Abstract
Background:
Discrepancies exist in the literature regarding the association of the extent of injuries assessed on magnetic resonance imaging (MRI) with recovery times.
Hypothesis:
MRI-detected edema in grade 1 hamstring injuries does not affect the return to play (RTP).
Study Design:
Retrospective cohort study.
Level of Evidence:
Level 4.
Methods:
Grade 1 hamstring injuries from 22 professional soccer players were retrospectively reviewed. The extent of edema-like changes on fluid-sensitive sequences from 1.5-T MRI were evaluated using craniocaudal length, percentage of cross-sectional area, and volume. The time needed to RTP was the outcome. Negative binomial regression analysis tested the measurements of MRI-detected edema-like changes as prognostic factors.
Results:
The mean craniocaudal length was 7.6 cm (SD, 4.9 cm; range, 0.9-19.1 cm), the mean percentage of cross-sectional area was 23.6% (SD, 20%; range, 4.4%-89.6%), and the mean volume was 33.1 cm3 (SD, 42.6 cm3; range, 1.1-161.3 cm3). The mean time needed to RTP was 13.6 days (SD, 8.9 days; range, 3-32 days). None of the parameters of extent was associated with RTP.
Conclusion:
The extent of MRI edema in hamstring injuries does not have prognostic value.
Clinical Relevance:
Measuring the extent of edema in hamstring injuries using MRI does not add prognostic value in clinical practice.
Keywords: magnetic resonance imaging, hamstring injury, soccer, return to play
Muscle injuries of the lower limbs are common in soccer,7,8,13 with more than 90% affecting the 4 major muscle groups: the hamstrings, the posterior calf, the adductors, and the quadriceps.25,26 Such injuries are a major problem for professional athletes, accounting for up to one-third of all sports-related injuries6,14,18 and a large portion of time lost to competition.1,8,9 Magnetic resonance imaging (MRI) can visualize soft tissues with excellent contrast and provide high spatial resolution and multiplanar assessment, especially useful when muscle injury is suspected.12,16 Current evidence regarding prediction of the time needed to return to play (RTP) is mainly related to hamstring research,1,8,15 with several studies suggesting that a number of MRI findings are associated with the amount of time needed to RTP.3-5,11,21,24 The edema-like changes seen on MRI are almost always responsible for the boundaries of acute muscle injuries. Partial tears (grade 2 injuries) and intramuscular tendon disruption increase the time needed to RTP.3,8,21,22 Thus, it is likely that 2 muscle injuries affecting the same anatomical region and exhibiting the same extent length, volume, or cross-sectional area of edema would not yield the same prognosis if 1 of the injuries demonstrates a partial tear or an intramuscular tendon discontinuity and the other injury provided edema-like changes only. There are discrepancies in the literature regarding the association of the extent of muscle injuries with the time needed to RTP, and this is probably because previous works measured the extent of the edema-like changes without taking into account the presence of concomitant partial tears or intramuscular (central) tendon disruption within the area of edema. Thus, to demonstrate whether the extent of MRI-detected edema-like changes is associated with time needed to RTP, one should include muscle injuries exhibiting such features only.
To test the hypothesis that the amount of edema-like changes in acute muscle injuries is not associated with the time needed to RTP, we assessed the association of the extent of MRI-detected edema-like changes with the time needed to RTP in a sample of male professional soccer players sustaining MRI-defined grade 1 hamstring injuries.
Methods
This study was approved by the local institutional review board, which also waived the requirement for signed informed consent because of the retrospective nature of the study. We retrospectively reviewed the records of male professional soccer players from an elite club. Each had sustained an acute hamstring injury that immediately prevented the athlete from participating in training or competition and had been assessed using MRI within 48 to 72 hours after the injury occurred. The clinical and radiological records, dated from 2011 to 2013, were reviewed by a sports medicine physician and a physiatrist. Only players with a clinically diagnosed acute muscle injury of the posterior thigh, exhibiting positive findings of hamstring injury on the initial MRI reports, and with follow-up data regarding length of time to RTP were included in the analysis.
