Abstract
Animal-free (AF) SERVA Collagenase AF-1 and Neutral Protease (NP) AF GMP Grade have recently become available for human islet isolation. This report describes the initial experiences of 3 different islet transplant centers. Thirty-four human pancreases were digested using 1 vial of the 6 different lots of Collagenase AF-1 (2,000–2,583 PZ-U/vial) supplemented with 4 different lots of NP AF in a range of 50 to 160 DMC-U per pancreas. Isolation, culture, and quality assessment were performed using standard techniques as previously described. All data are presented as mean ± standard error of the mean (SEM). Variability of pancreas weight was associated with a wide range of collagenase and NP activities, ranging from 12.7 to 46.6 PZ-U/g (26.0 ± 1.5 PZ-U/g) and 0.4 to 3.0 DMC-U/g (1.5 ± 0.1 DMC-U/g), respectively. Postpurification islet yield was 296,494 ± 33,620 islet equivalents (IEQ) equivalent to 3,274 ± 450 IEQ/g with a purity of 55.9% ± 3.2%. Quality assessment performed after 2 to 4 d of culture demonstrated a viability of 88.1% ± 1.5% and a stimulation index of 3.7 ± 0.7. Eighteen of the 34 preparations were transplanted into type 1 diabetic patients equivalent to a transplantation rate of 52.9%. Six preparations, which were infused into patients as first transplant, could be analyzed and increased the fasting C-peptide level from 0.11 ± 0.08 pretransplant to 1.23 ± 0.24 and 2.27 ± 0.31 ng/mL 3 and 6 mo posttransplant (P < 0.05), respectively. Insulin requirements were simultaneously reduced at the same time from 39.2 ± 3.8 IU/d before transplantation to 10.8 ± 4.1 and 4.0 ± 2.3 IU/d, after 3 and 6 mo posttransplant (P < 0.05), respectively. This study demonstrates the efficiency of AF SERVA Collagenase AF-1 and NP AF for clinical islet isolation and transplantation. The new plant-based production process makes these products a safe new option for the islet field.
Keywords: human islet isolation, human islet transplantation, collagenase, islet quality assessment
Introduction
The transplantation of isolated human islets has been established as a treatment for patients with type 1 diabetes to restore glucose counterregulation and to improve the insulin secretory response.1–3 The successful release of islets from the human pancreas essentially requires the synergistic interaction between collagenase and supplementary proteases produced by the bacterium Clostridium histolyticum or Bacillus thermoproteolyticus rokko. 4 Until now, the production of enzymes by different bacteria depends on the fermentation of animal-derived nutrients. In the past, manufacturing of some enzyme blends used the fermentation of material derived from bovine brain and heart tissue. Neuronal tissue from cattle was identified as one of the main risks for zoonotic transmission of misfolded proteins, termed prions, to humans.5 Prions are the causative agent for a group of neuronal disorders that include the bovine spongiform encephalopathy and different variants of the Creutzfeldt-Jakob disease (CJD).6 For that reason, reagents from animal origin, such as bovine serum or bovine serum albumin (BSA), have been banned from the human islet isolation procedure when performed for clinical purposes.7 In addition to mammals, even distantly related species, such as fish, are under investigation for the potential risk of prion transmission.8,9
In accordance with this preventive strategy, SERVA and Nordmark developed a manufacturing process that uses plant-based ingredients to produce animal-free (AF) Good Manufacturing Practice (GMP)-grade collagenase and neutral protease (NP). This report describes the initial experiences made in 3 different islet transplant centers utilizing Collagenase AF-1 and NP AF for the isolation of islets from 34 human pancreases.
Materials and Methods
Pancreases were retrieved with appropriate consent and ethical approval from 34 human multiorgan donors utilizing cold perfusion with Institute Georges Lopez–1(IGL-1) solution (IGL, Lissieu, France, n = 15), University of Wisconsin solution (Bridge to Life Ltd., London, United Kingdom, n = 10), histidine–tryptophan–ketoglutarate (Custodiol, Köhler Chemie GmbH, Alsbach, Germany, n = 3), Solution de Conservation des Organes et des Tissus (SCOT)-15 solution (Maco Pharma, Mouvaux, France, n = 4), and Celsior solution (IGL, n = 2). The donors (16 female/18 male) were characterized by a mean age of 51.4 ± 1.9 years, a body mass index of 25.3 ± 0.7, and a cold ischemia time of 7.3 ± 0.3 h.
