Abstract
Background:
The initial 6 weeks after surgery has been identified as an area for improvement in patient care. During this period, the persistence of symptoms that go unchecked can lead to unscheduled emergency room and clinic visits, calls to surgeons’ offices, and readmissions.
Purpose:
To analyze postoperative data from a previous study examining postoperative outcomes in 2 patient populations following breast reconstruction and anterior cruciate ligament (ACL) reconstruction with use of a patient-centered mobile application. Here, the authors establish whether this method of follow-up can provide useful insight specific to the orthopaedic patient population, and they determine whether the mobile platform has the potential to modify their postoperative treatment. In addition, the authors examine its utility for orthopaedic physicians and patients.
Study Design:
Case series; Level of evidence, 4.
Methods:
Eligible patients undergoing ACL reconstruction from 2 surgeons were consecutively recruited to use a mobile smartphone application that allowed physicians to monitor their recovery at home. Data from 32 patients were collected via the application and analyzed to evaluate recovery trends during the first 6 postoperative weeks. Following completion of the study, patients and physicians were interviewed on their experience.
Results:
Data collected from each question in the mobile application provided insightful trends on daily real-time indicators of postoperative recovery. The application identified 1 patient who required in-person reassessment to rule out a possible infection, following surgeon review of an uploaded image. It was estimated that the majority of patients could have avoided follow-up at 2 and 6 weeks, owing to the application’s efficacy. Participants described their satisfaction with the device as excellent (43%), good (40%), fair (10%), and poor (7%), and 94% (n = 30) of patients reported that they would respond to questions using a similar application in the future. Both physicians rated their experience as positive and identified useful traits in the web portal.
Conclusion:
This system can accurately assess patient recovery; it has the potential to change how postoperative orthopaedic patients are followed, and it is well received by patients and physicians. Recognition of the study’s limitations and employment of user feedback to improve the current application are essential before a formal randomized controlled trial is conducted.
Keywords: ACL reconstruction, smartphone, app, follow-up, mobile
Mobile communication has had a dramatic impact on daily life, with an estimated 3 billion people using mobile devices worldwide.4 In this technological age, the development of smartphones and mobile tablets has enhanced our ability to communicate, learn, and organize information. These innovations have created opportunities to incorporate technology into medical practice.6 Web-based questionnaires, automatic appointment and medication reminders, as well as patient learning tools have already been adopted in many areas of medicine.3,8,9 Web-based electronic entry of subjective follow-up data by patients is being used to determine the efficacy of certain therapeutic interventions.1
The application of emerging smartphone technology to surgical follow-up has been studied in several areas of ambulatory surgery. In a study examining surgical outpatient efficiency, mobile devices sent surveillance text messages to patients to determine the need to schedule an outpatient clinic appointment.4 Similarly, Martinez-Ramos and Lopez10 utilized mobile phone images sent from patients via email to assess local wound complications after ambulatory surgery and to avoid unnecessary visits. Wood et al15 applied these advances in technology to orthopaedic surgery and combined the use of a picture archiving system and a validated web-based subjective patient questionnaire to create an electronic follow-up clinic for arthroplasty patients. Semple et al14 recently showed evidence that using smartphone technology monitoring for patients undergoing postoperative breast reconstruction and anterior cruciate ligament (ACL) reconstruction is both feasible and acceptable to patients and surgeons.
In the setting of postoperative ACL reconstruction, an alternative to standard clinic-based follow-up may be beneficial for patients and surgeons. The utilization of web-based follow-up allows surgeons to monitor a patient’s subjective quality of recovery, including symptoms of pain, feelings of anxiety, and limitations in activities of daily living. This tool has the potential to enhance quality of care by providing daily updates about the patient’s physical impairment and mental health.13 Furthermore, while ACL reconstruction is considered a safe procedure with low complication rates, some complications can occur. Infection is rare and can occur in 0.3% to 1.7% of patients, with cases ranging from superficial infection of the surgical site to septic arthritis of the knee.7 Uploading pictures from a mobile tablet or smartphone in addition to clinical questions will allow for assessment and potential detection of early postoperative complications. This will also permit surgeons to intervene as indicated, as they would in a conventional follow-up setting. In addition, uploading photos for subsequent reassurance from physicians can resolve patient concerns and prevent unnecessary follow-up appointments and emergency department visits.