MRI Protocol and Assessment
Regarding the MRI protocol, all examinations were performed on the same 1.5-T MRI unit using a phased-array surface coil strapped over the region of interest of the affected limb and centered over the region of maximal tenderness, as identified by the player (skin markers were positioned accordingly). The protocol included coronal proton density (PD)–weighted fat-suppressed (FS) fast spin echo (FSE) (repetition time [TR], 3900 ms; echo time [TE], 25 ms; field of view [FOV], 23 × 33 cm; matrix, 256 × 320; slice thickness, 5 mm; interslice gap, 1 mm), sagittal PD-weighted FS FSE (TR, 3670 ms; TE, 25 ms; FOV, 26 × 33 cm; matrix, 256 × 320; slice thickness, 5 mm; interslice gap, 1 mm), axial T2-weighted FS FSE (TR, 5720 ms; TE, 74 ms; FOV, 28 × 28 cm; matrix, 355 × 448; slice thickness, 5 mm; interslice gap, 1.2 mm), and axial T1-weighted FSE (TR, 705 ms; TE, 11 ms; FOV, 28 × 28 cm; matrix, 355 × 448; slice thickness, 5 mm; interslice gap, 1.2 mm).
The MRI features of muscle injuries were assessed using consensus by 2 musculoskeletal radiologists with 2 and 9 years of clinical experience. Neither was aware of the clinical records of the players nor of the follow-up after injury and time to RTP. Injuries were assessed individually using all MRI sequences acquired in 3 planes to evaluate the entire extension and spectrum of injuries. The radiologists considered only the primary acute injury—the one exhibiting the greater extent and severity—for each player.
Severity of injuries was assessed using a modified Peetrons system for MRI evaluation8,19 as grade 1 (only edema-like changes are depicted, represented by an ill-defined high-signal abnormality on PD-weighted and T2-weighted sequences, exhibiting the characteristic “feathery” pattern) (Figure 1), grade 2 (in addition to the edema, a partial tear is depicted, represented by a well-defined high-signal abnormality on PD-weighted and T2-weighted sequences), and grade 3 (a complete tear is depicted).
Figure 1.
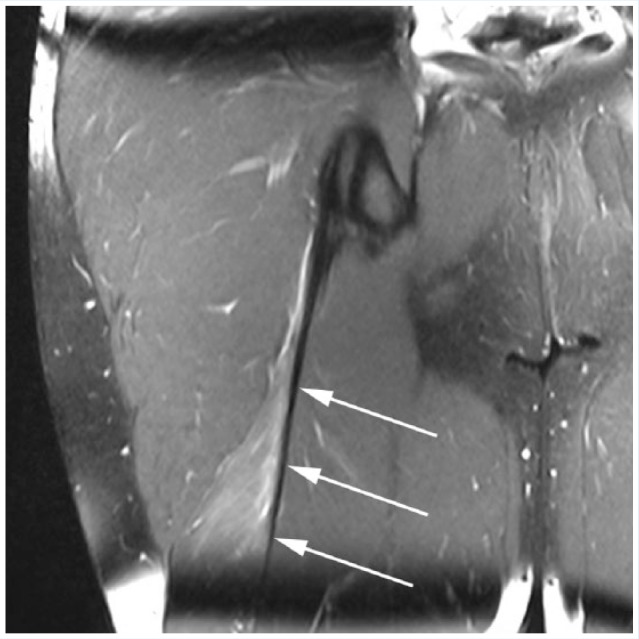
Acute hamstring injury adjacent to the proximal myotendinous junction of the long head of the biceps femoris muscle (coronal proton density–weighted fat-suppressed image) exhibiting the classic feathery pattern of edema. Note the normal appearance of the tendon at the proximal myotendinous junction (arrows).
