Abstract
Infectious agents are known causes of human cancers. Schistosoma japonicum and Schistosoma mansoni cause a percentage of colorectal cancers in countries where the respective Schistosoma species are prevalent. Colorectal cancer is a complication of ulcerative colitis and colonic Crohn’s disease, the two main forms of idiopathic inflammatory bowel disease (IIBD). Mycobacterium avium subspecies paratuberculosis (MAP), the cause of a chronic intestinal disease in domestic and wild ruminants, is one suspected cause of IIBD. MAP may therefore be involved in the pathogenesis of IIBD-associated colorectal cancer as well as colorectal cancer in individuals without IIBD (sporadic colorectal cancer) in countries where MAP infection of domestic livestock is prevalent and MAP’s presence in soil and water is extensive. MAP organisms have been identified in the intestines of patients with sporadic colorectal cancer and IIBD when high magnification, oil immersion light microscopy (×1000 total magnification rather than the usual ×400 total magnification) is used. Research has demonstrated MAP’s ability to invade intestinal goblet cells and cause acute and chronic goblet cell hyperplasia. Goblet cell hyperplasia is the little-recognized initial pathologic lesion of sporadic colorectal cancer, referred to as transitional mucosa, aberrant crypt foci, goblet cell hyperplastic polyps or transitional polyps. It is the even lesser-recognized initial pathologic feature of IIBD, referred to as hypermucinous mucosa, hyperplastic-like mucosal change, serrated epithelial changes, flat serrated changes, goblet cell rich mucosa or epithelial hyperplasia. Goblet cell hyperplasia is the precursor lesion of adenomas and dysplasia in the classical colorectal cancer pathway, of sessile serrated adenomas and serrated dysplasia in the serrated colorectal cancer pathway, and of flat and elevated dysplasia and dysplasia-associated lesions or masses in IIBD-associated intestinal cancers. MAP’s invasion of intestinal goblet cells may result in the initial pathologic lesion of IIBD and sporadic colorectal cancer. MAP’s persistence in infected intestines may result in the eventual development of both IIBD-associated and sporadic colorectal cancer.
Electronic supplementary material
The online version of this article (10.1186/s13027-017-0172-3) contains supplementary material, which is available to authorized users.
Keywords: Goblet, Carcinomas, Adenomas, Infection, Cancerization, Serrated, Transitional mucosa, Aberrant foci, Inflammatory bowel disease
Introduction
Infectious agents are known causes of human cancers [1–3]. Mycobacterium avium subspecies paratuberculosis (MAP), the cause of a chronic intestinal disease in domestic and wild ruminants called Johne’s disease [4], is a long suspected cause of Crohn’s disease [5, 6] and a recently proposed cause of ulcerative colitis [7], the other main form of idiopathic inflammatory bowel disease (IIBD). If MAP causes IIBD, it may be one cause of the colorectal cancers that are a complication of IIBD [8, 9]. MAP may also be one cause of colorectal cancer in patients without IIBD (sporadic colorectal cancer) in countries where MAP infection of domestic livestock is endemic [10] and MAP’s contamination of soil [11] and water [12] is extensive.
The possibility that MAP is involved in the pathogenesis of colorectal cancer, in a patient with or without IIBD [13], is based on the following observations.
Other microorganisms are known causes of colorectal cancer
Schistosoma mansoni and Schistosoma japonicum cause a percentage of colorectal cancers in countries where the respective Schistosoma species are endemic [14–16].
A particular lesion, goblet cell hyperplasia, is the little-recognized initial pathologic lesion of sporadic colorectal cancer, ulcerative colitis and Crohn’s disease
In 1969, Filipe and colleagues first described the histopathologic components of transitional mucosa [17–19], which will subsequently be referred to as “goblet cell hyperplasia” or the “goblet cell hyperplasia lesion” (see Additional file 1):
The actual goblet cell hyperplasia, simply an increase in the number of goblet cells lining the colonic crypts.
The hyperplastic goblet cells are hypertrophic, longer and plumber than normal.
The crypts lined by hyperplastic goblet cells are either longer and wider or shorter and wider than normal.
Other authors emphasized one additional feature of transitional mucosa, the greatly increased amount of extracellular mucus coating the lesion produced by the hypertrophic and hyperplastic goblet cells [20, 21].
Beginning in 1991, two groups published their gross and histologic tangential (parallel to the mucosal surface) visualization of transitional mucosa, noticing the crypts were wider than normal but not that they were lined predominantly or exclusively by goblet cells, and called their lesion “aberrant crypt foci,” which is merely the goblet cell hyperplasia lesion in cross section [22–25].
In 2003, Torlakovic and colleagues [26] redefined the “hyperplastic” polyp as a serrated polyp and split the former hyperplastic polyp into two categories, the microvesicular type serrated polyp and the goblet cell type serrated polyp. They recognized that their goblet cell type serrated polyp is the precursor of the microvesicular type serrated polyp and noted its similarity to transitional mucosa, but they did not realize that it is the identical lesion as transitional mucosa [26].
Goblet cell hyperplasia is the rarely recognized initial pathologic lesion of Crohn’s disease and therefore of Crohn’s disease-associated intestinal cancers. Van Patter and colleagues’ 1954 treatise on regional enteritis [27] described goblet cell hyperplasia as follows:
The epithelium of the small bowel normally contains a variable number of secreting units – the goblet cells. In the vicinity of the lesions, the number of goblet cells was increased enormously, frequently to the point of complete replacement of other epithelial elements [27].
They speculated that whatever caused Crohn’s disease was the cause of the observed goblet cell hyperplasia:
There is some evidence to suggest that the etiologic agent is to be found in the fecal stream and that it makes its first appearance in the proximal portion of the small bowel…If this agent resides in the fecal stream it may exert its influence on the normal epithelial cells in the region of the future lesion, causing them to be replaced by goblet cells [27].
