Abstract
Background
In high-income temperate countries, the number of hospitalizations for heart failure (HF) and acute myocardial infarction (AMI) increases during the winter. This finding has not been fully investigated in low- and middle-income countries with tropical and subtropical climates. We investigated the seasonality of hospitalizations for HF and AMI in Sao Paulo (Brazil), the largest city in Latin America.
Methods
This was a retrospective study using data for 76,474 hospitalizations for HF and 54,561 hospitalizations for AMI obtained from public hospitals, from January 2008 to April 2015. The average number of hospitalizations for HF and AMI per month during winter was compared to each of the other seasons. The autoregressive integrated moving average (ARIMA) model was used to test the association between temperature and hospitalization rates.
Findings
The highest average number of hospital admissions for HF and AMI per month occurred during winter, with an increase of up to 30% for HF and 16% for AMI when compared to summer, the season with lowest figures for both diseases (respectively, HF: 996 vs. 767 per month, p<0.001; and AMI: 678 vs. 586 per month, p<0.001). Monthly average temperatures were moderately lower during winter than other seasons and they were not associated with hospitalizations for HF and AMI.
Interpretation
The winter season was associated with a greater number of hospitalizations for both HF and AMI. This increase was not associated with seasonal oscillations in temperature, which were modest. Our study suggests that the prevention of cardiovascular disease decompensation should be emphasized during winter even in low to middle-income countries with tropical and subtropical climates.
Introduction
Coronary artery disease and heart failure (HF) are leading causes of morbidity and mortality worldwide.[1] In low- and middle-income countries, an aging population has been associated with an increased prevalence of both diseases. In Brazil, HF has become a leading cause of hospitalization while acute myocardial infarction (AMI) has become the main cause of death.[2, 3]
High-income countries with temperate climates are characterized by large seasonal oscillations in ambient temperature. In these countries, the association between winter and decompensated cardiovascular diseases has been clearly demonstrated. [4, 5] Biological mechanisms linking low temperatures to higher cardiovascular risk include persistently higher sympathetic nervous system activation, uncontrolled hypertension, and an increased incidence of respiratory diseases. Social and environmental mechanisms that hinge not only on low temperatures but on winter conditions more generally—such as shorter days, reduced physical activity, depression, and higher pollution levels—may also explain higher cardiovascular risk.[6, 7]
In low- and middle-income countries with a tropical and subtropical climate, the effect of mild winters on cardiovascular decompensation has not been fully investigated. In these countries, temperature does not oscillate much across seasons but other social and environmental factors such as precarious housing conditions, lack of thermal insulation, and greater pollution might increase the seasonal effect of winter on risk.[8–10]
In our study, we investigated the seasonality of hospitalizations for HF and AMI and tested the association between monthly average temperatures and hospitalizations for these diseases in the public health system of Sao Paulo, Brazil, the largest city in Latin America. We hypothesize that in Sao Paulo, the winter season is associated with increased cardiovascular risk even if seasonal temperature oscillations remain modest. We also speculate that this association might be rooted in the socio-economic circumstances faced by our studied population, i.e. the users of the public health system, such as greater exposure to air pollution, lack of thermal insulation, precarious housing, and other tribulations faced by those who live with low-income in such a megacity.
Methods
This was an observational, retrospective study of data obtained from 61 public hospitals in Sao Paulo. [11] The data was recorded prospectively on a monthly basis from January 2008 to April 2015 by the National Registry of Public Health, which is maintained by the Brazilian Public Health System. [12] To record the data, the National Registry requires that hospitals submit an official form (“Hospital Admission Authorization”) for each patient that is admitted under the auspices of the Brazilian Public Health System. This form contains the primary admission diagnosis and other patient data.