The purpose of our study was to analyze previously obtained data14 specific to orthopaedic patients to (1) document postoperative symptoms following ACL reconstruction, (2) establish if the use of a smartphone application (or “app”) has the potential to affect postoperative management specific to an orthopaedic surgical practice by safely eliminating conventional follow-up appointments, and (3) determine the acceptance of a mobile follow-up system for orthopaedic physicians and patients. We hypothesized that we will be able to accurately and efficiently monitor trends in patient recovery, that smartphone technology for monitoring will be well received by patients and physicians, and that this pilot study will provide an impetus for future incorporation of mobile monitoring into practice.
Methods
Device and Application
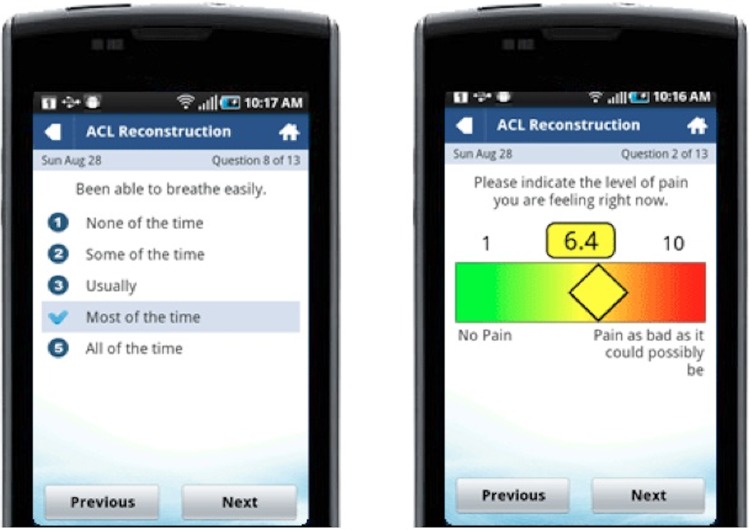
A study was initially carried out at our institution to determine the feasibility of mobile app technology to monitor the postoperative quality of at-home recovery for 2 patient populations (ACL reconstruction and breast reconstruction). This article represents the orthopaedic-specific results of this pilot study. A panel that included 2 sports medicine fellowship–trained orthopaedic surgeons (L.M., J.T.) was created to determine potential questions specific to patients undergoing postoperative ACL reconstruction to evaluate recovery. The mobile app recovery indicators included a visual analog scale (VAS) for pain and Likert questions from the Quality of Recovery–9 (QoR-9) questionnaire, a version of the Quality of Recovery–40 questionnaire, which has been validated to assess the quality of life of patients after surgery.12 Using a scale of this magnitude (ie, 40 items) did not seem feasible for daily self-assessments given its length, so we decided to utilize the QoR-9 in addition to limb-specific questions that were of interest to our 2 surgeons for the purpose of daily monitoring. This yielded 16 pilot measures to be collected daily via the application, as seen in Table 1. Figure 1 demonstrates the app’s intuitive interactive touch inputs. In addition, pictures of wound sites could be taken with the device and uploaded daily to the mobile app portal (QoC Health) (Figure 2). The device provided patients with access to educational information on their procedure and recovery, as well as key health team contacts. Responses and images could be accessed by surgeons through the QoC Health portal. Figure 3 demonstrates how the application can graph trends for each recovery indicator.
TABLE 1.
Pilot Indicators for Recovery After Anterior Cruciate Ligament Reconstructiona
| QoR-9 | Been free from nausea, vomiting, retching? |
| Been free from experiencing severe pain or constant moderate pain? | |
| Been able to breathe easily? | |
| Been free from headache, backache, or muscle pains? | |
| Been able to pass urine? | |
| Been able to look after personal toilet and hygiene unassisted? | |
| Been able to understand instructions and advice (not being confused)? | |
| Had support from others? | |
| Had a general sense of well-being? | |
| VAS | Please indicate the level of pain you are experiencing right now |
| Surgeon specific | How difficult is it to stand on your leg? |
| How difficult is it to walk on your leg? | |
| How difficult is it to go up and down stairs? | |
| How difficult is it to perform activities of daily living? | |
| How anxious (worried, nervous) do you feel? |
aQoR-9, Quality of Recovery–9; VAS, visual analog scale.
Figure 1.
Touchscreen technology for patients to respond to daily questions monitoring their recovery.
Figure 2.

Uploaded picture of wound site, accessible on the QoC Health provider portal.
Figure 3.
An example of a patient’s graph trending the recovery indicator “Been free from nausea, dry-retching or vomiting,” accessible via the QoC Health provider portal.
Institutional Approval and Confidentiality
Research ethics board approval for the pilot study was granted in July 2011. As there was no change in the current medical standard of care, there was no greater risk to patients by participating in the study. However, there is always risk of loss of confidentiality when data are collected and stored for patients. No patient was discharged from the hospital unless he or she met the usual discharge criteria applied to all patients and all standard practices of postsurgical care were followed.
