Abstract
Evidence suggests that long-term stress facilitates visceral pain through sensitization of pain pathways and promotes chronic visceral pain disorders such as the irritable bowel syndrome (IBS). This review will describe the importance of stress in exacerbating IBS-induced abdominal pain. Additionally, we will briefly review our understanding of the activation of the hypothalamic-pituitary-adrenal axis by both chronic adult stress and following early life stress in the pathogenesis of IBS. The review will focus on the glucocorticoid receptor and corticotropin-releasing hormone-mediated mechanisms in the amygdala involved in stress-induced visceral hypersensitivity. One potential mechanism underlying persistent effects of stress on visceral sensitivity could be epigenetic modulation of gene expression. While there are relatively few studies examining epigenetically mediated mechanisms involved in stress-induced visceral nociception, alterations in DNA methylation and histone acetylation patterns within the brain, have been linked to alterations in nociceptive signaling via increased expression of pro-nociceptive neurotransmitters. This review will discuss the latest studies investigating the long-term effects of stress on visceral sensitivity. Additionally, we will critically review the importance of experimental models of adult stress and early life stress in enhancing our understanding of the basic molecular mechanisms of nociceptive processing.
Keywords: Amygdala, Early life adversity, Irritable bowel syndrome, Models, animal, Visceral pain
Introduction
Irritable bowel syndrome (IBS) is a complicated condition with an unknown etiology. The IBS patient population is heterogeneous with subpopulations of IBS with diarrhea, IBS with constipation and a mixed population with episodes of diarrhea and constipation with symptoms differing from one patient to the next and with severity of symptoms ranging from debilitating to mild to moderate.1–6 Risk factors for IBS include being female and exposure to chronic stress.7–11 A common feature of IBS is that for many patients, their symptoms are worsened by stress and overlap with other stress disorders, including anxiety, depression, and post-traumatic stress disorder.12–15 In support of IBS being a stress-sensitive disorder, there is experimental evidence showing abnormal hypothalamic-pituitary-adrenal (HPA) axis reactivity in IBS patients as shown by a heightened HPA response to a corticotropin-releasing hormone (CRH) challenge, and an overall increase in hourly cortisol secretion in IBS compared to controls.16–18 Another interesting observation is that some patients with IBS, especially female IBS patients, can recall repetitive exposure to adversity in their childhood.19,20 In this review we will discuss the hypothesis that visceral pain disorders result from abnormalities of the brain-gut axis due to “multiple hits” which include external risk factors such as abuse history and chronic psychological stress in adulthood which together are capable of sensitizing the stress response system to cause alterations in nociceptive processing and the development of IBS pathophysiology. Taken together, the complex clinical phenotype makes recapitulating IBS in rodent models extremely challenging. However, an aim of this review will be to describe how the use of rodent models of adult stress, early life stress (ELS), and a dysregulated HPA axis has improved our understanding of stress in the pathophysiology of IBS.
Pathophysiology of Irritable Bowel Syndrome: Activation of the Brain-Gut Axis
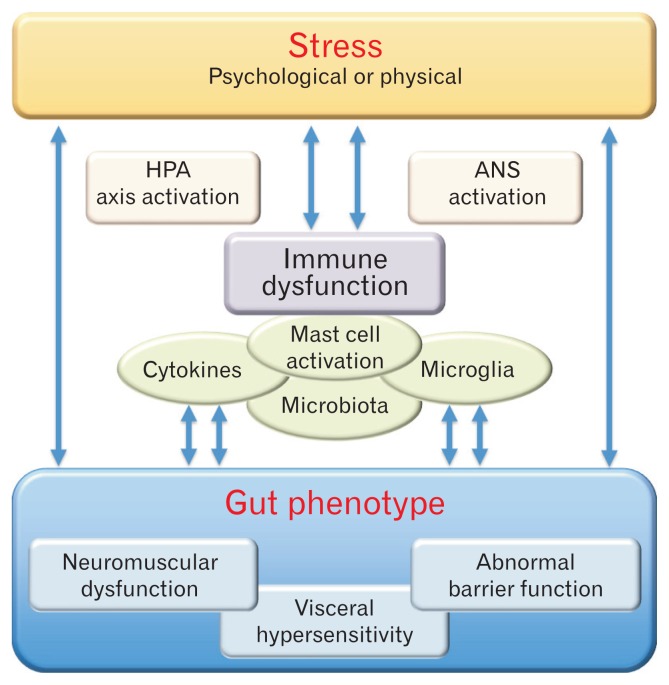
Evidence from clinical and basic research points to dysregulation of the bidirectional communication between the brain-gut axis in IBS.21 The brain-gut axis represents a dynamic interplay between central circuits and peripheral mechanisms. The messengers of this complex circuit include neural, endocrine, metabolic, and immune mediators that are activated by central factors such as stress (Fig. 1). Although IBS is not an inflammatory disorder, the immune system plays a role in the pathogenesis of IBS in at least a subset of patients and likely contributes to the etiology of IBS symptoms.22,23 A subset of IBS patients display a low grade chronic inflammation, and there is also evidence that following an enteric infection and combined with stressful life events, there is an increased risk of developed post-infectious IBS.24–27 Clearly, the immune system and inflammatory processes are modulated by the HPA and autonomic nervous systems. In support, IBS patients also show increased number and reactivity of mast cells.28,29 Data from peripheral blood mononuclear cells, as well as in mucosal biopsies, from IBS patients show that cytokines levels including TNF-α, IL-1β and IL-6 are increased in IBS.30–33 It is well recognized that proinflammatory cytokines can alter neurotransmitter release within the enteric nervous system to alter motility, secretion, and epithelial permeability via tight junction dysregulation to alter visceral sensitivity.34 There is also evidence for alterations in microbiota balance in IBS and alterations in the bidirectional communication between the gut microbiota, the CNS, and the enteric nervous system.35,36
Figure 1.
Pathophysiology of irritable bowel syndrome (IBS): activation of the brain-gut axis. Working model of stress-induced brain-gut dysfunction in IBS. Physical or psychological threats (actual or perceived) are stressors that activate both the hypothalamic-pituitary-adrenal (HPA) axis and the autonomic nervous system (ANS) to allow the individual to respond to the threat and to restore homeostasis. Prolong activation of the body’s stress response can lead to immune system dysfunction including activation of mast cells in the periphery and microglia in the spinal cord and the brain, release of proinflam-matory cytokines, and changes in host microbiota. Taken together, chronic stress and immune dysfunction provides an underlying mechanism for alterations in gut phenotypes including neuromuscular dysfunction, abnormal barrier function, and visceral hypersensitivity. Once established, these abnormal gut phenotypes facilitate further activation of the stress systems and immune dysfunction that maintains IBS symptoms.
Visceral Hypersensitivity in Irritable Bowel Syndrome
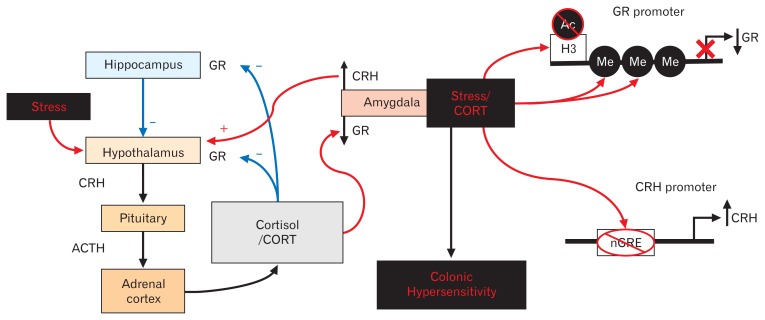
An important aspect to enhancing our understanding of IBS pathophysiology is the knowledge that IBS patients exhibit visceral hypersensitivity characterized by hyperalgesia and allodynia in a subset of IBS patients ranging from 33–90% of patients with IBS depending on the study.37–42 Although the cause of visceral hypersensitivity is unknown, clinical studies have shown that chronic stress worsens IBS symptomatology and ELS serves as a risk factor for IBS.43–46 The sympatho-medullary and the HPA axes are activated by exposure to stress; the sympatho-medullary axis releases epinephrine from the adrenal medulla, to allow the organism to “fight” or “flee” from a threat, whilst activation of the HPA axis releases cortisol (or corticosterone [CORT] in rodents) from the adrenal cortex to mobilize reserves of glucose with the goal of replenishing the expended sympatho-medullary system. Activation of the HPA axis by stress releases CRH from the paraventricular nucleus of the hypothalamus into the hypophyseal portal circulation. CRH then binds to a CRH type-1 receptor in the anterior pituitary stimulating the production and the release of adrenocorticotropic hormone (ACTH) from the pituitary gland into the systemic circulation. The circulating ACTH binds to receptors in the adrenal cortex to stimulate production of CORT, which binds to a cortisol binding globulin, prior to being released at target organs throughout the body. A pivotal role for CORT release from the HPA axis in response to stress is the initiation of feedback-inhibition through binding to the mineralocorticoid receptor (MR) and the GR47,48 at multiple nuclei, such as the hippocampus, the paraventricular nucleus of the hypothalamus, and anterior pituitary.49 In contrast to the feedback-inhibition, when CORT binds at the amygdala there is an increase in CRH release and the subsequent facilitation of the stress axis50,51 (Fig. 2).
