Abstract
Objective: To compare the availability, affordability and acceptability of two non-governmental organisation (NGO) led human immunodeficiency virus (HIV) testing service (HTS) modalities (mobile and stand-alone) with HTS at a public primary health care facility.
Methods: Adult participants who self-referred for HIV testing were enrolled as they exited the HTS modalities. Data collection using an electronic questionnaire took place between November 2014 and February 2015. Logistic regression analysis was used to assess differences in the participants' demographic characteristics and the availability, affordability and acceptability of HTS between modalities.
Results: There were 130 participants included in the study. Irrespective of modality, most participants walked to the service provider, had a travel time of <30 min and reported no costs. Participants were less likely to report waiting times of ⩾30 min compared to <15 min at the mobile modality compared to the public facility (aOR < 0.001, 95%CI < 0.001–0.03).
Conclusion: Irrespective of modality, HIV testing services were available and affordable in our study. Waiting times were significantly higher at the public facility compared to the NGO modalities. As South Africa moves toward achieving the first UNAIDS target, it is essential not only to make HTS available and affordable, but also to ensure that these services are acceptable, especially to those who have never been tested before.
Keywords: HIV testing services, availability, acceptability, affordability
Abstract
Objectif : Comparer la disponibilité, l'accessibilité et l'acceptabilité de deux modalités de services de test du virus de l'immunodéficience humaine (VIH) (HTS) : modalité mobile réalisée par des organisations non gouvernementales (ONG) et modalité autonome réalisée par une structure de soins de santé primaires.
Méthodes : Les participants adultes qui se sont présentés pour un test VIH ont été enrôlés lors de leur sortie des modalités de HTS. Le recueil de données, basé sur un questionnaire électronique, a eu lieu entre novembre 2014 et février 2015. Une analyse de régression logistique a été utilisée afin d'évaluer les différences des caractéristiques démographiques des participants et de la disponibilité, de l'accessibilité et de l'acceptabilité du HTS selon les modalités.
Résultats : Des 130 participants qui ont été inclus dans l'étude, quelle que soit la modalité, la majorité s'est rendue à pied chez le prestataire de soins, marchant pendant <30 min, et n'a subi aucun coût. Les participants des structures mobiles ont été moins susceptibles que ceux de la structure publique de rapporter un temps de trajet ⩾ 30 min comparés à <15 min (ORa < 0,001 ; IC95% < 0,001–0,03).
Conclusion : Les services de test VIH, quelle que soit la modalité, ont été disponibles et abordables dans notre étude. Les durées d'attente ont été significativement plus élevées dans la structure publique comparée aux modalités des ONG. Comme l'Afrique du Sud évolue vers l'atteinte de la première cible de l'ONUSIDA, il est essential non seulement de rendre le HST disponible et abordable, mais également de s'assurer que ces services sont acceptables, surtout à ceux qui n'ont jamais eu de test auparavant.
Abstract
Objetivo: Comparar la disponibilidad, la asequibilidad y la aceptabilidad de dos modalidades de servicios de pruebas diagnósticas del virus de inmunodeficiencia humana (VIH) (HTS móvil y fijo independiente) propuestas por organizaciones no gubernamentales (ONG) y los servicios diagnósticos propuestos en un establecimiento público de atención primaria de salud.
Métodos: Los adultos que acudían de manera espontánea en busca de pruebas diagnósticas se incluyeron en el estudio a la salida de los HTS. Se recogieron datos por conducto de un cuestionario electrónico de noviembre 2014 hasta febrero 2015. Mediante análisis de regresión logística se evaluaron las diferencias en las características demográficas de los participantes y la disponibilidad, la asequibilidad y la aceptabilidad de los HTS según las diferentes modalidades.
Resultados: Participaron en el estudio 130 personas. Con independencia de la modalidad, la mayoría de los participantes caminó hasta el punto de prestación de servicios, su tiempo de desplazamiento fue <30 min y refirió no haber incurrido en ningún gasto. Fue menos probable que los usuarios de los servicios móviles refiriesen un tiempo de espera ⩾ 30 min en lugar de <15 min, al compararlos con los usuarios del establecimiento público (P < 0,001; IC95% < 0,001–0,03).