All hard copies of the data (ie, surveys and interview notes) were stored in locked filing cabinets in the investigator’s office at our institution, with access restricted to ensure patient confidentiality. All patients were coded so that identifiers were absent from survey and interview data. Data sheets containing patient identifiers and identification numbers were stored separately from data sheets containing only patient identification numbers. No identifiers were or will be included on any hard copy data sheets that link with health information (ie, only identification numbers are used), and password-protected databases were used.
Health Canada was consulted for whether this monitoring concept on a smartphone would be considered a classification of a “medical device.” Because it is not diagnostic and is essentially “stored forward” data, it is not considered a “device.” The Canadian Medical Protective Agency was also consulted with regard to medical legal liability and the participating surgeons. The agency’s only stipulation was that of privacy standards and security of patient data.
Patient data collected via the mobile app is double encrypted on the server and the phone. Designed from the ground up to ensure security and privacy, the application conforms to leading health care audit and interoperability standards, including the Personal Health Information Act, Health Level 7, Information Technology Infrastructure Library, and Statement on Auditing Standards No. 70. Multiple layers of encryption—including resting-state Advanced Encryption Standard encryption, in-transmission content encryption based on unique per-patient public/private key pairs, and in-transmission Transport Layer Security/Secure Sockets Layer protocol encryption—were applied to maintain the highest level of patient confidentiality possible. The study also utilized modern infrastructure design leveraging distributed infrastructure as a service, as well as cloud computing services for seamless accessibility, redundancy, and scalability.9
Patients and Consent
