Abstract
The Department of Health’s ‘High Impact Intervention (HII) – Peripheral intravenous cannula care bundle’ lists six actions to be performed at the time of peripheral intravenous cannulation. Audit of compliance to these requires documentation. We assessed documentation on the anaesthetic charts of 50 surgical patients. Purpose-made stickers were then placed on all anaesthetic charts. Re-assessment of a further 50 patients’ charts demonstrated a significant improvement in documentation of the bundle post intervention (Fisher’s exact test P < 0.0001). This is an example of how a low-tech intervention can produce a high impact improvement in documentation.
Keywords: Peripheral venous access, peripheral cannulae, high impact intervention, documentation
Background
Peripheral intravenous cannulas are the most commonly used intravenous access in hospitalised patients. They are used in operating theatres for administration of medications, fluids and blood products as well as for blood sampling. They are usually considered a low-risk intervention; however, they may be associated with complications such as hematoma, phlebitis, pain and infection.
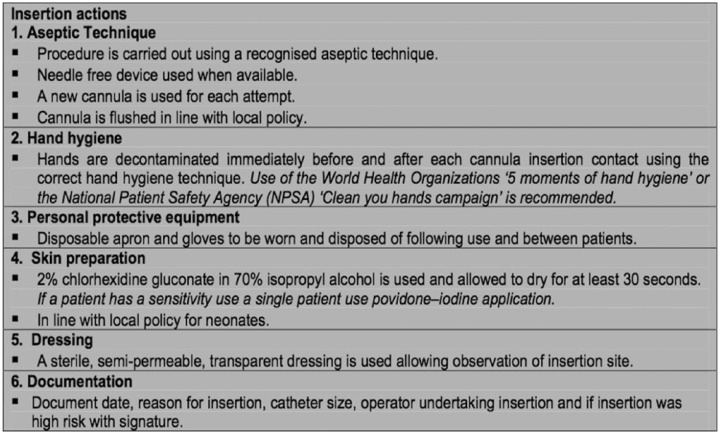
The ‘High Impact Intervention (HII) – Peripheral intravenous cannula care bundle’ lists six actions to be performed at the time of peripheral intravenous cannulation (Figure 1) (Department of Health, 2010). The aim of the care bundle is to ensure appropriate and high-quality patient care. Risk of infection is reduced when all elements within the clinical process are performed.
Figure 1.
Six actions in the Department of Health’s ‘High Impact Intervention – Peripheral intravenous cannula bundle’.
The Health and Social Care Act 2008: Code of Practice on the Prevention and Control of Infections and Related Guidance requires that ‘registered providers must audit compliance against key policies and procedures for infection prevention’ (Department of Health, 2015). Effective audit of compliance is only possible if documentation is complete.
Proper documentation is essential for continuity and legal documentation of care.
The Health and Care Professions Council (HCPC) on standards of conduct, performance and ethics 2016 states ‘Accurate and clear documentation of clinical record must be completed promptly as soon as possible after providing care, treatment or other services’ (Health and Care Professions Council, 2016).
The General Medical Council’s Good Medical Practice 2013 emphasises that registered doctors should maintain clear, accurate and legible documentation of clinical records (General Medical Council, 2013).
All actions within the bundle have been standard practice within our institution for many years; however, the anaesthetic charts currently in use in our hospital do not have a dedicated place for documentation of compliance with the care bundle.
The aim of this project was to assess compliance of documentation of peripheral line insertion in the anaesthetic department and to determine whether the use of sticker improves documentation of peripheral venous cannulation on the anaesthetic charts.
Methods
There are 20 main operating theatres and two postoperative recovery areas in our Trust. A two-part prospective audit was designed to collect data to measure documentation of peripheral venous cannulae sited in patients for elective surgical procedure before and after the proposed interventions.