A sparse literature discusses goblet cell hyperplasia and its prominent extracellular mucus component as major pathologic features of Crohn’s disease [28, 29] and as the precursor lesion of epithelial dysplasia and therefore of Crohn’s disease-associated intestinal cancers, calling the lesion hyperplastic-like mucosal change [30].
Described as “epithelial hyperplasia,” “metaplastic changes,” “goblet cell rich epithelium” or “hypermucinous mucosa,” more subtle but more extensive goblet cell hyperplasia has occasionally [31–35] been recognized as the precursor of dysplasia and colorectal cancer in ulcerative colitis. A single article describes goblet cell hyperplasia in ulcerative colitis as such and documents its uniform presence in ulcerative colitis-affected colons with dysplasia [32].
Known as “transitional mucosa,” goblet cell hyperplasia is the precursor of dysplasia and adenomas [36] in the classical colorectal cancer pathway [37]. Transitional mucosa lines the stalks of pedunculated polyps [38, 39], forms the bases of tubular and villous adenomas [38, 39] and surrounds colorectal carcinomas [18, 19, 40, 41]. Transitional mucosa is a major component of the field cancerization theory in colorectal cancer [42].
Known as the “goblet cell type serrated polyp” [26, 43], goblet cell hyperplasia is the precursor lesion of the microvesicular type serrated polyp [26] and therefore of the sessile serrated adenoma [43] – serrated dysplasia [44] – serrated carcinoma [45] serrated colorectal cancer pathway [46]. The “transitional polyp” [21, 47] has rarely been recognized as the precursor lesion in both classical and serrated colorectal cancer pathways [48].
Of course, dysplasia and colorectal cancer develop from the goblet cell hyperplasia lesion seen in cross section, aberrant crypt foci, by either [49] the classical [22–25, 36, 50–52] or serrated [49] pathways.
Known by its alternative names, including the recently rediscovered “flat serrated change” [53] or “serrated epithelial changes” [54–56], goblet cell hyperplasia is the precursor of flat and elevated dysplasia [57] and dysplasia-associated lesions or masses [58] in IIBD-associated intestinal cancers as well as of classical adenomas in IIBD patients [59–62]. Like sporadic colorectal cancer patients, IIBD patients develop colorectal cancer by the classical or serrated pathways [63, 64]. Like in IIBD patients, the flat dysplasia (“flat adenoma”) – flat carcinoma pathway occurs in sporadic colorectal cancer patients [52, 65–67].
Pathogenic microorganisms are the only natural cause of intestinal goblet cell hyperplasia
While small intestinal goblet cell hyperplasia results from azoxymethane administration [68] and massive small intestinal resection [69], pathogenic bacteria and parasites are the only natural causes of intestinal goblet cell hyperplasia [70, 71], including the protozoan parasite Giardia lamblia/intestinalis [72], the helminthes Trichinella spiralis [73] and Nippostrongylis brasiliensis [74, 75], the bacteria Yersinia enterocolitica [76] and various Shigella species [77].
Goblet cell hyperplasia results from infection with the human pathogenic helminths Schistosoma mansoni and Schistosoma japonicum [78, 79], where it has been specifically referred to as “transitional mucosa” [14] and is the precursor lesion of dysplasia and colorectal carcinoma in infected patients [14–16].
Since colonic type goblet cell hyperplasia caused by the human pathogenic bacterium Helicobacter pylori occurs in the stomach, where colonic type goblet cells are not normally present, it is called incomplete intestinal (colonic) metaplasia and is the immediate precursor lesion of gastric cancer [80, 81].
Goblet cell hyperplasia is the rarely recognized histopathologic feature of the resolving phase of the murine pathogenic bacterium Citrobacter rodentium (Fig. 1b) [82, 83], which is an animal model of IIBD [84], epithelial-mesenchymal transition and tumorigenesis [85, 86]. Citrobacter rodentium’s effects on and interactions with goblet cells have been documented to cause the more well-known pathologic features of transmissible murine colonic hyperplasia, including the elongation of crypts, “depletion” of the mucinogen granule compartment and variable shapes of the goblet cells (Fig. 1a) [87, 88].
Fig. 1.
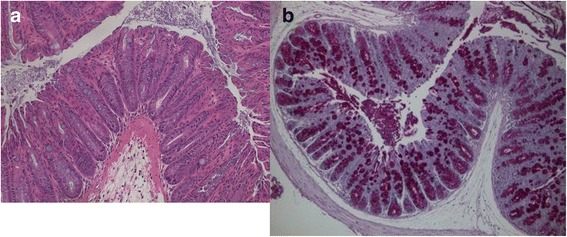
Goblet cell changes in Citrobacter rodentium infection. a The well-known pathologic features of Citrobacter rodentium infection include crypt elongation, and variation in shape and “depletion” of the apical mucinogen granule compartment of goblet cells. (H&E, original magnification ×200) b Goblet cell hyperplasia is the rarely recognized pathologic feature of the resolving phase of Citrobacter rodentium infection. (PAS, original magnification ×200) Photomicrographs courtesy of Dr. Bruce Vallance
MAP causes goblet cell hyperplasia
A single article demonstrates MAP flooding into and hovering in clouds above human intestinal goblet cells [89]. MAP attaches to and invades bovine intestinal goblet cells [90, 91] and causes acute [91] and chronic [92] goblet cell hyperplasia.
The persistence of a microorganism within infected tissues is one way that microorganism causes cancer, with proposed carcinogenic mechanisms including cycles of chronic inflammation and repair, chronic hyperplasia (‘proliferation’) which destabilizes DNA and suppression of apoptosis [2, 3].
MAP has been accidentally discovered in the intestines of patients with sporadic colorectal cancer
A follow-up to an article demonstrating that MAP organisms are small and require oil immersion (×100 oil immersion objective or ×1000 total magnification) to be identified by light microscopy [93] identified Mycobacterium avium organisms (of which MAP is a subspecies) in two of three control patients with sporadic colorectal cancer [94].