After arrival at the human islet isolation facilities (Cell Isolation and Transplantation Center, Department of Surgery, Geneva University Hospital, Geneva, Switzerland, Switzerland; Department of Immunology, Genetics and Pathology, Uppsala University, Sweden; and Nuffield Department of Surgical Sciences, Oxford University, United Kingdom), islets were isolated and purified as previously described.10–12 In detail, pancreas digestion was performed utilizing 1 vial of the 6 different lots of intraductally infused Collagenase AF-1 (2,000–2,583 PZ-U per vial) supplemented with 4 different lots of NP AF (SERVA/Nordmark Arzneimittel GmbH & Co. KG, Uetersen, Germany) added in a range of 50 to 160 DMC-U per pancreas. Integrity of collagenase classes I and II was previously assessed by a chromatograph equipped with an anion exchange Mono-Q column.
Subsequent to purification and after 2 to 4 d of culture, islet yield was determined in a standardized procedure converting islet yield to islet equivalents (IEQ) with an average diameter of 150 µm.13 Isolated islets were distinguished from exocrine tissue using insulin-specific dithizone staining (Sigma-Aldrich AB, Stockholm, Sweden).13 Viability and in vitro function of purified islets were assessed after 2 to 4 d of culture at 37 °C as previously described in detail.10–12
Isolations were categorized as failed when less than 100,000 IEQ were isolated from 1 donor pancreas.14,15 Isolation outcome was defined to be successful when total islet yield was more than 250,000 IEQ per pancreas.16,17 Product release criteria for clinical islet transplantation were ≥5,000 IEQ per kg recipient’s body weight, viability of ≥70%, purity of ≥30%, packed tissue volume of ≤7 mL, stimulation index of ≥1.0, endotoxin of ≤5 EU/kg, and the absence of bacterial contaminations determined as gram negative stain.18 Posttransplant function of islets transplanted into patients with type 1 diabetes mellitus was assessed by self-monitoring of blood glucose levels and documentation of insulin requirements. Plasma C-peptide levels and HbA1c were measured at follow-up visits 3 and 6 mo after transplantation utilizing standard methods.19,20 The C-peptide to glucose ratio was calculated as described by Faradji et al.21
Data Analysis
All statistical analysis was performed utilizing Prism version 6.0h for MacIntosh (GraphPad, La Jolla, CA, USA) and SPSS version 24.0.0.1. Correlation analysis of data was carried out by Spearman’s rank correlation. Islet graft function was analyzed at 3 and 6 mo posttransplant utilizing Dunn’s multiple comparison following the Friedman test. Differences were considered significant at P < 0.05. P values > 0.05 are termed nonsignificant. For clarity, results are expressed as mean ± standard error of the mean (SEM) rather than the correct nonparametric measures of median and quartiles.
Results
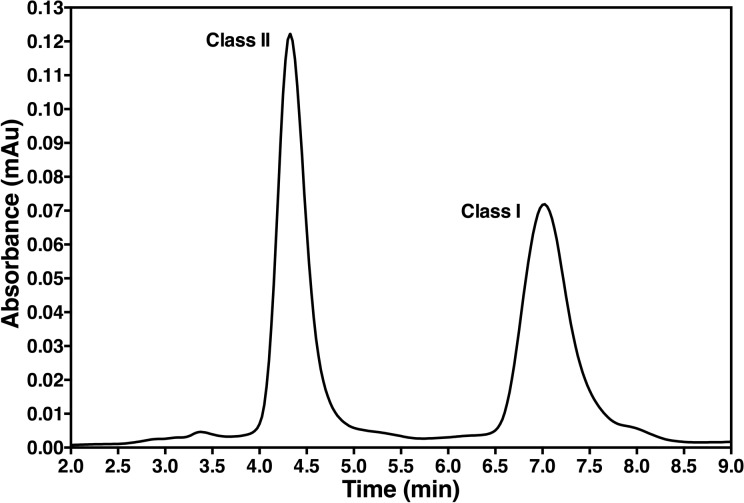
Collagenase integrity was assessed using Mono-Q chromatography. As shown in Fig. 1, the new manufacturing process did not affect the integrity of collagenase classes I and II. The collagenase classes II to I ratio of the 6 lots used in this study varied with a standard deviation of 0.09.