The extent of the edema-like changes was assessed using 3 parameters: the craniocaudal (longitudinal) length, the percentage of cross-sectional area of muscle affected by edema, and its volume. Assessment of the percentage of the cross-sectional area was performed using the axial T2-weighted sequence, with the slice exhibiting the largest area of edema used as the reference for manual segmentation of the cross-sectional area of edema as well as the cross-sectional area of the muscle involved (in cm2). To assess the volume of the edema, the axial T2-weighted slice exhibiting the largest area of edema was also used to measure the maximal anteroposterior and transversal dimensions, and the coronal or sagittal PD-weighted image exhibiting the largest extent of edema was used to measure the craniocaudal length (in cm). The volume of edema was approximated by applying the formula for a prolate ellipsoid (π/6 × anteroposterior × transverse × craniocaudal).10
The morphology and signal of the intramuscular tendon (tendon adjacent the myotendinous junction, not corresponding to the free tendon) were evaluated. The normal intramuscular tendon usually exhibits regular contours and markedly low signal intensity in PD-weighted and T2-weighted sequences. If any of the following MRI features were present, the intramuscular tendon was considered abnormal (affected by injury): thickening and high signal intensity of the central tendon, with or without irregular contours, waviness of the tendon, and partial or complete disruption of the central tendon. Because it may affect the time needed to RTP, the presence of chronic changes depicted on MRI (abnormally low signal intensity depicted in all pulse sequences with architectural distortion of the muscle fibers) and the presence of proximal or distal free tendon injury were also evaluated.
Rehabilitation and RTP
After sustaining an acute muscle injury, control of pain and swelling was of critical importance for the first 72 hours. The RICE (rest, ice, compression, and elevation) protocol was followed together with intense electrical muscle stimulation for analgesia and to control swelling. After this first period, if needed, concentric mobilization was started together with light stretching exercises. Next, eccentric exercises were performed (always taking care not to elicit pain). The final part of the rehabilitation program focused on muscle strength balance (limb-to-limb) and hamstring-to-quadriceps ratio with continuing strengthening exercises and, finally, sport-specific drills. All athletes included in this study followed this treatment and rehabilitation protocol.
The time needed to RTP was noted as the number of days between each acute muscle injury (day 0) and the return to unrestricted activity in training or competition. The supervising sports medicine physician gave the definite clearance for RTP.
Statistical Analysis
To evaluate the effect of the extent of MRI-detected edema-like changes on the time needed to RTP, we included MRI-defined grade 1 muscle injuries only. All injuries exhibiting partial or complete tears (grades 2 and 3) and injuries exhibiting free tendon or intramuscular tendon involvement were not included in the analysis.
We tested whether an increase in the craniocaudal length, in the percentage of the cross-sectional area, or in the volume of MRI-detected edema-like changes was associated with an increase in the time needed to RTP. As the outcome (numbers of days away) are count data, Poisson or negative binomial regression analysis is suited to investigate the relationships. We first used Poisson regression to fit these count data, but we detected an overdispersion problem since the scaled deviance (value/degrees of freedom) was greater than 1 (4.74 for volume, 5.09 for percentage of cross-sectional area, 4.50 for craniocaudal length), and the goodness-of-fit chi-square test was statistically significant (P < 0.01). It indicated the Poisson regression model does not fit the data. Thus, we finally applied negative binomial regression instead to control the data overdispersion, which showed the scale deviance to be 1.08 for volume, percent cross-sectional area, and craniocaudal length separately. Statistical significance was set at 0.05. All analyses were performed using the SAS software, version 9.4 (SAS Institute).
Results
A total of 22 grade 1 acute hamstring injuries were included in the analysis. The mean player age was 25.6 years (SD, 5.1 years; range, 19-34 years). The long head of the biceps femoris was the most commonly affected muscle (n = 18, 81.8%).
Regarding the extent of MRI-detected edema-like changes, the mean craniocaudal length was 7.6 cm (SD, 4.9 cm; range, 0.9-19.1 cm), the mean percentage of cross-sectional area was 23.6% (SD, 20%; range, 4.4%-89.6%), and the mean volume was 33.1 cm3 (SD, 42.6 cm3; range, 1.1-161.3 cm3). The mean time needed to RTP was 13.6 days (SD, 8.9 days; range, 3-32 days). None of the muscle injuries included in this study exhibited MRI-detected chronic features. The associations of the extent of MRI-detected edema-like changes with the time needed to RTP considering hamstring injuries only are presented in Table 1. No associations with the time needed to RTP were found for any of the parameters tested. The calculated statistical power varied between 0.15 and 0.34 for the relationships assessed.
