patients had an improved outcome and mortality was noted in 6% of the patients.
Table 2.
Cause of syndrome of inappropriate antidiuretic hormone secretion in the study group
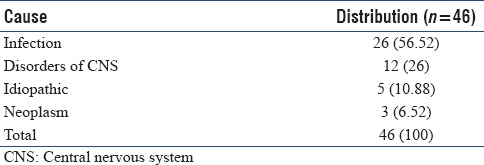
Table 4.
Profile of tuberculosis in patients with syndrome of inappropriate antidiuretic hormone secretion
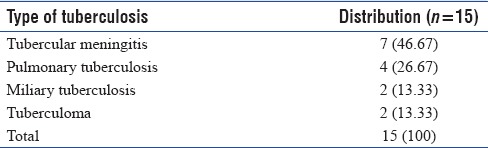
Table 3.
Infectious causes of syndrome of inappropriate antidiuretic hormone secretion in the study group
DISCUSSION
Despite being a commonly observed electrolyte imbalance, hyponatremia is incompletely understood. Its association with a plethora of underlying disease states and its multiple etiologies with differing pathophysiological mechanisms makes diagnosis challenging.[4] Hyponatremia of moderate-to-severe type causes increased inpatient mortality.[5,6,7,8] This study was as an attempt to describe the clinical profile and to find the etiology among patients with moderate-to-severe hyponatremia.
In our study, of 100 patients admitted with moderate-to-severe hyponatremia, slight male preponderance was observed. A similar gender distribution pattern was reported by Rahil et al. wherein 33 (62.3%) patients with hyponatremia were males and 20 (37.7%) were females.[9] In the present study, unlike many other studies, no association was found between gender and severity of hyponatremia (P = 0.642). The incidence of hyponatremia is higher in the elderly, owing to the impaired water and electrolyte homeostasis due to dietary and environmental variations.[4] In accordance with other reports,[2,5,10] in our study, hyponatremia was more prevalent among the elderly patients than in the younger patients.
Severe hyponatremia was more common than moderate hyponatremia. These findings were consistent with a study by Rahil et al.,[9] who studied the clinical presentation and etiology of moderate and severe hyponatremia in patients admitted to Hamad General Hospital in Doha from June 2007 to July 2008. Moderate-to-severe hyponatremia was reported in 53 patients, of which, moderate hyponatremia was observed in 31 (58.4%) patients, while severe hyponatremia was observed in 22 (41.6%) patients.[9] Another study conducted by Chowdhury et al. among 70 patients, reported mild hyponatremia, moderate hyponatremia, and severe hyponatremia in 27.14%, 37.14%, and 35.72% of the patients, respectively.[11]
Symptoms of hyponatremia range from mild (nausea, headache, and lethargy) to severe (seizures and coma).[12] In our study, when symptoms were correlated with severity of hyponatremia, confusion was significantly high in patients with severe hyponatremia as compared to moderate hyponatremia. In a study by Patni et al. in Nagpur, Maharashtra, similar findings were reported with drowsiness as the most common symptom (51%), followed by vomiting (14%) and seizures (6%).[13]
In more than half of the study population, CNS symptoms were observed. Recently, a descriptive study by Rao et al.[14] in Bangalore, Karnataka, reported 76% of patients with CNS symptoms which was similar to our study. A study by Rahil et al. showed CNS involvement in 24.5% of the patients with symptoms that ranged from confusion to coma.[9] Similarly, in our study, majority of the patients had altered sensorium, which was more common with severe hyponatremia than moderate hyponatremia.