For our study, the inclusion criteria were: Age >20 years and admission for HF or AMI as defined by the International Classification of Diseases (ICD-10) [13], in which code I50 represents HF and code I21 represents AMI. Data on monthly average temperatures were obtained from the Environmental Sanitation Technology Company of Sao Paulo, based on 24 hourly measurements per day, from six meteorological stations in the city.[14] To calculate monthly average temperatures for the city, we first calculated average temperatures for each station and month, and then calculated the mean temperature levels for all stations for each month. This study was conducted in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans and was approved by the Institutional Review Board of the Hospital Israelita Albert Einstein. The study was granted a waiver for informed consent.
Statistical analysis
For each diagnosis, the average number of hospitalizations per month was compared across the four seasons—both for all patients and within separate gender and ten-year age groups—using generalized linear models with Poisson distribution, identity link function and Bonferroni multiple comparisons. The boundaries of each season followed the meteorological definition for the South Hemisphere [15], i.e. winter is comprised of June, July and August; spring is comprised of September, October and November; summer includes December, January and February, and autumn includes March, April and May. Monthly average temperature levels (mean ± standard deviation) were compared across the four seasons by analysis of variances and Bonferroni multiple comparisons. The Box-Jenkins autoregressive integrated moving average (ARIMA) model was used to test the association between ambient temperature and the average number of hospitalization per month. [16] The modeling process proceeded in three steps: first, the temporal effect of the series of cardiovascular events was removed by the ARIMA model; second, model parameters were chosen according to the autocorrelations and partial autocorrelations; and finally, the white noise or stationary time series was used to estimate the coefficients. For each series in the study, a regression parameter was added to test the influence of model specifications on the significance of obtained results. A p<0.05 was considered statistically significant. All statistical analyses were performed using SPSS statistical software version 20.0.
Results
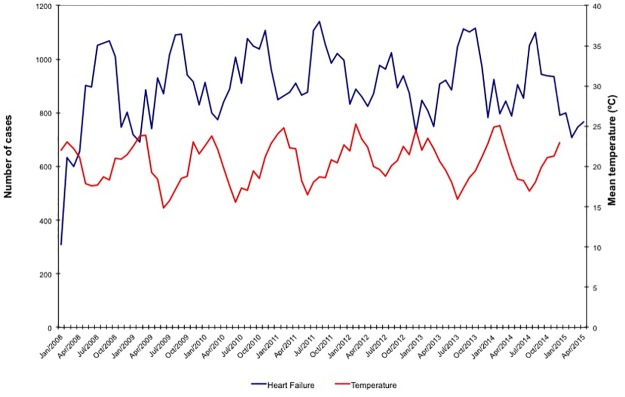
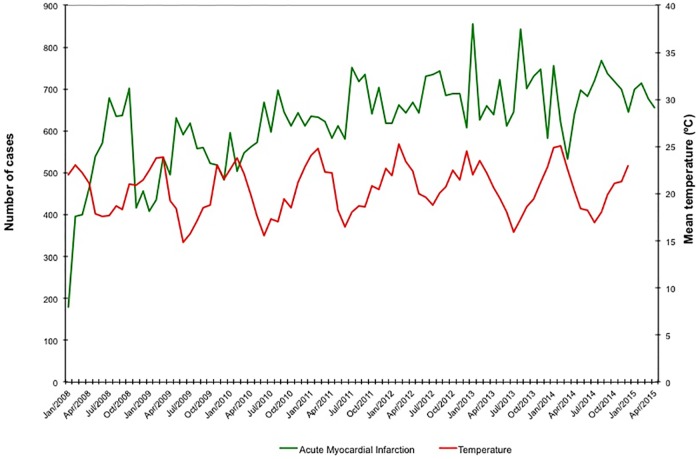
During the study period, the National Registry of Public Health recorded a total of 4,823,761 hospital admissions. Using the inclusion criteria outlined above, we identified 76,474 hospitalizations for HF (49.9% men, 67.7% ≥ 60 years) and 54,561 hospitalizations for AMI (63.3% men, 55.9% ≥ 60 years). Monthly average temperature levels and the number of hospitalizations for HF and AMI per month are illustrated in Figs 1 and 2. Seasonal average temperature levels were lowest in the winter (mean ± SD of 17.5 ± 1.3°C), moderately lower than the monthly average temperature recorded during the spring, summer and autumn (respectively, mean ± SD of 20.3 ± 1.4, 23.3 ± 1.2 and 20.7 ± 1.9; p <0.001 for comparison of winter vs. all other seasons).
