Abstract
Background
We investigated whether a public health intervention—a three-part documentary called Man Up which explored the relationship between masculinity and mental health, well-being and suicidality—could increase men’s intentions to seek help for personal and emotional problems.
Methods
We recruited men aged 18 years or over who were not at risk of suicide to participate in a double-blind randomised controlled trial. Participants were randomly assigned (1:1) via computer randomisation to view Man Up (the intervention) or a control documentary. We hypothesised that 4 weeks after viewing Man Up participants would report higher levels of intention to seek help than those who viewed the control documentary. Our primary outcome was assessed using the General Help Seeking Questionnaire, and was analysed for all participants. The trial was registered with the Australian New Zealand Clinical Trials Registry (ACTRN12616001169437, Universal Trial Number: U1111-1186-1459) and was funded by the Movember Foundation.
Results
Three hundred and fifty-four men were assessed for eligibility for the trial and randomised to view Man Up or the control documentary. Of these, 337 completed all stages (nine participants were lost to follow-up in the intervention group and eight in the control group). Linear regression analysis showed a significant increase in intentions to seek help in the intervention group, but not in the control group (coef.=2.06, 95% CI 0.48 to 3.63, P=0.01).
Conclusions
Our trial demonstrates the potential for men’s health outcomes to be positively impacted by novel, media-based public health interventions that focus on traditional masculinity.
Trial registration number
ACTRN12616001169437, Results.
Keywords: mental health, randomised trials, public health
Introduction
Mental health problems are common in men, with 18% of Australian males aged over 16 years experiencing mood disorders, anxiety disorders and/or substance use disorders in a given year.1 Of particular concern is the high rate of suicide among Australian men. In 2015, 3027 people in Australia died by suicide, of whom 2292 (75.7%) were men (equating to a rate of 19.4/100 000 men).2 Many theories have been put forward to explain these excess deaths in men, one of which is that conformity to traditional masculine norms may result in men being disinclined to reach out for help if they are facing tough times.3 Masculine norms are the script by which society tells men to live their life.4 These norms vary across time, places and groups, but in Australia the ‘dominant masculinity’ is one that endorses the norms of stoicism, independence, invulnerability and avoidance of negative emotions.5–7 Conformity to traditional masculine norms, and in particular the norm of self-reliance, has been shown to be associated with suicidal thinking.8 It has also been found to be related to poor mental health and other outcomes that may be precursors to suicidality, including alcohol and substance use, and reduced and delayed help-seeking.7–16 Men’s help-seeking behaviour has been cited as a key target for improving men’s health.13
If conformity to masculine norms confers risk for men’s mental health then interventions that address this risk may be beneficial. There is evidence from other areas that interventions that focus on masculine norms can bring about positive outcomes (eg, in promoting sexually protective behaviours, preventing violence and changing attitudes towards gender norms).17 As yet, however, little is known about equivalent interventions that focus on outcomes relating to help-seeking and mental health, or about how masculine norms might be targeted to improve these outcomes.7
We were funded by the Movember Foundation to develop and test one such public health intervention. We collaborated with Heiress Films to produce a documentary called Man Up. Man Up examined how society shapes the way men and boys see themselves and the way in which they act, and explored the way in which this might affect their mental health and, potentially, lead to thoughts of death as an escape. It was aired by the Australian Broadcasting Corporation (ABC), Australia’s national public free-to-air broadcaster, in October 2016. The screening was preceded and accompanied by a broader media campaign across social media, newsprint and radio that aimed to promote Man Up and create public discussion around the key ideas.
Before Man Up went to air, we conducted a randomised controlled trial to test its impact on men. We were guided by the theory of planned behaviour that proposes that attitudes towards behaviour, perceived behavioural control and subjective norms play a key role in behavioural intentions.18 Subjective norms in this case refer to the perceived social pressure to perform or not perform a certain behaviour. As previously described, masculine social norms act to encourage self-reliance and dissuade men from help-seeking. We were interested to see whether the Man Up intervention, with its focus on changing masculine social norms and increasing positive attitudes and perceived behavioural control related to help-seeking, could bring about a change in help-seeking intentions, as measured by our primary outcome measure: the General Help Seeking Questionnaire. We were also interested in a range of secondary outcomes including the degree to which men conformed to masculine norms, and other variables that might influence men’s perceived behavioural control including well-being, social support and resilience.