Table 1.
Negative binomial regression analysis to assess whether an increase in the extent of MRI-detected edema-like changes was associated with an increase in the number of days needed to RTP a
| Estimate | 95% CI | Exp (estimate) | 95% CI | P Value | |
|---|---|---|---|---|---|
| Edema volume | 0.005 | −0.001 to 0.011 | 1.005 | 0.999 to 1.011 | 0.13 |
| Edema, % CSA | 0.007 | −0.008 to 0.022 | 1.007 | 0.992 to 1.022 | 0.37 |
| CC length | 0.040 | −0.019 to 0.099 | 1.041 | 0.981 to 1.104 | 0.19 |
CC, craniocaudal; %CSA, percentage of cross-sectional area; Exp, exponential; MRI, magnetic resonance imaging; RTP, return to play.
No significant associations were demonstrated for all parameters tested.
Discussion
In this sample of acute, MRI-detected grade 1 hamstring injuries in soccer players, no associations with the time needed to RTP were found for any of the parameters of extent of edema-like changes tested. Previous studies demonstrated a relationship between the extent of injuries,4,11 mainly the craniocaudal (longitudinal) length and the percentage of the cross-sectional area of lesions affecting the hamstring muscles, and recovery time.2,23 Two previous studies demonstrated only a moderate correlation between the MRI-assessed craniocaudal length of hamstring injuries and RTP.4,23 Another study demonstrated substantial correlations of both MRI-detected craniocaudal length and cross-sectional area of hamstring injuries with RTP.11 According to these studies, more extensive injuries, meaning basically more extensive edema-like changes, were associated with longer recovery times. However, some discrepancies exist in the literature regarding the association of the extent of injuries with recovery times and specific measurements or parameters showing prognostic value in some studies but not others. A previous study demonstrated a weak association between the MRI-assessed craniocaudal length of hamstring injuries and the number of games missed, although such association was statistically significant.2 A recent prospective study showed that the MRI-assessed extent of acute injuries of the hamstring was not associated with the time needed to RTP.17 Furthermore, a recent systematic review demonstrated that there is no strong evidence for an association between the MRI-assessed extent of acute muscle injuries and the time needed to RTP.22
The lack of consistency regarding the association between the extent of muscle injuries and RTP could be explained by the fact that the majority of the previous studies measured the boundaries of the edema-like changes depicted on fluid-sensitive MRI sequences, almost always responsible for the greater extent of acute muscle injuries, without taking into account the presence (or absence) of concomitant macroscopic tears or intramuscular tendon involvement within the area of edema. By not excluding the presence of partial macroscopic tears (grade 2 injuries) or the presence of intramuscular tendon discontinuity within the area of edema, one cannot be sure which imaging factor is playing a role on the increase in the time needed to RTP.3,8,21
To the best of our knowledge, this is the first study to assess the associations of different measures of the extent of edema-like changes depicted on MRI with the time needed to RTP by including MRI-defined grade 1 acute hamstring injuries only. None of the MRI-assessed muscle injuries included in our analyses exhibited macroscopic tears of muscle fibers, free tendon involvement, or intramuscular tendon discontinuity. Thus, we could focus specifically on whether the extent of the edema-like changes alone can help predict the time needed to RTP.