Conclusión: El presente estudio reveló que los servicios de pruebas diagnósticas del VIH, sea cual fuere su modalidad, estaban disponibles y eran asequibles. Los tiempos de espera fueron significativamente más prolongados en el establecimiento público, en comparación con la espera en las modalidades de las ONG. A medida que Suráfrica progresa hacia el cumplimiento de la primera meta del Programa Conjunto de las Naciones Unidas sobre el VIH/SIDA, es primordial, no solo que los HTS estén disponibles y sean asequibles, sino que se garantice su aceptabilidad, sobre todo por parte las personas que nunca han recibido la prueba.
South Africa is progressing toward the first Joint United Nations Programme on HIV and AIDS (UNAIDS) target of having 90% of people living with the human immunodeficiency virus (HIV) know their status by the year 2020.1 In 2012, an estimated 65% of the South African population had ever tested for HIV.2 An estimated 23% of HIV-positive adults remain undiagnosed,3 with a higher estimated proportion among men (31.9%) than women (19%).3 The challenge is to reach those who do not access HIV testing services (HTS) and remain unaware of their HIV-positive status.
In South Africa, the majority of people who tested for HIV in 2012 (70%) utilised public health facilities, with the remaining 30% utilising private facilities, including those managed by non-governmental organisations (NGOs), and alternative testing modalities (e.g., mobile services).2
Published South African studies predominantly describe the demographics of people who utilise different HIV testing modalities, the proportions who were first-time testers and those who tested HIV-positive.4–7 There is limited literature on access to HIV testing services (HTS).
‘Access’ is a complex, multidimensional concept.8 Access to HTS is broader than mere utilisation of the service;9 it is dependent on three conceptually different dimensions:10 availability (the extent to which HTS are geographically accessible), affordability (the cost of the HTS in relation to the user's ability to pay) and acceptability (self-perceived quality of the HTS).11
Some studies have linked utilisation to the availability of services12 and determined the availability and acceptability of HTS at public health care facilities13 and mobile services.14,15 An improved understanding of access, including availability, affordability and acceptability, to public and private (NGO) HTS modalities from the user's perspective can inform policy and potentially lead to increased numbers of people becoming aware of their HIV-positive status.
The aim of this study was to investigate the availability, affordability and acceptability of two NGO-led HTS modalities (mobile and stand-alone) compared to HTS at a public primary health care (PHC) facility.
METHODS
Setting
The present study was conducted in a community in the Cape Metro district, Western Cape Province, South Africa. This purposively selected community, characterised by high unemployment rates, a mixture of formal and informal housing and a high disease burden,16 had a public PHC facility and an NGO, both providing HTS. The public PHC facility provided a range of services, including HTS and treatment services. HTS was offered as part of clinical care, but individuals could also self-refer for an HIV test, i.e., voluntarily decide to learn their HIV status and actively seek out HTS.17 The NGO offered HTS from two HTS modalities in the same community. A stand-alone centre (fixed site) offered HTS from a rented space in a local shopping centre, while mobile HTS was provided from pop-up tents and a caravan (mobile van) set up in appropriate open spaces in the community. Spaces were selected on an ad hoc basis and changed regularly. The NGO modalities only offered HTS.
All three modalities followed the same HIV testing algorithm, guidelines and rapid HIV testing kits, utilised trained HIV lay counsellors to provide HTS free of charge and operated during standard business hours.
Design
A cross-sectional survey compared the availability, affordability and acceptability of HTS at three HTS modalities: an NGO-led mobile service, an NGO-led stand-alone centre and a public PHC facility. As these modalities were all within 2 km of one another, it is plausible to assume that individuals needing HTS could self-refer to any of the three modalities.
Study population
Participants were eligible for study inclusion if they had self-referred for HTS at one of the modalities within the study area, were aged ⩾18 years, and consented to participate in the study. Participants were excluded if they were aged <18 years, had not self-referred for HTS, they had visited the HTS modality but no HIV test was performed or they did not provide written informed consent. A trained research assistant approached eligible participants when they exited the HTS modality. Enrolment was sequential until 50 clients from each modality were enrolled.
Data collection
Data collection took place over 2 months (November and December 2014) at the mobile and stand-alone modalities, and over 1 month (February 2015) at the public facility. The research assistant administered an electronic questionnaire using a hand-held digital device that automatically generated a unique study number for each participant (participant names were not collected). No information was collected that could link the participant to their HIV test result.
The electronic questionnaire collected demographic data (sex and age), and closed-ended questions that addressed the participant's perspective of the availability, affordability and acceptability of the HTS on that day. Although the questionnaire was in English, the research assistants spoke fluent English and isiXhosa (the local language in the study area), and were able to explain the meaning of the questions and the choice of answers to the clients, if required.