Fig. 1.
Mono-Q chromatography analysis of animal-free collagenase 1 (AF-1) performed at a wavelength of 280 nm (Nordmark Arzneimittel GmbH & Co. KG, Uetersen, Germany). The graph is representative for the 6 collagenase lots used in this study.
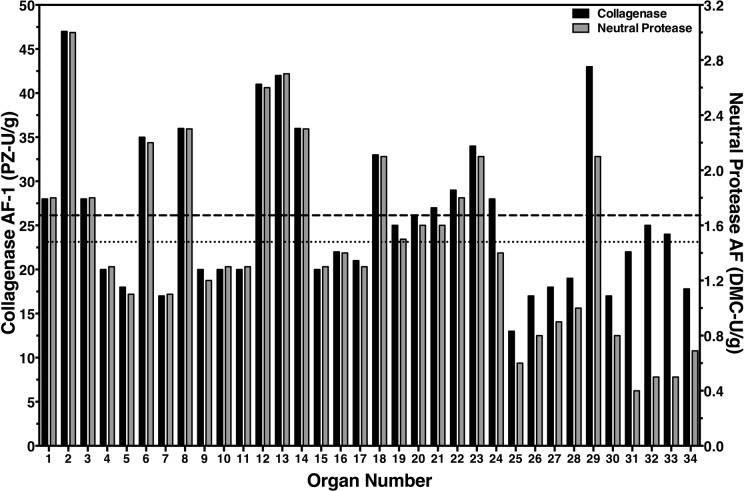
The variability of pancreas weight (47–164 g) was associated with a wide range of collagenase and NP activities which varied from 12.7 to 46.6 PZ-U/g and 0.4 to 3.0 DMC-U/g, respectively (Fig. 2). As a result, recirculation time required for significant islet release from the digested pancreas ranged from 13 to 41 min (21.5 ± 0.9 min). The percentage of nondigested tissue remaining in the digestion chamber after pancreas dissociation was 14.1% ± 1.3% varying from 1.3% to 33.0%.
Fig. 2.
Individual amount of intraductally perfused animal-free (AF) collagenase 1 (AF-1; black bars, left y-axis) and neutral protease AF activity (gray bars, right y-axis) per gram trimmed pancreas weight. The dashed and dotted lines indicate the mean of collagenase and neutral protease activity, respectively.
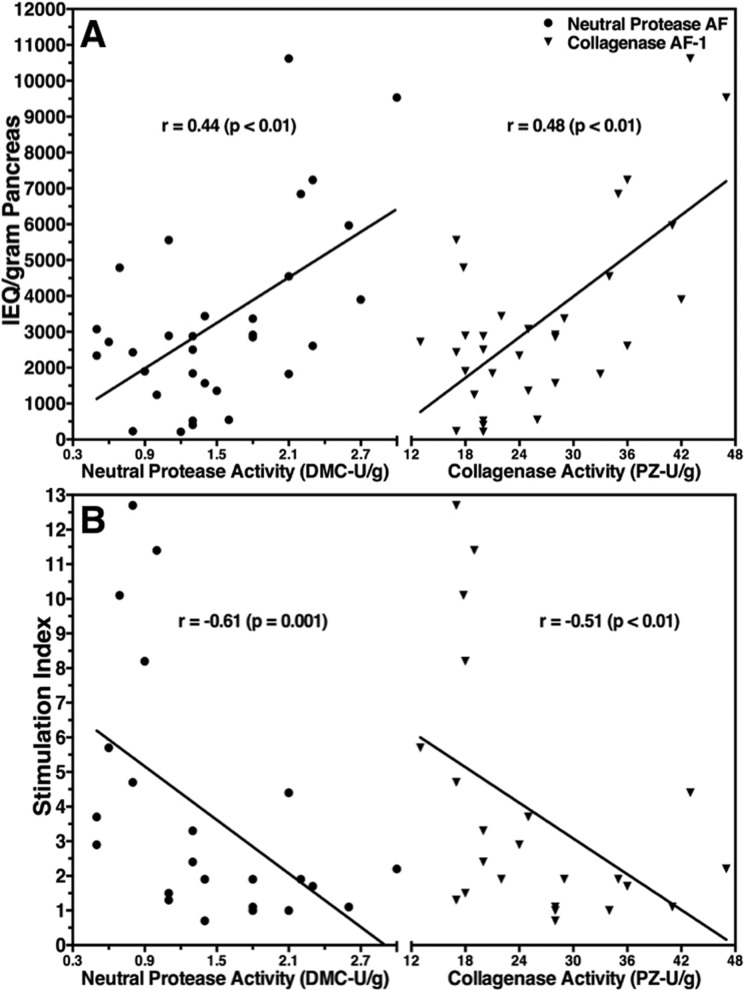
The postpurification total islet yield was 296,494 ± 33,620 IEQ per pancreas (27,826–823,125 IEQ). This corresponded to 3,274 ± 450 IEQ per gram of trimmed pancreas (218–10,624 IEQ/g) with an average purity of 55.9% ± 3.2% (21–86%). Islet yield per gram correlated positively with NP and with collagenase activity (Fig. 3A). In agreement with this observation, an inverse correlation was found between trimmed pancreas weight and islet yield per gram (r = −0.420, P < 0.05).
Fig. 3.
Effect of intraductally perfused animal-free (AF) neutral protease and collagenase AF-1 activity on purified islet yield per gram trimmed pancreas (A) and on glucose stimulation index (B). The correlation coefficient (r) was calculated using Spearman’s rank correlation.