Conclusion: The possibility that MAP causes colorectal cancer is a testable hypothesis
MAP organisms may be concentrated [95] in the following locations:
in the extracellular mucus that is a prominent component of the goblet cell hyperplasia lesion and mucinous and serrated carcinomas, and comprises the “mucus cap” [96, 97] or “coat” [98] of sessile serrated adenomas, contravening current recommendations [43, 98] to carefully wash off this prominent histopathologic feature.
within the hypertrophic apical granule compartment of the hyperplastic goblet cells lining the goblet cell hyperplasia lesion.
in the lamina propria and submucosa of the goblet cell hyperplasia lesion and adenomas.
within the tumor stroma of colorectal cancers.
MAP can also be identified in humans by culture, polymerase chain reaction and antibody evaluations of tissue, blood and stool [99–107].
Acknowledgements
My research would not be possible without the assistance of librarians past (Sandy Keno, Gail Leong and Kathryn Kane) and present (Dr. Beth Hill) at the Providence Sacred Heart Medical Center and Children’s Hospital’s Health Sciences Library in Spokane, Washington, now part of the Providence Library system, as well as the other libraries that participate in the FreeShare Library group within the Docline National Network of Libraries of Medicine. Dr. Bruce Vallance very kindly provided the photomicrographs for Fig. 1. Thank you to Judi Heidel of Perfectly Clear Copyediting Services for editing this paper.
Dedicated to the memory of Cyrus E. Rubin, M.D., mentor and friend.
Funding
None
Availability of data and materials
Not applicable
Abbreviations
- IIBD
Idiopathic inflammatory bowel disease
- H&E
Hematoxylin and eosin
- MAP
Mycobacterium avium subspecies paratuberculosis
- PAS
Periodic Acid-Schiff
Additional file
Descriptions and illustrations of the goblet cell hyperplasia lesion. The supplementary file discusses the descriptions and illustrations of the goblet cell hyperplasia lesion found in some of the references in the main text. (DOC 200 kb)
Authors’ contributions
Not applicable
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The author declares that no competing interests exist.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s13027-017-0172-3) contains supplementary material, which is available to authorized users.
References
- 1.Kuper H, Adami HO, Trichopoulos D. Infections as a major preventable cause of human cancer. J Intern Med. 2000;248:171–183. doi: 10.1046/j.1365-2796.2000.00742.x. [DOI] [PubMed] [Google Scholar]
- 2.Lax AJ, Thomas W. How bacteria could cause cancer: one step at a time. Trends Microbiol. 2002;10:293–299. doi: 10.1016/s0966-842x(02)02360-0. [DOI] [PubMed] [Google Scholar]
- 3.Vennervald BJ, Polman K. Helminths and malignancy. Parasite Immunol. 2009;31:686–696. doi: 10.1111/j.1365-3024.2009.01163.x. [DOI] [PubMed] [Google Scholar]
- 4.Clarke CJ. The pathology and pathogenesis of paratuberculosis in ruminants and other species. J Comp Pathol. 1997;116:217–261. doi: 10.1016/s0021-9975(97)80001-1. [DOI] [PubMed] [Google Scholar]
- 5.Kuenstner JT, Naser S, Chamberlin W, Borody T, Graham DY, McNees A, Hermon-Taylor J, Hermon-Taylor A, Dow CT, Thayer W, et al: The consensus from the Mycobacterium Avium Ssp. paratuberculosis (MAP) conference 2017. Front Public Health 2017;5:208. [DOI] [PMC free article] [PubMed]
- 6.Davis WC, Kuenstner JT, Singh SV: Resolution of Crohn's (Johne's) disease with antibiotics: what are the next steps? Expert Rev Gastroenterol Hepatol 2017;11:393-396. [DOI] [PubMed]
- 7.Pierce ES. Ulcerative colitis and Crohn's disease: is Mycobacterium Avium subspecies paratuberculosis the common villain? Gut Pathog. 2010;2:21. doi: 10.1186/1757-4749-2-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim ER, Chang DK. Colorectal cancer in inflammatory bowel disease: the risk, pathogenesis, prevention and diagnosis. World J Gastroenterol. 2014;20:9872–9881. doi: 10.3748/wjg.v20.i29.9872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi PM, Zelig MP. Similarity of colorectal cancer in Crohn's disease and ulcerative colitis: implications for carcinogenesis and prevention. Gut. 1994;35:950–954. doi: 10.1136/gut.35.7.950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lombard JE, Gardner IA, Jafarzadeh SR, Fossler CP, Harris B, Capsel RT, Wagner BA, Johnson WO. Herd-level prevalence of Mycobacterium Avium subsp. paratuberculosis infection in United States dairy herds in 2007. Prev Vet Med. 2013;108:234–238. doi: 10.1016/j.prevetmed.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Rhodes G, Henrys P, Thomson BC, Pickup RW. Mycobacterium Avium subspecies paratuberculosis is widely distributed in British soils and waters: implications for animal and human health. Environ Microbiol. 2013;15:2761–2774. doi: 10.1111/1462-2920.12137. [DOI] [PubMed] [Google Scholar]