Figure 2.
Amygdala-mediated mechanisms for stress-induced colonic hypersensitivity. The body’s neuroendocrine stress response (hypothalamic-pituitary-adrenal [HPA] axis) is initiated at the hypothalamus and causes the synthesis and release of corticotropin-releasing hormone (CRH) onto the anterior pituitary. Upon binding of CRH to its type 1 receptor, the pituitary gland secretes adrenocorticotropic hormone (ACTH) into the peripheral blood circulation leading to production of cortisol in humans or corticosterone (CORT) in rodents. Following release into the circulation, CORT binds to the glucocorticoid receptor (GR) to initiate negative feedback of the HPA axis at the level of the hypothalamus and the hippocampus. In contrast, CORT binding to GR at the amygdala leads to facilitation of HPA axis, thus promoting persistent stress activation.50,52–55 In this review, we discuss our recent data showing that stress activation or implantation of a CORT micropellet at the amygdala produces persistent colonic hypersensitivity to balloon distension along with decreased GR expression and increased CRH expression.56–60 Our findings have also revealed that a decrease in GR expression could be due to increased methylation (Me) of the GR promoter along with decreased acetylation (Ac) of histone 3 (H3) at the GR promoter.61,62 The persistent decrease in GR expression decreases the binding of GR to a negative GR response (nGRE) element in the CRH promoter, thus removing GR-induced repression of CRH expression. The loss of the repression of the CRH promoter induced a persistent increase in CRH expression, and inhibiting the increase in CRH expression reversed the stress-induced colonic hypersensitivity.62
Amygdala Facilitation of the Hypothalamic-Pituitary-Adrenal Axis
Neuroimaging studies in IBS patients have shown that there is altered brain activation in response to a nociceptive stimulus suggesting central sensitization.63–66 In particular, the amygdala has been found to consistently demonstrate altered activation to visceral stimulation in IBS patients.67 The amygdala is a brain nucleus that is important for the integration of the body’s neurophysiologic responses to stress, as well as modulating the perception of anxiety, which is increased in IBS.68 The amygdala, and more specifically the central nucleus of the amygdala (CeA), is a key brain nucleus involved in the facilitation of the stress response.50,69 Specifically, CORT acting via GR and MR mediated mechanisms in the CeA drives the HPA and autonomic components of the stress axis.50,70 Since stress worsens visceral pain in IBS patients, an overarching goal of our laboratory has been to investigate the mechanisms within the CeA that are involved in stress-induced nociception. To address this goal we have employed a series of rodent models. In one model, micropellets of CORT are implanted bilaterally on the dorsal CeA via stereotaxic surgery.51,71 The CORT micropellets are a pharmacological tool to model CeA dysfunction induced by a chronic stressor. We initially showed that CORT micropellets on the CeA increase colonic sensitivity to colorectal distension (CRD) in the absence of histological damage to the amygdala.56 In subsequent experiments, we demonstrated that following amygdala implants of CORT there are profound and persistent effects on gene expression in the CeA including a downregulation of GR and an upregulation in CRH (Fig. 2).57 These findings suggest that elevating CORT induced prolonged changes to GR and CRH homeostasis in the CeA that persist despite depletion of the source of CORT. To advance these studies, we aimed to determine the relationship between CRH expression in the CeA and visceral hypersensitivity. We tested the hypothesis, using a loss-of-function approach, that preventing the increase in CRH expression would inhibit the visceral nociceptive behaviors induced by elevated amygdala CORT. We sought to investigate whether CRH expression within the CeA is a key regulator of heightened visceral nociceptive behaviors. We showed that CRH knockdown in the CeA using antisense oligodeoxynucleotide (ASO) targeting CRH in the CeA, but not non-targeting random sequence oligodeoxynucleotide, inhibits visceral hypersensitivity.72 However, the role of GR and/or MR expression in the regulation visceral nociceptive behaviors remained to be determined. Thus, we tested our next hypothesis that, within the CeA, selective knockdown of GR in the absence of the CORT micropellets could promote colonic hypersensitivity. We found that GR knockdown in the CeA using oligodeoxynucleotide of ASO targeting GR, but not random sequence, in stress-naive rats induced colonic hypersensitivity, mirroring the effect of the CORT micropellet.73 The GR mRNA expression was knocked down 67–88% which is comparable to the decrease in expression with CORT-implanted on the CeA and treated with vehicle-induced decrease in GR expression.73 In summary, to our knowledge we were the first to demonstrate that decreasing GR within the CeA was sufficient to induce visceral hypersensitivity in a stress-naïve animal. Taken together, our data shows that stress is associated with a loss of GR signaling and thus an impaired ability of the CeA to respond appropriately to stress. Key to building upon these observations and to further understand the underlying mechanisms of chronic stress-induced CeA dysfunction, we used the approach of examining whether a stressor itself drives alterations in amygdala function in a rodent model. We confirmed earlier work that daily exposure to water avoidance stress for 7–10 days increases visceral sensitivity to CRD.58,74,75 We then advanced these observations by demonstrating that the water avoidance stressor increased CRH and decreased GR expression in the CeA closely resembling that seen in rats with CORT micropellets on the CeA.61 In the water avoidance stress model, we found that CRH knockdown in the CeA inhibits the stress-induced visceral hypersensitivity.72
Sex Linked Differences in Visceral Sensitivity
From epidemiological studies, evidence has shown that IBS-patients are more commonly female.9,76,77 In developed countries, the estimated female bias for IBS is between 2 to 5 for every male IBS patient,78 which is similar to other chronic pain and affective disorders. For example visceral pain disorders such as functional dyspepsia or chronic pelvic pain, somatic pain disorders such as fibromyalgia or migraines, and affective disorders such as chronic fatigue syndrome, anxiety or depression, all have female-predominate sex ratios.7,78,79 These sex-related differences in symptom expression begin around puberty, with the surge of gonadal hormones, but continues to increase through the mid-forties.80 Interestingly, the rate of newly diagnosed IBS patients decreases after the age of 50 and the sex ratio for IBS patients is similar in the elderly.78 Clinical evidence suggests that there may be differences in IBS symptom expression between men and women; men with IBS are more likely to experience loose and more frequent stools,81 whereas women with IBS experience more bloating, abdominal distension, and infrequent, hard stools,82,83 although some women with IBS report increased episodes of diarrhea during menses.8 While peripheral mediators likely affect GI motility, gender-associated differences in visceral pain perception in IBS patients have been demonstrated using brain imaging techniques such as positron emission tomography.84 A study by Naliboff et al85 has shown that compared to men with IBS, women with IBS utilized different areas of their brain, such as the amygdala, while experiencing a rectal distension they perceived as aversive. Moreover, other clinical studies have provided evidence that women’s perception of visceral pain can be influenced by their cyclical changes in gonadal hormones.86–88
Characteristic features of IBS can be recapitulated in experimental models. For example, sex differences in pain responsiveness and differences in regional brain activity resembling that observed in IBS have been seen in male and female animals.89–94 In rodents experimental methodology that includes CRD to assess visceral sensitivity or a mechanical stimulus applied to the hindpaw or tail to assess somatic sensitivity, have uncovered sex differences in nociceptive behaviors following ELS, with responses in females being greater than males.92,95 Studies performed in adult rodent models have demonstrated that estrogen and progesterone modulate pain reporting, and that variations in the response to colonic distension occurred during the estrus cycle.88 Specifically, in rodent models, colonic sensitivity was increased during proestrus or estrus, with the highest plasma levels of estrogen and progesterone, compared to diestrus or metestrus with significantly lower circulating hormonal levels.88,89 Other studies support the concept that female hormones modulate visceral pain; we showed that CeA-CORT micropellet implantation visceral hypersensitivity in females only during proes-trus/estrus.96 Thus, clinical and preclinical data support a significant and complicated role for ovarian hormones to modulate not only pain perception, but also the underlying pain circuitry, which may promote the sexual dimorphism in IBS. Estrogen has been shown to be an important modulator of brain development, specifically influencing the plasticity of nociceptive circuits.97,98 In one study, direct administration of female hormones into the brain induced visceral hypersensitivity in adult female rats.99 Visceral hyperalgesia can also be induced in male rats by estrogen administration,100 further demonstrating that estrogen can be a pivotal modulator of visceral pain processing. Evidence suggests that, within the central nervous system, estrogen alters the expression of specific genes related to pain signaling to increase perception of peripheral nociceptive stimuli.101–103 These estrogen-dependent alterations in gene expression increase neuronal excitability by promoting synaptic plasticity leading to increased visceral sensitivity in females, especially during periods of high cycling estrogen.104 Another estrogen-mediated mechanism that could drive visceral hypersensitivity is via the induction of μ-opioid receptor internalization within the medial preoptic nucleus and the posterodorsal medial amygdala.105 At the level of the spinal cord, multiple studies have characterized estrogen as an important modulator of visceral nociceptive signaling, specifically through an effect on the N-methyl-D-aspartate receptor,106 metabotropic glutamate receptor 2 (mGluR2),107 and ionotropic glutamate receptor subunit 2B activity108 within the spinal cord.
