Abstract
Purpose: A full 85% of Canadians fail to meet physical activity (PA) guidelines, and 69% report being sedentary. Physical therapists are uniquely positioned to promote an active lifestyle; thus, we explored the PA and sedentary behaviour (SB) of Master of Physical Therapy (MPT) students as well as the associated facilitators and barriers. Methods: We used a mixed-methods approach, accelerometry and photovoice (a focus group discussion in which participants discussed self-selected photographs). Accelerometer data were used to quantify PA (light, moderate, and vigorous) and SB. Thematic analysis of the focus group discussion was informed by the socio-ecological model. Results: A total of 26% of participants met national PA guidelines, and mean daily sedentary time for participants was 670.7 (SD 34.4) minutes. Photovoice analysis revealed four main themes related to the facilitators of and barriers to PA and SB: (1) priorities and life balance, (2) commitment and accountability, (3) environment, and (4) MPT programming. Conclusions: A full 74% of participants did not meet the recommended PA guidelines; this is concerning given their immanent roles as health care professionals. Physical therapists are well prepared to prescribe PA to clients. Not only do MPT students need competencies in prescribing PA and exercise, but they may also need to be supported in meeting PA guidelines themselves and limiting SB throughout their studies.
Key Words: health promotion, physical activity, sedentary lifestyle
Abstract
Objectif : au total, 85 % des Canadiens ne respectent pas les lignes directrices en matière d'activité physique (AP), et 69 % déclarent être sédentaires. Les physiothérapeutes sont en position idéale pour promouvoir des modes de vie active. Les auteurs ont donc exploré l'AP et le comportement sédentaire (CS) d'étudiants à la maîtrise en physiothérapie (MPT), de même que les incitatifs et les obstacles qui s'y associent. Méthodologie : les auteurs ont utilisé une méthode mixte, l'accélérométrie et la méthode photovoix (discussion d'un groupe de travail sur des photos qu'il sélectionnait lui-même). Ils ont utilisé les données d'accélérométrie pour quantifier l'AP (légère, modérée et vigoureuse) et le CS. Ils ont utilisé le modèle socioécologique pour étayer leur analyse thématique des discussions du groupe de travail. Résultats : au total, 26 % des participants respectaient les lignes directrices nationales en matière d'AP, alors que la période de sédentarité moyenne des participants était de 670,7 minutes (ÉT 34,4). L'analyse de photovoix a révélé quatre grands thèmes liés aux incitations et aux obstacles à l'AP et au CP : 1) priorités et équilibre de vie, 2) engagements et responsabilités, 3) environnement et 4) programme de MPT. Conclusions : un total de 74 % des participants ne respectaient pas les lignes directrices recommandées en matière d'AP. C'est inquiétant puisqu'ils deviendront bientôt des professionnels de la santé. Les physiothérapeutes sont bien préparés pour prescrire l'AP à leurs clients. Non seulement les étudiants à la MPT ont-ils besoin de compétences pour prescrire l'AP et l'exercice, mais ils ont peut-être aussi besoin de soutien pour respecter eux-mêmes les lignes directrices en matière d'AP et limiter leur CP pendant leurs études.
Mots clés : activité physique, mode de vie sédentaire, promotion de la santé
People can maintain optimal health throughout their lives by consistently engaging in physical activity (PA).1 For example, the Canadian Society for Exercise Physiology (CSEP) recommends that adults aged 18–64 years participate in at least 150 minutes of moderate to vigorous physical activity (MVPA) each week, in bouts of 10 minutes or more, to gain the associated health benefits.2 However, whether the health benefits resulting from an active lifestyle are sufficient to overcome the risk of deleterious health consequences associated with sedentary behaviour (SB), such as prolonged sitting, is the subject of ongoing debate.1,3–6 SB is reported to be an independent risk factor for chronic conditions, regardless of the amount of MVPA.1,3–6 Canadian adults aged 18–79 years spend approximately 10 of their waking hours each day being sedentary (i.e., engaging in activities characterized by an energy expenditure of 1.5 metabolic equivalents or less, such as sitting or reclining).7 This supports the hypothesis that many adults face barriers to mitigating the time they spend being sedentary, such as individual perspectives, the social environment, the physical built environment, and public policy.8
To overcome the barriers that may contribute to increased SB and decreased PA in people's lives, health care professionals, such as physical therapists, may increasingly be consulted to prescribe health-promoting activities—specifically, to increase PA and decrease SB.9,10 Small changes, such as replacing sedentary time with light PA, can be important for people's health.
