Abstract
Wellens’ syndrome represents critical occlusion of the proximal left anterior descending coronary artery. Electrocardiographic changes similar to Wellens’ wave are not exceptional to acute coronary occlusion and can also be seen in cardiac and non-cardiac conditions, such as left ventricular hypertrophy, persistent juvenile T wave, bundle branch blocks, cerebral haemorrhage, pulmonary oedema, pulmonary embolism, pheochromocytoma, Takotsubo syndrome, digitalis and cocaine-induced coronary vasospasm. Cocaine-induced pseudo-Wellens’ syndrome should be considered as one of the differentials, since cocaine is used frequently by young adults and can cause left anterior descending coronary vasospasm mimicking Wellens’ syndrome. Initiation of the beta-blocking agent in pseudo-Wellens’ syndrome as a part of acute coronary syndrome management can be disastrous. We illustrated a case of cocaine-induced pseudo-Wellens’ syndrome presented with typical chest pain associated with Wellenoid ECG.
Keywords: arrhythmias, cardiovascular medicine, cardiovascular system
Background
Wellens’ sign or warning (WS) has been correlated with precordial biphasic deep T wave inversion in the proximal left anterior descending (LAD) coronary artery territory in patient with unstable angina. WS heralds the devastating myocardial infarction and is important to identify early. Early detection of Wellens’ pattern ECG changes and timely management as acute coronary syndrome (ACS) can salvage massive myocardial necrosis. Underestimating seriousness of WS and proceeding with cardiac stress test can provoke massive anterior wall myocardial infarction.1–3 However, several cardiac and non-cardiac diseases including but not limited to left ventricular hypertrophy, persistent juvenile T wave, bundle branch blocks, cerebral haemorrhage, pulmonary oedema, pulmonary embolism, pheochromocytoma, Takotsubo syndrome, digitalis and cocaine-induced vasospasm can mimic Wellenoid ECG changes.4 5 Cocaine-induced proximal LAD coronary vasospasm occasionally has similar ECG changes to WS but no evidence of myocardial injury or coronary arteries occlusion. Utilisation of beta-blocking agent as a part of ACS treatment in the case of cocaine-induced pseudo-Wellens’ syndrome accentuates worsening of vasoconstriction due to unopposed alpha-adrenergic effect.6–12 The diagnosis of pseudo-Wellens’ syndrome can only be reached after excluding proximal LAD artery occlusion by coronary angiography. It is important for the physician to consider pseudo-Wellens’ syndrome as a differential because the use of beta-blocker in cocaine-induced proximal LAD coronary vasospasm can result in fatal outcome.
Case presentation
A 52-year-old African-American man presented with recurrent chest pain, intractable nausea and vomiting for 1 day. The chest pain was on the left side, substernal, sharp in nature, radiated to left arm, aggravated by exertion, relieved by rest, lasted for 20 minutes and associated with nausea, vomiting, light-headedness and diaphoresis. He experienced recurrent episodes of same pattern chest pain over 24 hours. He confessed smoking two to three bags of cocaine (equivalent to 3–4 g) approximately 2 hours prior to the onset of chest pain. He reported having occasional chest discomfort which subsided spontaneously in the past and outpatient exercise stress test and echocardiogram were normal 1 year ago. He was non-compliant with regular follow-up after the normal cardiac workup. His social history was significant for 30 packs year history of smoking and snorting two or three bags of crack cocaine on daily basis and occasional intravenous heroin for several years. He denied alcohol use. Vital signs were normal sinus rhythm of 80 beats per minute, blood pressure of 154/80 mm Hg, respiratory rate of 18 breaths per minutes and saturation at 98% on room air. Physical examinations were unremarkable on presentation.
All laboratory investigations including serial troponin and creatine kinase were normal. Urine drug screening was positive for cocaine. Serial ECGs showed new biphasic T wave in V2, V3 and V4 without Q wave, ST–T wave changes or left ventricular hypertrophy which was consistent with type A Wellens’ wave when compared with his normal baseline ECG (figure 1A–C). Chest X-ray was unremarkable. Management with oral Aspirin 325 mg and oral clopidogrel 300 mg was initiated promptly after sublingual nitroglycerin followed by intravenous unfractionated heparin infusion, intravenous morphine injection, oral amlodipine 10 mg daily, oral enalapril 20 mg daily and oral atorvastatin 40 mg daily.