- 12.King DN, Donohue MJ, Vesper SJ, Villegas EN, Ware MW, Vogel ME, Furlong EF, Kolpin DW, Glassmeyer ST, Pfaller S. Microbial pathogens in source and treated waters from drinking water treatment plants in the United States and implications for human health. Sci Total Environ. 2016;562:987–995. doi: 10.1016/j.scitotenv.2016.03.214. [DOI] [PubMed] [Google Scholar]
- 13.Rhodes JM. Unifying hypothesis for inflammatory bowel disease and associated colon cancer: sticking the pieces together with sugar. Lancet. 1996;347:40–44. doi: 10.1016/s0140-6736(96)91563-9. [DOI] [PubMed] [Google Scholar]
- 14.Ming-Chai C, Chi-Yuan C, Pei-Yu C, Jen-Chun H. Evolution of colorectal cancer in schistsosomiasis: transitional mucosal changes adjacent to large intestinal carcinoma in colectomy specimens. Cancer. 1980;46:1661–1675. doi: 10.1002/1097-0142(19801001)46:7<1661::aid-cncr2820460728>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 15.Madbouly KM, Senagore AJ, Mukerjee A, Hussien AM, Shehata MA, Navine P, Delaney CP, Fazio VW. Colorectal cancer in a population with endemic Schistosoma Mansoni: is this an at-risk population? Int J Color Dis. 2007;22:175–181. doi: 10.1007/s00384-006-0144-3. [DOI] [PubMed] [Google Scholar]
- 16.Wang M, QB W, He WB, Wang ZQ. Clinicopathological characteristics and prognosis of schistosomal colorectal cancer. Color Dis. 2016;18:1005–1009. doi: 10.1111/codi.13317. [DOI] [PubMed] [Google Scholar]
- 17.Filipe MI. Value of histochemical reactions for mucosubstances in the diagnosis of certain pathological conditions of the colon and rectum. Gut. 1969;10:577–586. doi: 10.1136/gut.10.7.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Filipe MI, Branfoot AC. Abnormal patterns of mucus secretion in apparently normal mucosa of large intestine with carcinoma. Cancer. 1974;34:282–290. doi: 10.1002/1097-0142(197408)34:2<282::aid-cncr2820340211>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 19.Greaves P, Filipe MI, Branfoot AC. Transitional mucosa and survival in human colorectal cancer. Cancer. 1980;46:764–770. doi: 10.1002/1097-0142(19800815)46:4<764::aid-cncr2820460421>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 20.Sundblad AS, Paz RA. Mucinous carcinomas of the colon and rectum and their relation to polyps. Cancer. 1982;50:2504–2509. doi: 10.1002/1097-0142(19821201)50:11<2504::aid-cncr2820501141>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 21.Heilmann KL, Schmidbauer G, Schyma G. The transitional polyp of the colorectal mucosa. Pathol Res Pract. 1987;182:690–693. [PubMed] [Google Scholar]
- 22.Pretlow TP, Barrow BJ, Ashton WS, O'Riordan MA, Pretlow TG, Jurcisek JA, Stellato TA. Aberrant crypts: putative preneoplastic foci in human colonic mucosa. Cancer Res. 1991;51:1564–1567. [PubMed] [Google Scholar]
- 23.Pretlow TP, O'Riordan MA, Pretlow TG, Stellato TA. Aberrant crypts in human colonic mucosa: putative preneoplastic lesions. J Cell Biochem Suppl. 1992;16G:55–62. doi: 10.1002/jcb.240501111. [DOI] [PubMed] [Google Scholar]
- 24.Roncucci L, Stamp D, Medline A, Cullen JB, Bruce WR. Identification and quantification of aberrant crypt foci and microadenomas in the human colon. Hum Pathol. 1991;22:287–294. doi: 10.1016/0046-8177(91)90163-j. [DOI] [PubMed] [Google Scholar]
- 25.Roncucci L, Medline A, Bruce WR. Classification of aberrant crypt foci and microadenomas in human colon. Cancer Epidemiol Biomarkers Prev. 1991;1:57–60. [PubMed] [Google Scholar]
- 26.Torlakovic E, Skovlund E, Snover DC, Torlakovic G, Nesland JM. Morphologic reappraisal of serrated colorectal polyps. Am J Surg Pathol. 2003;27:65–81. doi: 10.1097/00000478-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Van Patter WN, Bargen JA, Dockerty MB, Feldman WH, Mayo CW, Waugh JM. Regional enteritis. Gastroenterology. 1954;26:347–450. [PubMed] [Google Scholar]
- 28.Dvorak AM, Connell AB, Dickersin GR. Crohn's disease: a scanning electron microscopic study. Hum Pathol. 1979;10:165–177. doi: 10.1016/s0046-8177(79)80006-4. [DOI] [PubMed] [Google Scholar]
- 29.Nagel E, Bartels M, Pichlmayr R. Scanning electron-microscopic lesions in Crohn's disease: relevance for the interpretation of postoperative recurrence. Gastroenterology. 1995;108:376–382. doi: 10.1016/0016-5085(95)90063-2. [DOI] [PubMed] [Google Scholar]
- 30.Kilgore SP, Sigel JE, Goldblum JR. Hyperplastic-like mucosal change in Crohn's disease: an unusual form of dysplasia? Modern Pathol. 2000;13:797–801. doi: 10.1038/modpathol.3880138. [DOI] [PubMed] [Google Scholar]
- 31.Shnitka TK. Current concepts of the pathogenesis and pathology of inflammatory lesions of the intestine. Can Med Assoc J. 1964;91:7–22. [PMC free article] [PubMed] [Google Scholar]
- 32.Vaiphei K, Saha M, Sharma BC, Bhasin DK, Singh K. Goblet cell status in idiopathic ulcerative colitis--implication in surveillance program. Indian J Pathol Microbiol. 2004;47:16–21. [PubMed] [Google Scholar]
