Abstract
Purpose
Patients with tetraplegia consistently rank better use of the upper extremity as their top functional priority. Multiple case series have demonstrated that Upper Extremity Reconstruction (UER) is well-tolerated and can produce substantial functional improvements for appropriate candidates; however, UER remains critically underutilized. The mechanisms that drive differences in provider practice and referral patterns have been studied, but comprehensive examination of the patient factors that influence UER decisions has not been performed for American patients.
Methods
Nineteen patients with C4-C8 cervical spinal injuries were selected using purposive sampling: 9 patients had undergone UER, 10 had not undergone UER. Semi-structured interviews were conducted and transcripts evaluated using grounded theory methodology.
Results
Our study yielded a conceptual model that describes the characteristics common to all patients who undergo UER. Patients who selected reconstruction proceeded stepwise through a shared sequence of steps: 1) functional dissatisfaction 2) awareness of UER and 3) acceptance of surgery. Patients’ ability to meet these criteria was determined by three checkpoints: how well they coped, their access to information, and the acceptability of surgery. Extremely positive or negative coping prevented patients from moving from the Coping to the Information Checkpoint; thus, they remained unaware of UER and did not undergo surgery. A lack of knowledge regarding reconstruction was the strongest barrier to surgery among our participants.
Conclusions
We built a conceptual model that outlines how patients’ personal and contextual factors drive their progression to UER. Moving from functional dissatisfaction to understanding that they were candidates for UER was a substantial barrier for participants, particularly those with very high and very low coping skills.
Clinical Relevance
To improve utilization for all patients, interventions are needed to increase UER awareness. Standardizing introduction to UER during the rehabilitation process or improving e-content may represent key awareness access points.
Keywords: qualitative, spinal cord injury, surgery, tendon transfer, tetraplegia
Tetraplegia is a devastating outcome after cervical spinal cord injury (SCI). The functional losses individuals experience often result in profound caregiver dependence, financial hardship, and deep emotional distress.1–10 Persons with tetraplegia also stress the medical system. Patients are at increased risk for numerous medical conditions ranging from urinary tract infections to life threatening cardio-respiratory disease.9,11–13 Depending on cervical level and age at injury, the lifetime direct cost associated with tetraplegia ranges from 2.1 to 5.4 million dollars.14 Given such broad impact, interventions that foster patients’ independence are important at both the individual and societal level.
Although patients with tetraplegia experience deficits in multiple functional categories, they consistently rank hand and arm function as most important to their quality of life, making upper extremity reconstruction (UER) an appealing option.15–17 Even small gains in grasp or wrist extension can translate into substantial independence for tetraplegia patients.18–23 In fact, numerous studies demonstrate that UER has low complication rates and excellent long-term patient satisfaction.24–29 Yet, for all this potential benefit, only 10-14% of eligible U.S. patients ever undergo reconstruction.30,31,32
This paradox between high potential benefit and low utilization likely stems from multiple variables, but investigation of these factors in the surgical literature is limited and sometimes contradictory . Qualitative research from New Zealand indicates that patients decline surgery when they lack social support or when they cannot tolerate the prospect of increased dependency during the immediate post-operative phase when immobilization may be required.33,34 Some survey data from the U.S suggest that patients question the benefits of UER, are deterred by pessimistic first impressions of reconstruction, or harbor concerns about the length of their recovery.35–37 However, a conflicting survey found that 80% of respondents would be willing to tolerate 2-3 months of increased dependence to ultimately improve function.38
We sought to clarify and expand on this work by investigating the context surrounding UER barriers. Using the International Classification of Functioning’s (ICF) biopsychosocial model of health as our guiding framework, we performed a qualitative evaluation of why more patients do not select UER.39 (Figure 1) Our study explores the features that distinguish patients who undergo surgery from those who do not. We then analyze the personal and environmental factors that drive this division at critical “checkpoints” in patients’ progression toward surgery. We aim to provide a comprehensive understanding of patients’ experiences and identify points on the pathway where intervention will be most impactful to improve UER utilization.
Figure 1. International Classification of Function Psychosocial Model of Function.

Materials & Methods
Study Design
This was a cross-sectional observational study. Semi-structured interviews were conducted from August-September 2016 using a standardized interview guide created de novo by the authors. Initial prompts were derived from a literature review and the senior author’s clinical expertise. (Appendix 1) Informed consent was obtained prior to participation, and audio recording was conducted for all sessions. This study was approved by our institution’s research review board.