Availability
To determine the geographic accessibility of HTS for the users, questions pertained to mode of transport and time travelled (Table 1).
TABLE 1.
Questions asked concerning each dimension of ‘access’
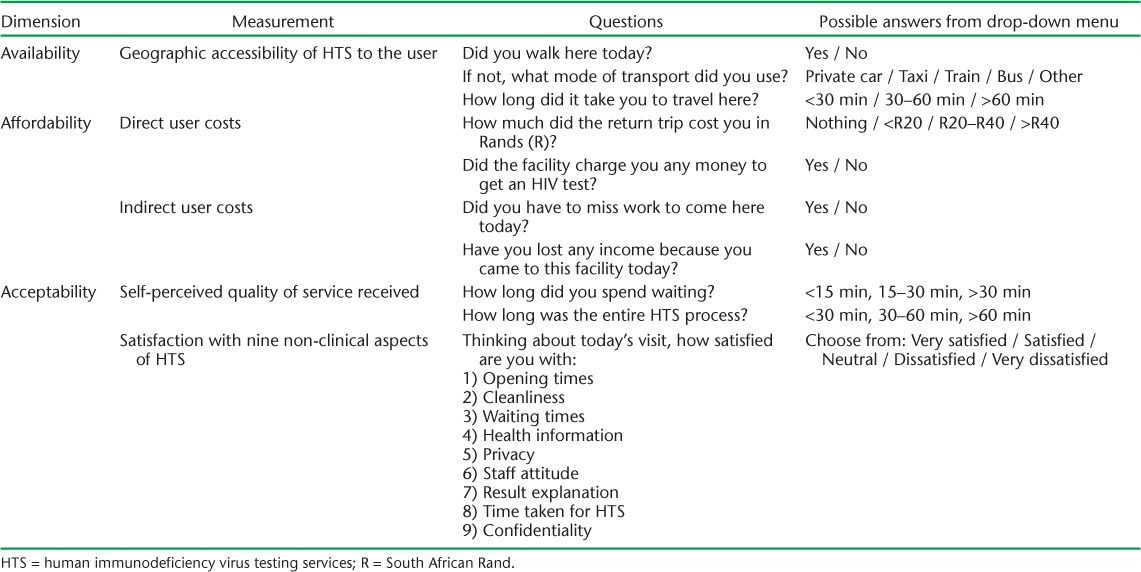
Affordability
To determine user costs, we asked questions about direct and indirect user costs (Table 1). An ‘affordability score’ was obtained for each participant and was calculated as follows: 0 = answered ‘no/nothing’ to all four questions; 1 = answered ‘yes’ to one of the questions; 2 = answered ‘yes’ to two of the questions. No participants answered ‘yes’ to more than two of the four questions. This resulted in a possible ‘affordability score’ of 0, 1 or 2.
Acceptability
Acceptability included the participants' perception of the quality of the service received and their satisfaction with nine non-clinical aspects of HTS (Table 1). A non-clinical satisfaction score was calculated for each participant using the nine Likert scale items ranging from 1 (very satisfied) to 5 (very dissatisfied). The minimum and maximum scores a participant could have were therefore 9 and 45, respectively.
Analysis
Data from the electronic questionnaire were downloaded into a Microsoft Access database (Microsoft Corp, Redmond, WA, USA). Logistic regression analysis was used to assess the differences in demographic characteristics and in the availability, affordability and acceptability of HTS for participants at: 1) NGO mobile vs. public facility, 2) NGO stand-alone vs. public facility, and 3) NGO stand-alone vs. NGO mobile. All variables were included in the multivariate analysis, irrespective of their association with the outcome in the uni-variate analysis. The level of significance in all analyses was P < 0.05. The analysis was completed in Stata v. 14 (StataCorp, College Station, TX, USA).
Ethics approval
The Health Research Ethics Committee of Stellenbosch University (S12/02/059) approved the study. The City of Cape Town Health Department granted permission (ID 10463) to enrol participants at the public facility. There were no incentives for testing or for participation in the study. All participants provided written informed consent, could discontinue the questionnaire at any time or decline to answer any questions without any negative consequences.
RESULTS
Of 151 participants initially enrolled in the study, 21 (14%) were excluded from the analysis for the following reasons: did not self-refer for HTS (17 at the public facility and 1 at the mobile facility), age < 18 years (2 at the stand-alone centre), did not have an HIV test (1 at the stand-alone centre). A total of 130 participants were eligible for analysis: 50 from the mobile facility, 49 from the stand-alone centre and 31 from the public facility.