Quality assessment performed after 2 to 4 d of culture demonstrated an average viability of 88.1% ± 1.5% (75–95%) and a glucose stimulation index of 3.7 ± 0.7 (0.7–12.7). When the stimulation index was opposed to NP or collagenase activity, an inverse correlation was observed for both enzymes (Fig. 3B). To specify the influence of the different activities, the ratio of PZ-U/g over DMC-U/g was calculated and a positive correlation between this ratio and the stimulation index was found (r = 0.535, P < 0.01). The average intracellular insulin content of isolated islets was 10.3 ± 2.2 ng/islet (1.6–30.4 ng/islet) and also correlated positively with the PZ to DMC ratio (r = 0.639, P < 0.01).
Defining isolation failure by a purified islet yield <100,000 IEQ per pancreas, 7 of the 34 isolations (20.6%) failed with respect to islet yield. Nineteen of the 34 islet preparations (55.9%) fulfilled the release criteria for clinical islet transplantation. From these successful preparations, 18 were actually transplanted into patients with type 1 diabetes, which is equivalent to a transplant rate of 52.9%. Eleven of these preparations were infused as the first transplant, 5 as the second, and 2 as the third transplant.
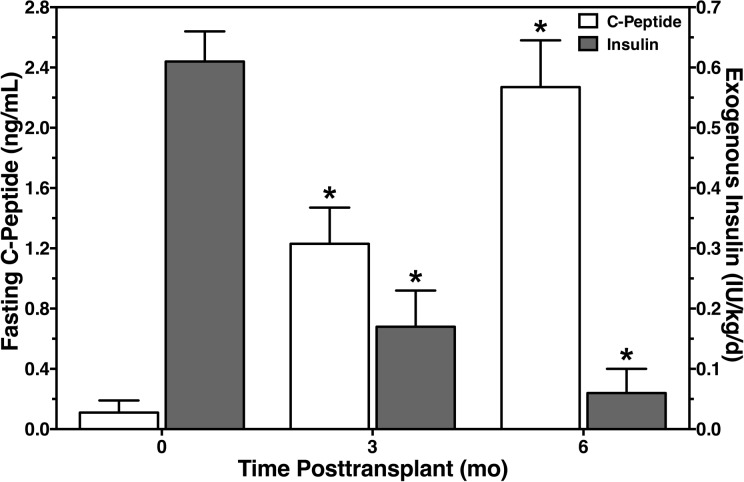
Data from 13 of the 18 transplanted preparations were made available and could be analyzed. Six of these preparations were infused into patients as the first transplant and substantially increased the fasting C-peptide level of 0.11 ± 0.08 ng/mL before transplantation when compared to 3 and 6 mo after transplantation (Fig. 4). The corresponding C-peptide to glucose ratio increased from 0.28 ± 0.25 pretransplant to 1.23 ± 0.27 and 1.89 ± 0.36 after 3 and 6 mo posttransplant (P < 0.05), respectively. At the same time, the recipients’ need for exogenous insulin simultaneously decreased from 39.2 ± 3.8 IU/d prior to transplantation to, respectively, 10.8 ± 4.1 IU/d and 4.0 ± 2.3 IU/d 3 and 6 mo posttransplant (P < 0.05). Daily insulin requirements determined per kg body weight are shown in Fig. 4.