Young adults transitioning to post-secondary education experience an almost fourfold decrease in PA as well as an increase in SB,11 and these behaviours often persist into later adulthood.12–14 In Canada, 15% of adults accumulate the recommended 150 minutes of MVPA each week,15 and only 0.1% of a sample of Canadian university students meet these PA guidelines.14 Similar findings exist across the globe. For example, 50% of college students in the United States are physically inactive and do not meet the national PA guidelines,10 and university students in the United Kingdom are sedentary for an average of 8 hours a day.16 One Canadian study that explored self-reported PA patterns of resident and staff physicians reported that participants were moderately to vigorously physically active for approximately 164 minutes each week;17 according to these self-reported data, participants exceeded the guidelines recommended by CSEP. Physical therapy clinicians and students in the United States self-reported higher exercise rates than those for the US adult population as a whole as well as for other health care professionals.18
Objective measures of physical activity, such as accelerometry, are considered more accurate than self-report assessment of PA. Much of the literature on PA and SB patterns among health care professionals, including physical therapy clinicians and students, however, has used self-report PA measures. The perceived facilitators of and barriers to regular PA among samples of university students living in the United Kingdom and Spain, and among medical residents and physicians in one province in Canada, have been documented.17,19,20 Facilitators of PA include positive social networks, perceived enjoyment, time, and university and programme characteristics,19,21 and barriers include such factors as fatigue after the work day, inconvenience and lack of time, family responsibilities, poor weather conditions, and academic pressure.17,21 Calls to action have been generated for health care professionals in higher education to address these concerns and integrate innovative ideas for promoting PA on university campuses;10 for example, designing campuses that promote PA and integrating sports time into the curriculum may facilitate the PA of university students.10,21 Health care professional colleges and programmes are logical venues for implementing such interventions; in doing so, they can serve as a prototype for other colleges and programmes.
Physical therapists are well positioned to promote physically active lifestyles with the potential to benefit population health.22,23 As such, MPT students are trained to prescribe PA and exercise across their patients' life span and to apply knowledge about behavioural change and health promotion across levels of care.22 Despite this knowledge and training, the amount of time that MPT students spend being physically active and not sedentary is not known. Furthermore, the perceived facilitators of and barriers to living an active life while they are attending university have not been reported.
Revealing the PA and SB patterns of university students requires a multifaceted, socio-ecological approach that will identify the factors that inform students' decisions about being sedentary or physically active. This study examined the PA and SB patterns of MPT students using the objective measure of accelerometry and revealed students' perceptions of the factors that influence their PA and SB using photovoice, a qualitative method that actively engaged participant investigators in the study.
Method
Participant recruitment
A convenience sample of MPT students was recruited from the first and second years of the University of Saskatchewan's MPT programme. A total of 80 eligible students were approached to participate, either face to face or by email, and 43 volunteered. After they had signed up and given their informed consent, participants completed two simultaneous phases of data collection: (1) accelerometry to objectively measure their PA and SB and (2) photovoice to capture their perceptions about the facilitators of and barriers to their being physically active. Ethics approval was obtained from the University of Saskatchewan Research Ethics Board in Behavioural Science Research (no. Beh 14–127).