Figure 1.
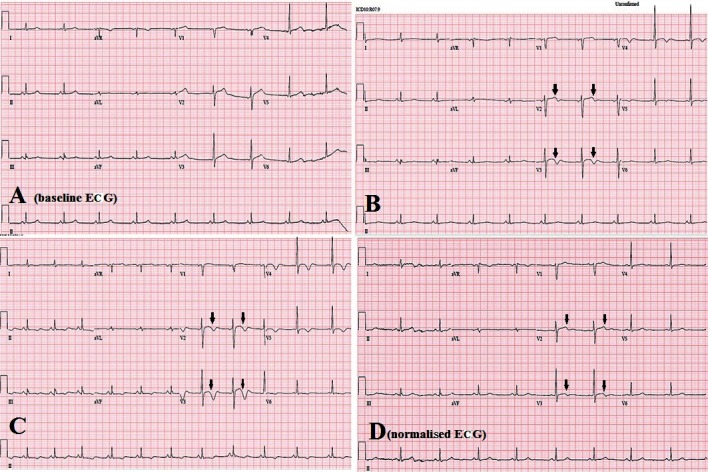
(A) Baseline ECG showing normal sinus rhythm. (B) ECG on presentation revealing biphasic T waves in V2–V4. (C) ECG demonstrating more prominent biphasic T waves in V2–V4. (D) Normalised ECG after resolution of chest pain.
Investigations
Bedside point-of-care echocardiogram showed normal left and right ventricular size and systolic function with left ventricular ejection fraction 60% without evidence of abnormal wall motion. ECG after relief of chest pain showed normal sinus rhythm with normalised T wave in V2 and V3 without ST segment changes (figure 1D). Given the recurrent episodic non-exertional chest pain relieved by nitroglycerin and Wellens’ wave on ECG, which was highly suspicious for proximal LAD occlusion, prompt decision was made to undergo cardiac catheterisation which revealed non-obstructive LAD (figure 2).
Figure 2.
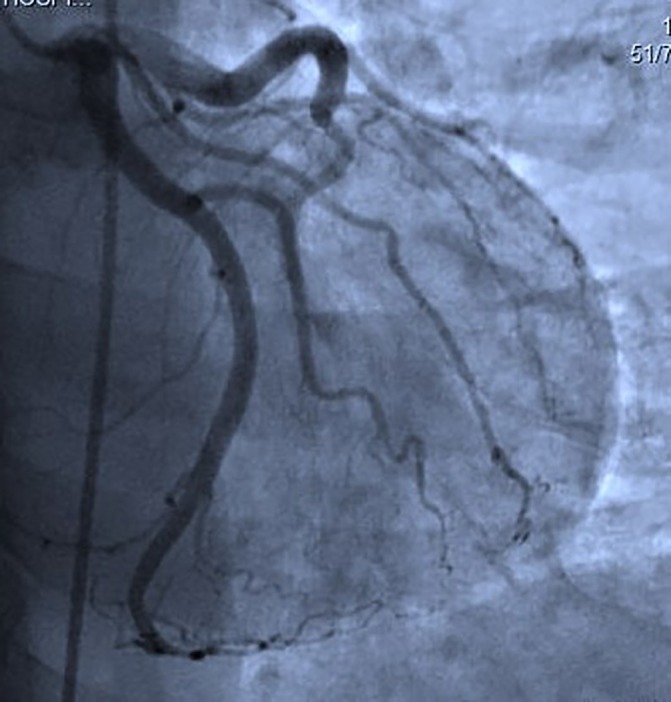
Coronary angiography depicting non-obstructive branches of left anterior descending coronary artery and left circumflex coronary artery.
Outcome and follow-up
Unstable angina with biphasic Wellenoid wave in V2–V3 resolved after the ACS treatment and non-obstructive coronaries confirmed the diagnosis of pseudo-Wellens’ syndrome due to cocaine-induced coronary vasospasm. He was asymptomatic during the hospitalisation and was discharged after 72 hours. Counselling for smoking cessation, cocaine detoxification and long-term drug rehabilitation were rendered but patient failed to follow-up after discharge.