Sex and age
Forty per cent of the participants at the mobile modality, 25% at the stand-alone modality and 26% at the public facility were male (Table 2). There was no significant difference in the proportion of males between modalities.
TABLE 2.
Participant demographics and availability, affordability and acceptability of HTS by modality, Cape Town, South Africa
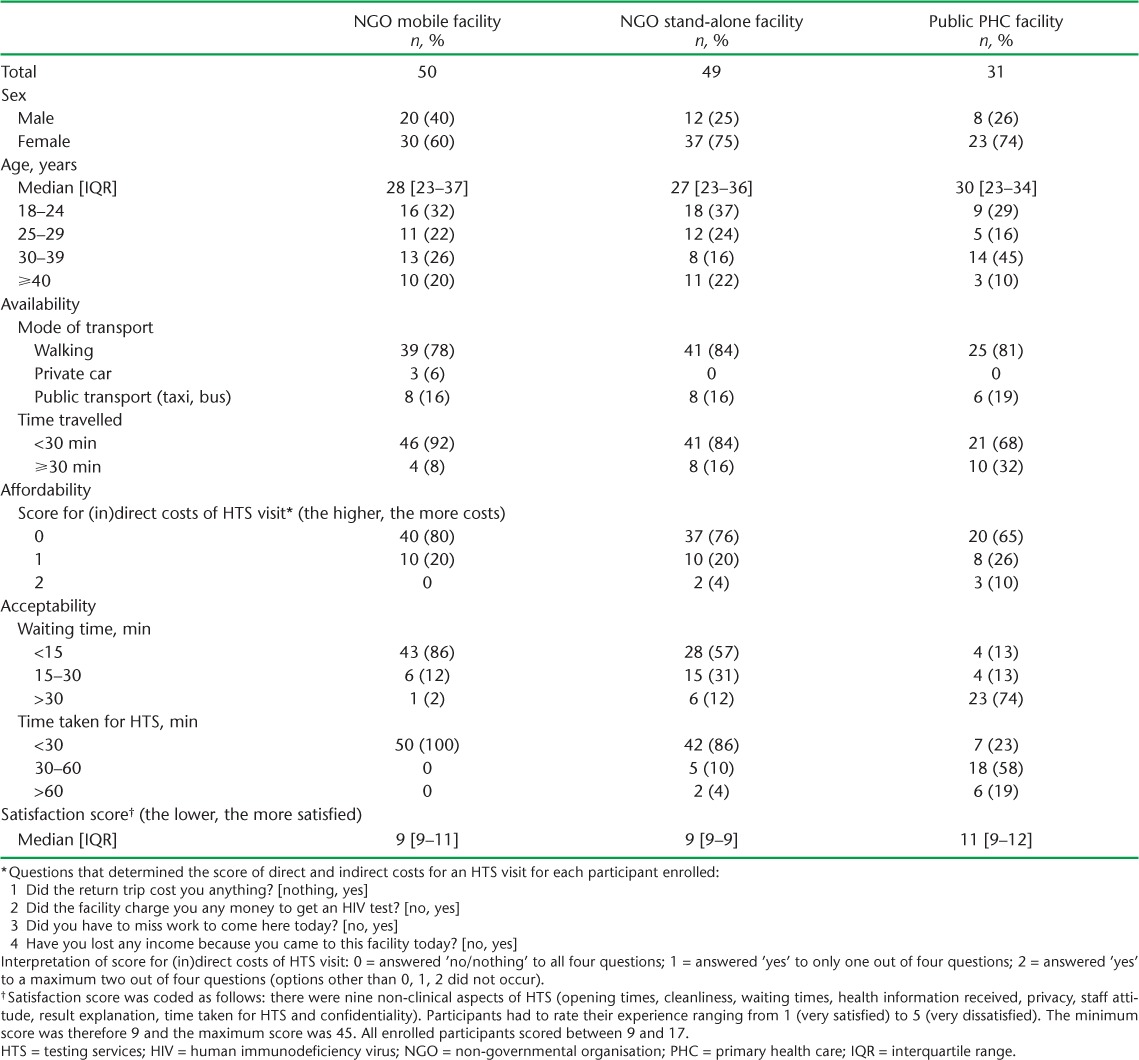
The median age of the participants at the mobile and stand-alone modalities was 28 years (confidence interval [CI] 95%CI 23–37) and 27 years (95%CI 23–36), respectively. At the public facility, the median age was 30 years (95%CI 23–34). More than a third of the participants at the mobile and stand-alone modalities were in the age group 18–24 years, while almost half of the participants at the public facility were in the age group 30–39 years.