Subjects
To recruit patients with C4-C8 cervical spinal injuries who had undergone UER, we searched patients’ electronic medical records at our institution for tendon transfer, tenodesis, and opponenplasty using International Classification of Disease (ICD9) and CPT codes. Patients who had not undergone surgery were recruited via email lists from the Department of Physical Medicine and Rehabilitation (PM&R). The researchers conducted screening phone calls to ensure patients had disability in all four limbs and that their injury occurred at least one year prior to interview. We excluded patients who were under age 18 or who did not speak English. Purposive sampling, (deliberate sampling wherein participants are selected to meet criteria defined a priori rather than randomly), was used to enroll an equal number of patients in the “surgery” (SG) and “no surgery” (NSG) groups.40
Data Collection
We conducted interviews at patients’ homes, our research facility, and via telephone. Initially, two investigators (X1 surgery resident; X2 medical student) were present at all interviews and held regular debriefing sessions to evaluate question clarity, interview style, and overall consistency. Participants were encouraged to clarify interview questions as needed and were invited to suggest changes or new questions to better reflect their experience at the end of each session. After standardizing delivery of the interview topics during the first 5 interviews, a single investigator conducted the remaining 14. All interviews were recorded and then transcribed verbatim by a member of the research team, which provided a second opportunity to evaluate interview consistency. We employed iterative (transcripts were re-analyzed as new themes arose) and emerging (explanatory ideas were identified and explored in-depth) analysis throughout data collection to identify developing themes. We amended our interview guide after interviews 7 and 12 to better capture these themes.41–43 Interviews continued until conceptual saturation, at which point participants no longer generated new themes.
Data Analysis
We used grounded theory and constant comparative analysis to structure our analysis.44–46 Investigators began open coding by independently reading 4 patient transcripts line-by-line to generate a broad list of themes. Redundant themes were eliminated and nested concepts were clustered into themes, codes, and sub-codes to generate a preliminary codebook. The initial 4 transcripts were recoded, discrepancies were reviewed, and the codebook amended. One primary investigator (X1) coded all 19 transcripts. Following a training exercise to unify coding methodology, four research assistants were added to diversify perspective (ensuring all important themes were captured), and to expedite the coding process. Ten transcripts were double-coded. The primary investigator and second coder compared transcripts in one-on-one meetings, discrepancies were evaluated, and no persistent disagreements emerged. Unclear code definitions were revised and the codebook updated periodically. (Appendix 2) Step-by-step study procedures, training exercises, and investigator contributions/credentials are summarized in a flow diagram. (Appendix 3)
Results
The study sample included 9 patients in the surgery group (SG) and 10 patients in the no surgery group (NSG). Table 1 summarizes patient demographic data. Initial analysis revealed that all patients who chose UER met three minimum conditions: 1) they were dissatisfied with their function 2) they became aware that they were candidates for UER and 3) they decided that surgery was acceptable. We then directed the bulk of our analysis to understanding why SG patients met these conditions whereas NSG patients did not. We propose three checkpoints that channeled individuals to either the SG or the NSG: how patients cope/adapt post-injury; how they access and use information; and how surgery stands to impact their lives. Based on the ICF framework, we then split our explanation of these checkpoints into the ‘personal’ and ‘contextual’ domains. Finally, we synthesized our findings into a conceptual model (Figure 2). This section will explain our model by providing an overview of the Coping, Information, and Surgical Impact Checkpoints and a detailed account of the personal or contextual experiences that move patients toward or away from surgery at each.
Table 1.
Patient Demographic Data
| Demographic | SG | NSG | Total |
|---|---|---|---|
| Sex | |||
| Male | 5 | 10 | 15 |
| Female | 4 | 0 | 4 |
| Age at injury | |||
| 18-25 | 4 | 5 | 9 |
| 26-35 | 1 | 1 | 2 |
| 36-45 | 3 | 1 | 4 |
| 46-55 | 1 | 1 | 2 |
| 56-65 | 0 | 2 | 2 |
| Ethnicity | |||
| Caucasian | 8 | 9 | 17 |
| African American | 1 | 0 | 1 |
| Hispanic | 0 | 1 | 1 |
| Cause of Injury | |||
| MVA | 6 | 2 | 8 |
| Diving | 1 | 4 | 5 |
| Other sport | 0 | 2 | 2 |
| Fall | 1 | 1 | 2 |
| Other traumatic cause | 1 | 1 | 2 |
| Level of Injury | |||
| C4 | 3 | 2 | 5 |
| C5 | 1 | 7 | 8 |
| C6 | 4 | 1 | 5 |
| C7 | 1 | 0 | 1 |
| C8 | 0 | 0 | 0 |
| AISA Grade | |||
| A | 4 | 4 | 8 |
| B | 2 | 4 | 6 |
| C | 3 | 0 | 3 |
| D | 0 | 2 | 2 |
| Living situation | |||
| Independent | 4 | 3 | 7 |
| Spouse/Partner | 1 | 5 | 6 |
| Parents | 2 | 2 | 4 |
| Assisted Living Facility | 2 | 0 | 2 |
| Educational Level | |||
| Secondary School | 6 | 1 | 7 |
| Vocational Training | 1 | 1 | 2 |
| Undergraduate Studies | 2 | 5 | 7 |
| Graduate Studies | 0 | 3 | 3 |
Figure 2. Path to Upper Extremity Reconstruction.

Conceptual model of progression to UER.