Study design
This project featured a mixed-methods approach to exploring the PA and SB of MPT students using accelerometry and photovoice. Accelerometry provides objective PA and SB patterns. Accelerometer data were analysed using ActiLife software (ActiGraph, Pensacola, FL). Photovoice allows for active engagement of research participants in the research process. Active engagement is increasingly being applied in health promotion and behavioural health research to clarify and inform health-promoting interventions that integrate multilevel socio-ecological factors.24 As a result, actively engaging the participants themselves through photovoice as contributing partners ensures that their perspectives, viewpoints, and values are highlighted and embedded throughout the research process.25,26 Photovoice integrates focus group discussion into its overall process, as described later. Qualitative data (photographs and focus group discussion) were thematically analyzed.
Accelerometers
Each participant wore a triaxial accelerometer (ActiGraph GT3X+; ActiGraph, Pensacola, FL) for 7 consecutive days in June 2014 (except while bathing or sleeping) to objectively capture PA and SB.27 Triaxial accelerometers measure acceleration in the vertical, anteroposterior, and mediolateral planes, thereby providing a spectrum of PA, including SB.28 The accelerometer was attached to a participant's body on an elastic belt positioned over the right hip. The accelerometers were initialized to collect movement data at a frequency of 100 Hertz. After the data were downloaded, 60-second epochs (movement data or activity counts captured every 60 seconds) were applied.15,29
Photovoice
Photovoice is a qualitative research methodology that has been successfully used in the university setting.24,30,31 Photovoice supports the emergence of participants' voices, providing them with pertinent and applicable evidence with which to address policies that have an impact on their lived experience.30,31 At the same time, it allows participants the opportunity to apply their unique knowledge to positively influence their context and environment. In this project, the MPT student participants applied their knowledge of health promotion, PA, and intervention design to their professional development and student experience at university by means of photovoice. Participants were asked to document the perceived facilitators of and barriers to being physically active or sedentary by capturing images of their daily experiences and reality through photography. This actively engaged the participants in illuminating the “why”24,30 in ways that supported and empowered them to become more physically active themselves and thereby potentially better understand the needs of their future patients and clients.
Participants were offered digital cameras so that they could take photographs of their experiences; however, most participants opted to use their own cameras for convenience and ease of use. Before data collection, participants received training in photovoice and in the ethical considerations of taking photographs, including ensuring privacy, obtaining informed consent, and avoiding taking images that could harm an individual's reputation.24
The photovoice process involved four steps:
During the week in which participants wore the accelerometers, they took photographs of the major facilitators of and barriers to their PA level and SB patterns.
Participants selected the two or three photographs that were most representative of these facilitators and barriers.
In the focus group, participants were asked a question about their photographs and were given time to reflect on their answer before engaging in group discussion.
Participants shared their responses to the guided questions while engaging in one 45-minute focus group.
Focus groups
The original goal was to conduct focus groups consisting of 6–10 participants each; however, because of participants' scheduling and availability constraints, we modified the process and organized four focus groups of 9–12 participants each. Focus groups were conducted in a classroom in the School of Physical Therapy building at a time and date convenient to the participants after they had worn the accelerometer for the requisite 7 days. Each focus group was audio recorded (with the participants' permission) and facilitated by a moderator and a recorder. Each discussion started with an introduction, followed by a series of guided questions related to the photographs taken by the participants. Each participant was given time to reflect on each question before engaging in group dialogue, allowing them to provide thoughtful responses in their own words and reflecting on the meaning of their chosen photographs.
The focus group facilitator encouraged as many participants as possible to engage in the discussion, and participant comments stimulated other participants' thinking and sharing. Furthermore, at the end of the focus group, the facilitator asked all group members whether anything had been missed in the discussion. Examples of the guided questions included “Why did you take this picture? “How does this impact or affect your daily lifestyle?” and “Is there anything you could do to strengthen or improve this situation you are describing (based on the photograph)?” Beverages and snacks were provided for participants during the focus group, and a small incentive was offered afterward (each participant received a $10 coffee card). The audio recordings were transcribed by Social Sciences Research Laboratory at the University of Saskatchewan.