Fig. 4.
Fasting C-peptide (white bars, left y-axis) and daily requirement of exogenous insulin per kg body weight (gray bars, right y-axis) measured in recipients with type 1 diabetes mellitus prior to and after islet allotransplantation. *P < 0.05 versus pretransplant.
Discussion
Previous production techniques for collagenase using the fermentation of bovine neuronal tissue by C. histolyticum or B. thermoproteolyticus rokko carry the risk of incorporating prions as potentially infectious vectors for CJD within the final enzyme product.6 As a consequence, new manufacturing strategies had been developed to produce mammalian tissue-free (MTF) collagenase blends.22,23 Indeed, the risk for the transmission of CJD into the human population by transplantation of collagenase-isolated islets had been regarded as low,24 but it was recently shown that prions can be transmitted between a variety of widely disparate species25 which are partially considered as clinically silent carriers of replicating prions.26 Taking this incalculable risk into account, an advanced manufacturing process was developed to use plant-based material for the production of AF GMP collagenase and NP.
Different variables such as pH, temperature, selection, and concentration of nutrients have a significant effect on the amount of collagenase produced by microbial organisms.27,28 Nevertheless, it is unknown so far whether the selection of different categories of nutrients has an effect on the quality and specific activity of collagenolytic enzymes produced by different bacteria for enzymatic islet isolation. Our study demonstrates that a vegan diet for C. histolyticum has no detrimental effects on the specific activity and efficiency of collagenase or NP. A preliminary study by Parnaud et al. demonstrated a similar efficiency for collagenase AF-1 to release islets from the human pancreas compared with collagenase NB-1 premium grade.29 The isolation success and transplantation rates obtained using collagenase AF-1 indicate a high efficiency when compared with previously published data collected from MTF collagenase-digested pancreases.22,23 We are aware of the fact that the thresholds for success and failure are arbitrarily chosen figures that have not been defined by an international consent. When isolation outcome is dichotomized,15,30 it becomes evident that a gray zone exists between the cutoff for success or failure. Islet preparations from this gray zone may nevertheless fulfill the worldwide established product release criteria for clinical islet transplantation particularly when the body weight of the potential recipient is relatively low or when the preparation is used as top-up transplant.
The present study demonstrates a transplant rate of more than 50% despite the large variability of perfused collagenase and NP activities. This observation also suggests that human islets can be successfully isolated within a wide range of varying isolation protocols.11,31,32 An explanation for this finding might be provided by previous experiments revealing that approximately only 35% of the total amount of collagenase activity perfused into the pancreas is bound to pancreatic tissue.33,34 Conversely, this means that intraductally perfused enzymes are usually administered in excessive activities are usually administered in excess. The most rational and effective method for optimizing the enzyme concentration without the risk of under- or overdosing seems to be conversion of the worldwide established vial-based enzyme administration to adjustment of collagenase and protease activity on a per gram basis.35
On the other hand, our correlation analysis showed the ambivalent effect of enzymes on isolation outcome. While higher enzyme concentrations seem to favor a higher yield of isolated islets, lower enzyme activities seem to be beneficial for islet functional integrity. To specify the detrimental effect of the different enzymes on islet integrity, we calculated the ratio between collagenase and NP activity. As this ratio correlated positively with the stimulation index and the insulin content, we assume that a careful and balanced reduction of NP activity benefit islet function and viability which is in accordance with previous studies.36–38
One of the disadvantages of our study is that only a marginal number of the pancreases processed were from donors younger than 30 years of age. This lack of younger donors is observed in nearly all islet isolation centers worldwide and reflects the allocation system differentially selecting younger and leaner donors for solid pancreas transplantation, whereas older and obese donors are allocated for islet transplantation.39
In summary, this study investigates the efficiency of SERVA Collagenase AF-1 and NP AF produced from C. histolyticum by fermentation of plant-based material. This newly established production process excludes the risk of incorporating prions or other animal-derived infectious agents in the final enzyme products. The efficiency of the enzymes is demonstrated by a transplant rate of more than 50% that was reached within a broad range of collagenase and NP activities.