Checkpoint 1: Coping & Adaptation
How patients cope with tetraplegia depends on many interrelated and evolving factors. Post-injury, patients face numerous tasks, beginning with how to manage their own emotions and identity and extending to how they negotiate relationships and integrate into their communities. Given this complexity, our analysis did not reveal a unique set of coping strategies that distinguished SG patients from NSG patients. In fact, at the individual-behavior level (for example patients’ ability to maintain perspective), SG and NSG patients were often indistinguishable. What separated patients was whether the balance of their coping behaviors was positive or negative and to what degree.
Ultimately, a continuum emerged with patients at coping extremes less likely to progress to UER. Patients with consistently exceptional coping generally did not experience enough dissatisfaction to move into the information-seeking phase, and defaulted to the NSG. Conversely, patients with extreme difficulty coping, lost self-efficacy, and became isolated from the mechanisms that could connect them to surgery. SG patients had the ‘goldilocks’ experience: enough negative coping to be dissatisfied, but not to the point that they disengaged, and enough positive coping to maintain self-efficacy without accepting their condition entirely. A detailed examination of positive/negative coping in the personal and contextual domains follows.
Personal Factors
Like patients in other studies of chronic conditions, our participants felt that their injury incited a “biographical disruption”.47–49 That is, because their identity was linked to physical ability, an abrupt functional loss damaged their sense of self. In this context, positive coping behaviors were those that helped patients accept a new identity. Although participants almost universally endorsed a period of mourning immediately following injury, those with robust coping skills could stay optimistic and maintain perspective. Patients who accepted their injury could start finding ways to maximize their remaining function, and viewed assistance as a necessary fact of their new lives rather than a personal failing.
Patients with poor coping made frequent comparisons to their pre-injured selves or non-injured peers. They felt that their increased needs made them a burden to their loved ones. Instead of focusing on function and setting goals, these patients concentrated on their barriers. Overall, highly positive coping helped patients rebuild an identity that they liked, but decreased their incentive to seek additional treatment. Patients with predominantly negative behaviors became overwhelmed with feelings of worthlessness, had an unfavorable self-concept, and lost agency. (Figure 3)
Figure 3. Personal Coping Domains.
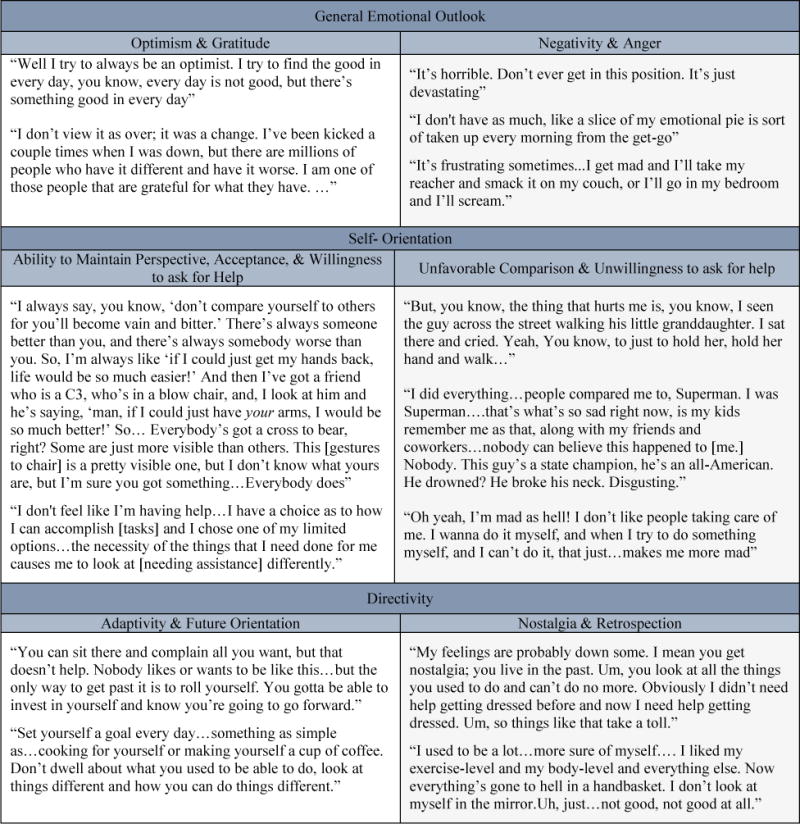
A comparison and positive and negative personal coping behaviors among participants
Contextual Factors
Contextual factors related to participants’ surroundings. Patients’ social support, physical environment, and financial resources influenced coping by combating or reinforcing isolation. Patients with few social connections felt abandoned, whereas those with affirmative relationships had greater ease resuming their pre-injury roles or forming new friendships. Although participants almost unanimously endorsed some version of the sentiment “you find out who your real friends are,” genuine friends helped patients stay connected. Dedicated companions assumed caregiver roles, navigated mobility challenges, and adapted their activities. In cases where friendships dissolved, patients reported that their friends viewed them as diseased or broken.