The trial was the centrepiece of a broader evaluation which also included an analysis of traffic to the Man Up website, engagement with social media platforms and a survey of those who had engaged with Man Up. We are also planning to conduct a before-and-after study that tracks the impact of Man Up in the community, capitalising on two consecutive waves of data from Ten to Men, the Australian Longitudinal Study on Male Health (http://www.tentomen.org.au). The findings of these other evaluation activities will be reported elsewhere.
Methods
Expert insight
An expert Advisory Group, comprising individuals with expertise in men’s health such as representatives from men’s focused community and service organisations and expert consultants, was convened to provide input into the design of the documentary and trial.
Participants
Recruitment began in January 2016. We recruited participants through a variety of avenues. We sent advertisements to the trial Advisory Group and asked members to distribute them through their networks. We also distributed advertisements via email to university staff and students, and placed advertisements on university noticeboards and in local newspapers, retail stores, sporting clubs, local school parent newsletters and local community ‘buy, swap, sell’ Facebook pages.
To be eligible to take part in the trial, participants had to be male and aged 18 years or more. Gender and age were self-reported. Men with mental health concerns or suicidal thoughts were not excluded from the study. However, men who were at active risk of suicide were ineligible to take part in the trial in order to minimise any potential unforeseen harm. Risk of suicide was assessed at baseline via the use of the Adult Suicide Ideation Questionnaire (ASIQ).19 Any participant who scored over the ASIQ’s critical threshold (as identified in the scale manual) at baseline met with one of our psychologists who assessed whether he should be excluded from participation (if he was at active risk of suicide or likely to be further harmed by his participation in the trial); continue in the trial with telephone support from the psychologist or continue in the trial without telephone support.
Randomisation and masking
We conducted a double-blind randomised controlled trial. All of the members of our research team and all participants were blind to the allocation of participants to the intervention and control groups throughout the trial, and the blinding was broken only at the conclusion of the analysis. Participants were informed that they would view one of two documentaries, but not that one of them was the intervention and the other was the control condition. Participants were randomly allocated (1:1 allocation) to the intervention or control arm of the trial after baseline data collection, via an automated randomisation process.
Procedures
Participants attended a group meeting with our research team where they were enrolled in the trial. Each participant completed the baseline questionnaire on an individually held iPad and received a AUD$50 retail store voucher for completing this stage. Baseline assessment occurred between 30 May and 27 August 2016. Forty-seven meetings were undertaken: 38 at the University of Melbourne and 9 in outer suburban and regional Victorian locations.
Participants were then given an individual login and asked to access their allocated documentary online at a time and place of their choosing over the following week, either alone, or if that was not practical, with immediate family/household members. Immediately after viewing, participants were asked to complete a postviewing questionnaire online. Participants received another AUD$50 retail store voucher for completing this stage. Participants viewed the documentaries between 30 May and 22 July 2016.
Four weeks after viewing the documentary participants were emailed a link to complete a follow-up questionnaire. They were given 2 weeks to do this. They received a AUD$100 retail store voucher for completing this stage. Participants completed the follow-up questionnaire between 30 June and 27 August 2016.
Intervention and control conditions
The intervention group viewed Man Up. Man Up was a three-part documentary (each part 1 hour) that examined the link between masculinity and men’s mental health and well-being in Australia, and how this might sometimes lead to suicidal thoughts and behaviours. The documentary was presented by Gus Worland, a Sydney radio and television personality. It featured men from all walks of life modelling positive health behaviours such as talking about personal problems, expressing emotions and seeking help. The link between masculinity and help-seeking was explicitly addressed in Man Up. The presenter talked to men who had experienced mental health problems and/or made suicide attempts, and a consistent theme that emerged was that ‘being a man’ and reaching out to formal or informal sources of help are often viewed as mutually exclusive. Importantly, many of the people Worland spoke to provided real-life examples of how reaching out for help had changed their trajectory for the better. Worland also spoke with mental health professionals and men’s health experts who reinforced the messages of the ‘men on the street’. His visit to Lifeline Australia demystified how these sorts of services operate.
The control group viewed a National Geographic documentary called Test Your Brain. 20 This documentary was chosen because it had a similar format to the intervention documentary (3×1 hours), but did not focus on any of the areas of interest in the trial. Instead, it focused on the inner workings of the brain and revealed new discoveries about attention, sensory perception and memory through interactive experiments.
Measures
A number of measures were administered to participants throughout the trial. Standardised measures yielding quantitative responses included: the General Help Seeking Questionnaire (GHSQ); the Conformity to Masculine Norms Inventory (CMNI-22); the Gender Role Conflict Scale Short Form (GRCS-SF); the MOS Social Support Survey; the Personal Well-Being Index-Adult; the Connor Davidson Resilience Scale and ASIQ.19 21–26 In addition, we asked participants purpose-designed questions related to demographics, content knowledge of the documentary (ie, engagement with the documentary), immediate impressions postviewing and impact on participants at follow-up. Table 1 describes each measure in more detail as well as the timing of administration.