Availability
Irrespective of modality, the majority of the participants walked to the HTS and reported a travel time of <30 min (Table 2). There was no significant difference in mode of transport or travel time between the modalities.
Affordability
Irrespective of modality, the majority of the participants had an affordability score of 0, i.e., they reported no costs incurred to access the HTS (Table 2). There was no significant difference in affordability between modalities.
Acceptability
There were significant differences in the reported waiting times between the modalities. The proportion of participants reporting the shortest waiting time (<15 min) was highest for those who utilised the mobile HTS (86%) compared to the stand-alone (57%) and public facility HTS (13%) (Table 2).
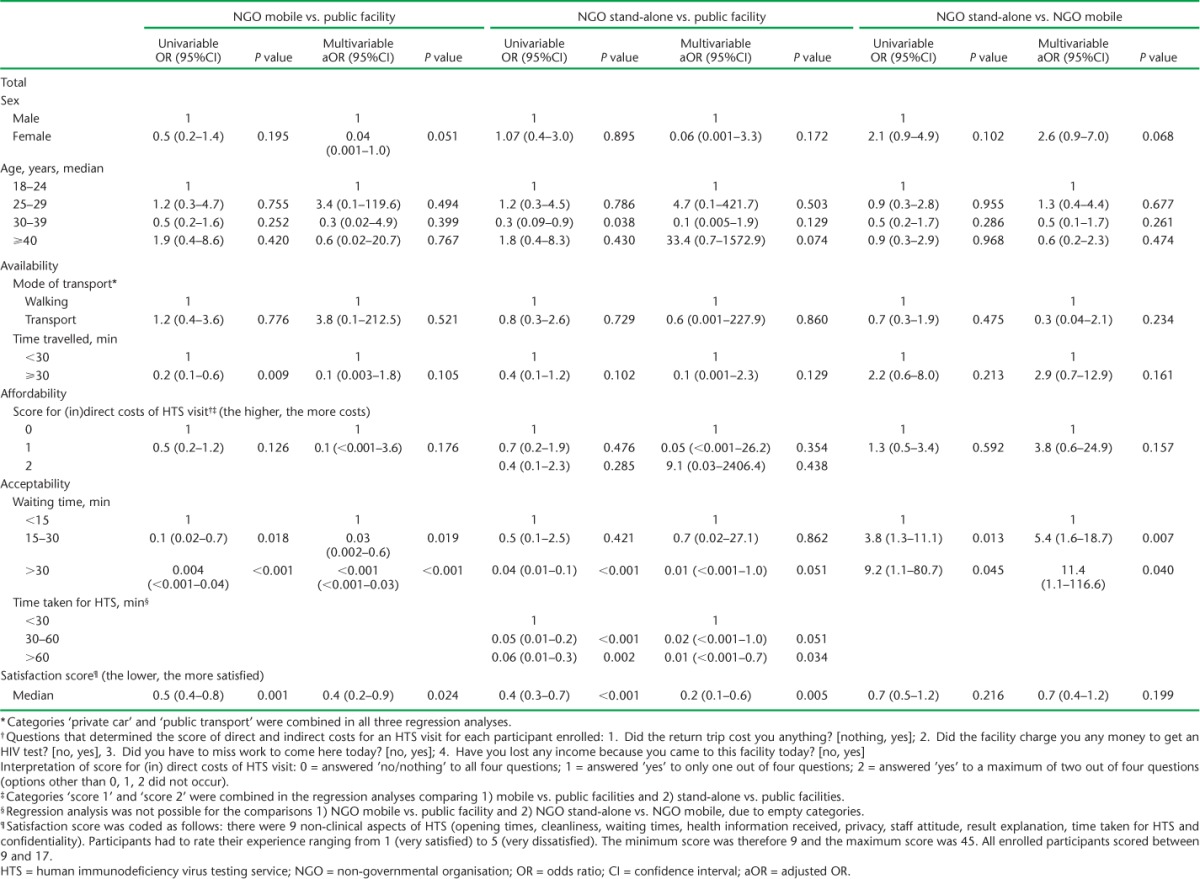
Participants at the mobile HTS were less likely to report waiting times of ⩾ 30 min compared to <15 min than those at the public facility (adjusted odds ratio [aOR] < 0.001, 95%CI 0.001–0.03). Participants at the stand-alone HTS were more likely than those at the mobile HTS to report waiting times of 15–30 min compared to <15 min (aOR 5.4, 95%CI 1.6–18.7) (Table 3).
