Abstract
A circumcising incision to deglove the penis for penile prosthesis (PP) implantation can increase the risk of ischemic injury to the glans penis. In order to avoid vascular complications, we describe a novel technique utilizing a ventral incision to perform the PP implantation and a double-dorsal patch graft, or “sliding technique” (ST), in patients with severe Peyronie's disease (PD). Three patients with severe PD and erectile dysfunction at our institution underwent ST and PP implantation through a ventral incision. This new approach was not only successful in facilitating the ST and PP implantation in these patients but also allowed for adequate exposure of the penile shaft with no reported loss of sensation. We also conducted a review of current literature regarding the approaches for PD. While ischemic complications of PP implantation and ST are rare, there are reports of ischemic injury in patients undergoing a circumcising incision. The combination of a circumcising incision and a patient's underlying peripheral artery disease potentially raises a patient's risk of this rare complication. Our innovative ventral incision provides an alternative method for PP implantation and ST in order to avoid ischemia of the penis, while still allowing for adequate exposure.
Peyronie's disease (PD) is a localized connective tissue disorder that results in curvature and deformity of the penis. While the exact pathophysiology of the condition is not yet known, PD is believed to be caused by chronic injury and inflammation of the penis that results in the formation of fibrous plaques in the penile tunica albuginea. These inelastic plaques alter the anatomic structure of the penis leading to painful erections, erectile dysfunction (ED), and penile deformities.1,2
Treatment options are based on the severity of the penile deformity and erectile function. While medical therapy and intralesional injections are used to correct mild deformities, persistent PD associated with severe penile deformity or ED indicates the need for surgical management. Surgical options include plication, plaque incision and grafting, and penile prosthesis (PP) implantation, with PP implantation as the treatment of choice for medically refractory PD with ED.1,2,3
In recent years, the “sliding technique” (ST) has been utilized for severe PD with ED as it allows for simultaneous PP implantation and penile length restoration.4,5 Exposure of the penile shaft for the ST is accomplished via a circumferential subcoronal incision followed by complete degloving of the penile shaft.6,7 This approach is generally preferred as it allows adequate exposure of the surgical site and allots space for deep corrective sutures. However, as the glans is the most distal aspect of the penis, it is susceptible to ischemic and lymphatic complications during degloving.8,9,10 Though rare, ischemic complications of the glans penis during PP implantation have been reported almost exclusively in patients with diabetes and peripheral vascular disease.11,12,13,14,15 To avoid these complications, we propose that a ventral incision without degloving of the penis can be a novel approach to perform the ST in patients with severe PD.
PATIENTS AND TECHNIQUE
We reviewed our database for patients who underwent PP implantation for PD and ED from January 2015 to December 2016. A total of 32 patients with severe ED and PD were treated with PP and penile plasty by a single surgeon. The etiology related to ED and PD included radical prostatectomy (65.6%, 21 patients), metabolic and vascular diseases (18.7%, 6 patients), radiation or brachytherapy for prostate cancers (9.4%, 3 patients), and radical cystectomy (6.3%, 2 patients). Among them, 62.5% (20 patients) with penile curvature <40° were treated with inflatable PP (11 AMS 700 CX [Boston Scientific, Marlborough, MA, USA] and 9 Coloplast Titan [Coloplast Corp, Minneapolis, MN, USA]) with penile modeling. 15.6% (5 patients) with penile curvature between 40° and 50° were treated with inflatable PP (1 AMS 700 CX and 4 Coloplast Titan) with penile plication. 21.9% (7 patients) with penile curvature more than 60° were treated with penile implants (6 Coloplast Titan and 1 Genesis [Coloplast Corp, Minneapolis, MN, USA]) and grafting procedure. Among the patients receiving grafting procedures, 5 patients underwent sliding penile size restoration with 3 surgeries performed through ventral incision (Figure 1 and 2) and 2 surgeries done with circumcision and degloving irrespective of the patients’ circumcision status.
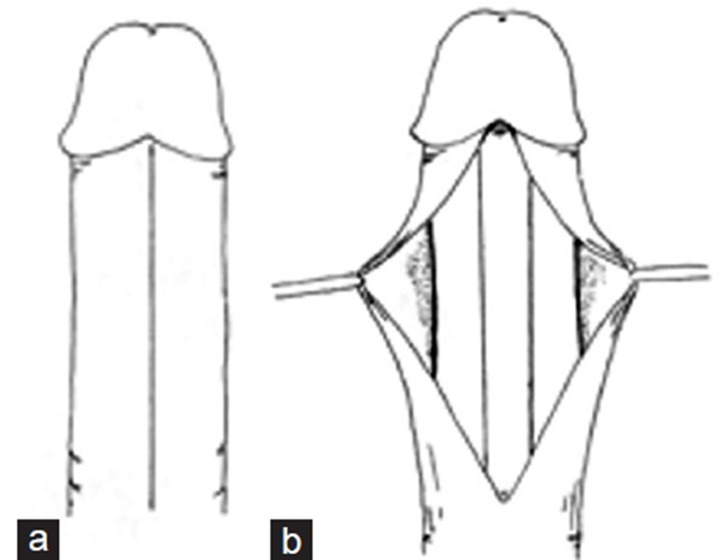
Figure 1.