- 33.Andersen SN, Lovig T, Clausen OP, Bakka A, Fausa O, Rognum TO. Villous, hypermucinous mucosa in long standing ulcerative colitis shows high frequency of K-ras mutations. Gut. 1999;45:686–692. doi: 10.1136/gut.45.5.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jass JR, Sugihara K, Love SB. Basis of sialic acid heterogeneity in ulcerative colitis. J Clin Pathol. 1988;41:388–392. doi: 10.1136/jcp.41.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jass JR, England J, Miller K. Value of mucin histochemistry in follow up surveillance of patients with long standing ulcerative colitis. J Clin Pathol. 1986;39:393–398. doi: 10.1136/jcp.39.4.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Takayama T, Katsuki S, Takahashi Y, Ohi M, Nojiri S, Sakamaki S, Kato J, Kogawa K, Miyake H, Niitsu Y. Aberrant crypt foci of the colon as precursors of adenoma and cancer. N Engl J Med. 1998;339:1277–1284. doi: 10.1056/NEJM199810293391803. [DOI] [PubMed] [Google Scholar]
- 37.Leslie A, Carey FA, Pratt NR, Steele RJ. The colorectal adenoma-carcinoma sequence. Br J Surg. 2002;89:845–860. doi: 10.1046/j.1365-2168.2002.02120.x. [DOI] [PubMed] [Google Scholar]
- 38.Lanza G, Jr, Altavilla G, Cavazzini L, Negrini R. Colonic mucosa adjacent to adenomas and hyperplastic polyps--a morphological and histochemical study. Histopathology. 1985;9:857–873. doi: 10.1111/j.1365-2559.1985.tb02871.x. [DOI] [PubMed] [Google Scholar]
- 39.Fenoglio-Preiser CM, Hutter RV. Colorectal polyps: pathologic diagnosis and clinical significance. CA Cancer J Clin. 1985;35:322–344. doi: 10.3322/canjclin.35.6.322. [DOI] [PubMed] [Google Scholar]
- 40.Dawson PA, Filipe MI. An ultrastructural and histochemical study of the mucous membrane adjacent to and remote from carcinoma of the colon. Cancer. 1976;37:2388–2398. doi: 10.1002/1097-0142(197605)37:5<2388::aid-cncr2820370531>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 41.Shamsuddin AK, Weiss L, Phelps PC, Trump BF. Colon epithelium. IV. Human colon carcinogenesis. Changes in human colon mucosa adjacent to and remote from carcinomas of the colon. J Natl Cancer Inst. 1981;66:413–419. [PubMed] [Google Scholar]
- 42.Patel A, Tripathi G, Gopalakrishnan K, Williams N, Arasaradnam RP. Field cancerisation in colorectal cancer: a new frontier or pastures past? World J Gastroenterol. 2015;21:3763–3772. doi: 10.3748/wjg.v21.i13.3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rex DK, Ahnen DJ, Baron JA, Batts KP, Burke CA, Burt RW, Goldblum JR, Guillem JG, Kahi CJ, Kalady MF, et al. Serrated lesions of the colorectum: review and recommendations from an expert panel. The American journal of gastroenterology. 2012;107:1315–1329. doi: 10.1038/ajg.2012.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Batts KP. The pathology of serrated colorectal neoplasia: practical answers for common questions. Modern Pathol. 2015;28(Suppl 1):S80–S87. doi: 10.1038/modpathol.2014.130. [DOI] [PubMed] [Google Scholar]
- 45.Garcia-Solano J, Perez-Guillermo M, Conesa-Zamora P, Acosta-Ortega J, Trujillo-Santos J, Cerezuela-Fuentes P, Makinen MJ. Clinicopathologic study of 85 colorectal serrated adenocarcinomas: further insights into the full recognition of a new subset of colorectal carcinoma. Hum Pathol. 2010;41:1359–1368. doi: 10.1016/j.humpath.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 46.Yamane L, Scapulatempo-Neto C, Reis RM, Guimaraes DP. Serrated pathway in colorectal carcinogenesis. World J Gastroenterol. 2014;20:2634–2640. doi: 10.3748/wjg.v20.i10.2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Franzin G, Scarpa A, Dina R, Zamboni G, Fratton A. Transitional polyps of the colon. Endoscopy. 1982;14:174–175. doi: 10.1055/s-2007-1021613. [DOI] [PubMed] [Google Scholar]
- 48.Ansher AF, Lewis JH, Fleischer DE, Cattau EL, Jr, Collen MJ, O'Kieffe DA, Korman LY, Benjamin SB. Hyperplastic colonic polyps as a marker for adenomatous colonic polyps. Am J Gastroenterol. 1989;84:113–117. [PubMed] [Google Scholar]
- 49.Rosenberg DW, Yang S, Pleau DC, Greenspan EJ, Stevens RG, Rajan TV, Heinen CD, Levine J, Zhou Y, O'Brien MJ. Mutations in BRAF and KRAS differentially distinguish serrated versus non-serrated hyperplastic aberrant crypt foci in humans. Cancer Res. 2007;67:3551–3554. doi: 10.1158/0008-5472.CAN-07-0343. [DOI] [PubMed] [Google Scholar]
- 50.Cheng L, Lai MD. Aberrant crypt foci as microscopic precursors of colorectal cancer. World J Gastroenterol. 2003;9:2642–2649. doi: 10.3748/wjg.v9.i12.2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siu IM, Pretlow TG, Amini SB, Pretlow TP. Identification of dysplasia in human colonic aberrant crypt foci. Am J Pathol. 1997;150:1805–1813. [PMC free article] [PubMed] [Google Scholar]
- 52.Kuramoto S, Oohara T. Minute cancers arising de novo in the human large intestine. Cancer. 1988;61:829–834. doi: 10.1002/1097-0142(19880215)61:4<829::aid-cncr2820610431>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 53.Atwaibi M, Batts KP, Weinberg DI, McCabe RP. Mo1705 Flat Serrated Change: Does it Predict the Development of Colonic Mucosal Dysplasia in Inflammatory Bowel Disease? Gastroenterology. 2012;142:S-665. [Google Scholar]