A study coordinator identified 40 prospective patients undergoing ACL reconstruction in the orthopaedic clinics of 2 surgeons at our institution. Of these patients, 32 (80%) consented for our study. Patients between the ages of 18 and 75 years, nonsmokers, English speaking, <100 days postsurgery, and with sound cognitive functioning were included. Patients with chronic pain, psychiatric disturbance, regular use of narcotic medication for pain, or allergies to morphine-like medication or local anesthetics were excluded. Physicians provided general information on the study and asked for consent to participate. The study coordinator tracked declines and acceptances to consent.
Thirty-two consenting patients attended an education session led by the study coordinator to familiarize themselves with the application. Patients were also guided through their first time using the mobile app and were loaned a device with the preprogrammed app to bring home. Patients were instructed to respond daily for the first 2 weeks and then weekly until 6 weeks postoperatively. Both surgeons were available to answer any patient questions or concerns via telephone/email or in person. The study coordinator saw all patients at their first follow-up visit 2 weeks after the date of surgery, where study process and procedure were reviewed. Their second follow-up visit occurred 6 weeks after the surgery date.
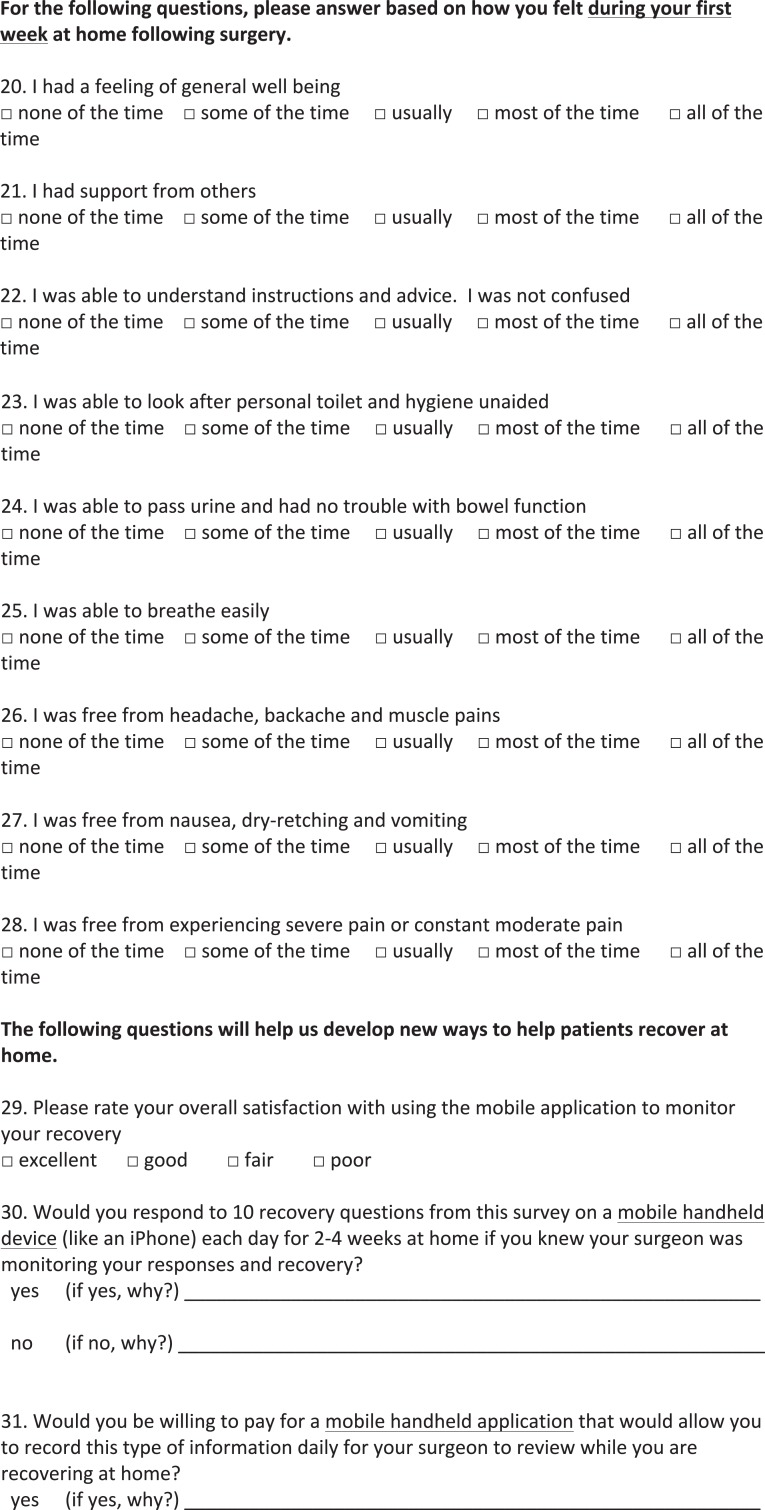
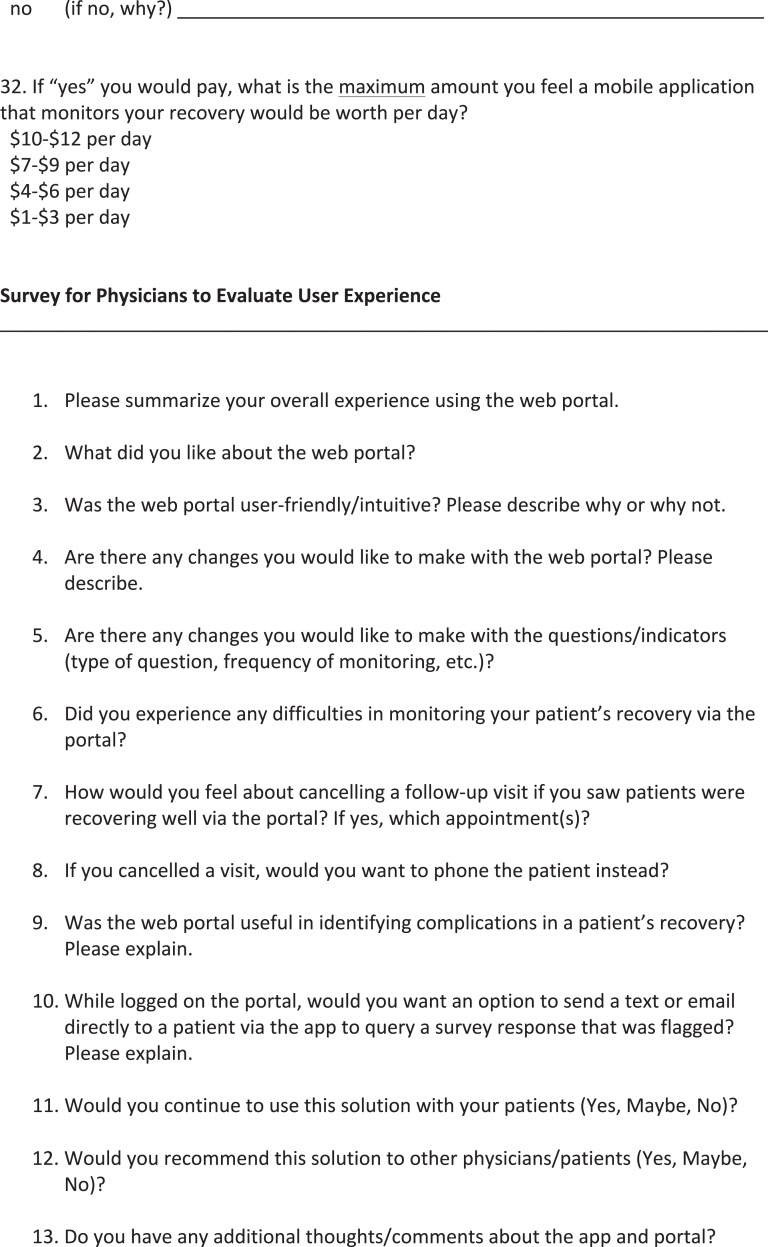
Follow-up Surveys
The study group was given a survey after completing 6 weeks of mobile app use. This survey, seen in the Appendix, asked questions about the patients’ recovery experience at home, including questions concerning anxiety and satisfaction with care, as well as the QoR-9 questions. Furthermore, the survey was used to determine their satisfaction with the device and their desire for future use and to establish the perceived value of the application. Physicians were given a 13-question survey to assess their experience and provide feedback for the app developers. This survey can also be found in the Appendix.