Models of Stress-induced Visceral Hypersensitivity in Rodents
To model stress in preclinical models, researchers have developed numerous animal models. We recently reviewed the most relevant rodent models, along with potential mediators of visceral pain and the reader is referred to this review, Greenwood-Van Meerveld et al.109
Rodent Models of Adult Stress
To understand the central pathways and cellular mechanisms underlying changes observed in the human brain and to design novel therapeutics for stress-induced visceral pain, there are multiple rodent models of stress. The Wistar Kyoto rat is a spontaneous or genetically-induced model in which a high anxiety trait is associated with elevated colonic sensitivity as demonstrated by an increased visceromotor response (VMR) induced by low levels of CRD.110–114 In other models, adult animals are exposed to stressors such as restraint stress, water avoidance stress, and a chronic variable stress.58,74,115,116 In these models, there is an increase in plasma CORT resembling that seen in IBS patients and an increase in visceral sensitivity.
Rodent Models of Early Life Stress
Evidence suggests that stressful events during development can have long lasting effects. For example, neonatal adversity increases the likelihood of developing a functional gastrointestinal disorder in adulthood.117 To enhance our understanding of the mechanisms by which adversity in early life contribute to IBS, animal models permit longitudinal studies of the life-long effects of early life adversity on visceral pain perception. Adverse early childhood experiences, such as neglect, poverty, or an abusive caregiver, have been modeled by specific ELS models. Preclinical studies in these rodent models have provided important experimental evidence to suggest that brain circuits are primed by exposure to stress or pain during early life, predisposing individuals to chronic pain disorders as adults.118 Furthermore, in adulthood, these models of ELS have been shown to induce chronic, sexually dimorphic visceral hypersensitivity.119 As a model for neglect, maternal separation induces visceral hyperalgesia and enhanced HPA-activity in adulthood compared to non-separated controls. Visceral hypersensitivity has also been observed in adult rats following ELS induced by limited nesting, a model for poverty-associated neglect or abuse.120 Although valid for some types of ELS, maternal separation and limited nesting do not directly model abusive relationships in early life in order to assess visceral pain behaviors in adulthood. By relying on conditioned responses to an odor to model an abusive relationship, the odor attachment learning (OAL) model of ELS exploits key developmental time points by using different pairings of an odor and a shock to control for trauma predictability and to teach a preference for the conditioned odor. In this model, we have shown that neonatal female rats exposed to an unpredictable odor-shock pairing group showed a colonic hypersensitivity in adulthood compared to females in the predictable ELS group or odor only controls. In contrast, colonic sensitivity was unaffected in adult males exposed to any of the OAL treatments.94,121 Building upon our observation in female rats, we found that removal of all circulating ovarian hormones via ovariectomy after puberty reversed unpredictable ELS-induced colonic hypersensitivity, whilst estradiol replacement restored colonic hypersensitivity in those same animals. These data indicate an essential role for circulating ovarian hormones in females in the maintenance of ELS-induced chronic visceral pain.95 Ours was the first study to show sex-related differences in visceral sensitivity following unpredictable ELS and suggests that the activational effects of estradiol may maintain IBS-like symptomatology.
Any childhood abuse has the potential to alter an individual’s ability to cope with stress in adulthood by changing the development of the nervous system. This observation can be recapitulated in experimental models in which adult rats exposed to an ELS paradigm as neonates are subjected to an additional stressor such as a repetitive water avoidance stress. Under this multiple “hit” experimental paradigm there was enhanced colonic hypersensitivity to distension when compared to non-manipulated control groups.122 Although adult stress induced visceral hypersensitivity in all animals exposed to ELS, the effect of a second stress in adult animals showed a sex dependency, with female rats being more vulnerable to the chronic adult stressor.95 Particularly, adult female rats exposed to the predictable ELS developed an exaggerated visceral hypersensitivity that resembled the effect apparent in females who experienced unpredictable ELS as neonates.122 Our findings suggested to us that the resilience factor that previously allowed female animals in the predictable ELS group to be normosensitive was disrupted by repeated exposure to a stressful experience in adulthood. Taken together, the neonatal OAL model in conjunction with an adult stress, provide a solid foundation for exploring the mechanisms by which sex, early life adverse experiences, and adult stress act together to induce chronic pain in adulthood representing an opportunity for future investigations to enhance our understanding of the etiology of functional pain disorders that may lead to promising novel therapeutic targets.
Epigenetic Mechanisms That Contribute to Irritable Bowel Syndrome Symptomatology
Having shown that long term exposure of the amygdala elevated levels of CORT or repetitive stress decreases GR and increases CRH expression in the CeA that persist despite depletion of the source of CORT or removal of the stressor, an intriguing question is what are the underlying mechanism(s) leading to the prolonged disruption in GR and CRH-regulated gene transcription? There is the potential that these changes in gene expression may have a significant and long-term impact on the brain-gut axis, suggesting the involvement of epigenetic mechanisms within the brain to mediate stress-induced visceral hypersensitivity and provide a foundation for exploring epigenetic mechanisms that contribute to IBS symptomatology. Epigenetics does not describe alterations to the genomic DNA sequence itself but refers to phenotypic trait variations that result from environmental cues.123 The specific mechanisms through which these epigenetic variations develop encompass modifications that regulate nucleosome assembly (the histone octamer and associated DNA segments), which forms the basic unit of chromatin. Dynamic remodeling of chromatin structure by histone modifications, such as acetylation, changes accessibility of the associated DNA to RNA polymerase to result in differential gene expression. In addition to the histone modifications, epigenetic mechanisms include modification of the DNA structure through methylation that alters binding of the transcriptional machinery leading to a further level of gene regulation, a concept referred to as the epigenome.124 Epigenetic mechanisms also involve small RNAs, termed microRNA (miRNA), that are not transcribed and do not participate in translation, but instead regulate gene expression by causing degradation of specific mRNAs.125 Thus, miRNAs are indirect modulators of the epigenome by altering mRNA translation in response to environmental cues without affecting transcription through chromatin modification as with the other epigenetic mechanisms. We explored the hypothesis that chronic stress-induced visceral hypersensitivity could be regulated by epigenetic mechanisms within the CNS (Fig. 2). We found that central administration of trichostatin A (TSA), a histone deacetylase inhibitor, significantly inhibited visceral hypersensitivity in adult rats exposed to repeated WAS.61 Ours was the first study to demonstrate that stress-induced visceral hypersensitivity involved a central epigenetic mechanism, providing a rationale for future studies investigating whether IBS-like symptomatology involved additional epigenetic mechanisms. Subsequently, visceral hypersensitivity induced by a repeated stressor or by CORT was shown to modify histone acetylation in the brain and spinal cord, leading to specific changes in pro- and anti-nociceptive gene expression.61,62,126 DNA methylation patterns within the brain and an increase in the expression of pronociceptive neurotransmitters have also been seen in a model of stress-induced visceral pain.61 Through the use of currently available histone deacetylase inhibitors such as TSA and suberoylanilide hydroxamic acid (SAHA), in our laboratory, we showed that subjecting male rats to water avoidance stress-induced visceral hypersensitivity could be inhibited by intracerebro-ventricular infusions of TSA preceding the