- 54.Johnson DH, Khanna S, Smyrk TC, Loftus EV, Jr, Anderson KS, Mahoney DW, Ahlquist DA, Kisiel JB. Detection rate and outcome of colonic serrated epithelial changes in patients with ulcerative colitis or Crohn's colitis. Aliment Pharmacol Ther. 2014;39:1408–1417. doi: 10.1111/apt.12774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Parian AM, Koh JM, Badamas J, Giardiello FM, Montgomery EA, Lazarev M. 42 Serrated Epithelial Changes Are Associated With Colorectal Dysplasia in Inflammatory Bowel Disease. Gastroenterology. 2013;144:S-11. [Google Scholar]
- 56.Parian A, Koh J, Limketkai BN, Eluri S, Rubin DT, Brant SR, Ha CY, Bayless TM, Giardiello F, Hart J, et al: Association between serrated epithelial changes and colorectal dysplasia in inflammatory bowel disease. Gastrointest Endosc 2016;84:87-95 e81. [DOI] [PMC free article] [PubMed]
- 57.Matkowskyj KA, Chen ZE, Rao MS, Yang GY. Dysplastic lesions in inflammatory bowel disease: molecular pathogenesis to morphology. Arch Pathol Lab Med. 2013;137:338–350. doi: 10.5858/arpa.2012-0086-RA. [DOI] [PubMed] [Google Scholar]
- 58.Blackstone MO, Riddell RH, Rogers BH, Levin B. Dysplasia-associated lesion or mass (DALM) detected by colonoscopy in long-standing ulcerative colitis: an indication for colectomy. Gastroenterology. 1981;80:366–374. [PubMed] [Google Scholar]
- 59.Torres C, Antonioli D, Odze RD. Polypoid dysplasia and adenomas in inflammatory bowel disease: a clinical, pathologic, and follow-up study of 89 polyps from 59 patients. Am J Surg Pathol. 1998;22:275–284. doi: 10.1097/00000478-199803000-00001. [DOI] [PubMed] [Google Scholar]
- 60.Engelsgjerd M, Farraye FA, Odze RD. Polypectomy may be adequate treatment for adenoma-like dysplastic lesions in chronic ulcerative colitis. Gastroenterology. 1999;117:1288–1294. doi: 10.1016/s0016-5085(99)70278-7. [DOI] [PubMed] [Google Scholar]
- 61.Quinn AM, Farraye FA, Naini BV, Cerda S, Coukos J, Li Y, Khor T, Odze RD. Polypectomy is adequate treatment for adenoma-like dysplastic lesions (DALMs) in Crohn's disease. Inflamm Bowel Dis. 2013;19:1186–1193. doi: 10.1097/MIB.0b013e318280e749. [DOI] [PubMed] [Google Scholar]
- 62.Neumann H, Vieth M, Langner C, Neurath MF, Mudter J. Cancer risk in IBD: how to diagnose and how to manage DALM and ALM. World J Gastroenterol. 2011;17:3184–3191. doi: 10.3748/wjg.v17.i27.3184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bossard C, Denis MG, Bezieau S, Bach-Ngohou K, Bourreille A, Laboisse CL, Mosnier JF. Involvement of the serrated neoplasia pathway in inflammatory bowel disease-related colorectal oncogenesis. Oncol Rep. 2007;18:1093–1097. [PubMed] [Google Scholar]
- 64.Shen J, Gibson JA, Schulte S, Khurana H, Farraye FA, Levine J, Burakoff R, Cerda S, Qazi T, Hamilton M, et al. Clinical, pathologic, and outcome study of hyperplastic and sessile serrated polyps in inflammatory bowel disease. Hum Pathol. 2015;46:1548–1556. doi: 10.1016/j.humpath.2015.06.019. [DOI] [PubMed] [Google Scholar]
- 65.Geboes K, De Hertogh G, Bisschops R, Geboes K. Flat adenomas, significance, detection, treatment. Ann Gastroenterol. 2010;23:266–269. [Google Scholar]
- 66.Naravadi V, Gupta N, Early D, Jonnalagadda S, Wani SB, Gaddam S, Sharma P, Edmundowicz SA, Bansal A, Rastogi A. Prevalence of advanced histological features and synchronous neoplasia in patients with flat adenomas. Gastrointest Endosc. 2016;83:795–799. doi: 10.1016/j.gie.2015.08.040. [DOI] [PubMed] [Google Scholar]
- 67.Zhan T, Hahn F, Hielscher T, Betge J, Kahler G, Ebert MP, Belle S. Frequent co-occurrence of high-grade dysplasia in large flat colonic polyps (>20 mm) and synchronous polyps. BMC Gastroenterol. 2015;15:82. doi: 10.1186/s12876-015-0312-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Olubuyide IO, Bristol JB, Williamson RC. Goblet cell changes during intestinal adaptation to azoxymethane and enteric bypass in the rat. Br J Cancer. 1985;51:383–388. doi: 10.1038/bjc.1985.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Haxhija EQ, Yang H, Spencer AU, Sun X, Teitelbaum DH. Intestinal epithelial cell proliferation is dependent on the site of massive small bowel resection. Pediatr Surg Int. 2007;23:379–390. doi: 10.1007/s00383-006-1855-9. [DOI] [PubMed] [Google Scholar]
- 70.Deplancke B, Gaskins HR. Microbial modulation of innate defense: goblet cells and the intestinal mucus layer. Am J Clin Nutr. 2001;73:1131S–1141S. doi: 10.1093/ajcn/73.6.1131S. [DOI] [PubMed] [Google Scholar]
- 71.Kim YS, Ho SB. Intestinal goblet cells and mucins in health and disease: recent insights and progress. Curr Gastroenterol Rep. 2010;12:319–330. doi: 10.1007/s11894-010-0131-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ponce-Macotela M, Gonzalez-Maciel A, Reynoso-Robles R, Martinez-Gordillo MN. Goblet cells: are they an unspecific barrier against Giardia Intestinalis or a gate? Parasitol Res. 2008;102:509–513. doi: 10.1007/s00436-007-0790-6. [DOI] [PubMed] [Google Scholar]
- 73.Knight PA, Brown JK, Pemberton AD. Innate immune response mechanisms in the intestinal epithelium: potential roles for mast cells and goblet cells in the expulsion of adult Trichinella spiralis. Parasitology. 2008;135:655–670. doi: 10.1017/S0031182008004319. [DOI] [PubMed] [Google Scholar]