Fig 1. Monthly average temperature levels and number of hospitalizations per month for heart failure.
Fig 2. Monthly average temperature levels and number of hospitalizations per month for acute myocardial infarction.
The average number of hospital admissions for HF and AMI per month peaked during winter, with an increase of up to 30% for HF and 16% for AMI, when compared to summer, which was the season with lowest figures for both diseases (respectively, HF: 996 vs. 767 per month, p<0.001; and AMI: 678 vs. 586 per month, p<0.001). These findings were not affected by gender (Tables 1 and 2). When analyzed within age groups, the average number of admissions for HF per month during winter was higher in patients older than 40, while the equivalent figure for AMI was higher in patients older than 50 (Tables 1 and 2). Using ARIMA analysis, we find that the average number of hospitalizations for AMI and HF per month increases during winter months; however, we did not find an association between temperature levels and hospitalizations (Table 3).
Table 1. Average number of hospitalizations per month for heart failure, per season, according to gender and age group.
| Characteristics of pts. with Heart Failure | Hospitalizations per Month | p | ||||
|---|---|---|---|---|---|---|
| Jan-Dec | Winter | Spring | Summer | Autumn | ||
| Gender | ||||||
| Female | 435 | 494 | 456 | 381 | 414 | <0.001 |
| Male | 434 | 502 | 451 | 386 | 406 | <0.001 |
| Age Group (years) | ||||||
| 20 to 29 | 14 | 15 | 13 | 14 | 14 | 0,102 |
| 30 to 39 | 33 | 34 | 34 | 31 | 33 | 0,108 |
| 40 to 49 | 75 | 85 | 73 | 70 | 73 | <0.001 |
| 50 to 59 | 159 | 181 | 164 | 141 | 152 | <0.001 |
| 60 to 69 | 206 | 233 | 216 | 184 | 194 | <0.001 |
| 70 to 79 | 211 | 244 | 225 | 183 | 196 | <0.001 |
| 80+ | 171 | 203 | 182 | 144 | 158 | <0.001 |
| Total | 869 | 996 | 907 | 767 | 820 | <0.001* |
*P<0.001 for comparisons between each season vs. the other three.
Table 2. Average number of hospitalizations per month for acute myocardial infarction, per season, according to gender and age group.
| Characteristics of pts. with AMI | Hospitalizations per Month | p | ||||
|---|---|---|---|---|---|---|
| Jan-Dec | Winter | Spring | Summer | Autumn | ||
| Gender | ||||||
| Female | 228 | 250 | 231 | 209 | 223 | <0.001 |
| Male | 392 | 429 | 394 | 378 | 372 | <0.001 |
| Age Group (years) | ||||||
| 20 to 29 | 4 | 4 | 3 | 4 | 4 | 0,116 |
| 30 to 39 | 18 | 18 | 18 | 19 | 17 | 0,685 |
| 40 to 49 | 79 | 81 | 81 | 77 | 78 | 0,298 |
| 50 to 59 | 172 | 185 | 172 | 170 | 164 | <0.001 |
| 60 to 69 | 171 | 187 | 176 | 159 | 164 | <0.001 |
| 70 to 79 | 117 | 135 | 118 | 106 | 110 | <0.001 |
| 80+ | 59 | 67 | 57 | 52 | 58a | <0.001 |
| Total | 620 | 678 | 626 | 586 | 595 | <0.001* |
*P<0.001 for comparisons between winter vs. other seasons, and spring vs. other seasons. There was no difference between summer and autumn. AMI, acute myocardial infarction. AMI, acute myocardial infarction
Table 3. ARIMA analysis on the seasonal variation of the rates of hospitalizations for acute myocardial infarction and heart failure, and on the association between hospitalization rates and temperature levels.
| Parameter | coefficient | Std. Error | T value | p | |
|---|---|---|---|---|---|
| Heart Failure | MA*1.12 | -0.29318 | 0.11708 | -2.5 | 0.012 |
| Temperature | 0.10976 | 0.32371 | 0.34 | 0.734 | |
| Acute Myocardial Infarction | MA*1.12 | -0.35871 | 0.11726 | -3.06 | 0.002 |
| Temperature | 0.1978 | 0.33522 | 0.59 | 0.555 |
*MA = moving average.