stress exposure.61 In a second study, we examined histone deacetylation in the brain using another model of visceral hypersensitivity induced by stereotaxic application of CORT to the CeA. Our study showed that prolonged exposure of the CeA to CORT produced not only visceral hypersensitivity but also deacetylation of histone 3 at lysine 9 (H3K9) at the GR promoter. Loss of promoter region acetylation lead to decreased GR expression within the CeA and a subsequent increase in the expression of CRH due to a loss of GR-mediated repression.119 Bilateral CeA-infusions of TSA or SAHA inhibited visceral hypersensitivity by preventing the change in histone acetylation.62 Concurrently, another laboratory employed the water avoidance stress model to investigate epigenetic mechanisms of visceral hypersensitivity within the dorsal root ganglion (DRG). They found that stress increased GR promoter methylation, causing a DRG-specific decrease in GR expression. The authors also found that exposing a male rat to the water avoidance stress had multiple additional effects on gene expression within the DRG including increased methylation of the cannabinoid receptor-1 promoter, causing decreased receptor expression and increased histone acetylation at the transient receptor potential cation channel subfamily V member 1 promoter, causing increased receptor expression.126 The stress-induced visceral hypersensitivity could be reversed through targeted knockdown of the DNA methyltransferase or the histone acetyltransferase that regulated the change in receptor expression.126 In a rodent model of chronic visceral hypersensitivity induced by neonatal maternal separation, a decrease in acetylation of histone 4 at lysine 12 in the lumbosacral spinal cord correlated with visceral hypersensitivity in adulthood.127 Furthermore, in a model of visceral hypersensitivity induced by 17β-estradiol in female rats, SAHA infused on to the lumbosacral spinal cord lead to hyperacetylation of H3K9 at the promoter for the metabotropic glutamate receptor-2 (mGLuR2).107 Counter intuitively, the SAHA-induced increase in mGluR2 expression inhibited the estradiol-induced visceral hypersensitivity.107
Evidence from models of chronic cystitis or esophageal reflux disease identified several miRNAs associated with chronic visceral pain.128,129 In a series of pivotal studies, Zhou and coworkers determined the importance of miR-29 on visceral hypersensitivity via a mechanism involving increased intestinal permeability.34,130,131 Increased expression of mi-R-29a and miR29b were associated with increased intestinal permeability in mice following stress exposure. In support of a role miR-29 they employed Mir29−/− mice and discovered that stress-induced intestinal permeability was significantly attenuated via a mechanism involving regulation of Claudin-1 mRNA expression.132
Through the use of animal models, the epigenetic modulation of gene expression in the early postnatal environment causes life-long alterations in pain responsiveness. Following exposure to ELS, epigenetically induced alterations in gene promoter accessibility regulate vulnerability or resilience to additional stressor in adulthood. Having previously shown that chronic psychological stress induces visceral hypersensitivity in adulthood via alterations in GR and CRH signaling within the CeA,61,72 whether the same mechanism(s) are involved following ELS remained to be unexplored. We therefore hypothesized that within the CeA, female-specific visceral hypersensitivity induced by exposure to unpredictable ELS, resulted in altered GR and CRH expression. Our results revealed marked differences in GR and CRH expression in adult female rats following both predictable and unpredictable ELS that were dependent on the context of the neonatal experience.133 We showed that GR expression in the CeA was increased in adult rats following predictable and unpredictable ELS, suggesting that in the CeA different mechanisms underlie ELS-induced and adult stress induced visceral hypersensitivity in the OAL model. GR has been shown to be a negative regulator of CRH via binding to the promoter region of the CRH gene to inhibit transcription.134 Increases in GR expression observed together with an increase in CRH following unpredictable ELS, suggest a dysfunction in the regulatory relationship between GR and CRH within the CeA. This mechanistic difference is likely a product of the complex interaction between the type of stress experienced and sex-related vulnerabilities. In support, we found that adult male rats exposed to an identical neonatal adverse early life experience showed no alterations in GR and CRH expression in the CeA, which supports our earlier observation that the colonic sensitivity was not significantly different between groups of adult males in the OAL model.133 These data suggest different mechanisms in the CeA in from adult rats exposed to ELS as compared to adult rats experiencing only adulthood stress. In an attempt to delineate the molecular mechanism within the CeA in adult rats exposed to ELS, we examined the role of CRH in modulating visceral hypersensitivity following ELS using targeted knockdown of CRH in the CeA via ASO sequences. Having shown that only unpredictable ELS increased CRH expression within the CeA of adult female rats, we found that following targeted knockdown of CRH in the CeA, there was an attenuation in the VMR to CRD following unpredictable ELS establishing that enhanced CRH expression underlies increased pain behaviors as a result of unpredictable ELS.133 In support, a selective CRH type-1 receptor antagonist administered directly into the CeA significantly decreased visceral hypersensitivity in the rats exposed to neonatal unpredictable ELS. These data provide compelling evidence that the predictability of an ELS experience plays a pivotal role in the reprograming of CRH expression in adulthood and the regulation of visceral hypersensitivity in a top-down manner through the CeA. Using a targeted knockdown approach, we also uncovered an inhibitory role of GR up-regulation on visceral hypersensitivity, as targeted knockdown of GR in the CeA resulted in an exaggerated visceral hypersensitivity in both predictable and unpredictable ELS groups compared to controls.133 Although not directly investigated in this study, these data suggest that up-regulation of GR serves as a compensatory mechanism within the CeA attempting to prevent the development of visceral hypersensitivity. To our knowledge, this is the first study to identify a potential protective role for GR up-regulation in the CeA following ELS. We speculate that disruption of this compensatory mechanism by GR knockdown could explain the exaggerated visceral hypersensitivity in animals exposed to ELS as compared to odor only controls.
Summary and Conclusion
Chronic physical and emotional stress can lead to potentially life-long visceral pain disorders such as IBS. Due to the complex etiology of functional bowel disorders, preclinical models are an essential tool for identifying and testing the efficacy of novel therapeutics. Researchers must strive to develop new animal models with multiple readouts that better mirror IBS and strengthen their translational relevance and predictive value for patients with IBS. Despite this lack of a perfect animal model that recapitulates all the symptoms of IBS, investigating the basic mechanisms of IBS-associated visceral pain can be done in experimental models. To date animal models have proven important for defining the central mechanisms of sensitization and nociceptive signaling, as well as discovering that chronic stress appears to be pivotal to all aspects of IBS in perpetuating and exacerbating abnormalities in GI function that resemble IBS including visceral hypersensitivity. We have provided evidence for a mechanism by which deregulation of corticosteroid receptors and CRH within the central amygdala induces stress-mediated chronic visceral pain. Given this link between altered amygdala function and stress-related IBS, we believe that understanding the central mechanisms of stress-induced visceral pain will be of significance for the future development of novel treatment options.
Acknowledgements
Greenwood-Van Meerveld is a Senior Research Career Scientist with the Department of Veterans Affairs (Award No. BX003610). Anthony C Johnson is a Career Development Awardee with the Department of Veterans Affairs (Award No. BX003630).
Footnotes
Financial support: None.
Conflicts of interest: None.
Author contributions: Beverley Greenwood-Van Meerveld drafted the first version of the manuscript, including the figures, and edited all subsequent versions; and Anthony C Johnson drafted the second version of the manuscript, finalized the figures, and edited all subsequent versions.