In the present study, nearly half of the study population had a history of hypertension, and nearly one-third had a history of diabetes mellitus. Similar findings were reported in a study by Rao et al.[14] wherein hypertension and diabetes were the most common comorbid conditions in majority of the patients.[14] Hyponatremic hypertensive syndrome is a well-known entity wherein the most common association is in patients with essential hypertension receiving diuretics, which interfere with the metabolism of a variety of electrolytes and cause electrolyte imbalance. Thiazide diuretics influence the sodium chloride cotransporter channel and also result in the nonosmotic release of vasopressin.[3]
The CNS is the most commonly involved system as observed in the present study as well as other studies with varying symptoms including headache, nausea, vomiting, muscle cramps, restlessness, lethargy, depressed reflexes, and disorientation. These symptoms are noticeable with a rapid or greater decrease in the serum sodium concentration, i.e., occurring within a span of few hours. Severe and rapidly developing hyponatremia results in complications including seizures, coma, permanent brain damage, respiratory arrest, brainstem herniation, and eventually death.[15]
Based on the hydration status, half of the study population was euvolemic while one-third were hypervolemic followed by hypovolemic cases. Further, based on osmolality, most of the patients had euvolemic hypoosmolar hyponatremia, followed by hypervolemic hypoosmolar hyponatremia, hypovolemic hypoosmolar hyponatremia, and hypervolemic isoosmolar hyponatremia. A similar pattern was reported in a study by Rao et al. wherein euvolemia (61%) followed by fluid overload (23%) and dehydration (16%) was observed. Isovolemic hypoosmolar hyponatremia was the most frequently reported type of hyponatremia.[14]
In hypotonic hyponatremia, water enters the brain, resulting in cerebral edema. This leads to intracranial hypertension due to the confinement of the fluid within the cranium along with the risk of cranial injury. Eventually, the fluid leaves the brain tissues within hours, reducing fluid overload and swelling of the brain.[16,17] The feedback mechanism is efficient even in cases of asymptomatic nature of severe hyponatremia that develops slowly. Nevertheless, this adaptation also has the risk of osmotic demyelination.[18,19,20] Severe aggressive treatment of hyponatremia including water restriction alone can result in severe osmotic demyelination.[21,22,23] Shrinkage of the brain induces demyelination of pontine and extrapontine neurons, which may result in neurologic dysfunction, including quadriplegia, pseudobulbar palsy, seizures, coma, and even death. Hepatic failure, potassium depletion, and malnutrition increase the risk of this complication.[24]
Hyponatremia occurs either due to water retention or loss of effective solute (sodium plus potassium) in excess of water. The water excretion capacity is generally so high that the retention of water is usually due to the impaired renal excretion of water. An exception to this is primary polydipsia, wherein excessive water consumption can deteriorate even normal renal excretory capacity. Decreased secretion of the ADH – arginine vasopressin results in the effective excretion of any water load. Therefore, the presence of high-serum ADH concentrations is indicative of hyponatremia and helps in the development and maintenance of hyponatremia.
Virtually, an excess of ADH concentration, usually caused by the SIADH or depletion of effective circulating volume, is the main cause of hyponatremia.[3,6] In spite of being the most usual etiological factor for hyponatremia in hospitalized elderly patients[7] as well as the most common cause of normovolemic hyponatremia, SIADH is generally diagnosed by exclusion of other causes, including diuretics, renal, liver, thyroid, adrenal, and pituitary diseases.[8]
In the present study, SIADH was the most common cause of hyponatremia noted in nearly half of the study population. In a prospective study conducted in a general medical-surgical setting, 66 patients (34%) had euvolemic hyponatremia, 38 (19%) had hypervolemic hyponatremia associated with edematous disorders, and 33 (17%) had hypovolemic conditions, chiefly related to gastrointestinal fluid loss or diuretic use.[3] In a study by Rahil et al., extra-renal fluid loss, including vomiting, diarrhea, or diaphoresis was the most frequent cause of hyponatremia which was found in 33.9% of the patients. SIADH was considered to be the cause in 20.7% of the patients.[9] Laczi reported that SIADH was the most common cause of euvolemic hyponatremia in their study in Hungary.[25] Another study by Panicker and Joseph[26] on the clinical profile of hyponatremia in ICU hospitalized patients reported SIADH as a predominant cause for hyponatremia.[26]