Acknowledgments
The authors wish to thank the islet isolation teams of the particular centers for their invaluable contribution to this study.
Author’s Note: Julia Saphörster and Manfred Kurfürst are employed by SERVA Electrophoresis GmbH, Uetersen, Germany.
Author Contribution: Daniel Brandhorst and Géraldine Parnaud contributed equally to this study.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: Pancreases were retrieved with appropriate consent and ethical approval from 34 human multiorgan donors utilizing cold perfusion with Institute Georges Lopez-1(IGL-1) solution.
Statement of Informed Consent: Appropriate consent was obtained from 34 human multiorgan donors.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by grants from the Juvenile Diabetes Foundation International (31-2008-617), the Swedish Medical Research Council (K2015-54X-12219-19-4), the Diabetes Wellness Foundation, the Oxford Biomedical Research Centre, and the Swiss National Science Foundation (310030_149798/1).
References
- 1. Barton FB, Rickels MR, Alejandro R, Hering BJ, Wease S, Naziruddin B, Oberholzer J, Odorico JS, Garfinkel MR, Levy M, et al. Improvement in outcomes of clinical islet transplantation: 1999-2010. Diabetes Care. 2012;35(7):1436–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rickels MR, Liu C, Shlansky-Goldberg RD, Soleimanpour SA, Vivek K, Kamoun M, Min Z, Markmann E, Palangian M, Dalton-Bakes C, et al. Improvement in beta-cell secretory capacity after human islet transplantation according to the CIT07 protocol. Diabetes. 2013;62(8):2890–2897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rickels MR, Fuller C, Dalton-Bakes C, Markmann E, Palanjian M, Cullison K, Tiao J, Kapoor S, Liu C, Naji A, et al. Restoration of glucose counterregulation by islet transplantation in long-standing type 1 diabetes. Diabetes. 2015;64(5):1713–1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McCarthy RC, Breite AG, Green ML, Dwulet FE. Tissue dissociation enzymes for isolating human islets for transplantation: factors to consider in setting enzyme acceptance criteria. Transplantation. 2011;91(2):137–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lee J, Hyeon JW, Kim SY, Hwang KJ, Ju YR, Ryou C. Review: laboratory diagnosis and surveillance of Creutzfeldt-Jakob disease. J Med Virol. 2015;87(1):175–186. [DOI] [PubMed] [Google Scholar]
- 6. Geschwind MD. Prion diseases. Continuum (Minneap Minn). 2015;21(6 Neuroinfectious Disease):1612–1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Avgoustiniatos ES, Scott WE, Suszynski TM, Schuurman HJ, Nelson RA, Rozak PR, Mueller KR, Balamurugan AN, Ansite JD, Fraga DW, et al. Supplements in human islet culture: human serum albumin is inferior to fetal bovine serum. Cell Transplantation. 2012;21(12):2805–2814. [DOI] [PubMed] [Google Scholar]
- 8. Malaga-Trillo E, Salta E, Figueras A, Panagiotidis C, Sklaviadis T. Fish models in prion biology: underwater issues. Biochim Biophys Acta. 2011;1812(3):402–414. [DOI] [PubMed] [Google Scholar]
- 9. Salta E, Kanata E, Ouzounis CA, Gilch S, Schatzl H, Sklaviadis T. Assessing proteinase K resistance of fish prion proteins in a scrapie-infected mouse neuroblastoma cell line. Viruses. 2014;6(11):4398–4421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Niclauss N, Wojtusciszyn A, Morel P, Demuylder-Mischler S, Brault C, Parnaud G, Ris F, Bosco D, Badet L, Benhamou PY, et al. Comparative impact on islet isolation and transplant outcome of the preservation solutions Institut Georges Lopez-1, University of Wisconsin, and Celsior. Transplantation. 2012;93(7):703–708. [DOI] [PubMed] [Google Scholar]