References
- 1.Drossman DA, Chang L, Bellamy N, et al. Severity in irritable bowel syndrome: a rome foundation working team report. Am J Gastroenterol. 2011;106:1749–1759. doi: 10.1038/ajg.2011.201. [DOI] [PubMed] [Google Scholar]
- 2.Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and rome IV. Gastroenterology. 2016;150:1262–1279. e2. doi: 10.1053/j.gastro.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 3.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 4.Grundmann O, Yoon SL. Irritable bowel syndrome: epidemiology, diagnosis and treatment: an update for health-care practitioners. J Gastroenterol Hepatol. 2010;25:691–699. doi: 10.1111/j.1440-1746.2009.06120.x. [DOI] [PubMed] [Google Scholar]
- 5.Choung RS, Locke GR., 3rd Epidemiology of IBS. Gastroenterol Clin North Am. 2011;40:1–10. doi: 10.1016/j.gtc.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Mearin F, Lacy BE, Chang L, et al. Bowel Disorders. Gastroenterology. 2016;150:1393–1407. e5. doi: 10.1053/j.gastro.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 7.Ouyang A, Wrzos HF. Contribution of gender to pathophysiology and clinical presentation of IBS: should management be different in women? Am J Gastroenterol. 2006;101(12 suppl):S602–S609. doi: 10.1111/j.1572-0241.2006.00975.x. [DOI] [PubMed] [Google Scholar]
- 8.Adeyemo MA, Spiegel BM, Chang L. Meta-analysis: do irritable bowel syndrome symptoms vary between men and women? Aliment Pharmacol Ther. 2010;32:738–755. doi: 10.1111/j.1365-2036.2010.04409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang L, Toner BB, Fukudo S, et al. Gender, age, society, culture, and the patient’s perspective in the functional gastrointestinal disorders. Gastroenterology. 2006;130:1435–1446. doi: 10.1053/j.gastro.2005.09.071. [DOI] [PubMed] [Google Scholar]
- 10.Bennett EJ, Tennant CC, Piesse C, Badcock CA, Kellow JE. Level of chronic life stress predicts clinical outcome in irritable bowel syndrome. Gut. 1998;43:256–261. doi: 10.1136/gut.43.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prusator DK, Andrews A, Greenwood-Van Meerveld B. Neurobiology of early life stress and visceral pain: translational relevance from animal models to patient care. Neurogastroenterol Motil. 2016;28:1290–1305. doi: 10.1111/nmo.12862. [DOI] [PubMed] [Google Scholar]
- 12.Roohafza H, Bidaki EZ, Hasanzadeh-Keshteli A, Daghaghzade H, Afshar H, Adibi P. Anxiety, depression and distress among irritable bowel syndrome and their subtypes: an epidemiological population based study. Adv Biomed Res. 2016;5:183. doi: 10.4103/2277-9175.190938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hertig VL, Cain KC, Jarrett ME, Burr RL, Heitkemper MM. Daily stress and gastrointestinal symptoms in women with irritable bowel syndrome. Nurs Res. 2007;56:399–406. doi: 10.1097/01.NNR.0000299855.60053.88. [DOI] [PubMed] [Google Scholar]
- 14.Maguen S, Madden E, Cohen B, Bertenthal D, Seal K. Association of mental health problems with gastrointestinal disorders in Iraq and Afghanistan veterans. Depress Anxiety. 2014;31:160–165. doi: 10.1002/da.22072. [DOI] [PubMed] [Google Scholar]
- 15.White DL, Savas LS, Daci K, et al. Trauma history and risk of the irritable bowel syndrome in women veterans. Aliment Pharmacol Ther. 2010;32:551–561. doi: 10.1111/j.1365-2036.2010.04387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang L, Sundaresh S, Elliott J, et al. Dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis in irritable bowel syndrome. Neurogastroenterol Motil. 2009;21:149–159. doi: 10.1111/j.1365-2982.2008.01171.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dinan TG, Quigley EM, Ahmed SM, et al. Hypothalamic-pituitary-gut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker? Gastroenterology. 2006;130:304–311. doi: 10.1053/j.gastro.2005.11.033. [DOI] [PubMed] [Google Scholar]
- 18.Fukudo S, Nomura T, Hongo M. Impact of corticotropin-releasing hormone on gastrointestinal motility and adrenocorticotropic hormone in normal controls and patients with irritable bowel syndrome. Gut. 1998;42:845–849. doi: 10.1136/gut.42.6.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kanuri N, Cassell B, Bruce SE, et al. The impact of abuse and mood on bowel symptoms and health-related quality of life in irritable bowel syndrome (IBS) Neurogastroenterol Motil. 2016;28:1508–1517. doi: 10.1111/nmo.12848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bradford K, Shih W, Videlock EJ, et al. Association between early adverse life events and irritable bowel syndrome. Clin Gastroenterol Hepatol. 2012;10:385–390. e3. doi: 10.1016/j.cgh.2011.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mayer EA, Naliboff BD, Chang L, Coutinho SV. V. stress and irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2001;280:G519–G524. doi: 10.1152/ajpgi.2001.280.4.G519. [DOI] [PubMed] [Google Scholar]
- 22.Ohman L, Simrén M. Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions. Nat Rev Gastroenterol Hepatol. 2010;7:163–173. doi: 10.1038/nrgastro.2010.4. [DOI] [PubMed] [Google Scholar]
- 23.O’Malley D, Quigley EM, Dinan TG, Cryan JF. Do interactions between stress and immune responses lead to symptom exacerbations in irritable bowel syndrome? Brain Behav Immun. 2011;25:1333–1341. doi: 10.1016/j.bbi.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 24.Barbara G, De Giorgio R, Stanghellini V, Cremon C, Corinaldesi R. A role for inflammation in irritable bowel syndrome? Gut. 2002;51(suppl 1):i41–i44. doi: 10.1136/gut.51.suppl_1.i41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barbara G, Cremon C, Carini G, et al. The immune system in irritable bowel syndrome. J Neurogastroenterol Motil. 2011;17:349–359. doi: 10.5056/jnm.2011.17.4.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marshall JK, Thabane M, Garg AX, Clark WF, Moayyedi P, Collins SM Walketon Health Study Investigators. Eight year prognosis of postinfectious irritable bowel syndrome following waterborne bacterial dysentery. Gut. 2010;59:605–611. doi: 10.1136/gut.2009.202234. [DOI] [PubMed] [Google Scholar]
- 27.Spence MJ, Moss-Morris R. The cognitive behavioural model of irritable bowel syndrome: a prospective investigation of patients with gastroenteritis. Gut. 2007;56:1066–1071. doi: 10.1136/gut.2006.108811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wouters MM, Vicario M, Santos J. The role of mast cells in functional GI disorders. Gut. 2016;65:155–168. doi: 10.1136/gutjnl-2015-309151. [DOI] [PubMed] [Google Scholar]
- 29.O’Sullivan M, Clayton N, Breslin NP, et al. Increased mast cells in the irritable bowel syndrome. Neurogastroenterol Motil. 2000;12:449–457. doi: 10.1046/j.1365-2982.2000.00221.x. [DOI] [PubMed] [Google Scholar]
- 30.Hughes PA, Harrington AM, Castro J, et al. Sensory neuroimmune interactions differ between irritable bowel syndrome subtypes. Gut. 2013;62:1456–1465. doi: 10.1136/gutjnl-2011-301856. [DOI] [PubMed] [Google Scholar]
- 31.Swan C, Duroudier NP, Campbell E, et al. Identifying and testing candidate genetic polymorphisms in the irritable bowel syndrome (IBS): association with TNFSF15 and TNFalpha. Gut. 2013;62:985–994. doi: 10.1136/gutjnl-2011-301213. [DOI] [PubMed] [Google Scholar]
- 32.Gwee KA, Collins SM, Read NW, et al. Increased rectal mucosal expression of interleukin 1beta in recently acquired post-infectious irritable bowel syndrome. Gut. 2003;52:523–526. doi: 10.1136/gut.52.4.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liebregts T, Adam B, Bredack C, et al. Immune activation in patients with irritable bowel syndrome. Gastroenterology. 2007;132:913–920. doi: 10.1053/j.gastro.2007.01.046. [DOI] [PubMed] [Google Scholar]
- 34.Camilleri M, Madsen K, Spiller R, Greenwood-Van Meerveld B, Verne GN. Intestinal barrier function in health and gastrointestinal disease. Neurogastroenterol Motil. 2012;24:503–512. doi: 10.1111/j.1365-2982.2012.01921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pigrau M, Rodiño-Janeiro BK, Casado-Bedmar M, et al. The joint power of sex and stress to modulate brain-gut-microbiota axis and intestinal barrier homeostasis: implications for irritable bowel syndrome. Neurogastroenterol Motil. 2016;28:463–486. doi: 10.1111/nmo.12717. [DOI] [PubMed] [Google Scholar]