Data analysis
Accelerometer analysis
Accelerometer data were first compiled to determine the number of participants who had met the valid wear-time criteria. A valid wear day was defined as 600 minutes or more of monitor wear time. An interval of at least 60 consecutive minutes of zero activity was defined as non–wear time.15,27 Non–wear time was subtracted from 1,440 minutes (i.e., 24 h) to determine wear time. Only participants with 6 or more valid wear days were included in our results.
The epoch-level data were analyzed using ActiLife software (version 6.10.2). The variables of primary interest obtained from the accelerometers included average minutes of sedentary time, light PA, moderate PA, vigorous PA, and MVPA in bouts of 10 minutes or more per day. Data were analyzed using descriptive statistics to provide a snapshot of participants' activity levels (both PA and SB). The time spent at each intensity level was calculated according to cut-point thresholds reported by Troiano and colleagues29 (see Table 1). The Troiano algorithm is a common method of accounting for incidental interruptions, and using it allowed us to correlate our data with data from the US 2008 National Health and Nutrition Examination Survey.29 MVPA in bouts of 10 minutes or more was determined by recorded counts above the moderate-intensity cut-point, with no more than two observation points allowed below this threshold in any 10 consecutive minutes (i.e., 8 of 10 min had to consist of ≥2,020 counts/min to be accepted).15
Table 1.
Cut-Points Used to Determine the Time Spent at Each Level of Movement Intensity
| Intensity | Metabolic equivalents | Example | Accelerometer count range (counts per min) |
| Sedentary | 1 to <2 | Sitting, reclining, standing | <100 (including wear-time zeros) |
| Light | 2 to <3 | Walking <3.2 km/h; light play | 100–2,019 |
| Moderate | 3 to <6 | Walking >3.2 km/h; aerobics | 2,020–5,998 |
| Vigorous | ≥6 | Jogging, running | ≥5,999 |
Photovoice analysis
A thematic analysis of the transcribed photovoice focus group discussions was informed by the socio-ecological model (SEM).32,33 The SEM provides a framework for understanding the multilayered determinants of health that influence PA and SB by integrating individual, interpersonal, community, organizational, and societal factors.32 The focus group transcripts were categorized into themes and sub-themes using the SEM framework as a guide; a theme had to appear in at least three transcripts to be included in the final theme development.
Results
Participant demographics
We recruited 43 participants (43.8% of the MPT student population), 31 first-year and 12 second-year students (7 men, 36 women), aged 22–33 years, with a mean age of 24.9 (SD 2.6) years. Of the 43 participants, 35 met the valid wear-time criteria and were included in this study. No missing data were observed among the 35 participants with valid wear-time.
Accelerometer results
The average accelerometer wear time was 914.5 minutes (≈15 h) per day. Of the 35 individuals who met the valid wear-time criteria, 9 (25.7%) met the CSEP guideline of at least 150 minutes of MVPA each week (as recorded in ≥10-min bouts), 11 (31.4%) accumulated 100–149 minutes, 10 (28.6%) accumulated 50–99 minutes, and 5 (14.3%) accumulated 0–49 minutes.
Participants spent, on average, the following number of minutes each day in each PA category: 206.9 (SD 15.8) minutes (≈3.4 h) in light PA, 32.7 (SD 11.7) minutes (≈0.54 h) in moderate PA, and 4.2 (SD 1.2) minutes in vigorous PA (≈0.07 h). They spent a total of 36.9 (SD 12.9) minutes each day in MVPA. However, when the time spent in MVPA was broken down into bouts of MVPA accumulated over 10 consecutive minutes or more, time spent in MVPA decreased to 16.7 (SD 4.7) minutes. The same group of participants spent, on average, 670.7 (SD 34.4) minutes in SB daily, equivalent to an average of 11.2 hours per day.