TABLE 3.
Univariable and multivariable associations between participants' demographic characteristics and availability, affordability and acceptability of HTS at three modalities in Cape Town, South Africa
The majority of the participants at the mobile and stand-alone services reported a duration of <30 min for the entire HTS process (respectively 100% and 86%), compared to only 23% of participants at the public facility (Table 2).
Irrespective of which HTS modality they utilised, the majority of the participants reported being very satisfied with their HTS experience. All of the participants had a satisfaction score of between 9 and 17 (of a possible range of 9–45; the lower the score, the greater the level of satisfaction). Participants utilising the mobile and stand-alone modalities were significantly more satisfied than those utilising the PHC facility (respectively P = 0.024 and P = 0.005). There was no significant difference in satisfaction scores for participants at the mobile compared to the stand-alone services (Table 3).
The highest possible satisfaction score (9, meaning ‘very satisfied’ on all nine non-clinical aspects of HTS) was reported by the majority of the participants who utilised the mobile and stand-alone services (respectively 68% and 76%) (Figure). Lower levels of satisfaction (range 13–17) were reported by participants who utilised the public facility.
FIGURE.
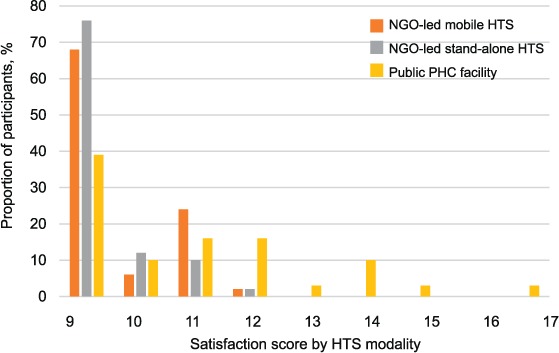
Distribution of satisfaction scores across HTS modality in Cape Town, South Africa. NGO = non-governmental organisation; HTS = human immunodeficiency virus testing services; PHC = primary health care.
DISCUSSION
Improving access to HTS is vital to increase the number of people who undergo testing to be aware of their HIV-positive status. This study analysed access to HTS for those who self-referred for an HIV test at NGO-managed mobile and stand-alone modalities compared to a public facility. Of those included in the study, there was a larger proportion of men at the mobile modality compared to the public facility and the stand-alone centre, although these differences were not significant. Previous studies have shown that mobile HTS is utilised by a higher proportion of men compared to other HTS modalities,4,14,15 while women tend to access public facilities.18
Irrespective of modality, the majority of the participants walked to the HTS and reported a travel time of <30 min. This highlights the close proximity of the HTS to the user. This finding is in agreement with previous studies showing that mobile services are conveniently situated in communities,14 providing users with the immediate opportunity to test,13 and that physical proximity of health care is no longer a problem for reaching public facilities.19 Findings may be different in rural settings, where the service may be further from the user.
The majority of the participants reported no costs related to utilising the HTS, making HIV testing affordable to the users in our setting. This finding differs from previous studies that found the costs involved in obtaining health services challenging.20–22 In areas outside our setting, where there may be longer distances between public facilities and users, reducing the distance between testing services and their users is one way of reducing transport costs, making mobile HTS a viable consideration.
Participants at the public facility reported longer waiting times than those at the mobile and stand-alone modalities. Levels of dissatisfaction with waiting times at public health care facilities in South Africa have been widely reported.18,19,23,24 Longer waiting times are expected at public facilities due to high patient loads and because of the number of services offered (i.e., not only HTS), but they may be a barrier to service uptake. Addressing staff shortages and improving patient flow25 may reduce waiting times. Operational research is required to identify what interventions would be most effective in reducing waiting times in different contexts.
While the majority of the participants reported that they were very satisfied with their HTS experience, those who utilised mobile and stand-alone modalities reported greater levels of satisfaction than those utilising the public facility. Satisfaction is a subjective concept, and self-reported perceptions are often driven by previous experiences.11 Furthermore, the small sample size limits generalisability. Our findings nevertheless replicate findings in previous studies: high levels of patient acceptability were reported for mobile HTS,14 and mobile HTS were found more acceptable than HTS at public facilities in terms of waiting times, cleanliness and perceived friendliness of staff.13 Our study showed that although user satisfaction at the public facility was high, satisfaction levels were more widely distributed than at mobile and stand-alone modalities.