Statistical Analysis
Following completion of our institution’s larger feasibility study, descriptive statistics were used to summarize demographic and clinical variables of the orthopaedic population. Data collected via the application were utilized to show trends and frequency distributions of questions related to patients’ ACL reconstruction recovery during the 6-week postoperative period.
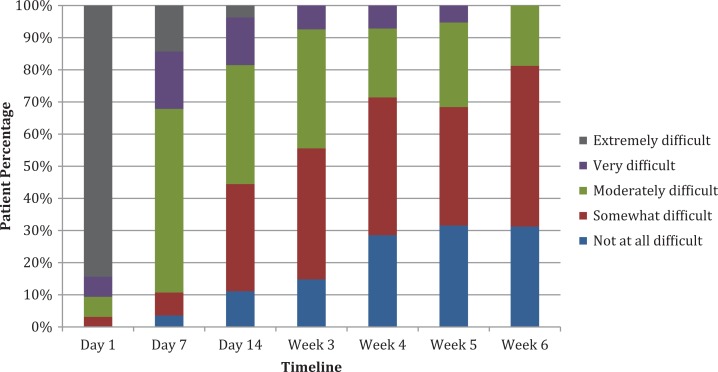
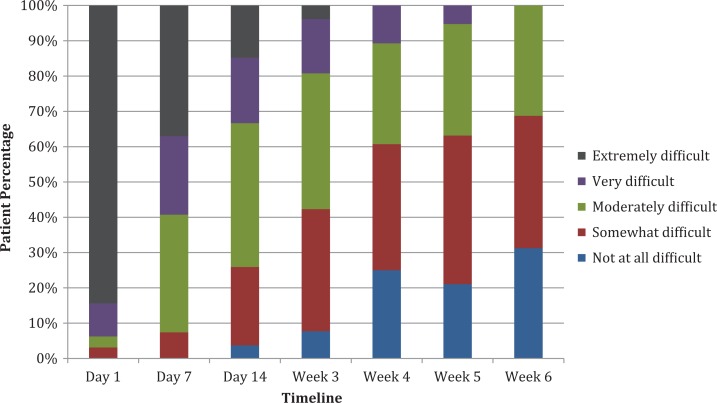
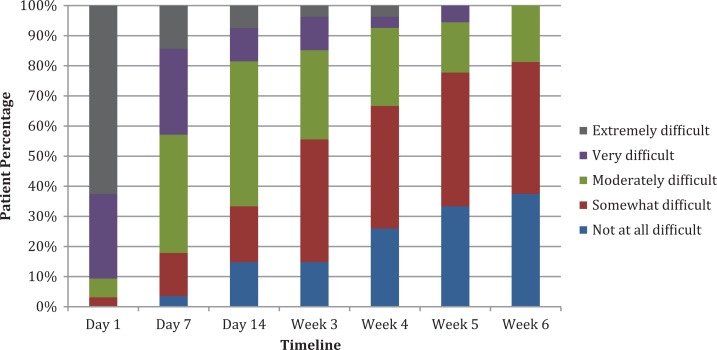
Results
Table 2 presents the patient demographics of the study group, and Table 3 provides the surgical procedures undertaken. Figures 4 to 7 provide examples of the frequency distributions of responses to 4 of the daily questions collected by the app that monitored the patient recovery experience. For postoperative day 14, we found that 11% had no difficulty standing on the operated leg, while only 4% had no difficulty walking. This improved to 31% at 6 weeks for both questions. Ability to perform daily activities of living followed a similar distribution, with 15% of respondents having no difficulty at 2 weeks, increasing to 38% at 6 weeks. Interestingly, our patients’ level of anxiety seemed to increase between weeks 2 and 6, peaking in week 4, when 54% of patients reported feeling anxious about their recovery.