Table 1.
Measures used in each stage of the trial
| Measure | Example items | Scoring | Baseline | Postviewing | Follow-up | |
| Primary outcome | ||||||
| Likelihood of seeking help | General Help Seeking Questionnaire (GHSQ-Self) |
If you were having a personal or emotional problem, how likely is it that you would seek help from the following people or services? Including: intimate partner, friend or doctor. Plus three purpose-designed responses: online health chat rooms, online searches for health information and social media | 10 items. 1 (extremely unlikely) to 7 (extremely likely). Total score used for analysis | ✓ | ✓ | |
| Secondary outcomes | ||||||
| Likelihood of recommending a male or female friend seek help | General Help Seeking Questionnaire-Modified. (GHSQ-male friend, GHSQ-female friend) | How likely is it that you would recommend a male/female friend seek help from the following people or services? | 10 items. 1 (extremely unlikely) to 7 (extremely likely). Total score used for analysis | ✓ | ✓ | |
| Conformity to masculine norms | Conformity to Masculine Norms Inventory 22 | My work is the most important part of my life. I like to talk about my feelings. | 22 items. 0 (strongly disagree) to 3 (strongly agree). Total score used for analysis. | ✓ | ✓ | |
| Experience of masculinity | Gender Role Conflict Scale-Short Form | Affection with other men makes me feel tense. My work or school often disrupts other parts of my life. | 16 items. 1 (strongly disagree) to 6 (strongly agree). Total score used for analysis. | ✓ | ✓ | |
| Social support | MOS Social Support Survey 100 | How often is each of the following kinds of support available to you?’ Including: Someone to give you good advice in a crisis. Someone who shows you love and affection. | 19 items. 1 (none of the time) to 5 (all of the time). Total score was transformed to a 0–100 scale for analysis. | ✓ | ✓ | |
| Psychological distress | Kessler-10 scale | In the last 30 days: , About how often did you feel nervous? About how often did you feel worthless? | 10 items. 1 (none of the time) to 5 (all of the time). Total score used for analysis. | ✓ | ✓ | |
| Well-being | Personal Well-Being Index-Adult | How satisfied are you with…living, health, achieving in life, relationships, safety, community connectedness and future security. | 7 items. 0 (no satisfaction at all) to 10 (completely satisfied). Total score was averaged to yield a score out of 100 | ✓ | ✓ | |
| Resilience | Connor Davidson Resilience Scale 10 | I am able to adapt when changes occur. Under pressure, I stay focused and think clearly. | 10 items. 0 (not true at all) to 4 (true nearly all the time). Total score used for analysis. | ✓ | ✓ | |
| Suicidality | Adult Suicide Ideation Questionnaire | I thought it be better if I was not alive. I thought about the ways people kill themselves. | 25 items. 0 (I never had this thought) to 2 (almost every day). Total score was used for analysis. | ✓ | ✓ | |
| Purpose designed | ||||||
| Demographics | Purpose designed demographic questions | Age, gender, postcode, country of birth, language spoken, Aboriginal or Torres Strait Islander origin, sexual orientation, marital status, education, employment status. | 11 items. Individually analysed. | ✓ | ||
| Content knowledge of the documentary | Purpose designed test questions | In Episode 1, which workplace did Gus visit? (intervention). In Episode 1, which city did they visit? (control). | six multiple-choice items. Individually analysed. | ✓ | ||
| Immediate impressions postviewing | Purpose designed postviewing questions | How much did you enjoy the documentary? Do you think the documentary will have a positive (or negative) impact on men? | 13 closed and open ended items. Individually analysed. | ✓ | ||
| Impact at follow-up | Purpose designed follow-up questions | Do you think the documentary will have a positive (or negative) impact on men? Did the documentary trigger any changes for the better (or worse) in you? Did you change your attitudes or behaviours in any of the following ways? | 18 closed and open-ended items. Individually analysed. | ✓ | ||
Changes to trial outcomes
There were no changes to the trial outcomes after recruitment had commenced.
Sample size
Our sample size calculations assumed a correlation of 0.45 between baseline and follow-up measurements, 90% power and a 5% significance level. To detect a moderate difference between the groups (Cohen’s D=0.3), we required an initial sample size of 131 per group. We assumed a drop-out rate of 25% so our target sample size was approximately 165 per group.