In this study, we evaluated the cause of SIADH as treating the underlying etiology would prevent considerable morbidity and mortality. The main cause of SIADH was infections, of which TB was the leading infectious cause. Further, the profile of TB in patients with SIADH in decreasing order of occurrence was as follows: tubercular meningitis, pulmonary TB, miliary TB, and tuberculomas. Similarly, Vorherr et al. reported a case of pulmonary TB with hyponatremia and detected antidiuretics in tuberculous lung tissues.[27] Bryant implied SIADH as a cause in patients with infectious pulmonary disease such as pulmonary TB.[28] Cockcroft et al. reported severe hyponatremia caused by SIADH which led to miliary TB in a 74-year-old woman.[29] Similarly, Weiss and Katz reported hyponatremia resulting from SIADH in patients with pulmonary TB.[30] Later on, it was affirmed that an increased ADH level in the presence of hyponatremia in pulmonary TB cases is a marker of ectopic ADH production. Few studies demonstrated that the ADH level was not detectable following full anti-TB therapy.[31,32] More than 60% of the patients with TB may present with hyponatremia or SIADH as the first presentation.[33]
Another mechanism including endocrine system involvement in TB can also induce hyponatremia and is an important factor of consideration in patients with pulmonary TB. The adrenal glands are directly involved in TB,[17] which leads to overt or subclinical adrenal insufficiency and hyponatremia, along with the pituitary gland involvement.[2] Childhood tubercular meningitis can lead to hypopituitarism in 20% of the cases, years after effective treatment. The reason seemed to be tubercular lesions impressing the hypothalamus, pituitary stalk, and indirectly or directly, the pituitary gland itself.[5]
SIADH is a reversible condition in most of the cases, with effective pulmonary TB treatment.[33] Therefore, it should be carefully looked for by the treating physician as a cause of hyponatremia. Furthermore, patients who were affected by hyponatremia were more likely to have higher mortality as suggested in a study by Sharma et al.[34] In the present study, majority of the patients had an improved outcome and mortality was noted in few of the patients. These finding are consistent with another study conducted by Joseph and Panicker where mortality was noted in 7% of patients.
CONCLUSION
Based on the findings of this study, it may be concluded that hyponatremia can present with protean clinical manifestations. The presentation can vary from mild symptoms such as vomiting, lethargy, and malaise to severe forms such as confusion, seizure, and coma. Majority of patients report CNS symptoms and these patients are likely to have euvolemic hypoosmolar hyponatremia with SIADH as the predominant cause. The severity of hyponatremia is independent of age, sex and type of hyponatremia, as it is the rapidity with which hyponatremia develops that decides the clinical presentation and not just the levels of serum sodium. The most common etiology of hyponatremia in the present study was SIADH. Furthermore, it was observed that patients with SIADH having infectious etiologies, especially TB, are more likely to develop hyponatremia.
Clinicians need to be aware about the common occurrence of hyponatremia, its early identification, and its association with a large variety of diseases. In developing nations, like India, TB is still a common health hazard, remains latent, and can often present only as symptomatic hyponatremia. TB can induce hyponatremia in several ways such as local invasion of adrenal glands or pituitary gland, tubercular meningitis, and SIADH (via pulmonary infection). Therefore, evaluating for the cause of hyponatremia is equally important, as treating the underlying cause would prevent considerable morbidity and mortality associated with this enigmatic electrolyte disorder. Thus, the treating physician should have a high degree of suspicion for TB as a cause of hyponatremia, as our study found TB as the most common infectious cause of SIADH.