TABLE 2.
Patient Demographics
| Sample, No. | 32 |
| Male | 18 |
| Female | 14 |
| Age, y | |
| Median | 28 |
| Mean | 33 |
| Range | 21-55 |
TABLE 3.
Study Group Proceduresa
| ACL Reconstruction | No. of Patients |
|---|---|
| With hamstring autograft | 28 |
| Revision with tibialis posterior allograft | 2 |
| With bone–patellar tendon–bone autograft | 1 |
| With hamstring autograft + PLC reconstruction with Achilles allograft | 1 |
aACL, anterior cruciate ligament; PLC, posterolateral corner.
Figure 4.
Frequency distributions for the question “How difficult is it to stand on your leg?”
Figure 5.
Frequency distributions for the question “How difficult is it to walk on your leg?”
Figure 6.
Frequency distributions to the question “How difficult is it to perform activities of daily living?”
Figure 7.
Frequency distributions to the question “How anxious (worried, nervous) do you feel?”
Aggregate data were also collected for the remaining 12 daily questions posed by the app. As a result, we found that all patients still had some degree of difficulty going up and down stairs at 2 weeks and that only 22% responded that they had no difficulty with this task at 6 weeks postoperatively. Postoperative nausea and vomiting resolved for >92% of patients by postoperative day 14 and were not an issue by week 3. Urinary and bowel symptoms were also reported, with 78% of patients achieving normal bowel function at 2 weeks postoperatively and nearly all urinary retention resolving (96%) within the first week.
Figure 8 shows the trend in the level of pain experienced by the pilot group in the first 30 days postoperatively. Patients responded on a continuous touchscreen scale of 1 to 10 on the mobile device, where 1 indicated no pain and 10 indicated pain as bad as it could possibly be. Patients reported a mean score of 4.2 (SD = 2.20) on day 1, 4.1 (SD = 2.48) on day 7, 2.6 (SD = 1.71) on day 14, and 2.7 (SD = 1.70) on day 30.
Figure 8.
Mean daily visual analog scale scores in postoperative period.
In this group of 32 participants, the app identified 1 (3%) who needed to return for an appointment to rule out a possible infection following review of an uploaded image. Antibiotics were initiated, which resolved a superficial wound infection and may have prevented a single readmission. No other complications, such as stiffness, reinjury, or deep vein thrombosis, occurred in the study group. Aside from this 1 patient, no other patients required any changes to their postoperative treatment.
Of the 32 patients, 31 (97%) completed the survey of their study experience. They reported their overall satisfaction with the mobile device as excellent (43%), good (40%), fair (10%), and poor (7%). When asked if they would respond to similar questions on a mobile device in the future, knowing that the surgeon was monitoring recovery, 30 (94%) responded yes, and 2 (6%) responded no. Comments from patients who responded yes included “It would create a sensation of being in control of my progress,” “Easy and can be done anytime,” and “It would provide good potential feedback for both parties.” The 1 no response was due to disliking mobile devices and lacking a data plan.
Of the study patients, 47% stated that they would be willing to pay for an app like this in the future. Patients who responded as being unwilling to pay for the app described either not being that worried about their recovery outside the hospital or feeling that such a health care service should be provided free of cost. Some patients did report that daily responses seemed to be excessive, as it became an annoyance to respond to the same questions with the same answers every day. The 2 surgeons involved in the study completed a survey to assess their experience with this mode of follow-up. Both rated their experience as positive and identified portability, ease of use, and user-friendliness as the most positive traits of the mobile app. The physicians both concluded that they would continue to use this solution and would recommend it to other physicians and patients.
Discussion
The data collected from each question in the mobile app provided insightful trends on daily indicators of postoperative ACL reconstruction recovery, such as pain levels, feelings of anxiety, and the limitations of the affected leg. This gave surgeons important recovery information not often discussed during routine follow-up visits and at time points to which they would not otherwise have access. The utilization of this method provided surgeons with an easy, portable way to monitor subjective quality of recovery on a real-time basis. Continued collection of aggregate data on this patient population will provide the care team with a method of identifying patients who fall outside the normal variances of postoperative recovery. This will also allow surgeons to plan follow-up visits on a more individualized basis, if needed at all. Recorded data of patients’ abilities to stand, walk, use stairs, and perform activities of daily living are useful not only for orthopaedic care providers but for home care staff and physical therapists to set goals and manage expectations.
This application has the potential to enhance future patient-physician communication and improve education about what to expect postoperatively. For example, our study results show that >70% of our patients still had varying degrees of difficulty standing on the affected leg at 4 weeks postoperatively. Interestingly, >50% of patients also had some degree of anxiety about their recovery at this point. Comments from the postpilot survey about reasons for their anxiety included “uncertainty,” “fear of unknown,” and “not sure if I should be recovering faster.” A preoperative patient who is well educated about his or her upcoming recovery experience, including normal variances in recovery milestones, could suffer less postoperative anxiety. In a study of preoperative education for patients undergoing hip and knee replacement, McDonald et al11 found that this may be true if the education is tailored toward patients who are in need of more social support, those with preoperative anxiety, and those with preexisting mobility issues.
At the conclusion of the study, both surgeons estimated that the majority of patients could have avoided their follow-up appointments at 2 and 6 weeks owing to the efficacy of the application. The future utilization of this method of outpatient follow-up could also save time and money for patients, physicians, and hospitals. In Ontario, an estimated 3000 ACL reconstructions were performed in 2008, with numbers steadily increasing each year since 2001.5 In 1 study examining 13,571 patients undergoing ACL reconstruction, rates of 90-day deep vein thrombosis and pulmonary thromboembolism were 0.29% and 0.20%, respectively, while 0.94% had a wound complication recorded and 1.34% were readmitted to an orthopaedic ward within 30 days.7 The removal of postoperative appointments at 2 and 6 weeks for approximately 3000 patients could result in 5834 fewer outpatient follow-up visits per year in Ontario, after adjustment for the aforementioned possible complication rates.
With this system, physicians can identify outliers in recovery milestones and flag answers that may indicate complications and poor recovery. It may be useful to limit clinic appointments to this population to investigate the reasons for their poor responses. The reduction in the number of visits could minimize waiting times and create an opportunity to increase availability for new referrals within Canada’s socialized health care system. In addition, decreasing the number of follow-up appointments will be cost-effective for patients by reducing travel costs and time lost from work.
Two studies on the follow-up of surgical outpatients also described the success of web-based systems to avoid unnecessary follow-up visits.4,13 Armstrong et al2 modeled cost-effectiveness scenarios with mobile app home monitoring, taking into account the total of the health care system, patient, and external costs. The breast reconstruction group was given mobile devices similar to the ACL reconstruction group. For patients undergoing breast reconstruction, the researchers demonstrated that a mean Can$136 was spent in the mobile app follow-up care stream, whereas Can$381 was spent in the in-person follow-up care stream in the first postoperative month. We acknowledge the need for a formal cost analysis for patients undergoing ACL reconstruction, which will evaluate the fees and savings incurred by developing and utilizing an electronic follow-up clinic for this population of patients undergoing ambulatory surgery.
Patient feedback on the app was very positive, as 94% of participants reported their desire to use it as a mode of follow-up in the future. Our results on patient satisfaction with the application mirror a similar orthopaedic study conducted by Wood et al,15 where 95% of patients reported that a web-based e-clinic was more convenient than a standard clinic and was the preferred method of future follow-up. Patients in a study by Martinez-Ramos and Lopez10 also described the usefulness of a telemedicine system that sent daily postoperative pictures. Procedures included operations for inguinal or umbilical hernias, hallux valgus, carpal tunnel syndrome, Dupuytren disease, varicose veins, hydrocele, and varicocele. Physician and patient satisfaction, desire for future use, as well as constructive feedback should provide an impetus to improve the app and continue to study its relevance to postoperative orthopaedic follow-up.
We recognize limitations in our study. Equitable access to this web-based service is not universal, as not everyone can afford to pay for a smartphone/tablet or for a mobile app for 1 of these devices. In this study, participants were loaned a device with the preprogrammed application. Furthermore, both physicians recognized the need to incorporate range of motion data into the app, as the addition of this information would represent a more accurate depiction of patient recovery. Also, while orthopaedic physician feedback was positive, the sample size was small (n = 2). It is possible that the addition of surgeons to the study will result in different feelings about the mobile app and web portal, as well as suggestions for improvements.
A number of important issues can be investigated in future research and app development. In the subjective assessment of patient recovery, an area that should be addressed is the establishment of minimum scores that would act as red flags and determine when a visit to the hospital or physician may be warranted. Furthermore, from a medicolegal perspective, it may be prudent to develop an automated response that informs patients that their scores and images have actually been reviewed by the surgeon. In addition, patients who more easily forget to respond may benefit from a built-in reminder system. Since typical follow-up occurs at 1, 2, and 6 weeks, web-based responses at each interval may be more clinically relevant and attractive to patients than the system proposed in this study. The ability for patients to ask questions that they can flag as emergency, urgent, or nonurgent may also be a feature that reduces their anxiety and increases their satisfaction. After the fine-tuning of the mobile app, a prospective randomized controlled trial should be conducted to compare standard clinic-based follow-up with mobile web-based follow-up alone.