(a) Ventral incision along the penile raphe from the frenulum to the base of the penile shaft. (b) Ventral incision through Buck's fascia to expose the corpus spongiosum and cavernosum.
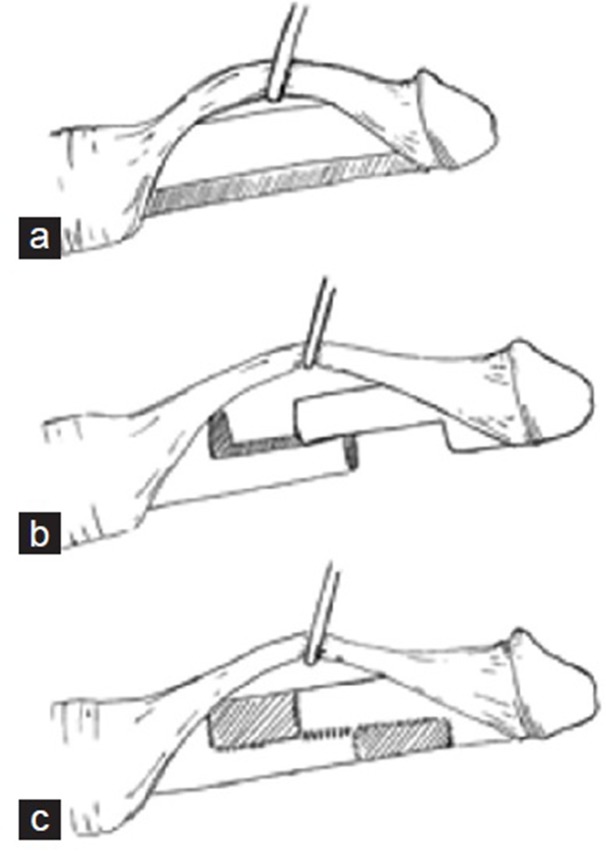
Figure 2.
Lateral view of a schematic demonstrating the sliding technique and grafting. (a) Dorsal retraction of the skin, fascia, and neurovascular bundle. (b) Stretching of penis with neurovascular bundle at maximum tension after incisions of the cavernous tissue. (c) Double dorsal-ventral patch graft after insertion of two prostheses into the cavernosa.
The patient ages ranged from 33 to 77 years old with follow-up from 6 to 18 months. Residual curvature was found in 16/20 patients (80%) in modeling group with curvature ranging from 5° to 20°. 1/5 patients (20%), who received plication, reported residual curvature of 15°. For patients treated with graft procedures, no patients had residual curvature at the first postoperation follow-up, but 1 patient (1/7, 14.3%) developed recurrent curvature of 15° at 6-month follow-up due to infrequent inflation of PP and possible graft contraction. However, only 1 patient in this entire cohort (1/32, 3.1%) was dissatisfied with the curvature correction, and all patients reported that residual/recurrent curvature did not affect their sexual activities. 50% patients reported subjective loss of penile length regardless of the penile reconstructive techniques. There was no incidence of glans ischemia. There was no sensation loss among patients receiving modeling, plication, or grafting though ventral incision. One patient with grafting procedure though circumcision reported temporal decrease of glans sensation that was resolved at the last follow-up.