We found no significant associations of craniocaudal length, edema volume, or percentage of the cross-sectional area of muscle affected by edema with the time needed to RTP in this sample of acute hamstring injuries. Our results potentially open the discussion of whether measuring the extent of acute muscle injuries on MRI is useful with regard to prognosis. Furthermore, we feel that our results should be taken into account when applying classification systems for acute muscle injuries. A recent classification system of acute muscle injuries using MRI included the evaluation of longitudinal length and percentage of cross-sectional area of injuries when assessing their severity.20
MRI features other than the extent of hamstring injuries were evaluated by previous works, with some features demonstrating usefulness in predicting the time needed to RTP. Clinically suspected acute hamstring injuries exhibiting negative (normal) MRI were shown to be related to shorter recovery times compared with those injuries exhibiting positive MRI findings, especially injuries exhibiting at least partial macroscopic tears on MRI.8 The involvement of the intramuscular tendon (at the myotendinous junction) was demonstrated to be related to longer recovery times compared with hamstring injuries without such involvement, especially when discontinuity of the intramuscular tendon is present.3,21 Thus, instead of measuring the extent of acute hamstring injuries, it would probably be more relevant to depict other MRI features existing within the area of edema, such as macroscopic tears or intramuscular (central) tendon involvement.3,8,21
Our study has some limitations. First, as in all elite sports environments, the supervising sports medicine physician responsible for the definite clearance for RTP was not blinded to the initial MRI findings, which might have introduced bias regarding the decision. Second, this study lacks substantial statistical power because of the low number of injuries included. However, this is a very homogeneous sample of pure grade 1 acute hamstring injuries in soccer players completing the same rehabilitation protocol (no associated partial or complete tears, no tendon involvement, and no evidence of chronic injury in muscles affected), which is a strength of this study. Finally, we cannot rule out the influence of potential previous injuries on the time needed to RTP. To minimize such influence, we carefully searched for MRI features of chronic muscle injuries associated with acute findings, and none of the grade 1 injuries included in this study exhibited MRI-detected chronic features.
Conclusion
This study provides no evidence that the extent of MRI-detected edema-like changes in grade 1 acute hamstring injuries is associated with the time needed to RTP in this sample of professional soccer players. As MRI-detected edema-like changes represent the boundaries of the majority of acute muscle injuries, being responsible for their greater extent, we question the usefulness of measuring the extent of muscle injuries for prognostic purposes, including in those classification systems currently available.
Acknowledgments
The authors would like to thank Ricardo Sasaki, PT, and Ling Li, PhD, for their great help with data collection and analysis.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2007;35:197-206. [DOI] [PubMed] [Google Scholar]
- 2. Cohen SB, Towers JD, Zoga A, et al. Hamstring injuries in professional football players: magnetic resonance imaging correlation with return to play. Sports Health. 2011;3:423-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Comin J, Malliaras P, Baquie P, Barbour T, Connell D. Return to competitive play after hamstring injuries involving disruption of the central tendon. Am J Sports Med. 2013;41:111-115. [DOI] [PubMed] [Google Scholar]
- 4. Connell DA, Schneider-Kolsky ME, Hoving JL, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183:975-984. [DOI] [PubMed] [Google Scholar]
- 5. Cross TM, Gibbs N, Houang MT, Cameron M. Acute quadriceps muscle strains: magnetic resonance imaging features and prognosis. Am J Sports Med. 2004;32:710-719. [DOI] [PubMed] [Google Scholar]