Discussion
In our analysis of data for Sao Paulo, we find an increase in the average number of hospitalizations per month for HF and AMI during the winter when compared to each of the other seasons, and an increase of up to 30 and 16%, respectively, when winter figures are compared to summer. The monthly average temperature during winter was only moderately lower than in other seasons, and we did not observe an association between ambient temperature and hospital admissions.
Numerous studies examining data from high-income countries with temperate climates have demonstrated an association between winter and the incidence and mortality from HF and AMI. [17–19] In these countries, the oscillation in temperature levels across seasons is quite large, with a marked decrease during the winter. Extremely cold temperatures can induce systemic adrenergic activation, increased peripheral vascular resistance, and systemic hypertension resulting in increases in both cardiac oxygen consumption and demands on cardiac output.[20, 21] Low ambient temperatures can also induce the release of fibrinogen and coagulation factors that may result on a hypercoagulable state and a higher risk of atherothrombosis. [22]
Similar assessments on the effects of winter on cardiovascular risk in low- and middle-income tropical countries are scarcer but still suggestive. A study conducted in Havana (Cuba), found higher mortality in AMI patients during winter.[8] In Bangladesh, a study using one small registry found that hospital admission rates for several cardiovascular decompensated diseases, including AMI and HF, peaked during the winter.[9] Some recent studies have shown that this increase in cardiovascular risk can be attributed, at least partially, to a decline in temperature. One large multinational study that tested the association between ambient temperature and general mortality found that most of the temperature-related deaths could be attributed to low temperatures typical of winter and not to high temperatures typical of summer. [23] Even if this association was more evident in high-income temperate countries, it was still present in low- and middle-income tropical countries such as Brazil and Thailand. Studies conducted in Taipei and Hong Kong also found that low temperature days and daily temperature oscillation are associated with increased risk for AMI and HF.[24–26] Similar to Sao Paulo, Taipei and Hong Kong have a humid subtropical climate and mild winters. Unlike Sao Paulo, however, they have a slightly wider gap in monthly average temperatures across seasons [27] and a much higher income per capita. [28] These differences hinder a direct comparison across these sites but they also suggest that lower temperatures might not be the only variable affecting the observed association between winter and increased hospitalizations for HF and AMI.
Two previous studies have examined the influence of winter on cardiovascular risk in Sao Paulo, Brazil. One study found an increase in mortality for AMI during winter but it relied exclusively on data for a single year (1997) [29]. Another study examined a larger dataset and found that hospitalization for HF increases during winter. [30] However, this study did not test whether this perceived increase was statistically significant and neither did it incorporate ambient temperature into its analysis.