- 74.Soga K, Yamauchi J, Kawai Y, Yamada M, Uchikawa R, Tegoshi T, Mitsufuji S, Yoshikawa T, Arizono N. Alteration of the expression profiles of acidic mucin, sialytransferase, and sulfotransferases in the intestinal epithelium of rats infected with the nematode Nippostrongylus brasiliensis. Parasitol Res. 2008;103:1427–1434. doi: 10.1007/s00436-008-1152-8. [DOI] [PubMed] [Google Scholar]
- 75.Moro K, Yamada T, Tanabe M, Takeuchi T, Ikawa T, Kawamoto H, Furusawa J, Ohtani M, Fujii H, Koyasu S. Innate production of T(H)2 cytokines by adipose tissue-associated c-kit(+)Sca-1(+) lymphoid cells. Nature. 2010;463:540–544. doi: 10.1038/nature08636. [DOI] [PubMed] [Google Scholar]
- 76.Mantle M, Atkins E, Kelly J, Thakore E, Buret A, Gall DG. Effects of Yersinia enterocolitica infection on rabbit intestinal and colonic goblet cells and mucin: morphometrics, histochemistry, and biochemistry. Gut. 1991;32:1131–1138. doi: 10.1136/gut.32.10.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yang JY, Lee SN, Chang SY, Ko HJ, Ryu S, Kweon MN. A mouse model of shigellosis by intraperitoneal infection. J Infect Dis. 2014;209:203–215. doi: 10.1093/infdis/jit399. [DOI] [PubMed] [Google Scholar]
- 78.Marillier RG, Michels C, Smith EM, Fick LC, Leeto M, Dewals B, Horsnell WG, Brombacher F. IL-4/IL-13 independent goblet cell hyperplasia in experimental helminth infections. BMC Immunol. 2008;9:11. doi: 10.1186/1471-2172-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Couto JL, Ferreira Hda S, da Rocha DB, Duarte ME, Assuncao ML, Coutinho Ede M. Structural changes in the jejunal mucosa of mice infected with Schistosoma Mansoni, fed low or high protein diets. Rev Soc Bras Med Trop. 2002;35:601–607. doi: 10.1590/s0037-86822002000600010. [DOI] [PubMed] [Google Scholar]
- 80.Correa P, Houghton J. Carcinogenesis of helicobacter pylori. Gastroenterology. 2007;133:659–672. doi: 10.1053/j.gastro.2007.06.026. [DOI] [PubMed] [Google Scholar]
- 81.Semino-Mora C, Doi SQ, Marty A, Simko V, Carlstedt I, Dubois A. Intracellular and interstitial expression of helicobacter pylori virulence genes in gastric precancerous intestinal metaplasia and adenocarcinoma. J Infect Dis. 2003;187:1165–1177. doi: 10.1086/368133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Barthold SW, Coleman GL, Jacoby RO, Livestone EM, Jonas AM. Transmissible murine colonic hyperplasia. Vet Pathol. 1978;15:223–236. doi: 10.1177/030098587801500209. [DOI] [PubMed] [Google Scholar]
- 83.Bergstrom KS, Morampudi V, Chan JM, Bhinder G, Lau J, Yang H, Ma C, Huang T, Ryz N, Sham HP, et al. Goblet cell derived RELM-beta recruits CD4+ T cells during infectious colitis to promote protective intestinal epithelial cell proliferation. PLoS Pathog. 2015;11:e1005108. doi: 10.1371/journal.ppat.1005108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Higgins LM, Frankel G, Douce G, Dougan G, MacDonald TT. Citrobacter rodentium infection in mice elicits a mucosal Th1 cytokine response and lesions similar to those in murine inflammatory bowel disease. Infect Immun. 1999;67:3031–3039. doi: 10.1128/iai.67.6.3031-3039.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chandrakesan P, Roy B, Jakkula LU, Ahmed I, Ramamoorthy P, Tawfik O, Papineni R, Houchen C, Anant S, Umar S. Utility of a bacterial infection model to study epithelial-mesenchymal transition, mesenchymal-epithelial transition or tumorigenesis. Oncogene. 2014;33:2639–2654. doi: 10.1038/onc.2013.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Newman JV, Kosaka T, Sheppard BJ, Fox JG, Schauer DB. Bacterial infection promotes colon tumorigenesis in Apc(min/+) mice. J Infect Dis. 2001;184:227–230. doi: 10.1086/321998. [DOI] [PubMed] [Google Scholar]
- 87.Bergstrom KS, Guttman JA, Rumi M, Ma C, Bouzari S, Khan MA, Gibson DL, Vogl AW, Vallance BA. Modulation of intestinal goblet cell function during infection by an attaching and effacing bacterial pathogen. Infect Immun. 2008;76:796–811. doi: 10.1128/IAI.00093-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chan JM, Bhinder G, Sham HP, Ryz N, Huang T, Bergstrom KS, Vallance BA. CD4+ T cells drive goblet cell depletion during Citrobacter rodentium infection. Infect Immun. 2013;81:4649–4658. doi: 10.1128/IAI.00655-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Golan L, Livneh-Kol A, Gonen E, Yagel S, Rosenshine I, Shpigel NY. Mycobacterium Avium paratuberculosis invades human small-intestinal goblet cells and elicits inflammation. J Infect Dis. 2009;199:350–354. doi: 10.1086/596033. [DOI] [PubMed] [Google Scholar]
- 90.Schleig PM, Buergelt CD, Davis JK, Williams E, Monif GR, Davidson MK. Attachment of Mycobacterium Avium subspecies paratuberculosis to bovine intestinal organ cultures: method development and strain differences. Vet Microbiol. 2005;108:271–279. doi: 10.1016/j.vetmic.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 91.Khare S, Nunes JS, Figueiredo JF, Lawhon SD, Rossetti CA, Gull T, Rice-Ficht AC, Adams LG. Early phase morphological lesions and transcriptional responses of bovine ileum infected with Mycobacterium Avium subsp. paratuberculosis. Vet Pathol. 2009;46:717–728. doi: 10.1354/vp.08-VP-0187-G-FL. [DOI] [PubMed] [Google Scholar]