Thus, to conclude, a thorough understanding of the pathophysiological process of hyponatremia and its associated risk factors is of great importance in prompt and effective treatment of this potentially life-threatening condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fried LF, Palevsky PM. Hyponatremia and hypernatremia. Med Clin North Am. 1997;81:585–609. doi: 10.1016/s0025-7125(05)70535-6. [DOI] [PubMed] [Google Scholar]
- 2.Fall PJ. Hyponatremia and hypernatremia. A systematic approach to causes and their correction. Postgrad Med. 2000;107:75–82. doi: 10.3810/pgm.2000.5.1.1068. [DOI] [PubMed] [Google Scholar]
- 3.Freda BJ, Davidson MB, Hall PM. Evaluation of hyponatremia: A little physiology goes a long way. Cleve Clin J Med. 2004;71:639–50. doi: 10.3949/ccjm.71.8.639. [DOI] [PubMed] [Google Scholar]
- 4.Han DS, Cho BS. Therapeutic approach to hyponatremia. Nephron. 2002;92(Suppl 1):9–13. doi: 10.1159/000065371. [DOI] [PubMed] [Google Scholar]
- 5.Pham PC, Pham PM, Pham PT. Vasopressin excess and hyponatremia. Am J Kidney Dis. 2006;47:727–37. doi: 10.1053/j.ajkd.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 6.Lindner G, Schwarz C. An update on the current management of hyponatremia. Minerva Med. 2012;103:279–91. [PubMed] [Google Scholar]
- 7.Pillai BP, Unnikrishnan AG, Pavithran PV. Syndrome of inappropriate antidiuretic hormone secretion: Revisiting a classical endocrine disorder. Indian J Endocrinol Metab. 2011;15(Suppl 3):S208–15. doi: 10.4103/2230-8210.84870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marupudi NI, Mittal S. Diagnosis and management of hyponatremia in patients with aneurysmal subarachnoid hemorrhage. J Clin Med. 2015;4:756–67. doi: 10.3390/jcm4040756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rahil AI, Khan FY. Clinical profile of hyponatraemia in adult patients admitted to Hamad General Hospital, Qatar: Experience with 53 Cases. J Clin Diag Res. 2009;3:1419–25. [Google Scholar]
- 10.Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000;342:1581–9. doi: 10.1056/NEJM200005253422107. [DOI] [PubMed] [Google Scholar]
- 11.Chowdhury R, Samanta T, Pan K, Sarkar A, Chakrabarti S. Can hyponatraemia predict mortality in Intensive Care Unit patients: A prospective study in a tertiary care hospital of Kolkata. Int J Med Pharm Sci. 2013;3:26–30. [Google Scholar]
- 12.Boscoe A, Paramore C, Verbalis JG. Cost of illness of hyponatremia in the United States. Cost Eff Resour Alloc. 2006;4:10. doi: 10.1186/1478-7547-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patni M, Humaney N, Jeswani J, Deoke S. Clinico-etiological profile of hyponatremia in patients admitted in Intensive Care Unit of tertiary health care rural center. JMSCR. 2015;3:6975–82. [Google Scholar]
- 14.Rao MY, Sudhir U, Anil Kumar T, Saravanan S, Mahesh E, Punith K, et al. Hospital-based descriptive study of symptomatic hyponatremia in elderly patients. J Assoc Physicians India. 2010;58:667–9. [PubMed] [Google Scholar]
- 15.Vandergheynst F, Sakr Y, Felleiter P, Hering R, Groeneveld J, Vanhems P, et al. Incidence and prognosis of dysnatraemia in critically ill patients: Analysis of a large prevalence study. Eur J Clin Invest. 2013;43:933–48. doi: 10.1111/eci.12123. [DOI] [PubMed] [Google Scholar]
- 16.Sherlock M, O’Sullivan E, Agha A, Behan LA, Rawluk D, Brennan P, et al. The incidence and pathophysiology of hyponatraemia after subarachnoid haemorrhage. Clin Endocrinol (Oxf) 2006;64:250–4. doi: 10.1111/j.1365-2265.2006.02432.x. [DOI] [PubMed] [Google Scholar]
- 17.Mulloy AL, Caruana RJ. Hyponatremic emergencies. Med Clin North Am. 1995;79:155–68. doi: 10.1016/s0025-7125(16)30089-x. [DOI] [PubMed] [Google Scholar]