- 36.Kelly JR, Kennedy PJ, Cryan JF, Dinan TG, Clarke G, Hyland NP. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392. doi: 10.3389/fncel.2015.00392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Farzaei MH, Bahramsoltani R, Abdollahi M, Rahimi R. The role of visceral hypersensitivity in irritable bowel syndrome: pharmacological targets and novel treatments. J Neurogastroenterol Motil. 2016;22:558–574. doi: 10.5056/jnm16001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van der Veek PP, Van Rood YR, Masclee AA. Symptom severity but not psychopathology predicts visceral hypersensitivity in irritable bowel syndrome. Clin Gastroenterol Hepatol. 2008;6:321–328. doi: 10.1016/j.cgh.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 39.Kanazawa M, Palsson OS, Thiwan SI, et al. Contributions of pain sensitivity and colonic motility to IBS symptom severity and predominant bowel habits. Am J Gastroenterol. 2008;103:2550–2561. doi: 10.1111/j.1572-0241.2008.02066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Keszthelyi D, Troost FJ, Masclee AA. Irritable bowel syndrome: methods, mechanisms, and pathophysiology. Methods to assess visceral hypersensitivity in irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2012;303:G141–G154. doi: 10.1152/ajpgi.00060.2012. [DOI] [PubMed] [Google Scholar]
- 41.Mertz H, Naliboff B, Munakata J, Niazi N, Mayer EA. Altered rectal perception is a biological marker of patients with irritable bowel syndrome. Gastroenterology. 1995;109:40–52. doi: 10.1016/0016-5085(95)90267-8. [DOI] [PubMed] [Google Scholar]
- 42.Ludidi S, Conchillo JM, Keszthelyi D, et al. Rectal hypersensitivity as hallmark for irritable bowel syndrome: defining the optimal cutoff. Neurogastroenterol Motil. 2012;24:729–733. e345–e346. doi: 10.1111/j.1365-2982.2012.01926.x. [DOI] [PubMed] [Google Scholar]
- 43.Maizels M, Aurora S, Heinricher M. Beyond neurovascular: migraine as a dysfunctional neurolimbic pain network. Headache. 2012;52:1553–1565. doi: 10.1111/j.1526-4610.2012.02209.x. [DOI] [PubMed] [Google Scholar]
- 44.Lampe A, Doering S, Rumpold G, et al. Chronic pain syndromes and their relation to childhood abuse and stressful life events. J Psychosom Res. 2003;54:361–367. doi: 10.1016/S0022-3999(02)00399-9. [DOI] [PubMed] [Google Scholar]
- 45.Scarinci IC, McDonald-Haile J, Bradley LA, Richter JE. Altered pain perception and psychosocial features among women with gastrointestinal disorders and history of abuse: a preliminary model. Am J Med. 1994;97:108–118. doi: 10.1016/0002-9343(94)90020-5. [DOI] [PubMed] [Google Scholar]
- 46.Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choiniere M. A systematic literature review of 10 years of research on sex/gender and pain perception - part 2: do biopsychosocial factors alter pain sensitivity differently in women and men? Pain. 2012;153:619–635. doi: 10.1016/j.pain.2011.11.026. [DOI] [PubMed] [Google Scholar]
- 47.Sapolsky RM, McEwen BS, Rainbow TC. Quantitative autoradiography of [3H]corticosterone receptors in rat brain. Brain Res. 1983;271:331–334. doi: 10.1016/0006-8993(83)90295-0. [DOI] [PubMed] [Google Scholar]
- 48.Reul JM, de Kloet ER. Two receptor systems for corticosterone in rat brain: microdistribution and differential occupation. Endocrinology. 1985;117:2505–2511. doi: 10.1210/endo-117-6-2505. [DOI] [PubMed] [Google Scholar]
- 49.Herman JP, Cullinan WE. Neurocircuitry of stress: central control of the hypothalamo-pituitary-adrenocortical axis. Trends Neurosci. 1997;20:78–84. doi: 10.1016/S0166-2236(96)10069-2. [DOI] [PubMed] [Google Scholar]
- 50.Schulkin J, Gold PW, McEwen BS. Induction of corticotropin-releasing hormone gene expression by glucocorticoids: implication for understanding the states of fear and anxiety and allostatic load. Psychoneuroendocrinology. 1998;23:219–243. doi: 10.1016/S0306-4530(97)00099-1. [DOI] [PubMed] [Google Scholar]
- 51.Shepard JD, Barron KW, Myers DA. Corticosterone delivery to the amygdala increases corticotropin-releasing factor mRNA in the central amygdaloid nucleus and anxiety-like behavior. Brain Res. 2000;861:288–295. doi: 10.1016/S0006-8993(00)02019-9. [DOI] [PubMed] [Google Scholar]
- 52.Herman JP, Figueiredo H, Mueller NK, et al. Central mechanisms of stress integration: hierarchical circuitry controlling hypothalamo-pituitary-adrenocortical responsiveness. Front Neuroendocrinol. 2003;24:151–180. doi: 10.1016/j.yfrne.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 53.Makino S, Gold PW, Schulkin J. Corticosterone effects on corticotro-pin-releasing hormone mRNA in the central nucleus of the amygdala and the parvocellular region of the paraventricular nucleus of the hypothalamus. Brain Res. 1994;640:105–112. doi: 10.1016/0006-8993(94)91862-7. [DOI] [PubMed] [Google Scholar]
- 54.McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 55.Perrin MH, Vale WW. Corticotropin releasing factor receptors and their ligand family. Ann N Y Acad Sci. 1999;885:312–328. doi: 10.1111/j.1749-6632.1999.tb08687.x. [DOI] [PubMed] [Google Scholar]
- 56.Greenwood-Van Meerveld B, Gibson M, Gunter W, Shepard J, Foreman R, Myers D. Stereotaxic delivery of corticosterone to the amygdala modulates colonic sensitivity in rats. Brain Res. 2001;893:135–142. doi: 10.1016/S0006-8993(00)03305-9. [DOI] [PubMed] [Google Scholar]
- 57.Tran L, Greenwood-Van Meerveld B. Altered expression of glucocorticoid receptor and corticotropin-releasing factor in the central amygdala in response to elevated corticosterone. Behav Brain Res. 2012;234:380–385. doi: 10.1016/j.bbr.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 58.Myers B, Greenwood-Van Meerveld B. Differential involvement of amygdala corticosteroid receptors in visceral hyperalgesia following acute or repeated stress. Am J Physiol Gastrointest Liver Physiol. 2012;302:G260–G266. doi: 10.1152/ajpgi.00353.2011. [DOI] [PubMed] [Google Scholar]
- 59.Myers B, Greenwood-Van Meerveld B. Corticosteroid receptor-mediated mechanisms in the amygdala regulate anxiety and colonic sensitivity. Am J Physiol Gastrointest Liver Physiol. 2007;292:G1622–G1629. doi: 10.1152/ajpgi.00080.2007. [DOI] [PubMed] [Google Scholar]
- 60.Myers B, Greenwood-Van Meerveld B. Elevated corticosterone in the amygdala leads to persistent increases in anxiety-like behavior and pain sensitivity. Behav Brain Res. 2010;214:465–469. doi: 10.1016/j.bbr.2010.05.049. [DOI] [PubMed] [Google Scholar]
- 61.Tran L, Chaloner A, Sawalha AH, Greenwood Van-Meerveld B. Importance of epigenetic mechanisms in visceral pain induced by chronic water avoidance stress. Psychoneuroendocrinology. 2013;38:898–906. doi: 10.1016/j.psyneuen.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 62.Tran L, Schulkin J, Ligon CO, Greenwood-Van Meerveld B. Epigenetic modulation of chronic anxiety and pain by histone deacetylation. Mol Psychiatry. 2015;20:1219–1231. doi: 10.1038/mp.2014.122. [DOI] [PubMed] [Google Scholar]
- 63.Wilder-Smith CH. The balancing act: endogenous modulation of pain in functional gastrointestinal disorders. Gut. 2011;60:1589–1599. doi: 10.1136/gutjnl-2011-300253. [DOI] [PubMed] [Google Scholar]
- 64.Elsenbruch S, Rosenberger C, Bingel U, Forsting M, Schedlowski M, Gizewski ER. Patients with irritable bowel syndrome have altered emotional modulation of neural responses to visceral stimuli. Gastroenterology. 2010;139:1310–1319. doi: 10.1053/j.gastro.2010.06.054. [DOI] [PubMed] [Google Scholar]
- 65.Hall GB, Kamath MV, Collins S, et al. Heightened central affective response to visceral sensations of pain and discomfort in IBS. Neurogastroenterol Motil. 2010;22:276–e80. doi: 10.1111/j.1365-2982.2009.01436.x. [DOI] [PubMed] [Google Scholar]
- 66.Hubbard CS, Hong J, Jiang Z, et al. Increased attentional network functioning related to symptom severity measures in females with irritable bowel syndrome. Neurogastroenterol Motil. 2015;27:1282–1294. doi: 10.1111/nmo.12622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tillisch K, Mayer EA, Labus JS. Quantitative meta-analysis identifies brain regions activated during rectal distension in irritable bowel syndrome. Gastroenterology. 2011;140:91–100. doi: 10.1053/j.gastro.2010.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Myers B, Greenwood-Van Meerveld B. Role of anxiety in the pathophysiology of irritable bowel syndrome: importance of the amygdala. Front Neurosci. 2009;3:47. doi: 10.3389/neuro.21.002.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87:873–904. doi: 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- 70.Schulkin J, McEwen BS, Gold PW. Allostasis, amygdala, and anticipatory angst. Neurosci Biobehav Rev. 1994;18:385–396. doi: 10.1016/0149-7634(94)90051-5. [DOI] [PubMed] [Google Scholar]