- 11. Cross SE, Hughes SJ, Clark A, Gray DW, Johnson PR. Collagenase does not persist in human islets following isolation. Cell Transplant. 2012;21(11):2531–2535. [DOI] [PubMed] [Google Scholar]
- 12. Ståhle M, Foss A, Gustafsson B, Lempinen M, Lundgren T, Rafael E, Tufveson G, Korsgren O, Friberg A. Clostripain, the missing link in the enzyme blend for efficient human islet isolation. Transplant Direct. 2015;1(5):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ricordi C, Gray DW, Hering BJ, Kaufman DB, Warnock GL, Kneteman NM, Lake SP, London NJ, Socci C, Alejandro R, et al. Islet isolation assessment in man and large animals. Acta Diabetol Lat. 1990;27(3):185–195. [DOI] [PubMed] [Google Scholar]
- 14. Lakey JR, Warnock GL, Rajotte RV, Suarez-Alamazor ME, Ao Z, Shapiro AM, Kneteman NM. Variables in organ donors that affect the recovery of human islets of Langerhans. Transplantation. 1996;61(7):1047–1053. [DOI] [PubMed] [Google Scholar]
- 15. Hanley SC, Paraskevas S, Rosenberg L. Donor and isolation variables predicting human islet isolation success. Transplantation. 2008;85(7):950–955. [DOI] [PubMed] [Google Scholar]
- 16. Zeng Y, Torre MA, Karrison T, Thistlethwaite JR. The correlation between donor characteristics and the success of human islet isolation. Transplantation. 1994;57(6):954–958. [DOI] [PubMed] [Google Scholar]
- 17. Nano R, Clissi B, Melzi R, Calori G, Maffi P, Antonioli B, Marzorati S, Aldrighetti L, Freschi M, Grochowiecki T, et al. Islet isolation for allotransplantation: variables associated with successful islet yield and graft function. Diabetologia. 2005;48(5):906–912. [DOI] [PubMed] [Google Scholar]
- 18. Ricordi C, Strom TB. Clinical islet transplantation: advances and immunological challenges. Nat Rev Immunol. 2004;4(4):259–268. [DOI] [PubMed] [Google Scholar]
- 19. Ryan EA, Paty BW, Senior PA, Lakey JR, Bigam D, Shapiro AM. Beta-score: an assessment of beta-cell function after islet transplantation. Diabetes Care. 2005;28(2):343–347. [DOI] [PubMed] [Google Scholar]
- 20. Bellin MD, Kandaswamy R, Parkey J, Zhang HJ, Liu B, Ihm SH, Ansite JD, Witson J, Bansal-Pakala P, Balamurugan AN, et al. Prolonged insulin independence after islet allotransplants in recipients with type 1 diabetes. Am J Transplant. 2008;8(11):2463–2470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Faradji RN, Monroy K, Messinger S, Pileggi A, Froud T, Baidal DA, Cure PE, Ricordi C, Luzi L, Alejandro R. Simple measures to monitor beta-cell mass and assess islet graft dysfunction. Am J Transplant. 2007;7(2):303–308. [DOI] [PubMed] [Google Scholar]
- 22. Caballero-Corbalan J, Brandhorst H, Asif S, Korsgren O, Engelse M, de Koning E, Pattou F, Kerr-Conte J, Brandhorst D. Mammalian tissue-free liberase: a new GMP-graded enzyme blend for human islet isolation. Transplantation. 2010;90(3):332–333. [DOI] [PubMed] [Google Scholar]
- 23. O’Gorman D, Kin T, Imes S, Pawlick R, Senior P, Shapiro AM. Comparison of human islet isolation outcomes using a new mammalian tissue-free enzyme versus collagenase NB-1. Transplantation. 2010;90(3):255–259. [DOI] [PubMed] [Google Scholar]
- 24. Elsaadany S, Tyshenko MG, Oraby T, Malcolm AJ, Senior P, Shapiro AM, Catford A, Salem T, Wu J, Krewski D, et al. The risk to human islet cell transplant recipients of acquiring variant Creutzfeldt-Jakob disease: a provisional quantitative risk assessment. Transplantation. 2011;92(1):e2–e4. [DOI] [PubMed] [Google Scholar]