COMMENT
There are three main approaches to the surgical management of chronic PD described in the literature: plication, plaque incision and grafting, and PP implantation. Each technique offers its own advantages and disadvantages. Plication techniques, such as the Nesbit procedure, are performed in order to correct the abnormal curvature of the penis due PD, but at the cost of penile length. Plaque incision and grafting is generally indicated for a shorter penis with severe deformities. However, opening the tunica albuginea can potentially worsen ED. In patients with severe PD with ED, PP implantation is the preferred treatment.1,2,3
PP implantation is the most popular and widely utilized method due to its low mechanical failure rate, high success rates from 86% to 100%, and patient preference of the procedure over oral therapy and injection.4 One nationwide US survey demonstrated that 75% of practicing urologists utilized PP for the treatment of PD.5 Penile modeling, plication, or grafting procedures can be performed when it is necessary with PP implantation depending on the severity and the deformity of the PD. Despite satisfaction rates ranging from 72% to 100%, there are still a number of drawbacks from PP including pain, diminished sensitivity, mechanical failure, and infection. Although inflatable PP corrects penile deformity and allows for adequate erectile rigidity, it does not address the loss of length. Loss of penile length has been reported in 54% of patients postoperatively and is one of the primary concerns of patients.16 Maximal sizing and postoperative rehabilitation with inflatable PP implantation have been recommended to prevent the loss of penile length in patients with severe ED unrelated to PD.17,18 Recent studies have demonstrated that the ST is an effective method to not only perform PP implantation but also restore length in patients with severe PD and ED.6,7,16,19
Rolle et al.7 conducted a multicentric study on the outcomes of the ST with complete degloving of the penile shaft in 28 patients. The ST demonstrated an intraoperative straightening of all penises, an average increase of 3.2 cm in penile length, and an overall increase in patient satisfaction rate at the expense of a slight increase in complications. Hematoma formation was the most common postoperative complication reported followed by PP infection, and profuse bleeding. This technique should be used very selectively for patient with severe penile deformity and significant loss of penile length, since the majority of patients with PD and ED can be treated with PP plus modeling, plication, or grafting procedures.20 The ST was only used in 15.6% (5/32) of patients in our cohort for complete deformity correction and size restoration.
Ischemia of the penis after PP implantation is a rare complication with only a few cases reported, making the incidence difficult to establish.11,12,13,14,15 While Rolle et al.7 did not note any ischemic complications in their cohort, the study was limited by small sample size with only 18% of enrolled patients having diabetes. Nevertheless, ischemic complications during PP implantation should be considered in patients with peripheral vascular disease. In recent reports of ischemia during PP implantation, a circumferential incision with degloving of the penis was performed to expose the cavernosum.11,12 The combination of degloving the penis and a patient's underlying peripheral vascular disease could potentially predispose patients to ischemic complications. Therefore, we report a novel technique with a ventral incision of the penis to avoid vascular complications in patients with underlying peripheral vascular disease. Other studies have demonstrated the efficacy of a ventral incision in other penile surgeries such as plication.8,9,10 To our knowledge, this is the first time a ventral incision has been utilized to perform the ST in patients with severe PD and ED needing PP and grafting. We believe that this novel approach can potentially have multiple benefits for patients. In addition to reducing the risk of ischemic complications, a ventral incision can reduce exposure to infectious organism, reduce operative time, and improve postoperative pain control. Though degloving the penis ideally improves exposure of the surgical site, our experience with this approach did not interfere with visualization or execution of the procedure. Lastly, through our limited experience, a ventral incision can potentially be a safe alternative approach to the ST. While there were no major operative complications for the three patients undergoing degloving incision, one of those patients reported a temporary decrease in sensation of the glans. On the other hand, there were no major operative, postoperative, loss of sensation, or ischemia noted during our study for the two patients undergoing a ventral incision.
CONCLUSION
The ST is an effective option to simultaneously implant a PP and restore penile length to patients with severe PD and ED. However, the use of a circumferential incision with degloving of the penis can potentially lead to unnecessary complications, especially in patients with underlying peripheral vascular disease. We believe that a ventral incision to expose the penis to perform the ST is a potentially safer option, especially for patients with peripheral artery disease. However, the true efficacy and safety of our technique is limited to our experience with three patients who underwent a ventral incision. Further studies with larger samples will be needed to evaluate the safety of this incision and compare the efficacy and complication rates of our technique with circumcising incision and degloving of the penis.
AUTHOR CONTRIBUTIONS
RW contributed to the concept of the study and the design and technique of the procedure. AF and RW drafted, revised, and approved the manuscript.
COMPETING INTERESTS
Both authors declared no competing interests.