Discussion
ECG changes reflecting stenosis of LAD coronary artery in correlation with exercise-induced inverted U wave was mentioned by Gerson et al in 1979.1 Wellens and colleagues were pioneers to link T wave changes in ECG with critical stenosis (>50%) of proximal LAD coronary artery.2 Criteria to diagnose Wellens’ syndrome are as follows:
history of recent chest pain
biphasic or symmetric deep inverted T wave in V2–V3 which may extend to V4–V6
ECG changes present in angina-free period
absence of Q waves in precordial leads
proper R wave progression in precordial leads
no or minimal ST elevation (<1 mm)
normal or slight cardiac enzymes elevation.
Wellens’ waves are subclassified into type A (biphasic T wave in leads V2 and V3, accountable for 24%) and type B (symmetric and deeply inverted T waves in leads V2 and V3, accountable for 76%).3 These signs are important to recognise as they reflect an underlying severe proximal LAD stenosis. However, Wellens' sign is not a telltale sign of acute proximal LAD occlusion because similar ECG patterns have been encountered in occlusions of branches of LAD. Moreover, myriads of other cardiac conditions, such as cardiac memory T wave, canyon T wave, Takotsubo syndrome and drug-induced coronary vasospasm, and non-cardiac conditions, such as cerebral T wave, global T wave inversion, juvenile T wave, pulmonary embolism and pheochromocytoma, may have Wellenoid electrocardiographic changes.4 5
Cocaine-induced coronary spasm in LAD, pseudo-Wellens’ syndrome, is considered as one of the possible differentials. Limited case reports of cocaine-induced pseudo-Wellens’ syndrome are found in the literature.6–9 Cocaine blocks presynaptic catecholamine reuptake and results in peripheral vasoconstriction, positive chronotropic and inotropic effects on myocardium. Cocaine metabolites also impose direct vasoconstriction on coronary arteries via alpha-adrenergic stimulation.10–12 Among the chest pain associated with cocaine use, 56%–86% of patients have abnormal ECG but myocardial infarction occurred in 0.7%–6%.9 However, only coronary angiography can differentiate pseudo-Wellens’ syndrome from Wellens’ syndrome. All patients with Wellenoid ECG findings need to be treated aggressively as ACS until proximal LAD occlusion is ruled out by coronary angiography.
Medical management of cocaine-induced pseudo-Wellens' syndrome is challenging and differs from the conventional ACS guideline. Intravenous benzodiazepine is the favoured initial medication to relieve chest pain and neuropsychiatric effect of cocaine. Nitroglycerin can also be safely use in cocaine-induced vasospasm. Calcium channel blocker (CCB) is selected over beta blockers which are contraindicated as unopposed alpha-adrenergic effect can portend to exacerbating of coronary vasospasm. Long-acting CCB is considered in cases unresponsive to benzodiazepine and nitroglycerin, although the role of CCB on cocaine-induced chest pain is not clear. CCB is thought to have antispasmodic effect on coronary arteries. Phentolamine, antiplatelets and anticoagulation are safe to use in cocaine-related chest pain.8–12
In our case, the patient complained of recurrent chest pain at rest which was typical of cardiac chest pain. Serial troponin I were also normal. Biphasic T waves in V2–V4 without pathological Q wave, no ST elevation and proper R wave progression met the ECG criteria for type A pattern Wellens’ wave. Symptomatic relief of chest pain and ECG normalisation were observed 4–6 hours after giving Aspirin, heparin infusion, nitroglycerin, CCB and ACEI. Non-obstructive coronaries on cardiac catheterisation supported the diagnosis of cocaine-induced pseudo-Wellens’ syndrome. The biphasic T waves in ECG were most likely caused by cocaine-induced selective coronary vasospasm in proximal LAD.