- 92.Charavaryamath C, Gonzalez-Cano P, Fries P, Gomis S, Doig K, Scruten E, Potter A, Napper S, Griebel PJ. Host responses to persistent Mycobacterium Avium subspecies paratuberculosis infection in surgically isolated bovine ileal segments. Clin Vac Immunol. 2013;20:156–165. doi: 10.1128/CVI.00496-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jeyanathan M, Alexander DC, Turenne CY, Girard C, Behr MA. Evaluation of in situ methods used to detect Mycobacterium Avium subsp. paratuberculosis in samples from patients with Crohn's disease. J Clin Microbiol. 2006;44:2942–2950. doi: 10.1128/JCM.00585-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jeyanathan M, Boutros-Tadros O, Radhi J, Semret M, Bitton A, Behr MA. Visualization of Mycobacterium Avium in Crohn's tissue by oil-immersion microscopy. Microbes Infect. 2007;9:1567–1573. doi: 10.1016/j.micinf.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 95.Pierce ES. Where are all the Mycobacterium Avium subspecies paratuberculosis in patients with Crohn's disease? PLoS Pathog. 2009;5:e1000234. doi: 10.1371/journal.ppat.1000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lee EJ, Kim MJ, Chun SM, Jang SJ, Kim DS, Lee DH, Youk EG. Sessile serrated adenoma/polyps with a depressed surface: a rare form of sessile serrated adenoma/polyp. Diagn Pathol. 2015;10:75. doi: 10.1186/s13000-015-0325-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pereyra L, Gomez EJ, Gonzalez R, Fischer C, Erana GB, Torres AG, Correa L, Mella JM, Panigadi GN, Luna P, et al. Finding sessile serrated adenomas: is it possible to identify them during conventional colonoscopy? Dig Dis Sci. 2014;59:3021–3026. doi: 10.1007/s10620-014-3295-z. [DOI] [PubMed] [Google Scholar]
- 98.Sweetser S, Smyrk TC, Sugumar A. Serrated polyps: critical precursors to colorectal cancer. Expert Rev Gastroenterol Hepatol. 2011;5:627–635. doi: 10.1586/egh.11.67. [DOI] [PubMed] [Google Scholar]
- 99.Naser SA, Ghobrial G, Romero C, Valentine JF. Culture of Mycobacterium Avium subspecies paratuberculosis from the blood of patients with Crohn's disease. Lancet. 2004;364:1039–1044. doi: 10.1016/S0140-6736(04)17058-X. [DOI] [PubMed] [Google Scholar]
- 100.Timms VJ, Daskalopoulos G, Mitchell HM, Neilan BA. The association of Mycobacterium Avium subsp. paratuberculosis with inflammatory bowel disease. PLoS One. 2016;11:e0148731. doi: 10.1371/journal.pone.0148731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Singh AV, Singh SV, Makharia GK, Singh PK, Sohal JS. Presence and characterization of Mycobacterium Avium subspecies paratuberculosis from clinical and suspected cases of Crohn's disease and in the healthy human population in India. Int J Infect Dis. 2008;12:190–197. doi: 10.1016/j.ijid.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 102.Banche G, Allizond V, Sostegni R, Lavagna A, Bergallo M, Sidoti F, Daperno M, Rocca R, Cuffini AM. Application of multiple laboratory tests for Mycobacterium Avium Ssp. paratuberculosis detection in Crohn's disease patient specimens. New Microbiol. 2015;38:357–367. [PubMed] [Google Scholar]
- 103.Singh SV, Kumar N, Sohal JS, Singh AV, Singh PK, Agrawal ND, Gupta S, Chaubey KK, Kumar A, Rawat KD. First mass screening of the human population to estimate the bio-load of Mycobacterium Avium subspecies paratuberculosis in North India. J Biol Sci. 2014;14:237. [Google Scholar]
- 104.Singh SV, Kuenstner JT, Davis WC, Agarwal P, Kumar N, Singh D, Gupta S, Chaubey KK, Kumar A, Misri J, et al. Concurrent resolution of chronic diarrhea likely due to Crohn's disease and infection with Mycobacterium Avium paratuberculosis. Front Med. 2016;3:49. doi: 10.3389/fmed.2016.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tuci A, Tonon F, Castellani L, Sartini A, Roda G, Marocchi M, Caponi A, Munarini A, Rosati G, Ugolini G, et al. Fecal detection of Mycobacterium Avium paratuberculosis using the IS900 DNA sequence in Crohn's disease and ulcerative colitis patients and healthy subjects. Dig Dis Sci. 2011;56:2957–2962. doi: 10.1007/s10620-011-1699-6. [DOI] [PubMed] [Google Scholar]
- 106.Feller M, Huwiler K, Stephan R, Altpeter E, Shang A, Furrer H, Pfyffer GE, Jemmi T, Baumgartner A, Egger M. Mycobacterium Avium subspecies paratuberculosis and Crohn's disease: a systematic review and meta-analysis. Lancet Infect Dis. 2007;7:607–613. doi: 10.1016/S1473-3099(07)70211-6. [DOI] [PubMed] [Google Scholar]
- 107.Abubakar I, Myhill D, Aliyu SH, Hunter PR. Detection of Mycobacterium Avium subspecies paratuberculosis from patients with Crohn's disease using nucleic acid-based techniques: a systematic review and meta-analysis. Inflamm Bowel Dis. 2008;14:401–410. doi: 10.1002/ibd.20276. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable