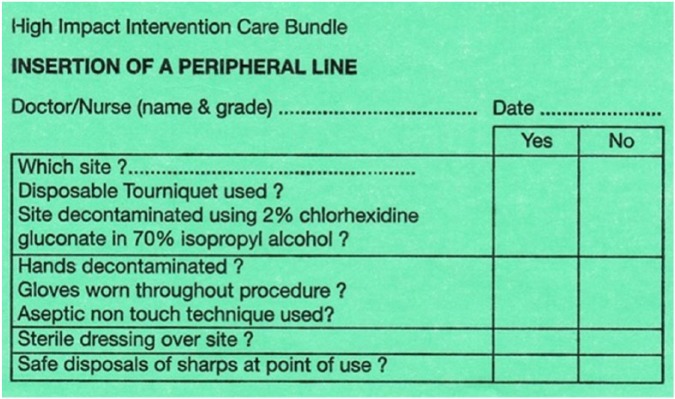
The proposed intervention was the placement of a green sticker that included date of insertion and name of the inserting anaesthetic doctor. It incorporated all the important elements of the high impact intervention care bundle such as asepsis, dressing and disposal of sharps.
A baseline audit measured documentation of the HII actions on the anaesthetic charts of 50 consecutive patients who had cannulae inserted in theatre. Purpose-made stickers of the HII care bundle actions were then placed on the anaesthetic charts of patients before surgery (Figure 2).
Figure 2.
Purpose- made stickers for documentation of the ‘HII – Peripheral intravenous cannula care bundle’ actions.
Data were subsequently collected from a further 50 patients’ anaesthetic charts post intervention.
Anaesthetists working in the operating theatres were not aware that data were being collected either pre or post intervention.
Results
The two-tailed Fisher’s exact test was used to calculate the P value. A P value < 0.001 is considered statistically highly significant.
The six HII actions for peripheral cannula insertion were documented in 1/50 patients (2%) prior to intervention and in 26/50 patients (52%) post intervention (Fisher’s exact test P < 0.0001).
Discussion
Placement of stickers on anaesthetic charts significantly improves the documentation of the six actions to be performed at the time of peripheral intravenous cannulation in the Department of Health’s ‘High Impact Intervention (HII) – Peripheral intravenous cannula care bundle’. Documentation of these is important in order to be able to demonstrate compliance with this standard.
Importantly, the improvement in documentation did not require education or behavioural change of those anaesthetists working in the operating theatres. In fact, since all actions within the bundle have been standard practice within our institution for many years, no behaviour change was necessary beyond improving documentation. Instead, the mere presence of a designated space to document the actions resulted in the improvement. With our project, we were able to assess the true impact of the sticker. We have only shown that this sticker is useful over a short period of time. It is uncertain as to whether this benefit will be maintained in distant future. To ensure sustainability of the project, future print runs of anaesthetic charts will be re-designed to include this space.
This is low-tech intervention, which produces a high-impact improvement in documentation of compliance with care standards.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Peer review statement: Not commissioned; blind peer-reviewed.
References
- Department of Health. (2010) UK Government Web Archive – The National Archives. London: Department of Health; Available at: http://hcai.dh.gov.uk/whatdoido/high-impact-interventions/ (accessed 19 April 2017). [Google Scholar]
- Department of Health. (2015) The Health and Social Care Act 2008: code of practice on the prevention and control of infections and related guidance. London: Department of Health; Available at: https://www.gov.uk/government/publications/the-health-and-social-care-act-2008-code-of-practice-on-the-prevention-and-control-of-infections-and-related-guidance (accessed 19 April 2017). [Google Scholar]
- General Medical Council (GMC). (2013) Record your work clearly, accurately and legibly. London: GMC; Available at: http://www.gmcuk.org/guidance/good_medical_practice/record_work.asp (accessed 19 April 2017). [Google Scholar]
- Health and Care Professions Council (HCPC). (2016) Standards of conduct, performance and ethics. London: HCPC; Available at: http://www.hcpc.uk.org/aboutregistration/standards/standardsofconductperformanceandethics/ (accessed 19 April 2017). [Google Scholar]