A major strength of this study is that it was able to compare three dimensions of access—availability, affordability and acceptability—across three different HTS modalities: two NGO-led modalities and a public PHC facility. While many studies differentiate between NGO-led and public HTS in terms of the different populations they reach and clinical outcomes, literature comparing the availability, affordability and acceptability of these different HIV testing modalities from a user's perspective are limited. When formulating policy aimed at increasing access to HTS, it is essential to understand the user's perspective.26 To make conclusive statements that can inform policy aimed at increasing access to HTS, the study needs to be repeated in a larger population sample.
In this study, we did not record people who had self-referred for an HIV test but who did not wish to participate in the study, potentially introducing selection bias. The data were self-reported, which may have biased the results. The main findings nevertheless concur with similar studies in South Africa. The study required users to report their experience of the HTS modality they had just utilised. Many individuals have been tested for HIV multiple times, and future studies should consider the perspective of users who have utilised two or more different HTS modalities to provide rich comparative data. Like most other studies, this study included only people who had actually tested for HIV. Those who may have left the service before being tested for HIV and those who had never been tested for HIV were not included, and their perspectives are therefore not documented.
CONCLUSION
Irrespective of modality, HIV testing services were available and affordable in our study, with no difference between NGO mobile and stand-alone modalities and the public facility. In terms of the acceptability of services from a user's perspective, however, the waiting times were significantly higher and the satisfaction scores lower at the public facility compared to the mobile and stand-alone modalities. As South Africa moves toward achieving the first UNAIDS target, it is essential to make HTS not only available and affordable, but also acceptable to clients, especially those who have never before been tested. Future studies should include participants who have never been tested for HIV, to gain a further perspective on access to HTS.
Acknowledgments
The stand-alone centres and mobiles services described in this publication were supported by Cooperative Agreement Number U2GGH000320, funded by the Centers for Disease Control and Prevention (CDC, Atlanta, GA, USA). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the CDC or the Department of Health and Human Sciences (Washington, DC, USA).
The authors would like to thank research assistants M Moletseli and T Wonxie for collecting the data, the Cape Town City Health Directorate for providing approval and support for this study to be conducted within one of their primary health care facilities. K Jennings and P Nkuruziza also provided input to the manuscript.
Footnotes
Conflicts of interest: none declared.
References
- 1. Joint United Nations Programme on HIV/AIDS (UNAIDS). . 90–90–90: an ambitious treatment target to help end the AIDS epidemic. Geneva, Switzerland: UNAIDS, 2014. http://www.unaids.org/en/resources/documents/2014/90-90-90 Accessed October 2017. [Google Scholar]
- 2. Shisana O, Rehle T T, Simbayi L C, . et al. South African national HIV prevalence, incidence and behaviour survey. Pretoria, South Africa: HSRC, 2012. http://www.hsrc.ac.za/en/research-data/view/6871 Accessed October 2017. [Google Scholar]
- 3. Johnson L F, Rehle T M, Jooste S, Bekker L-G.. Rates of HIV testing and diagnosis in South Africa: successes and challenges. AIDS 2015; 29: 1401– 1409. [DOI] [PubMed] [Google Scholar]
- 4. Mabuto T, Latka M H, Kuwane B, Churchyard G J, Charalambous S, Hoffmann C J.. Four models of HIV counseling and testing: utilization and test results in South Africa. PLOS ONE 2014; 9: e102267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Suthar A B, Ford N, Bachanas P J, . et al. Towards universal voluntary HIV testing and counselling: a systematic review and meta-analysis of community-based approaches. PLOS Med 2013; 10: e1001496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Van Rooyen H, Barnabas R, Baeten J, . et al. High HIV testing uptake and linkage to care in a novel program of home-based HIV counseling and tetsing with a facilitated referral in KwaZulu-Natal, South Africa. J Acquir Immune Defic Syndr 2013; 64: 27– 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maheswaran H, Thulare H, Stanistreet D, Hons B A, Tanser F.. Starting a home and mobile HIV testing service in a rural area of South Africa. J Acquir Immune Defic Syndr 2012; 59: 43– 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gulliford M, Figueroa-Munoz J, Morgan M, . et al. What does ‘access to health care’ mean? J Health Serv Res Policy 2002; 7: 186– 188. [DOI] [PubMed] [Google Scholar]