Analysis
We conducted an intention-to-treat analysis. To test the effectiveness of the intervention, we used a linear regression model where the primary outcome variable was the difference between follow-up and baseline GHSQ scores and the predictor variables were an indicator variable representing treatment group and a variable representing baseline GHSQ scores. We undertook a similar analysis for the secondary outcomes. For all outcome measures, we report effect sizes on their original metric and as a standardised mean difference (SMD).
The dates that each participant completed each stage of the trial (baseline, post-viewing, follow-up) were automatically recorded. Participants’ engagement with the documentary was assessed via six ‘test questions’ (two per episode). We used basic descriptive analysis to assess participants’ adherence to the requirements of the trial protocol (ie, watching the documentary within 1 week of baseline and completing the follow-up questionnaire within 2 weeks of receiving it).
The data provided by participants at baseline and follow-up related to the primary and secondary outcomes are the foci of this paper. Findings related to the qualitative data supplied by participants will be described in a separate paper.
Results
Trial sample
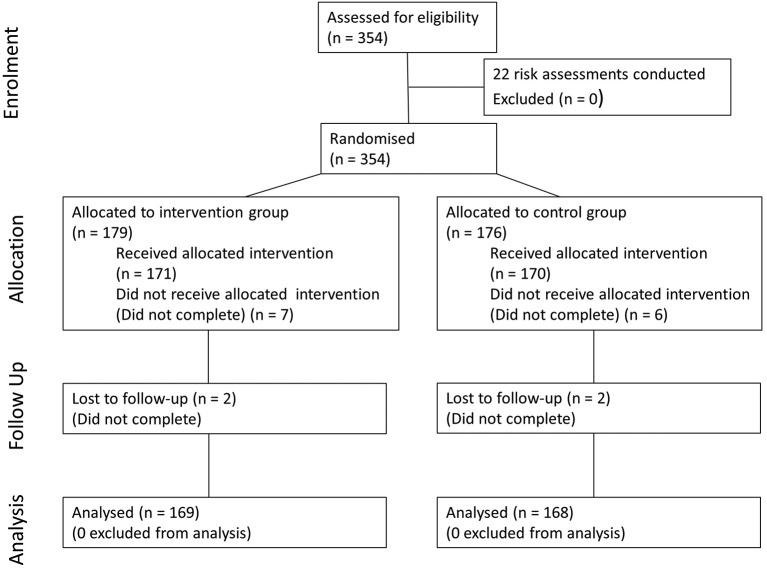
Figure 1 shows the progress of participants through the trial. Twenty-two participants (6%) were assessed for exclusion based on their suicide risk by the trial psychologist after scoring above the critical threshold on the ASIQ, but none was excluded. Ultimately, 169 participants in the intervention group and 168 in the control group were included in the primary and secondary analyses.
Figure 1.
Flow diagram of participant progress through the phases of the trial.
Table 2 shows the demographic characteristics of participants. Participants in each group appeared to be evenly matched on the variables examined.
Table 2.
Demographic characteristics of participants
| Intervention (n=169) |
Control (n=168) |
|
| Mean age (years) | 38.8 (SD12.7) | 38.8 (SD 14.4) |
| Country of birth | ||
| Australia | 117 (69.2%) | 113 (67.3%) |
| Other | 52 (30.8%) | 55 (32.7%) |
| Language spoken at home | ||
| English | 147 (87.0%) | 140 (83.3%) |
| Other | 22 (13.0%) | 28 (16.7%) |
| Aboriginal or Torres Strait Islander | ||
| Neither | 167 (98.8%) | 165 (98.2%) |
| Aboriginal | 1 (0.6%) | 1 (0.6%) |
| Torres Strait Islander | 0 (0.0%) | 0 (0.0%) |
| Prefer not to answer | 1 (0.6%) | 2 (1.2%) |
| Sexuality | ||
| Heterosexual/straight | 151 (89.3%) | 140 (83.3%) |
| Bisexual | 2 (1.2%) | 7 (4.2%) |
| Homosexual/gay | 14 (8.3%) | 18 (10.7%) |
| Not sure | 1 (0.6%) | 1 (0.6%) |
| Other | 0 (0.0%) | 1 (0.6%) |
| Prefer not to say | 1 (0.6%) | 1 (0.6%) |
| Marital status | ||
| Married/de facto | 95 (56.2%) | 96 (57.1%) |
| Never married | 64 (37.9%) | 65 (38.7%) |
| Divorced/separated | 8 (4.7%) | 6 (3.6%) |
| Widowed | 1 (0.6%) | 1 (0.6%) |
| Prefer not to answer | 1 (0.6%) | 0 (0.0%) |
| Studying | ||
| No | 126 (74.6%) | 109 (64.9%) |
| Full-time student | 32 (18.9%) | 45 (26.8%) |
| Part-time student | 11 (6.5%) | 14 (8.3%) |
| Education | ||
| Year 11 or less | 12 (7.1%) | 13 (7.8%) |
| Year 12 or equivalent | 157 (92.9%) | 155 (92.3%) |
| Certificate/undergraduate diploma | 33 (19.4%) | 23 (14.2%) |
| Bachelor degree | 56 (33.1%) | 58 (34.5%) |
| Postgraduate qualification | 52 (30.8%) | 52 (31.0%) |
| Doctorate/PhD | 12 (7.1%) | 13 (7.7%) |
| Employment | ||
| Employed | 123 (72.8%) | 118 (70.2%) |
| Unemployed and looking for work | 17 (10.1%) | 23 (13.7%) |
| Neither working nor looking for work | 29 (17.2%) | 27 (16.1%) |
Primary and secondary outcomes analyses
Table 3 shows the mean scores on the primary outcome and each of the secondary outcomes for the intervention and control groups at baseline and follow-up, and results of the linear regression analyses.