In our study, we found an increase in hospitalizations for HF and AMI during the winter despite a moderate average winter temperature of 17.5°C, only 2.8 to 5.8°C lower than the other seasons. Besides the direct effects of low ambient temperatures on the cardiovascular system, environmental aspects linked to winter could help explain our findings. Sao Paulo winters are characterized by low humidity, limited rains and a higher frequency of thermal inversions, which occur when cold air gets trapped near the surface and underneath a layer of warmer air. [31] Together, these conditions prevent the dispersion of pollutants such as carbon monoxide (CO), nitrogen dioxide (NO2), sulfur dioxide (SO2), and inhalable particulate matter (PM10) that are associated with increased cardiovascular risk. [32] Lower ambient temperatures, low humidity, and high pollution could also reinforce each other as they contribute to a higher incidence of respiratory diseases and influenza, with a consequent increase in cardiovascular risk.[33]
On the socio-economic side, Sao Paulo is the economic engine of Brazil, with an estimated 11,253,503 inhabitants. [34] The city has been characterized by several decades of mostly unplanned urban growth. At present, approximately 40% of the population of its larger metropolitan area live in precarious housing conditions.[35] Moreover, its inhabitants are often exposed to massive traffic jams and significant pollution. [36] These issues are especially salient to its low-income citizens, a group that relies heavily on the services provided by the Brazilian Public Health System. The importance of socio-economic variables on winter risk has been noted in a recent multicenter study conducted in 14 European countries. This study found that Portugal had the highest rate of excess winter mortality, even though it has a milder winter than several other countries included in the analysis. [37] This study also demonstrated that per capita national income, per capita health expenditure, poverty rates, and several indicators of residential thermal standards were associated with excess winter mortality. These findings support the hypothesis that not only temperature levels, but also adverse socio-economic conditions may increase the effect of winter on cardiovascular risk.
Our study has several limitations. First, this was an observational study and despite statistical adjustments, a causal and definite relationship between seasonality and hospital admissions for HF and AMI cannot be determined. Second, we analyzed data maintained by the Brazilian Public Health System that accounts for 66% of hospital admissions in the country [38]. Data pertaining to the private health system were not available. Third, our dataset does not contain information on clinical characteristics besides age and sex. Similarly, we lacked data on pollution levels. For these reasons, we could neither adjust our results for comorbidities nor explore the direct effect of pollution on cardiovascular risk during winter. Finally, the Brazilian National Registry of Public Health provides only monthly data on hospital admissions so we could not analyze daily or weekly variation that could have revealed an association between cold days and an increase in cardiovascular risk. In spite of these limitations, our analysis of data for Sao Paulo demonstrates the seasonality of hospital admissions for HF and AMI, with an increase during relatively mild winters. Considering that mean temperatures were only moderately lower during the winter when compared to other seasons, our study raises the possibility that other factors related to disorderly urban occupation and urban poverty, such as a greater exposure to pollution and the lack of thermal protection in precarious housing, might also be associated with the seasonal increase in cardiovascular risk. This broader issue deserves further investigation.
In conclusion, in the megacity of Sao Paulo, winters were associated with an increased number of hospitalization for both HF and AMI. This relationship did not hinge on seasonal temperature oscillations. Our findings suggest that the prevention of cardiovascular disease decompensation should be emphasized during winter even in low to middle-income countries with modest temperature oscillations.