- 25. Hedman C, Bolea R, Marin B, Cobriere F, Filali H, Vazquez F, Pitarch JL, Vargas A, Acin C, Moreno B, et al. Transmission of sheep-bovine spongiform encephalopathy to pigs. Vet Res. 2016;47(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hammarstrom P, Nystrom S. Porcine prion protein amyloid. Prion. 2015;9(4):266–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lima CA, Marques DA, Barros Neto B, Lima Filho JL, Carneiro-da-Cunha MG, Porto AL. Fermentation medium for collagenase production by Penicillium aurantiogriseum URM4622. Biotechnol Prog. 2011;27(5):1470–1477. [DOI] [PubMed] [Google Scholar]
- 28. Suphatharaprateep W, Cheirsilp B, Jongjareonrak A. Production and properties of two collagenases from bacteria and their application for collagen extraction. N Biotechnol. 2011;28(6):649–655. [DOI] [PubMed] [Google Scholar]
- 29. Parnaud G, Lavallard V, Meier R, Bedat B, Bosco D, Berney T. Human islet isolation using animal-free collagenase and neutral protease. 2013. https://tech4pco.com/ipita2013/mobis/lecture/566.
- 30. Kaddis JS, Danobeitia JS, Niland JC, Stiller T, Fernandez LA. Multicenter analysis of novel and established variables associated with successful human islet isolation outcomes. Am J Transplant. 2010;10(3):646–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Szot GL, Lee MR, Tavakol MM, Lang J, Dekovic F, Kerlan RK, Stock PG, Posselt AM. Successful clinical islet isolation using a GMP-manufactured collagenase and neutral protease. Transplantation. 2009;88(6):753–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Balamurugan AN, Breite AG, Anazawa T, Loganathan G, Wilhelm JJ, Papas KK, Dwulet FE, McCarthy RC, Hering BJ. Successful human islet isolation and transplantation indicating the importance of class 1 collagenase and collagen degradation activity assay. Transplantation. 2010;89(8):954–961. [DOI] [PubMed] [Google Scholar]
- 33. Friberg AS, Korsgren O, Hellgren M. A vast amount of enzyme activity fails to be absorbed within the human pancreas: implications for cost-effective islet isolation procedures. Transplantation. 2013;95(6):e36–e38. [DOI] [PubMed] [Google Scholar]
- 34. Kin T, O’Gorman D, Zhai X, Pawlick R, Imes S, Senior P, Shapiro AM. Nonsimultaneous administration of pancreas dissociation enzymes during islet isolation. Transplantation. 2009;87(11):1700–1705. [DOI] [PubMed] [Google Scholar]
- 35. Brandhorst H, Kurfurst M, Johnson PR, Korsgren O, Brandhorst D. Comparison of neutral proteases and collagenase class I as essential enzymes for human islet isolation. Transplant Direct. 2016;2(1):e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wolters GH, Vos-Scheperkeuter GH, van Deijnen JH, van Schilfgaarde R. An analysis of the role of collagenase and protease in the enzymatic dissociation of the rat pancreas for islet isolation. Diabetologia. 1992;35(8):735–742. [DOI] [PubMed] [Google Scholar]
- 37. Bucher P, Bosco D, Mathe Z, Matthey-Doret D, Andres A, Kurfuerst M, Ramsch-Gunther N, Buhler L, Morel P, Berney T. Optimization of neutral protease to collagenase activity ratio for islet of Langerhans isolation. Transplant Proc. 2004;36(4):1145–1146. [DOI] [PubMed] [Google Scholar]
- 38. Brandhorst H, Brendel MD, Eckhard M, Bretzel RG, Brandhorst D. Influence of neutral protease activity on human islet isolation outcome. Transplant Proc. 2005;37(1):241–242. [DOI] [PubMed] [Google Scholar]
- 39. Berney T, Johnson PR. Donor pancreata: evolving approaches to organ allocation for whole pancreas versus islet transplantation. Transplantation. 2010;90(3):238–243. [DOI] [PubMed] [Google Scholar]