Patients used financial and social capital to augment function. Participants who could afford to modify their homes reported more independence in household and personal care tasks. Patients also used out-of-pocket funds to fill insurance gaps and pay for wheelchair-adapted vans or additional caregivers. Well-connected participants reported that their social network helped with home renovations, and transportation. Patients who could not afford additional care felt that their progress was unfairly limited or reported increased isolation, which further reinforced feelings of helplessness. (Figure 4)
Figure 4. Contextual Coping Domains.

A comparison and positive and negative contextual coping influences among participants
Checkpoint 2: Information Access & Use
If the balance of patients’ personal and contextual coping behaviors produced dissatisfaction with their function, becoming aware of UER was the next major breakpoint. UER-aware patients were often unsure of how they first learned about surgery, but identified PM&R physicians or physical therapists as the likely source. To reflect this, we included a direct provider-awareness connection in our model. Most NSG patients reported no or minimal awareness of UER. To understand why, we examined this Information Checkpoint using the same ‘personal’ and ‘contextual’ lenses we applied to Coping.
Personal Factors
Patients differed in their motivation to obtain tetraplegia-related information. Patients who believed ongoing research would yield better treatments remained actively engaged with medical information. Participants thought that by remaining up-to-date, they would be able benefit from medical advances sooner; however, they tended to focus on stem cell treatments and exoskeletons, with no one reporting regular research on UER. Patients also sought information for tetraplegic-specific issues such as wheelchair maintenance, home care, or insurance through online SCI forums, but were skeptical of medical advice unless it was provided by a member they trusted. Participants preferred medical information from their doctors or patients with whom they could talk directly, though actually connecting to fellow patients was challenging. Patients with few information-seeking behaviors thought the SCI materials were not particularly relevant, or lost interest over time. One participant found it too depressing. Several patients also noted limitations in their ability to process complex medical information or ask the right questions. (Figure 5)
Figure 5. Personal Information-Seeking Behaviors.

A comparison and positive and information-seeking behaviors among participants
Contextual Factors
Technology, particularly touchscreen devices and voice-recognition software improved patients’ information access; however, patients varied in their usage. Some patients reported poor internet access or difficulty obtaining adaptive devices; others with limited technological fluency found their devices difficult to use. Similarly, patients who received printed newsletters from hospitals indicated that this information was often inaccessible because they were physically unable to turn the pages. A minority stated that they simply did not know where to get UER information. Predictably, many of the contextual factors that supported good coping (such as strong social networks and financial resources) improved information access. (Figure 6)
Figure 6. Information Context.

A comparison and positive and negative information access influences among participants
Checkpoint 3: Surgical Impact
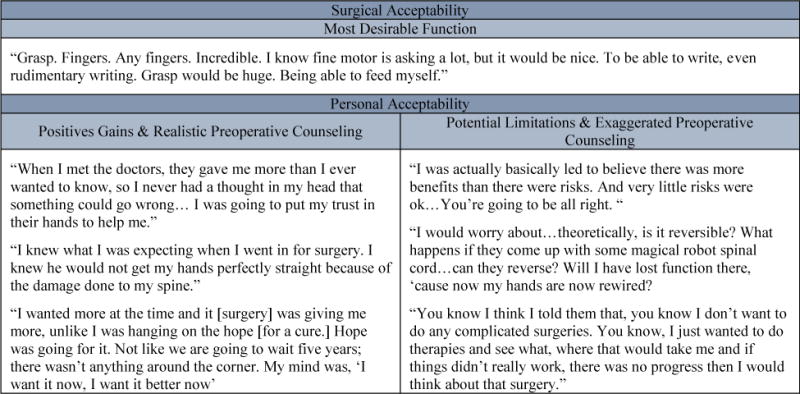
If patients successfully moved through the Information Checkpoint and became aware that they were candidates, the final roadblock to UER was Surgical Impact. Patients almost uniformly stated that improved grip strength was their biggest surgical priority, both because they wanted to be able to perform specific physical tasks, and for broader reasons like increased family participation. Patients wanted to understand operative mechanics, possible risks, and the function they could expect following surgery.
Personal Factors
Patients who elected to undergo UER weighted potential functional gains far above other aspects of the decision, even discounting possible complications. Although surgical patients generally agreed that their surgeon offered realistic pre-operative counseling, one patient felt the benefits were exaggerated. Patients who were hoping for a definitive cure (even if they recognized its unlikelihood) expressed more hesitation about surgery than those who felt they had achieved their maximal functional gains. Several patients also communicated a preference for less invasive treatments; others thought immobilization would harm their rehabilitation progress. The few patients who declined surgery did not point to a specific surgical fact that deterred them, but indicated that they found the entire process to be intimidating. (Figure 7)
Figure 7. Personal Surgical Acceptability.
Comparison of the personal factors that influence acceptability of UER.
Contextual Factors
To determine the contextual impact, most patients weighed potential functional benefits against the impact their recovery would have on their families’ lives and their external commitments. In general, patients reported that they would tolerate more immobilization and longer rehabilitation times if the benefits they stood to gain were great. Patients acknowledged that their caregivers’ burden would increase during recovery, but many felt that increased care was a surmountable obstacle. Potential candidates found immobilization to be a stronger deterrent than rehabilitation. Students/employees suggested that the amount of time they would need off would be a large factor in their decision, though they were reluctant to commit to a prohibitive cutoff point. (Figure 8)
Figure 8. Contextual Acceptability Domains.