Supporting information
(XLS)
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. We would like to acknowledge Rogério Ruscitto Prado for his support with statistics.
Abbreviations
- AMI
acute myocardial infarction
- ARIMA
autoregressive integrated moving average
- HF
heart failure
Data Availability
Relevant data are available at: http://www2.datasus.gov.br/DATASUS/index.php?area=0203/.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–128. doi: 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albuquerque DC, Neto JD, Bacal F, Rohde LE, Bernardez-Pereira S, Berwanger O, et al. I Brazilian Registry of Heart Failure—Clinical Aspects, Care Quality and Hospitalization Outcomes. Arquivos brasileiros de cardiologia. 2015;104(6):433–42. doi: 10.5935/abc.20150031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Campos AM, Placido-Sposito A, Freitas WM, Moura FA, Guariento ME, Nadruz WJ, et al. ST-elevation myocardial infarction risk in the very elderly. BBA clinical. 2016;6:108–12. doi: 10.1016/j.bbacli.2016.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gallerani M, Boari B, Manfredini F, Manfredini R. Seasonal variation in heart failure hospitalization. Clinical cardiology. 2011;34(6):389–94. doi: 10.1002/clc.20895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spencer FA, Goldberg RJ, Becker RC, Gore JM. Seasonal distribution of acute myocardial infarction in the second National Registry of Myocardial Infarction. Journal of the American College of Cardiology. 1998;31(6):1226–33. [DOI] [PubMed] [Google Scholar]
- 6.Fares A. Winter cardiovascular diseases phenomenon. North American journal of medical sciences. 2013;5(4):266–79. doi: 10.4103/1947-2714.110430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah AS, Langrish JP, Nair H, McAllister DA, Hunter AL, Donaldson K, et al. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet. 2013;382(9897):1039–48. doi: 10.1016/S0140-6736(13)60898-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rivero A, Bolufe J, Ortiz PL, Rodriguez Y, Reyes MC. Influence of climate variability on acute myocardial infarction mortality in Havana, 2001–2012. MEDICC review. 2015;17(2):14–9. [DOI] [PubMed] [Google Scholar]
- 9.Khan RC, Halder D. Effect of seasonal variation on hospital admission due to cardiovascular disease—findings from an observational study in a divisional hospital in Bangladesh. BMC cardiovascular disorders. 2014;14:76 doi: 10.1186/1471-2261-14-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diaz A, Ferrante D, Badra R, Morales I, Becerra A, Varini S, et al. Seasonal variation and trends in heart failure morbidity and mortality in a South American community hospital. Congest Heart Fail. 2007;13(5):263–6. [DOI] [PubMed] [Google Scholar]
- 11.TABNET Prefeitura de Sao Paulo [http://tabnet.saude.prefeitura.sp.gov.br/cgi/tabcgi.exe?secretarias/saude/TABNET/cnes/estab.def.
- 12.Brasil. Ministerio da Saude. Secretaria Executiva. Datasus. Informaçoes de Saude. Morbidade e informações epidemiológicas [http://www2.datasus.gov.br/DATASUS/index.php?area=0203.
- 13.World Health Organization. International Classification of Diseases. [http://www.who.int/classifications/icd/en/.
- 14.CETESB-SP. Companhia de Tecnologia de Saneamento Ambiental—Relatório de qualidade do ar no Estado de São Paulo São Paulo [http://ar.cetesb.sp.gov.br/publicacoes-relatorios/.
- 15.National Oceanic and Atmospheric Administration [https://www.ncdc.noaa.gov/news/meteorological-versus-astronomical-seasons.
- 16.Box GEP J G. Time series analysis: forecasting and control. Revised Ed: ed. San Francisco: Holden Day; 1976. [Google Scholar]
- 17.Boulay F, Berthier F, Sisteron O, Gendreike Y, Gibelin P. Seasonal variation in chronic heart failure hospitalizations and mortality in France. Circulation. 1999;100(3):280–6. [DOI] [PubMed] [Google Scholar]
- 18.Loughnan ME, Nicholls N, Tapper NJ. Demographic, seasonal, and spatial differences in acute myocardial infarction admissions to hospital in Melbourne Australia. International journal of health geographics. 2008;7:42 doi: 10.1186/1476-072X-7-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stewart S, McIntyre K, Capewell S, McMurray JJ. Heart failure in a cold climate. Seasonal variation in heart failure-related morbidity and mortality. Journal of the American College of Cardiology. 2002;39(5):760–6. [DOI] [PubMed] [Google Scholar]