Table 3.
Results of the linear regressions*
| Intervention (n=169) | Control (n=168) | Linear Regression | ||||||||
| Baseline Mean (SD) |
Follow-up Mean(SD) |
Mean difference | Baseline Mean (SD) |
Follow-up Mean (SD) |
Mean difference | Coef. | 95% CI | P | SMD† | |
| Primary outcome | ||||||||||
| GHSQ-Self | 44.64 (10.03) | 47.53 (10.80) | 2.89 | 43.89 (9.37) | 44.96 (8.90) | 1.07 | 2.06 | 0.48 to 3.63 | 0.011 | 0.13 |
| Secondary outcomes | ||||||||||
| GHSQ-male friend | 50.12 (10.83) | 52.72 (11.07) | 2.60 | 49.67 (10.03) | 49.76 (10.48) | 0.10 | 2.66 | 0.88 to 4.44 | 0.004 | 0.15 |
| GHSQ-female friend | 51.12 (10.69) | 52.83 (11.24) | 1.71 | 50.82 (10.03) | 50.60 (10.49) | −0.22 | 2.05 | 0.28 to 3.82 | 0.023 | 0.12 |
| CMNI | 26.25 (6.23) | 25.56 (5.79) | −0.69 | 26.41 (5.72) | 26.76 (5.65) | 0.35 | −1.07 | −1.78 to −0.36 | 0.003 | −0.15 |
| GRCS-SF | 47.46 (12.46) | 47.11 (11.77) | −0.36 | 48.73 (11.05) | 48.43 (10.93) | −0.30 | −0.35 | −1.83 to 1.12 | 0.639 | −0.02 |
| PWI-A | 67.79 (16.03) | 66.92 (16.10) | −0.87 | 67.68 (14.91) | 66.26 (16.85) | −1.42 | 0.56 | −1.42 to 2.54 | 0.577 | 0.03 |
| K10 | 20.03 (6.03) | 18.76 (6.04) | −1.27 | 20.17 (6.70) | 19.48 (6.55) | −0.70 | −0.61 | −1.47 to 0.25 | 0.165 | −0.07 |
| CD-RISC-10 | 28.55 (5.81)* | 28.00 (6.18)* | −0.55 | 28.95 (6.11) | 28.07 (5.78) | −0.88 | 0.25 | −0.55 to 1.05 | 0.543 | 0.03 |
| MOS100 | 73.12 (19.31) | 72.51 (19.21) | −0.61 | 74.91 (17.54) | 74.30 (19.43) | −0.61 | −0.20 | −2.39 to2.00 | 0.860 | −0.01 |
| ASIQ | 12.75 (13.11) | 13.46 (13.93) | 0.74 | 12.40 (17.26) | 12.20 (16.39) | −0.20 | 1.03 | −1.39 to 3.44 | 0.405 | 0.04 |
*The outcome is the difference between follow-up and baseline scores, with an indicator variable for treatment arm and controlling for baseline scores. **n=168.
†Standardised mean difference.