Environmental Factors that Influence acceptability of UER
Discussion
UER can be transformative for patients with tetraplegia, but remains critically underutilized. Understanding how or why barriers to UER materialize is difficult because patients have diverse and complex experiences. Our qualitative examination is distinct in the amount of emphasis given to the personal and contextual factors that shape patients’ decisions to pursue reconstruction. We offer a conceptual model to outline the patient experience, first identifying the three conditions necessary to choose UER: functional dissatisfaction, awareness of UER, and surgical acceptability. We further develop this idea through our detailed examination of how patients fulfill these conditions through Coping, Information, and Acceptability Checkpoints. Our model provides a novel framework to understand where barriers to UER exist, and what behaviors could be leveraged for interventions at each step.
Our findings echo those from other fields that report inadequate coping skills correlate with low self-efficacy to produce poor outcomes, as well as upper extremity research that indicates highly activated/engaged patients experience less pain and disability.50–54 Our conclusion that patients with extreme-negative coping behaviors do not progress to UER is therefore predictable. Potentially more surprising, is our finding that, in strict progression-to-UER terms, high coping is not advantageous. By demonstrating that exceptional coping can actually hinder progress, our study questions the traditional conclusion that self-efficacious patients do best. Instead, we propose that, in select cases, doing well (coping with injury) actually prevents patients from doing better or at least, improving hand function with UER.
Psychology literature has shown that patients with disabilities sometimes demonstrate a preference for their current state, and irrationally discount better treatments (status quo bias), but the paradox that patients could cope so well that they miss an opportunity to improve function is not well-characterized in the surgical literature.55–57 Furthermore, participants with excellent coping skills were not so much “choosing” their status quo, as lacking exposure to UER. The degree to which patients with tetraplegia prefer non-invasive treatments overall is not completely understood, but warrants further investigation as several subjects expressed a generalized fear of surgery, and patients’ preference for non-operative treatment is becoming increasingly recognized.58–60
This study has several limitations. We did not employ objective functional metrics to correlate patients’ perceived function with actual function. It is also possible that by their willingness to participate, study subjects represented a more proactive cohort than exists in the general SCI population. Because it was difficult to identify patients who were aware of but declined surgery a priori, our understanding of surgical acceptability was less rich than other parts of the model. Our sample was also predominantly white and from a single geographic location, which may limit the transferability of these findings. Although smaller than most quantitative studies, our sample size is consistent with other qualitative studies in this population and reflects our aim to provide a more complete understanding of the patient experience than might be had from a statistical comparison between two samples. Additionally, participants were added until conceptual saturation was reached, thus increasing our sample size would not generate new themes. Finally, our model may suggest a more linear progression than actually occurs for most patients. The contextual factors that shape patients’ decisions likely have impact at multiple stages and may change over time.
Ultimately, our study suggests that coping is not a good leverage point to maximize surgical uptake. Given the breadth of factors our interviews identified, attempts to improve coping will be challenging and likely to be inefficient. Coping-directed interventions would also continue to ignore high-performers. Promising interventions will likely be those that move more patients into the information-seeking phase and ensure available and accurate UER resources. Interventions that promote introduction to hand surgery at multiple standard points may improve utilization, but will require physician buy-in, particularly from PM&R doctors who do not always share surgeons’ belief in the benefits of reconstruction.
Improving UER e-content has potential given patients’ growing preference for electronic media. Focusing on patient-led forums may have particular merit considering the study by Wagner et al. that found patients trusted UER if they learned about it from a fellow patient, and aligns with participants’ preference to speak with other surgical patients prior to reconstruction.36 However, implementation must be thoughtful to overcome some patients’ lower trust of online materials. Video-chatting could be an area of expansion. Ultimately, ensuring an opportunity for all eligible patients to make an informed decision about UER is important in supporting patients’ function. Our model provides a framework for these crucial efforts.
Supplementary Material
Appendix 1: Interview Question Guide
Appendix 2: Codebook
Appendix 3: Study Flow Diagram
Acknowledgments
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number 2 K24-AR053120-06. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Manns PJ, Chad KE. Components of quality of life for persons with a quadriplegic and paraplegic spinal cord injury. Qual Health Res. 2001;11(6):795–811. doi: 10.1177/104973201129119541. [DOI] [PubMed] [Google Scholar]
- 2.Geyh S, Nick E, Stirnimann D, et al. Self-efficacy and self-esteem as predictors of participation in spinal cord injury—an ICF-based study. Spinal Cord. 2012;50(9):699–706. doi: 10.1038/sc.2012.18. [DOI] [PubMed] [Google Scholar]
- 3.Putzke JD, Richards JS, Hicken BL, DeVivo MJ. Predictors of life satisfaction: A spinal cord injury cohort study. Arch Phys Med Rehabil. 2002;83(4):555–561. doi: 10.1053/apmr.2002.31173. [DOI] [PubMed] [Google Scholar]
- 4.Nielsen MS. Post-traumatic stress disorder and emotional distress in persons with spinal cord lesion. Spinal Cord 0000. 41(5):296–302. doi: 10.1038/sj.sc.3101427. [DOI] [PubMed] [Google Scholar]
- 5.Kennedy P, Rogers BA. Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil. 2000;81(7):932–937. doi: 10.1053/apmr.2000.5580. [DOI] [PubMed] [Google Scholar]
- 6.Bushnik T, Wright J, Burdsall D. Personal attendant turnover: association with level of injury, burden of care, and psychosocial Outcome. Top Spinal Cord Inj Rehabil. 2007;12(3):66–76. [Google Scholar]
- 7.Forrest G, Schwam A, Cohen E. Time of care required by patients discharged from a rehabilitation unit. Am J Phys Med Rehabil. 2002;81(1):57–62. doi: 10.1097/00002060-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Manns PJ, Chad KE. Determining the relation between quality of life, handicap, fitness, and physical activity for persons with spinal cord injury. Arch Phys Med Rehabil. 1999;80(12):1566–1571. doi: 10.1016/s0003-9993(99)90331-3. [DOI] [PubMed] [Google Scholar]
- 9.Krause JS, Saunders LL. Socioeconomic and behavioral risk factors for mortality: do risk factors observed after spinal cord injury parallel those from the general USA population? Spinal Cord. 2012;50(8):609–613. doi: 10.1038/sc.2012.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krause JS, Saunders LL, DeVivo MJ. Income and risk of mortality after spinal cord injury. Arch Phys Med Rehabil. 2011;92(3):339–345. doi: 10.1016/j.apmr.2010.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wannapakhe J, Arrayawichanon P, Saengsuwan J, Amatachaya S. Medical complications and falls in patients with spinal cord injury during the immediate phase after completing a rehabilitation program. J Spinal Cord Med. 2015;38(1):84–90. doi: 10.1179/2045772313Y.0000000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adriaansen JJ, Post MW, de Groot S, et al. Secondary health conditions in persons with spinal cord injury: a longitudinal study from one to five years post-discharge. J Rehabil Med. 2013;45(10):1016–1022. doi: 10.2340/16501977-1207. [DOI] [PubMed] [Google Scholar]
- 13.Jensen MP, Truitt AR, Schomer KG, Yorkston KM, Baylor C, Molton IR. Frequency and age effects of secondary health conditions in individuals with spinal cord injury: a scoping review. Spinal Cord. 2013;51(12):882–892. doi: 10.1038/sc.2013.112. [DOI] [PubMed] [Google Scholar]
- 14.Cao Y. Lifetime direct costs after spinal cord injury. Top Spinal Cord Inj Rehabil. 2011;16(4):10–16. [Google Scholar]
- 15.Anderson KD. Targeting Recovery: Priorities of the spinal cord-injured population. J Neurotrauma. 2004;21(10):1371–1383. doi: 10.1089/neu.2004.21.1371. [DOI] [PubMed] [Google Scholar]
- 16.Hanson RW, Franklin MR. Sexual loss in relation to other functional losses for spinal cord injured males. Arch Phys Med Rehabil. 1976;57(6):291–293. [PubMed] [Google Scholar]
- 17.Snoek GJ, MJ IJ, Hermens HJ, Maxwell D, Biering-Sorensen F. Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord. 2004;42(9):526–532. doi: 10.1038/sj.sc.3101638. [DOI] [PubMed] [Google Scholar]
- 18.Lipscomb PR, Elkins EC, Henderson ED. Tendon transfers to restore function of hands in tetraplegia, especially after fracture-dislocation of the sixth cervical vertebra on the seventh. J Bone Joint Surg Am. 1958;40-a(5):1071–1080. [PubMed] [Google Scholar]
- 19.Freehafer AA. Tendon transfers to improve grasp in patients with cervical spinal cord injury. Paraplegia. 1975;13(1):15–24. doi: 10.1038/sc.1975.4. [DOI] [PubMed] [Google Scholar]
- 20.Hentz VR, Brown M, Keoshian LA. Upper limb reconstruction in quadriplegia: Functional assessment and proposed treatment modifications. J Hand Surg Am. 1983;8(2):119–131. doi: 10.1016/s0363-5023(83)80001-x. [DOI] [PubMed] [Google Scholar]