REFERENCES
- 1.Nehra A, Alterowtiz R, Culkin DJ, Faraday MM, Hakim LS, et al. Peyronie's disease: AUA guideline. J Urol. 2015;194:745–53. doi: 10.1016/j.juro.2015.05.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levine AL, Larsen SM. Surgery for Peyronie's disease. Asian J Androl. 2013;15:27–34. doi: 10.1038/aja.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ralph D, Gonzalez-Cadavid N, Mirone V, Perovic S, Sohn M, et al. The management of Peyronie's disease: evidence-based 2010 guidelines. J Sex Med. 2010;7:2359–74. doi: 10.1111/j.1743-6109.2010.01850.x. [DOI] [PubMed] [Google Scholar]
- 4.Rajpurkar A, Dhabuwala CB. Comparison of satisfaction rates and erectile function in patients treated with sildenafil, intracavernous prostaglandin E1 and penile implant surgery for erectile dysfunction in urology practice. J Urol. 2003;170:159–63. doi: 10.1097/01.ju.0000072524.82345.6d. [DOI] [PubMed] [Google Scholar]
- 5.Shindel AW, Bullock TL, Brandes S. Urologist practice patterns in the management of Peyronie's disease: a nationwide survey. J Sex Med. 2008;5:954–64. doi: 10.1111/j.1743-6109.2007.00674.x. [DOI] [PubMed] [Google Scholar]
- 6.Rolle L, Ceruti C, Timpano M, Sedigh O, Destefanis P, et al. A new, innovative, lengthening surgical procedure for Peyronie's disease by penile prosthesis implantation with double dorsal-ventral patch graft: the ‘sliding technique’. J Sex Med. 2012;9:2389–95. doi: 10.1111/j.1743-6109.2012.02675.x. [DOI] [PubMed] [Google Scholar]
- 7.Rolle L, Falcone M, Ceruti C, Timpano M, Sedigh O, et al. A prospective multicentric international study on the surgical outcomes and patients’ satisfaction rates of the ‘sliding’ technique for end-stage Peyronie's disease with sever shortening of the penis and erectile dysfunction. BJU Int. 2016;117:814–20. doi: 10.1111/bju.13371. [DOI] [PubMed] [Google Scholar]
- 8.Dugi DD, Morey AF. Penoscrotal plication as a uniform approach to reconstruction of penile curvature. BJU Int. 2009;105:1440–4. doi: 10.1111/j.1464-410X.2009.08991.x. [DOI] [PubMed] [Google Scholar]
- 9.Adibi M, Hudak SJ, Morey AF. Penile plication without degloving enables effective correction of complex Peyronie's deformities. Urology. 2012;79:831–5. doi: 10.1016/j.urology.2011.12.036. [DOI] [PubMed] [Google Scholar]
- 10.Garaffa G, Sacca A, Christopher AN, Ralph D. Circumcision is not mandatory in penile surgery. BJU Int. 2009;105:222–4. doi: 10.1111/j.1464-410X.2009.08763.x. [DOI] [PubMed] [Google Scholar]
- 11.Gomez BG, Otero JR, Sicilia L, Alcaide EJ, Garcia-Cruz E, et al. Ischemic gangrene of the glans following penile prosthesis implantation. Case Rep Urol. 2013;2013:1–4. doi: 10.1155/2013/323574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yildirim A, Basok EK, Basaran A, Tokuc R. Gangrene of the distal penis after implantation of malleable penile prosthesis in a diabetic patient. Adv Ther. 2008;25:143–7. doi: 10.1007/s12325-008-0021-2. [DOI] [PubMed] [Google Scholar]
- 13.Bejany DE, Perito PE, Lustgarten M, Rhmy RK. Gangrene of the penis after implantation of penile prosthesis: case reports, treatment recommendations and review of the literature. J Urol. 1993;150:190–1. doi: 10.1016/s0022-5347(17)35433-2. [DOI] [PubMed] [Google Scholar]
- 14.McClellan DS, Masih BK. Gangrene of the penis as a complication of penile prosthesis. J Urol. 1985;133:862–3. doi: 10.1016/s0022-5347(17)49260-3. [DOI] [PubMed] [Google Scholar]
- 15.Kardar AH, Pettersson BA. Penile gangrene: a complication of penile prosthesis: a case report. Scand J Urol Nephrol. 1995;29:355–6. doi: 10.3109/00365599509180591. [DOI] [PubMed] [Google Scholar]
- 16.Anaissie J, Yafi FA. A Review of surgical strategies for penile prosthesis implantation in patients with Peyronie's disease. Transl Androl Urol. 2016;5:342–50. doi: 10.21037/tau.2016.04.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henry GD, Carrion R, Jennermann C, Wang R. Prospective evaluation of postoperative penile rehabilitation: penile length/girth maintenance 1 year following Coloplast Titan inflatable penile prosthesis. J Sex Med. 2015;12:1298–304. doi: 10.1111/jsm.12833. [DOI] [PubMed] [Google Scholar]
- 18.Egydio PH, Kuehhas FE. Penile lengthening and widening without grafting according to a modified ‘sliding’ technique. BJU Int. 2015;116:965–72. doi: 10.1111/bju.13065. [DOI] [PubMed] [Google Scholar]
- 19.Pryor MB, Carrion R, Wang R, Henry G. Patient satisfaction and penile morphology changes with postoperative penile rehabilitation 2 years after coloplast titan prosthesis. Asian J Androl. 2016;18:754–8. doi: 10.4103/1008-682X.163266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garaffa G, Minervini A, Christopher NA, Minhas S, Ralph DJ. The management of residual curvature after penile prosthesis implantation in men with Peyronie's disease. BJU Int. 2011;108:1152. doi: 10.1111/j.1464-410X.2010.10023.x. [DOI] [PubMed] [Google Scholar]