ASIQ, Adult Suicide Ideation Questionnaire; CD-RISC-10, Connor Davidson Resilience Scale 10; CMNI, Conformity to Masculine Norms Index; GHSQ-female friend, General Help Seeking Questionnaire (female friend); GHSQ-male friend, General Help Seeking Questionnaire (male friend); GHSQ-Self, General Help Seeking Questionnaire (self); GRCS-SF, Gender Role Conflict Scale-Short Form; K10, Kessler 10; MOS100, Mos Social Support Survey (0–100 score); PWI-A, Personal Well-Being Index-Adult (index score).
For the primary outcome, in the intervention group the difference between follow-up and baseline scores on the GHSQ-self was 2.89. For the control group, the difference was 1.07. In linear regression analysis, this difference was significant and favoured the intervention (coef.=2.06, 95% CI 0.48 to 3.63, P=0.011). This translated to an SMD of 0.13 between the intervention and control group.
For the secondary outcomes, differences between the intervention and control groups were observed for three of the nine outcomes. These were increases in both the GHSQ-male friend scores (coef.=2.66, 95% CI 0.88 to 4.44, P=0.004, SMD=0.15) and GHSQ-female friend scores (coef.=2.05, 95% CI 0.28 to 3.82, P=0.023, SMD=0.12), and a decrease in the CMNI scores (coef.=−1.07, 95% CI −1.78 to −0.36, P=0.003, SMD=−0.15).
Trial protocol adherence analyses
Analysis of time elapsed between the baseline, postviewing and follow-up stages for each participant demonstrated that 81% of participants viewed the documentary within 1 week of completing the baseline assessment as requested, and 92% of participants completed the follow-up survey within the requested 2 weeks of viewing the documentary. In addition, almost all participants were able to answer the six test questions correctly (intervention range=86.5% to 98.2%, control range=95.3% to 100.0%).
Discussion
Men who viewed Man Up in our trial demonstrated significant changes in attitudes. After viewing the documentary, they indicated that they were more likely to seek help if they were facing difficulties and more likely to recommend that a friend do the same. They also demonstrated a shift in their conformity to traditional masculine norms. The fact that men who viewed our control documentary showed no such changes leads us to conclude that Man Up was responsible for these positive outcomes.
These findings are perhaps all the more remarkable because of the scalability of Man Up as an intervention. When Man Up was first aired, it was viewed by an average of 6 42 000 viewers for each of its three episodes (on the ABC free-to-air and internet catch-up television). It was recently rescreened on the ABC, and is still available online (eg, on ABC internet television, and on the Man Up website, which was originally a stand-alone site and is now hosted by the Movember Foundation), so the above figure is clearly an underestimate of the documentary’s reach. While the effects noted in the trial were arguably small, the social media campaign that surrounded the documentary has further worked to amplify these effects by engaging viewers and non-viewers in discussions around the key messages of Man Up and will continue to do so.
The relationship between masculinity and poor mental health and heightened risk of suicide is obviously a complex one. The mechanisms by which masculine norms such as self-reliance may impact on these sorts of outcomes have been discussed elsewhere.8 10 Help-seeking may be implicated here. Men who are self-reliant may view reaching out to others as a sign of weakness and may therefore be disinclined to seek help if they are facing tough times. This in turn may mean that these men have reduced opportunities for talking through their problems and learning strategies to deal with them. The findings of the trial indicate that the Man Up intervention led to an improvement in intentions to seek help scores. Based on the available evidence this could translate into improved well-being over time.13
It is worth commenting here on the remaining secondary outcomes. We did not find any association between viewing Man Up and these, most of which were direct measures of mental health, well-being and suicidality. Arguably, these outcomes may have been too distal, and less likely to be impacted on in the short term. Taking a programme logic approach and using the above argument about help-seeking acting as one of the mechanisms by which masculinity may affect these more distal outcomes, it is possible to see that shifting a proximal outcome such as intentions of reaching out for help might ultimately translate into improved mental health and well-being and reduced levels of suicidality in the longer term. It is also interesting to note that while changes were observed in the CMNI, there were no changes in the GRCS. The CMNI purports to measure conformity to masculine gender role norms, while the GRCS measures conflict and stress, or the pathology associated with masculinity.22 Perhaps what is observed in the trial is a reduction in conformity to masculine norms, rather than reductions in the conflict and stress associated with masculinity.
Other documentaries around the world have explored the link between masculinity and well-being (such as ‘The Mask You Live In’). It is possible that these too have had a significant impact on the way in which men and boys view themselves, and on their attitudes towards seeking help, but none has been as rigorously evaluated as Man Up. The evaluation evidence that we present here has implications for other media-based interventions that might be used as part of a public health approach to address mental health issues and suicidal thoughts and behaviours in men.
While the trial had a number of strengths, the following limitations should be acknowledged. The online viewing conditions of the trial provided a ‘real-world’ experience and increased the generalisability of our findings. However, we acknowledge that other people may have influenced participants. The sample was also relatively well educated and students were over-represented, which somewhat limits the generalisability of our findings.27 We acknowledge also that we lost some participants to follow-up, however this number was minimal and was evenly spread across the two arms of the trial (n=17 (4.8%), nine intervention, eight control).
Conclusion
One of the stand-out risk factors for poor mental health and well-being and heightened levels of suicidality in men is conformity to traditional masculine norms, and one of the mechanisms through which this relationship might operate is by men feeling that seeking help is a sign of weakness. We took a public health approach to addressing masculinity as a risk factor, creating a documentary that explored the relationship in a manner that was both scientific and engaging. Our trial of the documentary, conducted before it went to air, indicated that it was successful in increasing the intentions of men to seek help if they were facing emotional problems and would encourage their male and female friends to do the same. It also had the effect of shifting men’s views of masculinity. When Man Up was aired its reach was considerable, which suggests that as an intervention it may have had a major impact on societal attitudes. These findings suggest that documentaries and other media-based interventions have huge potential in the suite of interventions designed to improve men’s mental health and well-being and reduce their high suicide rate.
What is already known on this subject.
There is a need for interventions that work to improve men’s mental health and well-being and reduce their levels of suicidality. A public health approach would suggest that addressing risk factors for poor mental health and heightened suicidality in men might reap benefits. Conformity to masculine norms has been shown to be a risk factor for both poor mental health and suicidal thinking, and it has been suggested that elements of masculinity—such as self-reliance—may reduce men’s likelihood of seeking help for personal and emotional problems.
What this study adds.
This trial showed that a documentary focusing on masculinity, mental health and well-being and suicidality could bring about positive changes in men’s intentions to seek help. The findings point to the value of using media-based population health interventions to bring about positive attitudinal change, particularly for groups which may be hard to reach by other means.
Acknowledgments
The authors would like to thank the Movember Foundation for supporting the development and evaluation of Man Up. They would also like to thank Heiress Films for producing the documentary and associated social media campaign, and the Australian Broadcasting Corporation for screening the documentary. The authors are grateful to the Advisory Group that provided guidance at various critical stages in the project. They would also like to acknowledge Gus Worland and everyone else who appeared in the documentary, and the men who took part in the randomised controlled trial that examined its impact.
Footnotes
Contributors: KK was responsible for the day-to-day implementation of the randomised controlled trial (RCT) and had input into each stage of study design, evaluation and interpretation. She was mostly responsible for writing the paper. MS also was responsible for the day-to-day implementation of the RCT and supported the study design, data interpretation and manuscript preparation. MJS had input into study design, data analysis and manuscript preparation. AP had input into study design, data interpretation and manuscript preparation. JP oversaw the Man Up project and had input into each stage of study design and data evaluation, data interpretation and manuscript preparation.
Funding: Funding for Man Up was provided by the Movember Foundation. Funds supported the development of the documentary and associated social media campaign, as well as their evaluation. The Movember Foundation had no role in the design or conduct of the randomised controlled trial reported here, or in the collection, management and analysis of the data, or in preparation of this manuscript.
Competing interests: None declared.