- 20.Westheim A, Os I, Thaulow E, Kjeldsen SE, Eritsland J, Eide IK. Haemodynamic and neurohumoral effects of cold pressor test in severe heart failure. Clin Physiol. 1992;12(1):95–106. [DOI] [PubMed] [Google Scholar]
- 21.Rodriguez-Garcia JL, Paule A, Dominguez J, Garcia-Escribano JR, Vazquez M. Effects of the angiotensin II antagonist losartan on endothelin-1 and norepinephrine plasma levels during cold pressor test in patients with chronic heart failure. International journal of cardiology. 1999;70(3):293–301. [DOI] [PubMed] [Google Scholar]
- 22.Yeh CJ, Chan P, Pan WH. Values of blood coagulating factors vary with ambient temperature: the Cardiovascular Disease Risk Factor Two-Township Study in Taiwan. The Chinese journal of physiology. 1996;39(2):111–6. [PubMed] [Google Scholar]
- 23.Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386(9991):369–75. doi: 10.1016/S0140-6736(14)62114-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goggins WB, Chan EY. A study of the short-term associations between hospital admissions and mortality from heart failure and meteorological variables in Hong Kong: Weather and heart failure in Hong Kong. International journal of cardiology. 2017;228:537–42. doi: 10.1016/j.ijcard.2016.11.106 [DOI] [PubMed] [Google Scholar]
- 25.Goggins WB, Chan EY, Yang CY. Weather, pollution, and acute myocardial infarction in Hong Kong and Taiwan. International journal of cardiology. 2013;168(1):243–9. doi: 10.1016/j.ijcard.2012.09.087 [DOI] [PubMed] [Google Scholar]
- 26.Qiu H, Yu IT, Tse LA, Tian L, Wang X, Wong TW. Is greater temperature change within a day associated with increased emergency hospital admissions for heart failure? Circ Heart Fail. 2013;6(5):930–5. doi: 10.1161/CIRCHEARTFAILURE.113.000360 [DOI] [PubMed] [Google Scholar]
- 27.Hong Kong Observatory [http://www.weather.gov.hk/cis/climahk_e.htm.
- 28.Global Metro Monitor [https://www.brookings.edu/research/global-metro-monitor/
- 29.Sharovsky R, Ce sar LA. Increase in mortality due to myocardial infarction in the Brazilian city of Sao Paulo during winter. Arquivos brasileiros de cardiologia. 2002;78(1):106–9. [DOI] [PubMed] [Google Scholar]
- 30.Godoy HL, Silveira JA, Segalla E, Almeida DR. Hospitalization and mortality rates for heart failure in public hospitals in Sao Paulo. Arquivos brasileiros de cardiologia. 2011;97(5):402–7. [DOI] [PubMed] [Google Scholar]
- 31.Sanchez-Ccoyllo OR, de F. The influence of meteorological conditions on the behavior of pollutants concentrations in Sao Paulo, Brazil. Environ Pollut. 2002;116(2):257–63. [DOI] [PubMed] [Google Scholar]
- 32.Saldiva PH, Pope CA 3rd, Schwartz J, Dockery DW, Lichtenfels AJ, Salge JM, et al. Air pollution and mortality in elderly people: a time-series study in Sao Paulo, Brazil. Archives of environmental health. 1995;50(2):159–63. doi: 10.1080/00039896.1995.9940893 [DOI] [PubMed] [Google Scholar]
- 33.Barnes M, Heywood AE, Mahimbo A, Rahman B, Newall AT, Macintyre CR. Acute myocardial infarction and influenza: a meta-analysis of case-control studies. Heart. 2015;101(21):1738–47. doi: 10.1136/heartjnl-2015-307691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Política IBdGe. [http://www.ibge.gov.br/home/estatistica/populacao/censo2010/indicadores_sociais_municipais/indicadores_sociais_municipais_tab_uf_zip.shtm.
- 35.UN-Habitat. São Paulo: A Tale of Two Cities. Nairobi, Kenya: UNON; 2010. 157 p.
- 36.CETESB-SP. Emissoes Veiculares no Estado de Sao Paulo Sao Paulo2013 [http://veicular.cetesb.sp.gov.br/wp-content/uploads/sites/35/2013/12/relatorio-emissoes-veiculares-2013.pdf
- 37.Healy JD. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. Journal of epidemiology and community health. 2003;57(10):784–9. doi: 10.1136/jech.57.10.784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brasil. Ministério do Planejamento, Orçamento e Gestão. Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional por Amostra de Domicílios. Acesso e Utilização de Serviços de Saúde. 2013 [http://biblioteca.ibge.gov.br/visualizacao/livros/liv94074.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLS)
Data Availability Statement
Relevant data are available at: http://www2.datasus.gov.br/DATASUS/index.php?area=0203/.