Conclusion
Innovations in mobile technology can have dramatic impacts in medicine. This system has the potential to assess patient recovery trends in greater detail and change the postoperative treatment plan for patients recovering well and poorly, and it was well received by the patients and physicians at our institution. It will be important to study the financial implications of this method of follow-up for patients, physicians, and hospitals. Recognizing the limitations of this study and those of the current application is essential before moving forward with a study comparing standard clinic follow-up and mobile web-based follow-up alone.
Appendix
Surveys
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.S. and S.S. are shareholders in QoC Health Inc.
Ethical approval for this study was obtained from Women’s College Hospital Research Ethics Board (2011-0023-E).
References
- 1. Alexander I. The impact of future trends in electronic data collection on musculoskeletal research and evidence-based orthopaedic care. Arthroscopy. 2003;19(9):1007–1011. [DOI] [PubMed] [Google Scholar]
- 2. Armstrong K, Semple J, Coyte P. Replacing ambulatory surgical follow-up visits with mobile app home monitoring: modelling cost-effective scenarios. J Med Internet Res. 2014;16(9):e213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Benhamou P, Boizel R, Perreal F, et al. One-year efficacy and safety of web-based follow-up using cellular phone in type-1 diabetic patients under insulin pump therapy: the PumpNet study. Diabetes Metab. 2007;33:220–226. [DOI] [PubMed] [Google Scholar]
- 4. Corrigan MA, Murphy RK, Dhillon P, et al. Improving surgical outpatient efficiency through mobile phone text messaging. Surg Innov. 2011;18(4):354–357. [DOI] [PubMed] [Google Scholar]
- 5. Dwyer T, Wasserstein D, Mahomed N, Gandhi R, Ogilvie-Harris D. Predictors of complication and re-operation after knee cruciate ligament reconstruction in Ontario 1992-2008. J Bone Joint Surg. 2012;308:94–99. [Google Scholar]
- 6. Franko O. Smartphone apps for orthopaedic surgeons. Clin Orthop Relat Res. 2011;(469):2042–2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jameson S, James P, Serrano-Pedraza I, Reed M, Deehan D. Complications following anterior cruciate ligament reconstruction in the English NHS. Knee. 2012;19:14–19. [DOI] [PubMed] [Google Scholar]
- 8. Kinnula S, Tapiainen T, Pokka T, Uhari M. Post-discharge follow-up of hospital associated infections in paediatric patients with conventional questionnaires and electronic surveillance. J Hosp Infect. 2012;80:13–16. [DOI] [PubMed] [Google Scholar]
- 9. Lau C, Kim J, Matsen F, Kim Y. Asynchronous web-based patient-centered home telemedicine system. IEEE Trans Biomed Eng. 2002;49(12):1452–1462. [DOI] [PubMed] [Google Scholar]
- 10. Martinez-Ramos C, Lopez R. Mobile phone-based telemedicine system for the follow-up of patients undergoing ambulatory surgery. Telemed J E Health. 2009;15(6):531–537. [DOI] [PubMed] [Google Scholar]
- 11. McDonald S, Hetrick S, Green S. Pre-operative education for hip or knee replacement. Cochrane Database Syst Rev. 2004;(1):CD003526. [DOI] [PubMed] [Google Scholar]
- 12. Myles PS, Weitkamp B, Jones K, Melick J, Hensen S. Validity and reliability of a postoperative Quality of Recovery score: the QoR-40. Br J Anesth. 2000;84(1):1115. [DOI] [PubMed] [Google Scholar]
- 13. Ochiai S, Tonotsuka H, Haro H. Prospective analysis of health-related quality of life and clinical evaluations in patients with anterior cruciate ligament injury undergoing reconstruction. Arch Orthop Trauma Surg. 2011;131:1091–1094. [DOI] [PubMed] [Google Scholar]
- 14. Semple J, Sharpe S, Murnaghan L, Theodoropoulos J, Metcalfe K. Using a mobile app for monitoring post-operative quality of recovery of patients at home: a feasibility study. JMIR Mhealth Uhealth. 2015;3(1):e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wood G, MacDonald S, McCalden R, Bourne R. An electronic clinic for arthroplasty follow-up: a pilot study. Can J Surg. 2011;54(6):381–386. [DOI] [PMC free article] [PubMed] [Google Scholar]