Ethics approval: The trial was approved by the Health Science Human Ethics Subcommittee at the University of Melbourne. It was registered with the Australian New Zealand Clinical Trials Registry (ACTRN12616001169437, Universal Trial Number: U1111-1186-1459).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Slade T, Johnston A, Oakley Browne MA, et al. . 2007 national survey of mental health and wellbeing: methods and key findings. Aust N Z J Psychiatry 2009;43:594–605. 10.1080/00048670902970882 [DOI] [PubMed] [Google Scholar]
- 2. Australian bureau of statistics. 3303.0 causes of death Australia, 2015. Canberra: Australian bureau of statistics, 2016. [Google Scholar]
- 3. Houle J, Mishara BL, Chagnon F. An empirical test of a mediation model of the impact of the traditional male gender role on suicidal behavior in men. J Affect Disord 2008;107:37–43. 10.1016/j.jad.2007.07.016 [DOI] [PubMed] [Google Scholar]
- 4. Thompson E, Pleck J : Levant R, Pollock W, Masculinity ideologies: a review of research instrumentation on men and masculinities. New York: A new psychology of men, 1995. [Google Scholar]
- 5. Thompson EH, Bennett KM. Measurement of masculinity ideologies: a (critical) review. Psychol Men Masc 2015;16:115–33. 10.1037/a0038609 [DOI] [Google Scholar]
- 6. Connell RW. Masculinities: The field of knowledge Horlacher S, Configuring masculinity in theory and literary practice. EBook: Brill, 2015:39–52. [Google Scholar]
- 7. Rice S, Fallon B, Bambling M. Men and depression: The impact of masculine role norms throughout the lifespan. The Australian Educational and Developmental Psychologist 2011;28:133–44. 10.1375/aedp.28.2.133 [DOI] [Google Scholar]
- 8. Pirkis J, Spittal MJ, Keogh L, et al. . Masculinity and suicidal thinking. Soc Psychiatry Psychiatr Epidemiol 2017;52:319–27. 10.1007/s00127-016-1324-2 [DOI] [PubMed] [Google Scholar]
- 9. Monk D, Ricciardelli LA. Three dimensions of the male gender role as correlates of alcohol and cannabis involvement in young Australian men. Psychol Men Masc 2003;4:57–69. 10.1037/1524-9220.4.1.57 [DOI] [Google Scholar]
- 10. Wong YJ, Ho MR, Wang SY, et al. . Meta-analyses of the relationship between conformity to masculine norms and mental health-related outcomes. J Couns Psychol 2017;64:80–93. 10.1037/cou0000176 [DOI] [PubMed] [Google Scholar]
- 11. Coleman D. Traditional Masculinity as a Risk Factor for Suicidal Ideation: Cross-Sectional and Prospective Evidence from a Study of Young Adults. Arch Suicide Res 2015;19:366–84. 10.1080/13811118.2014.957453 [DOI] [PubMed] [Google Scholar]
- 12. Easton SD, Renner LM, O’Leary P. Suicide attempts among men with histories of child sexual abuse: examining abuse severity, mental health, and masculine norms. Child Abuse Negl 2013;37:380–7. 10.1016/j.chiabu.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 13. Galdas PM, Cheater F, Marshall P. Men and health help-seeking behaviour: literature review. J Adv Nurs 2005;49:616–23. 10.1111/j.1365-2648.2004.03331.x [DOI] [PubMed] [Google Scholar]
- 14. Levant RF, Wimer DJ, Williams CM, et al. . The Relationships between masculinity variables, health risk behaviors and attitudes toward seeking psychological help. Int J Mens Health 2009;8:3–21. 10.3149/jmh.0801.3 [DOI] [Google Scholar]
- 15. Boman EKO, Walker GA. Predictors of men’s health care utilization. Psychol Men Masc 2010;11:113–22. 10.1037/a0018461 [DOI] [Google Scholar]
- 16. Nam SK, Chu HJ, Lee MK, et al. . A meta-analysis of gender differences in attitudes toward seeking professional psychological help. J Am Coll Health 2010;59:110–6. 10.1080/07448481.2010.483714 [DOI] [PubMed] [Google Scholar]
- 17. Dworkin SL, Fleming PJ, Colvin CJ. The promises and limitations of gender-transformative health programming with men: critical reflections from the field. Cult Health Sex 2015;17(Suppl 2):128–43. 10.1080/13691058.2015.1035751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ajzen I. The theory of planned behavior. Organ behav hum decis process 1991;50:179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- 19. Reynolds WM. Adult suicidal ideation questionniare: professional manual. USA: PAR, 1991. [DOI] [PubMed] [Google Scholar]
- 20. National geographic. Test your brain. USA, 2016. [Google Scholar]
- 21. Wilson CJ, Deane FP, Ciarrochi J, et al. . Measuring help seeking intentions: properties of the general help seeking questionnaire. Canadian Journal of Counselling 2005;39:15–28. [Google Scholar]
- 22. Mahalik JR, Locke BD, Ludlow LH, et al. . Development of the conformity to masculine norms inventory. Psychol Men Masc 2003;4:3–25. 10.1037/1524-9220.4.1.3 [DOI] [Google Scholar]
- 23. Wester SR, Vogel DL, O’Neil JM, et al. . Development and evaluation of the gender role conflict scale short form. Psychol Men Masc 2012;13:199–210. 10.1037/a0025550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991;32:705–14. 10.1016/0277-9536(91)90150-B [DOI] [PubMed] [Google Scholar]
- 25. Simmons C. The personal wellbeing index : Simmons C, Lehman P, Tools for strenghth-based assessment and evaluation. New York: Springer, 2012. [Google Scholar]
- 26. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 2003;18:76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- 27. Australian Bureau of Statistics. 6227.0 - Education and Work. Australia, 2015. [Google Scholar]