- 21.Dunkerley AL, Ashburn A, Stack EL. Deltoid triceps transfer and functional independence of people with tetraplegia. Spinal Cord. 2000;38(7):435–441. doi: 10.1038/sj.sc.3101025. [DOI] [PubMed] [Google Scholar]
- 22.Welraeds D, Ismail AA, Parent A. Functional reconstruction of the upper extremity in tetraplegia. Application of Moberg’s and Allieu’s procedures. Acta Orthop Belg. 2003;69(6):537–545. [PubMed] [Google Scholar]
- 23.Elhassan BT, Wagner ER, Spinner RJ, Bishop AT, Shin AY. Contralateral trapezius transfer to restore shoulder external rotation following adult brachial plexus injury. J Hand Surg Am. 2016;41(4):e45–e51. doi: 10.1016/j.jhsa.2015.12.026. [DOI] [PubMed] [Google Scholar]
- 24.Meiners T, Abel R, Lindel K, Mesecke U. Improvements in activities of daily living following functional hand surgery for treatment of lesions to the cervical spinal cord: self-assessment by patients. Spinal Cord. 2002;40(11):574–580. doi: 10.1038/sj.sc.3101384. [DOI] [PubMed] [Google Scholar]
- 25.Wangdell J, Friden J. Satisfaction and performance in patient selected goals after grip reconstruction in tetraplegia. J Hand Surg Eur Vol. 2010;35(7):563–568. doi: 10.1177/1753193410373184. [DOI] [PubMed] [Google Scholar]
- 26.Jaspers Focks-Feenstra JH, Snoek GJ, Bongers-Janssen HMH, Nene AV. Long-term patient satisfaction after reconstructive upper extremity surgery to improve arm-hand function in tetraplegia. Spinal Cord. 2011;49(8):903–908. doi: 10.1038/sc.2011.21. [DOI] [PubMed] [Google Scholar]
- 27.Gregersen H, Lybæk M, Lauge Johannesen I, Leicht P, Nissen UV, Biering-Sørensen F. Satisfaction with upper extremity surgery in individuals with tetraplegia. J Spinal Cord Med. 2015;38(2):161–169. doi: 10.1179/2045772314Y.0000000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bednar MS. Tendon transfers for tetraplegia. Hand Clin. 2016;32(3):389–396. doi: 10.1016/j.hcl.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 29.Lamb DW, Chan K. Surgical reconstruction of the upper limb in traumatic tetraplegia. A review of 41 patients. Bone Joint J. 1983;65(3):291–298. doi: 10.1302/0301-620X.65B3.6841399. [DOI] [PubMed] [Google Scholar]
- 30.Curtin CM, Gater DR, Chung KC. Upper extremity reconstruction in the tetraplegic population, a national epidemiologic study. J Hand Surg Am. 2005;30(1):94–99. doi: 10.1016/j.jhsa.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Moberg E. Surgical treatment for absent single-hand grip and elbow extension in quadriplegia. Principles and preliminary experience. J Bone Joint Surg Am. 1975;57(2):196–206. [PubMed] [Google Scholar]
- 32.Bryden AM, Wuolle KS, Murray PK, Peckham PH. Perceived outcomes and utilization of upper extremity surgical reconstruction in individuals with tetraplegia at model spinal cord injury systems. Spinal Cord. 2004;42(3):169–176. doi: 10.1038/sj.sc.3101579. [DOI] [PubMed] [Google Scholar]
- 33.Dunn JA, Hay-Smith EJC, Whitehead LC, Keeling S. Issues influencing the decision to have upper limb surgery for people with tetraplegia. Spinal Cord. 2012;50(11):844–847. doi: 10.1038/sc.2012.58. [DOI] [PubMed] [Google Scholar]
- 34.Dunn JA, Hay-Smith EJC, Whitehead LC, Keeling S. Liminality and decision making for upper limb surgery in tetraplegia: a grounded theory. Disabil Rehabil. 2013;35(15):1293–1301. doi: 10.3109/09638288.2012.727945. [DOI] [PubMed] [Google Scholar]
- 35.Curtin CM, Hayward RA, Kim HM, Gater DR, Chung KC. Physician perceptions of upper extremity reconstruction for the person with tetraplegia. J Hand Surg Am. 2005;30(1):87–93. doi: 10.1016/j.jhsa.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 36.Wagner JP, Curtin CM, Gater DR, Chung KC. Perceptions of people with tetraplegia regarding surgery to improve upper-extremity function. J Hand Surg Am. 2007;32(4):483–490. doi: 10.1016/j.jhsa.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 37.Punj V, Curtin C. Understanding and overcoming barriers to upper limb surgical reconstruction after tetraplegia: The need for interdisciplinary collaboration. Arch Phys Med Rehabil. 2016;97(6, Supplement):S81–S87. doi: 10.1016/j.apmr.2015.11.022. [DOI] [PubMed] [Google Scholar]
- 38.Anderson KD, Friden J, Lieber RL. Acceptable benefits and risks associated with surgically improving arm function in individuals living with cervical spinal cord injury. Spinal Cord. 2008;47(4):334–338. doi: 10.1038/sc.2008.148. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization, WHO. Towards a Common Language for Functioning, Disability and Health: International classification of functioning, disability and health (ICF) Geneva: World Health Organization; 2002. [Google Scholar]