- 6. Darrow CJ, Collins CL, Yard EE, Comstock RD. Epidemiology of severe injuries among United States high school athletes: 2005-2007. Am J Sports Med. 2009;37:1798-1805. [DOI] [PubMed] [Google Scholar]
- 7. Ekstrand J, Hägglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39:1226-1232. [DOI] [PubMed] [Google Scholar]
- 8. Ekstrand J, Healy JC, Walden M, Lee JC, English B, Hägglund M. Hamstring muscle injuries in professional football: the correlation of MRI findings with return to play. Br J Sports Med. 2012;46:112-117. [DOI] [PubMed] [Google Scholar]
- 9. Elliott MC, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39:843-850. [DOI] [PubMed] [Google Scholar]
- 10. Geirsson RT, Christie AD, Patel N. Ultrasound volume measurements comparing a prolate ellipsoid method with a parallel planimetric area method against a known volume. J Clin Ultrasound. 1982;10:329-332. [DOI] [PubMed] [Google Scholar]
- 11. Gibbs NJ, Cross TM, Cameron M, Houang MT. The accuracy of MRI in predicting recovery and recurrence of acute grade one hamstring muscle strains within the same season in Australian Rules football players. J Sci Med Sport. 2004;7:248-258. [DOI] [PubMed] [Google Scholar]
- 12. Hayashi D, Hamilton B, Guermazi A, de Villiers R, Crema MD, Roemer FW. Traumatic injuries of thigh and calf muscles in athletes: role and clinical relevance of MR imaging and ultrasound. Insights Imaging. 2012;3:591-601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Junge A, Dvorak J, Graf-Baumann T, Peterson L. Football injuries during FIFA tournaments and the Olympic Games, 1998-2001: development and implementation of an injury-reporting system. Am J Sports Med. 2004;32(1 suppl):80S-89S. [DOI] [PubMed] [Google Scholar]
- 14. Junge A, Engebretsen L, Mountjoy ML, et al. Sports injuries during the Summer Olympic Games 2008. Am J Sports Med. 2009;37:2165-2172. [DOI] [PubMed] [Google Scholar]
- 15. Kerkhoffs GM, van Es N, Wieldraaijer T, Sierevelt IN, Ekstrand J, van Dijk CN. Diagnosis and prognosis of acute hamstring injuries in athletes. Knee Surg Sports Traumatol Arthrosc. 2013;21:500-509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Koulouris G, Connell D. Hamstring muscle complex: an imaging review. Radiographics. 2005;25:571-586. [DOI] [PubMed] [Google Scholar]
- 17. Moen MH, Reurink G, Weir A, Tol JL, Maas M, Goudswaard GJ. Predicting return to play after hamstring injuries. Br J Sports Med. 2014;48:1358-1363. [DOI] [PubMed] [Google Scholar]
- 18. Orchard J, Seward H. Epidemiology of injuries in the Australian Football League, seasons 1997-2000. Br J Sports Med. 2002;36:39-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peetrons P. Ultrasound of muscles. Eur Radiol. 2002;12:35-43. [DOI] [PubMed] [Google Scholar]
- 20. Pollock N, James SL, Lee JC, Chakraverty R. British athletics muscle injury classification: a new grading system. Br J Sports Med. 2014;48:1347-1351. [DOI] [PubMed] [Google Scholar]
- 21. Pollock N, Patel A, Chakraverty J, Suokas A, James SL, Chakraverty R. Time to return to full training is delayed and recurrence rate is higher in intratendinous (‘c’) acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med. 2016;50:305-310. [DOI] [PubMed] [Google Scholar]
- 22. Reurink G, Brilman EG, de Vos RJ, et al. Magnetic resonance imaging in acute hamstring injury: can we provide a return to play prognosis? Sports Med. 2015;45:133-146. [DOI] [PubMed] [Google Scholar]
- 23. Schneider-Kolsky ME, Hoving JL, Warren P, Connell DA. A comparison between clinical assessment and magnetic resonance imaging of acute hamstring injuries. Am J Sports Med. 2006;34:1008-1015. [DOI] [PubMed] [Google Scholar]
- 24. Slavotinek JP, Verrall GM, Fon GT. Hamstring injury in athletes: using MR imaging measurements to compare extent of muscle injury with amount of time lost from competition. AJR Am J Roentgenol. 2002;179:1621-1628. [DOI] [PubMed] [Google Scholar]
- 25. Volpi P, Melegati G, Tornese D, Bandi M. Muscle strains in soccer: a five-year survey of an Italian major league team. Knee Surg Sports Traumatol Arthrosc. 2004;12:482-485. [DOI] [PubMed] [Google Scholar]
- 26. Walden M, Hägglund M, Ekstrand J. UEFA Champions League study: a prospective study of injuries in professional football during the 2001-2002 season. Br J Sports Med. 2005;39:542-546. [DOI] [PMC free article] [PubMed] [Google Scholar]