Clinical and ECG differentiation between cocaine-induced pseudo-Wellens’ syndrome and typical Wellens’ syndrome without coronary angiogram is extremely difficult. High index of suspicion and aggressive management are required for Wellenoid ECG changes and chest pain in cocaine user until critical LAD obstruction was excluded. Use of beta blockers can be disastrous and is contraindicated in cocaine-induced pseudo-Wellens’ syndrome and also cardiac stress test can be fatal in Wellens’ syndrome. It is important for the physician to be aware of cocaine-induced Wellens’ pattern ECG changes as a possible differential diagnosis and judicious use of beta-blocking agent as a part of ACS regimen.
Learning points.
Awareness of cocaine-induced pseudo-Wellens’ syndrome, selective proximal left anterior descending coronary vasospasm, as a possible differential diagnosis of Wellens’ syndrome.
To acknowledge the management of cocaine-induced chest pain with Wellens’ pattern ECG changes.
To acknowledge the side effects of beta-blocking agents in cocaine-induced coronary vasospasm.
Footnotes
Contributors: ANL: was involved in the conception of the idea, manuscript preparation, patient care and assay analysis. SL: was involved in the manuscript preparation, correlative assay and interpretation. RG: was involved in the patient care and manuscript preparation. DM: was involved in the conception of the idea, patient care and proof-reading. All the authors approved the submitted manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gerson MC, Phillips JF, Morris SN, et al. Exercise-induced U-wave inversion as a marker of stenosis of the left anterior descending coronary artery. Circulation 1979;60:1014–20. 10.1161/01.CIR.60.5.1014 [DOI] [PubMed] [Google Scholar]
- 2.de Zwaan C, Bär FW, Janssen JH, et al. Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. Am Heart J 1989;117:657–65. 10.1016/0002-8703(89)90742-4 [DOI] [PubMed] [Google Scholar]
- 3.Rhinehardt J, Brady WJ, Perron AD, et al. Electrocardiographic manifestations of Wellens’ syndrome. Am J Emerg Med 2002;20:638–43. 10.1053/ajem.2002.34800 [DOI] [PubMed] [Google Scholar]
- 4.Y-Hassan S. The pathogenesis of reversible T-wave inversions or large upright peaked T-waves: Sympathetic T-waves. Int J Cardiol 2015;191:237–43. 10.1016/j.ijcard.2015.04.233 [DOI] [PubMed] [Google Scholar]
- 5.Morris N, Howard L. BET 1: In patients with suspected acute coronary syndrome, does wellens’ sign on the electrocardiograph identify critical left anterior descending artery stenosis? Emer Med J 2017;34:264.2–6. 10.1136/emermed-2017-206665.1 [DOI] [PubMed] [Google Scholar]
- 6.Dhawan SS. Pseudo-Wellens’ syndrome after crack cocaine use. Can J Cardiol 2008;24:404 10.1016/S0828-282X(08)70608-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oksuz F, Sensoy B, Sen F, et al. ‘Action potential-like’ ST elevation following pseudo-Wellens’ electrocardiogram. Indian Heart J 2015;67:472–5. 10.1016/j.ihj.2015.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Langston W, Pollack M. Pseudo-Wellens syndrome in a cocaine user. Am J Emerg Med 2006;24:122–3. 10.1016/j.ajem.2005.07.017 [DOI] [PubMed] [Google Scholar]
- 9.Keller KB, Lemberg L. The cocaine-abused heart. Am J Crit Care 2003;12:262–6. [PubMed] [Google Scholar]
- 10.Lange RA, Cigarroa RG, Flores ED, et al. Potentiation of cocaine-induced coronary vasoconstriction by beta-adrenergic blockade. Ann Intern Med 1990;112:897–903. 10.7326/0003-4819-112-12-897 [DOI] [PubMed] [Google Scholar]
- 11.Benzaquen BS, Cohen V, Eisenberg MJ. Effects of cocaine on the coronary arteries. Am Heart J 2001;142:402–10. 10.1067/mhj.2001.117607 [DOI] [PubMed] [Google Scholar]
- 12.McCord J, Jneid H, Hollander JE, et al. Management of cocaine-associated chest pain and myocardial infarction. Circulation 2008;117:1897–907. [DOI] [PubMed] [Google Scholar]