- 40.Devers KJ, Frankel RM. Study design in qualitative research–2: Sampling and data collection strategies. Educ Health (Abingdon) 2000;13(2):263–271. doi: 10.1080/13576280050074543. [DOI] [PubMed] [Google Scholar]
- 41.Turner DW., III Qualitative interview design: A practical guide for novice investigators. The qualitative report. 2010;15(3):754. [Google Scholar]
- 42.Forman J, Creswell JW, Damschroder L, Kowalski CP, Krein SL. Qualitative research methods: Key features and insights gained from use in infection prevention research. Am J Infect Control. 2008;36(10):764–771. doi: 10.1016/j.ajic.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 43.Gillham B. Research Interviewing: The Range of Techniques. Berkshire, England: Open University Press; 2005. [Google Scholar]
- 44.Corbin JM, Strauss A. Grounded theory research: Procedures, canons, and evaluative criteria. Qual Sociol. 1990;13(1):3–21. [Google Scholar]
- 45.Tolley EE, Mack N, Robinson ET, Succop SM. Qualitative Methods in Public Health: a field guide for applied research. 2nd. San Francisco, CA: Wiley; 2016. [Google Scholar]
- 46.Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant. 2002;36(4):391–409. [Google Scholar]
- 47.Bourke JA, Hay-Smith EJC, Snell DL, DeJong G. Attending to biographical disruption: the experience of rehabilitation following tetraplegia due to spinal cord injury. Disabil Rehabil. 2015;37(4):296–303. doi: 10.3109/09638288.2014.918188. [DOI] [PubMed] [Google Scholar]
- 48.Williams S. Chronic illness as biographical disruption or biographical disruption as chronic illness? Reflections on a core concept. Sociol Health Illn. 2000;22(1):40–67. [Google Scholar]
- 49.Dickson A, Allan D, O’carroll R. Biographical disruption and the experience of loss following a spinal cord injury: An interpretative phenomenological analysis. Psychol Health. 2008;23(4):407–425. doi: 10.1080/14768320701219136. [DOI] [PubMed] [Google Scholar]
- 50.Philip EJ, Merluzzi TV, Zhang Z, Heitzmann CA. Depression and cancer survivorship: importance of coping self-efficacy in post-treatment survivors. Psychooncology. 2013;22(5):987–994. doi: 10.1002/pon.3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bosmans MWG, Hofland HW, De Jong AE, Van Loey NE. Coping with burns: the role of coping self-efficacy in the recovery from traumatic stress following burn injuries. J Behav Med. 2015;38(4):642–651. doi: 10.1007/s10865-015-9638-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.MacNeil L, Esposito-Smythers C, Mehlenbeck R, Weismoore J. The effects of avoidance coping and coping self-efficacy on eating disorder attitudes and behaviors: A stress-diathesis model. Eat Behav. 2012;13(4):293–296. doi: 10.1016/j.eatbeh.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 53.Alok R, Das SK, Agarwal GG, Tiwari SC, Salwahan L, Srivastava R. Problem-focused coping and self-efficacy as correlates of quality of life and severity of fibromyalgia in primary fibromyalgia patients. J Clin Rheumatol. 2014;20(6):314–316. doi: 10.1097/RHU.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 54.Gruber JS, Hageman M, Neuhaus V, Mudgal CS, Jupiter JB, Ring D. Patient Activation and Disability in Upper Extremity Illness. J Hand Surg Am. 39(7):1378–1383.e1373. doi: 10.1016/j.jhsa.2014.03.042. [DOI] [PubMed] [Google Scholar]
- 55.Wasserman D. Disability, diversity, and preference for the status quo: bias or justifiable preference? Am J Bioeth. 2015;15(6):11–12. doi: 10.1080/15265161.2015.1028676. [DOI] [PubMed] [Google Scholar]
- 56.Mitchell F. Facilitators and barriers to informed choice in self-directed support for young people with disability in transition. Health Soc Care Community. 2015;23(2):190–199. doi: 10.1111/hsc.12137. [DOI] [PubMed] [Google Scholar]
- 57.Campbell SM, Wahlert L. Is disability conservationism rooted in status quo bias? Am J Bioeth. 2015;15(6):20–22. doi: 10.1080/15265161.2015.1028671. [DOI] [PubMed] [Google Scholar]
- 58.Mittal R, Harris IA, Adie S, Naylor JM. Factors affecting patient participation in orthopaedic trials comparing surgery to non-surgical interventions. Contemp Clin Trials Commun. 2016;3:153–157. doi: 10.1016/j.conctc.2016.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chhabra KR, Sacks GD, Dimick JB. Surgical decision making: Challenging dogma and incorporating patient preferences. JAMA. 2017;317(4):357–358. doi: 10.1001/jama.2016.18719. [DOI] [PubMed] [Google Scholar]
- 60.Boss EF, Mehta N, Nagarajan N, et al. Shared Decision Making and Choice for Elective Surgical Care. Otolaryngol Head Neck. 2015;154(3):405–420. doi: 10.1177/0194599815620558. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1: Interview Question Guide
Appendix 2: Codebook
Appendix 3: Study Flow Diagram