- 18.Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med. 2009;122:857–65. doi: 10.1016/j.amjmed.2009.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chitsazian Z, Zamani B, Mohagheghfar M. Prevalence of hyponatremia in Intensive Care Unit patients with brain injury in Kashan Shahid-Beheshti hospital in 2012. Arch Trauma Res. 2013;2:91–4. doi: 10.5812/atr.9877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chatterjee N, Sengupta N, Das C, Chowdhuri AR, Basu AK, Pal SK, et al. A descriptive study of hyponatremia in a tertiary care hospital of Eastern India. Indian J Endocrinol Metab. 2012;16:288–91. doi: 10.4103/2230-8210.93757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agarwal SM, Agrawal A. A comparative study of the clinico-aetiological profile of hyponatremia at presentation with that developing in the hospital. Indian J Med Res. 2011;134:118–22. [PMC free article] [PubMed] [Google Scholar]
- 22.Miyashita J, Shimada T, Hunter AJ, Kamiya T. Impact of hyponatremia and the syndrome of inappropriate antidiuresis on mortality in elderly patients with aspiration pneumonia. J Hosp Med. 2012;7:464–9. doi: 10.1002/jhm.1936. [DOI] [PubMed] [Google Scholar]
- 23.Vurgese TA, Radhakrishan SB, Mapkar OA. Frequency and etiology of hyponatremia in adult hospitalized patients in medical wards of a general hospital in Kuwait. Kuwait Med J. 2006;38:211–3. [Google Scholar]
- 24.Padhi R, Panda BN, Jagati S, Patra SC. Hyponatremia in critically ill patients. Indian J Crit Care Med. 2014;18:83–7. doi: 10.4103/0972-5229.126077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laczi F. Etiology, diagnostics and therapy of hyponatremias. Orv Hetil. 2008;149:1347–54. doi: 10.1556/OH.2008.28409. [DOI] [PubMed] [Google Scholar]
- 26.Panicker GI, Joseph S. A prospective study on clinical profile of hyponatremia in ICU hospitalized patients. Int J Biomed Adv Res. 2014;5:297–303. [Google Scholar]
- 27.Vorherr H, Massry SG, Fallet R, Kaplan L, Kleeman CR. Antidiuretic principle in tuberculous lung tissue of a patient with pulmonary tuberculosis and hyponatremia. Ann Intern Med. 1970;72:383–7. doi: 10.7326/0003-4819-72-3-383. [DOI] [PubMed] [Google Scholar]
- 28.Bryant DH. The syndrome of inappropriate secretion of antidiuretic hormone in infectious pulmonary disease. Med J Aust. 1972;1:1285–8. doi: 10.5694/j.1326-5377.1972.tb116493.x. [DOI] [PubMed] [Google Scholar]
- 29.Cockcroft DW, Donevan RE, Copland GM, Ibbott JW. Miliary tuberculosis presenting with hyponatremia and thrombocytopenia. Can Med Assoc J. 1976;115:871–3. [PMC free article] [PubMed] [Google Scholar]
- 30.Weiss H, Katz S. Hyponatremia resulting from apparently inappropriate secretion of antidiuretic hormone in patients with pulmonary tuberculosis. Am Rev Respir Dis. 1965;92:609–16. doi: 10.1164/arrd.1965.92.4.609. [DOI] [PubMed] [Google Scholar]
- 31.Merrill C, Elixhauser A. Hospitalization in the United States, 2002: HCUP Fact Book no. 6. AHRQ Publication no. 05-0056, June 2005. Rockville, MD: Agency for Healthcare Research and Quality; 2005. Jun, [Google Scholar]
- 32.Thurman JM, Berl T. Therapy in Nephrology and Hypertension, a Companion to Brenner & Rector's the Kidney. Therapy of dysnatremic disorders. 3rd ed. Philadelphia: Saunders; 2008. pp. 337–52. [Google Scholar]
- 33.Liamis G, Kalogirou M, Saugos V, Elisaf M. Therapeutic approach in patients with dysnatraemias. Nephrol Dial Transplant. 2006;21:1564–9. doi: 10.1093/ndt/gfk090. [DOI] [PubMed] [Google Scholar]
- 34.Sharma SK, Mohan A, Banga A, Saha PK, Guntupalli KK. Predictors of development and outcome in patients with acute respiratory distress syndrome due to tuberculosis. Int J Tuberc Lung Dis. 2006;10:429–35. [PubMed] [Google Scholar]