- 9. Levesque J-F, Harris M F, Russell G.. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health 2013; 12: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thiede M, Akweongo P, McIntyre D.. Exploring the dimensions of access. : Mooney G, McIntyre D, . The Economics of Health Equity. Cambridge, UK: Cambridge University Press, 2007: 103– 123. [Google Scholar]
- 11. McIntyre D, Thiede M, Birch S.. Access as a policy-relevant concept in low- and middle-income countries. Health Econ Policy Law 2009; 4: 179– 193. [DOI] [PubMed] [Google Scholar]
- 12. Hutchinson P L, Mahlalela X.. Utilization of voluntary counseling and testing services in the Eastern Cape, South Africa. AIDS Care 2006; 18: 446– 455. [DOI] [PubMed] [Google Scholar]
- 13. Meehan S-A, Leon N, Naidoo P, Jennings K, Burger R, Beyers N.. Availability and acceptability of HIV counselling and testing services. A qualitative study comparing clients' experiences of accessing HIV testing at public sector primary health care facilities or non-governmental mobile services in Cape Town, South Africa. BMC Public Health 2015; 15: 845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Van Rooyen H, McGrath N, Chirowodza A, . et al. Mobile VCT: reaching men and young people in urban and rural South African pilot studies (NIMH Project Accept, HPTN 043). AIDS Behav 2012; 17: 2946– 2953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Meehan S-A, Naidoo P, Claassens M M, Lombard C, Beyers N.. Characteristics of clients who access mobile compared to clinic HIV counselling and testing services: a matched study from Cape Town, South Africa. BMC Health Serv Res 2014; 14: 1– 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Statistics South Africa. . Census 2011: interactive data in SuperCROSS. Pretoria, South Africa: SSA, 2011. http://www.statssa.gov.za/?page_id=1417 Accessed October 2017. [Google Scholar]
- 17. South Africa Department of Health. . National HIV Testing Services Policy 2016. Pretoria, South Africa: DoH, 2016. http://www.hst.org.za/publications/national-hiv-testing-services-policy Accessed October 2017. [Google Scholar]
- 18. Chimbindi N, Bärnighausen T, Newell M-L.. Patient satisfaction with HIV and TB treatment in a public programme in rural KwaZulu-Natal: evidence from patient-exit interviews. BMC Health Serv Res 2014; 14: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Burger R, Bredenkamp C, Grobler C.. Have public health spending and access in South Africa become more equitable since the end of apartheid ? Dev South Afr 2012; 29: 681– 703. [Google Scholar]
- 20. Western Cape Government Health. . Annual Report 2014/5. Cape Town, South Africa: West Cape Government Health, 2015. https://www.westerncape.gov.za/assets/departments/health/wcghannual_report2014_2015.pdf Accessed October 2017. [Google Scholar]
- 21. Sam-Agudu N A, Folayan M O, Ezeanolue E.. Seeking wider access to HIV testing for adolescents in sub-Saharan Africa. Pediatr Res 2016; 79: 838– 845. [DOI] [PubMed] [Google Scholar]
- 22. Mubyazi G M, Bloch P, Magnussen P, . et al. Women's experiences and views about costs of seeking malaria chemoprevention and other antenatal services: a qualitative study from two districts in rural Tanzania. Malar J 2010; 9: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Burger R, Van der Berg S.. How well is the South African public health care system serving its people? : Hofmeyr Jan, . Risk and opportunity. Cape Town, South Africa: Institute for Justice and Reconciliation, 2008. [Google Scholar]
- 24. Harris B, Goudge J, Ataguba J E, . et al. Inequities in access to health care in South Africa. J Public Health Policy 2011; 32 Suppl 1: S102– S123. [DOI] [PubMed] [Google Scholar]
- 25. World Health Organization. . Global health sector response to HIV, 2000–2015. Focus on innovations in Africa. Geneva, Switzerland: WHO, 2015. http://apps.who.int/iris/bitstream/10665/198065/1/9789241509824_eng.pdf?ua=1 Accessed October 2017. [Google Scholar]
- 26. Peltzer K. Patient experiences and health system responsiveness in South Africa. BMC Health Serv Res 2009; 9: 117. [DOI] [PMC free article] [PubMed] [Google Scholar]