- 71.Shepard JD, Barron KW, Myers DA. Stereotaxic localization of corticosterone to the amygdala enhances hypothalamo-pituitary-adrenal responses to behavioral stress. Brain Res. 2003;963:203–213. doi: 10.1016/S0006-8993(02)03978-1. [DOI] [PubMed] [Google Scholar]
- 72.Johnson AC, Tran L, Greenwood-Van Meerveld B. Knockdown of corticotropin-releasing factor in the central amygdala reverses persistent viscerosomatic hyperalgesia. Transl Psychiatry. 2015;5:e517. doi: 10.1038/tp.2015.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Johnson AC, Greenwood-Van Meerveld B. Knockdown of steroid receptors in the central nucleus of the amygdala induces heightened pain behaviors in the rat. Neuropharmacology. 2015;93:116–123. doi: 10.1016/j.neuropharm.2015.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bradesi S, Schwetz I, Ennes HS, et al. Repeated exposure to water avoidance stress in rats: a new model for sustained visceral hyperalgesia. Am J Physiol Gastrointest Liver Physiol. 2005;289:G42–G53. doi: 10.1152/ajpgi.00500.2004. [DOI] [PubMed] [Google Scholar]
- 75.Hong S, Fan J, Kemmerer ES, Evans S, Li Y, Wiley JW. Reciprocal changes in vanilloid (TRPV1) and endocannabinoid (CB1) receptors contribute to visceral hyperalgesia in the water avoidance stressed rat. Gut. 2009;58:202–210. doi: 10.1136/gut.2008.157594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chial HJ, Camilleri M. Gender differences in irritable bowel syndrome. J Gend Specif Med. 2002;5:37–45. [PubMed] [Google Scholar]
- 77.Heitkemper M, Jarrett M. Irritable bowel syndrome: does gender matter? J Psychosom Res. 2008;64:583–587. doi: 10.1016/j.jpsychores.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 78.Mulak A, Taché Y, Larauche M. Sex hormones in the modulation of irritable bowel syndrome. World J Gastroenterol. 2014;20:2433–2448. doi: 10.3748/wjg.v20.i10.2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Meleine M, Matricon J. Gender-related differences in irritable bowel syndrome: potential mechanisms of sex hormones. World J Gastroenterol. 2014;20:6725–6743. doi: 10.3748/wjg.v20.i22.6725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Heitkemper MM, Chang L. Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome? Gend Med. 2009;(6 suppl 2):152–167. doi: 10.1016/j.genm.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Herman J, Pokkunuri V, Braham L, Pimentel M. Gender distribution in irritable bowel syndrome is proportional to the severity of constipation relative to diarrhea. Gend Med. 2010;7:240–246. doi: 10.1016/j.genm.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 82.Hyams JS, Burke G, Davis PM, Rzepski B, Andrulonis PA. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J Pediatr. 1996;129:220–226. doi: 10.1016/S0022-3476(96)70246-9. [DOI] [PubMed] [Google Scholar]
- 83.Talley NJ, Zinsmeister AR, Van Dyke C, Melton LJ., 3rd Epidemiology of colonic symptoms and the irritable bowel syndrome. Gastroenterology. 1991;101:927–934. doi: 10.1016/0016-5085(91)90717-Y. [DOI] [PubMed] [Google Scholar]
- 84.Berman S, Munakata J, Naliboff BD, et al. Gender differences in regional brain response to visceral pressure in IBS patients. Eur J Pain. 2000;4:157–172. doi: 10.1053/eujp.2000.0167. [DOI] [PubMed] [Google Scholar]
- 85.Naliboff BD, Berman S, Chang L, et al. Sex-related differences in IBS patients: central processing of visceral stimuli. Gastroenterology. 2003;124:1738–1747. doi: 10.1016/S0016-5085(03)00400-1. [DOI] [PubMed] [Google Scholar]
- 86.Hellstrom B, Anderberg UM. Pain perception across the menstrual cycle phases in women with chronic pain. Percept Mot Skills. 2003;96:201–211. doi: 10.2466/pms.2003.96.1.201. [DOI] [PubMed] [Google Scholar]
- 87.Kane SV, Sable K, Hanauer SB. The menstrual cycle and its effect on inflammatory bowel disease and irritable bowel syndrome: a prevalence study. Am J Gastroenterol. 1998;93:1867–1872. doi: 10.1111/j.1572-0241.1998.540_i.x. [DOI] [PubMed] [Google Scholar]
- 88.Sapsed-Byrne S, Ma D, Ridout D, Holdcroft A. Estrous cycle phase variations in visceromotor and cardiovascular responses to colonic distension in the anesthetized rat. Brain Res. 1996;742:10–16. doi: 10.1016/S0006-8993(96)00989-4. [DOI] [PubMed] [Google Scholar]
- 89.Iwasaki-Sekino A, Mano-Otagiri A, Ohata H, Yamauchi N, Shibasaki T. Gender differences in corticotropin and corticosterone secretion and corticotropin-releasing factor mRNA expression in the paraventricular nucleus of the hypothalamus and the central nucleus of the amygdala in response to footshock stress or psychological stress in rats. Psychoneuro-endocrinology. 2009;34:226–237. doi: 10.1016/j.psyneuen.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 90.Ji Y, Tang B, Traub RJ. The visceromotor response to colorectal distention fluctuates with the estrous cycle in rats. Neuroscience. 2008;154:1562–1567. doi: 10.1016/j.neuroscience.2008.04.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ji Y, Tang B, Cao DY, Wang G, Traub RJ. Sex differences in spinal processing of transient and inflammatory colorectal stimuli in the rat. Pain. 2012;153:1965–1973. doi: 10.1016/j.pain.2012.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kayser V, Berkley KJ, Keita H, Gautron M, Guilbaud G. Estrous and sex variations in vocalization thresholds to hindpaw and tail pressure stimulation in the rat. Brain Res. 1996;742:352–354. doi: 10.1016/S0006-8993(96)01108-0. [DOI] [PubMed] [Google Scholar]
- 93.Ralya A, McCarson KE. Acute estrogen surge enhances inflammatory nociception without altering spinal fos expression. Neurosci Lett. 2014;575:91–95. doi: 10.1016/j.neulet.2014.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vendruscolo LF, Pamplona FA, Takahashi RN. Strain and sex differences in the expression of nociceptive behavior and stress-induced analgesia in rats. Brain Res. 2004;1030:277–283. doi: 10.1016/j.brainres.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 95.Chaloner A, Greenwood-Van Meerveld B. Sexually dimorphic effects of unpredictable early life adversity on visceral pain behavior in a rodent model. J Pain. 2013;14:270–280. doi: 10.1016/j.jpain.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 96.Gustafsson JK, Greenwood-Van Meerveld B. Amygdala activation by corticosterone alters visceral and somatic pain in cycling female rats. Am J Physiol Gastrointest Liver Physiol. 2011;300:G1080–G1085. doi: 10.1152/ajpgi.00349.2010. [DOI] [PubMed] [Google Scholar]
- 97.Fitch RH, Denenberg VH. A role for ovarian hormones in sexual differentiation of the brain. Behav Brain Sci. 1998;21:311–327. doi: 10.1017/S0140525X98001216. [DOI] [PubMed] [Google Scholar]
- 98.Handa RJ, Burgess LH, Kerr JE, O’Keefe JA. Gonadal steroid hormone receptors and sex differences in the hypothalamo-pituitary-adrenal axis. Horm Behav. 1994;28:464–476. doi: 10.1006/hbeh.1994.1044. [DOI] [PubMed] [Google Scholar]
- 99.Myers B, Schulkin J, Greenwood-Van Meerveld B. Sex steroids localized to the amygdala increase pain responses to visceral stimulation in rats. J Pain. 2011;12:486–494. doi: 10.1016/j.jpain.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 100.Aloisi AM, Ceccarelli I. Role of gonadal hormones in formalin-induced pain responses of male rats: modulation by estradiol and naloxone administration. Neuroscience. 2000;95:559–566. doi: 10.1016/S0306-4522(99)00445-5. [DOI] [PubMed] [Google Scholar]
- 101.Vamvakopoulos NC, Chrousos GP. Evidence of direct estrogenic regulation of human corticotropin-releasing hormone gene expression. Potential implications for the sexual dimophism of the stress response and immune/inflammatory reaction. J Clin Invest. 1993;92:1896–1902. doi: 10.1172/JCI116782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Miller WJ, Suzuki S, Miller LK, Handa R, Uht RM. Estrogen receptor (ER)beta isoforms rather than ERalpha regulate corticotropin-releasing hormone promoter activity through an alternate pathway. J Neurosci. 2004;24:10628–10635. doi: 10.1523/JNEUROSCI.5540-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Uht RM, Anderson CM, Webb P, Kushner PJ. Transcriptional activities of estrogen and glucocorticoid receptors are functionally integrated at the AP-1 response element. Endocrinology. 1997;138:2900–2908. doi: 10.1210/endo.138.7.5244. [DOI] [PubMed] [Google Scholar]
- 104.Aloisi AM, Bonifazi M. Sex hormones, central nervous system and pain. Horm Behav. 2006;50:1–7. doi: 10.1016/j.yhbeh.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 105.Eckersell CB, Popper P, Micevych PE. Estrogen-induced alteration of muopioid receptor immunoreactivity in the medial preoptic nucleus and medial amygdala. J Neurosci. 1998;18:3967–3976. doi: 10.1523/JNEUROSCI.18-10-03967.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tang B, Ji Y, Traub RJ. Estrogen alters spinal NMDA receptor activity via a PKA signaling pathway in a visceral pain model in the rat. Pain. 2008;137:540–549. doi: 10.1016/j.pain.2007.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Cao DY, Bai G, Ji Y, Traub RJ. Epigenetic upregulation of metabotropic glutamate receptor 2 in the spinal cord attenuates oestrogen-induced visceral hypersensitivity. Gut. 2015;64:1913–1920. doi: 10.1136/gutjnl-2014-307748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ji Y, Bai G, Cao DY, Traub RJ. Estradiol modulates visceral hyperalgesia by increasing thoracolumbar spinal GluN2B subunit activity in female rats. Neurogastroenterol Motil. 2015;27:775–786. doi: 10.1111/nmo.12549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Greenwood-Van Meerveld B, Prusator DK, Johnson AC. Animal models of gastrointestinal and liver diseases. Animal models of visceral pain: pathophysiology, translational relevance, and challenges. Am J Physiol Gastrointest Liver Physiol. 2015;308:G885–G903. doi: 10.1152/ajpgi.00463.2014. [DOI] [PubMed] [Google Scholar]
- 110.Gunter WD, Shepard JD, Foreman RD, Myers DA, Greenwood-Van Meerveld B. Evidence for visceral hypersensitivity in high-anxiety rats. Physiol Behav. 2000;69:379–382. doi: 10.1016/S0031-9384(99)00254-1. [DOI] [PubMed] [Google Scholar]
- 111.Greenwood-Van Meerveld B, Johnson AC, Cochrane S, Schulkin J, Myers DA. Corticotropin-releasing factor 1 receptor-mediated mechanisms inhibit colonic hypersensitivity in rats. Neurogastroenterol Motil. 2005;17:415–422. doi: 10.1111/j.1365-2982.2005.00648.x. [DOI] [PubMed] [Google Scholar]
- 112.Johnson AC, Tran L, Schulkin J, Greenwood-Van Meerveld B. Importance of stress receptor-mediated mechanisms in the amygdala on visceral pain perception in an intrinsically anxious rat. Neurogastroenterol Motil. 2012;24:479–486. e219. doi: 10.1111/j.1365-2982.2012.01899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bravo JA, Dinan TG, Cryan JF. Alterations in the central CRF system of two different rat models of comorbid depression and functional gastrointestinal disorders. Int J Neuropsychopharmacol. 2011;14:666–683. doi: 10.1017/S1461145710000994. [DOI] [PubMed] [Google Scholar]
- 114.Gibney SM, Gosselin RD, Dinan TG, Cryan JF. Colorectal distension-induced prefrontal cortex activation in the Wistar-Kyoto rat: implications for irritable bowel syndrome. Neuroscience. 2010;165:675–683. doi: 10.1016/j.neuroscience.2009.08.076. [DOI] [PubMed] [Google Scholar]
- 115.Gué M, Del Rio-Lacheze C, Eutamene H, Théodorou V, Fioramonti J, Buéno L. Stress-induced visceral hypersensitivity to rectal distension in rats: role of CRF and mast cells. Neurogastroenterol Motil. 1997;9:271–279. doi: 10.1046/j.1365-2982.1997.d01-63.x. [DOI] [PubMed] [Google Scholar]
- 116.Winston JH, Xu GY, Sarna SK. Adrenergic stimulation mediates visceral hypersensitivity to colorectal distension following heterotypic chronic stress. Gastroenterology. 2010;138:294–304.e3. doi: 10.1053/j.gastro.2009.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Leserman J, Drossman DA. Relationship of abuse history to functional gastrointestinal disorders and symptoms: some possible mediating mechanisms. Trauma Violence Abuse. 2007;8:331–343. doi: 10.1177/1524838007303240. [DOI] [PubMed] [Google Scholar]
- 118.Beggs S, Currie G, Salter MW, Fitzgerald M, Walker SM. Priming of adult pain responses by neonatal pain experience: maintenance by central neuroimmune activity. Brain. 2012;135(pt 2):404–417. doi: 10.1093/brain/awr288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Prusator DK, Greenwood-Van Meerveld B. Sex-related differences in pain behaviors following three early life stress paradigms. Biol Sex Differ. 2016;7:29. doi: 10.1186/s13293-016-0082-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Prusator DK, Greenwood-Van Meerveld B. Gender specific effects of neonatal limited nesting on viscerosomatic sensitivity and anxiety-like behavior in adult rats. Neurogastroenterol Motil. 2015;27:72–81. doi: 10.1111/nmo.12472. [DOI] [PubMed] [Google Scholar]
- 121.Tyler K, Moriceau S, Sullivan RM, Greenwood-van Meerveld B. Long-term colonic hypersensitivity in adult rats induced by neonatal unpredictable vs predictable shock. Neurogastroenterol Motil. 2007;19:761–768. doi: 10.1111/j.1365-2982.2007.00955.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Prusator DK, Greenwood-Van Meerveld B. Sex differences in stress-induced visceral hypersensitivity following early life adversity: a two hit model. Neurogastroenterol Motil. 2016;28:1876–1889. doi: 10.1111/nmo.12891. [DOI] [PubMed] [Google Scholar]
- 123.Waddington CH. Canalization of development and the inheritance of acquired characters. Nature. 1942;150:563–565. doi: 10.1038/150563a0. [DOI] [PubMed] [Google Scholar]
- 124.Bernstein BE, Meissner A, Lander ES. The mammalian epigenome. Cell. 2007;128:669–681. doi: 10.1016/j.cell.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 125.Farh KK, Grimson A, Jan C, et al. The widespread impact of mammalian MicroRNAs on mRNA repression and evolution. Science. 2005;310:1817–1821. doi: 10.1126/science.1121158. [DOI] [PubMed] [Google Scholar]
- 126.Hong S, Zheng G, Wiley JW. Epigenetic regulation of genes that modulate chronic stress-induced visceral pain in the peripheral nervous system. Gastroenterology. 2015;148:148–157.e7. doi: 10.1053/j.gastro.2014.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Moloney RD, Stilling RM, Dinan TG, Cryan JF. Early-life stress-induced visceral hypersensitivity and anxiety behavior is reversed by histone deacetylase inhibition. Neurogastroenterol Motil. 2015;27:1831–1836. doi: 10.1111/nmo.12675. [DOI] [PubMed] [Google Scholar]
- 128.Zhang J, Banerjee B. Role of microRNA in visceral pain. J Neurogastroenterol Motil. 2015;21:159–171. doi: 10.5056/jnm15027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sengupta JN, Pochiraju S, Kannampalli P, et al. MicroRNA-mediated GABA Aα-1 receptor subunit down-regulation in adult spinal cord following neonatal cystitis-induced chronic visceral pain in rats. Pain. 2013;154:59–70. doi: 10.1016/j.pain.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhou Q, Zhang B, Verne GN. Intestinal membrane permeability and hypersensitivity in the irritable bowel syndrome. Pain. 2009;146:41–46. doi: 10.1016/j.pain.2009.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zhou Q, Verne GN. New insights into visceral hypersensitivity--clinical implications in IBS. Nat Rev Gastroenterol Hepatol. 2011;8:349–355. doi: 10.1038/nrgastro.2011.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhou Q, Costinean S, Croce CM, et al. MicroRNA 29 targets nuclear factor-κB-repressing factor and claudin 1 to increase intestinal permeability. Gastroenterology. 2015;148:158–169.e8. doi: 10.1053/j.gastro.2014.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Prusator DK, Greenwood-Van Meerveld B. Amygdala-mediated mechanisms regulate visceral hypersensitivity in adult females following early life stress: importance of the glucocorticoid receptor and corticotropin-releasing factor. Pain. 2017;158:296–305. doi: 10.1097/j.pain.0000000000000759. [DOI] [PubMed] [Google Scholar]
- 134.Yao M, Denver RJ. Regulation of vertebrate corticotropin-releasing factor genes. Gen Comp Endocrinol. 2007;153:200–216. doi: 10.1016/j.ygcen.2007.01.046. [DOI] [PubMed] [Google Scholar]