Photovoice results
Four themes were identified from the students showing their photographs and the focus group discussions: (1) priorities and life balance, (2) commitment and accountability, (3) environment, and (4) MPT programming.
Theme 1: Priorities and life balance
School comes first
Numerous participants admitted to prioritizing school responsibilities and academics, which required prolonged SB over PA: “Put school first because it has to get done and it's important to all of us,” “My lifestyle choices are based around studying,” and “We prioritize school … it's the central focus of our schedules” (see Figures S1, S2, and S3 online). Participants also specifically prioritized academics over healthy lifestyle choices: “Sacrifice either sleep or school work to get physical activity” (see Figure S4 online). Another participant expressed frustration with finding time for both PA and the studying required to maintain high academic standards: “It's a disaster area when I study, and I'm buried under books for the most part and don't find enough time to go out and exercise … studying is a big barrier” (see Figure 1).
Figure 1.
Buried in books, no time for exercise.
Binge working out
Participants engaged in adequate and consistent PA at times when academic demands were low, but school work often interrupted these routines. In response to one participant's photograph related to injuries being a barrier to maintaining PA levels (see Figure S5 online), another participant stated, “I should probably work out, and I'll be less sore; it's not really an injury,” followed by
It's like binge working out … have a week where I work every day, I go to the gym, I work really hard, and then you're busy again, so I can't work out for 2 weeks … and go again, and it's like I never worked out before, and you're sore because it's been so long since you last did that thing.
Participants discussed their frustration with trying to maintain a regular exercise routine while juggling a varying course schedule consisting of different modules. Participants commonly discontinued exercising during examinations or major projects:
I totally agree; I did that last module. I started working out for 3 weeks straight, and I was doing really well, and then finals hit, and I was like done. I didn't work out all through finals, and then I've done a little bit throughout practicum and stuff, but I haven't really gotten back into the flow of it again.
Finding life balance
Participants identified finding life balance as a personal solution or facilitator to help them combat the barriers to PA. They recognized the importance of PA in the physical therapy profession and were compelled to live up to the reputation that physical therapists lead a healthier lifestyle than the general population:
People come to school with salads for lunch now, and they used to bring like a burger or whatever, like people that altered their lifestyle throughout the programme just to try to live up to that reputation; I guess that physio is living healthier in life. And it also really encourages me to be more active out in the community, such as, yeah, the marathon
and “Have to maintain a physical lifestyle to do our job” (photograph not shown). Scheduling PA into their daily calendars as a priority and accessing on-campus facilities supported students' engagement in activities and ensured that different life domains were equally represented: “Scheduling your time, and then work really hard, and then do something you really enjoy doing” (see Figure S6 online).
Theme 2: Commitment and accountability
Friends, family, and pets
Participation in PA was facilitated when students had someone or something to hold them accountable for their actions. Photographs in this theme included photographs of friends and family members (not shown). As one participant stated, “It was nice having friends who like to do activities, because then if they want to do activities, of course you're going to be active.” Social groups had a positive, facilitative influence on activity levels and helped motivate participants to be active outside school. One participant divulged that she would not be as active without the support of friends: “Having people to work out with is the reason I stay active.” Another participant described a family member as a positive role model: “Having a role model of [a] healthy lifestyle and always working out, no matter how busy she seems … that's kind of how I learned how to be physically active.”
Pets were also highlighted as an important factor in facilitating consistent PA, as indicated by this participant: “That's my dog; it's kind of to symbolize guilt. I feel like I have to exercise her, so it's a facilitator for me because it's mostly like, oh, dog needs to walk, so I'll walk, like I'll make time for that” (see Figure 2a). This was confirmed by another participant:
This picture I took in front of the river too because I wanted to show that our city does a really good job preserving by the river and all the trails, and it's actually really nice to be out there, and Sadie likes to go for walks; otherwise, she might go stir-crazy in my house, so keeping her out. That's pretty much it, so it's a facilitator to physical activity (see Figure 2b).
Figure 2.
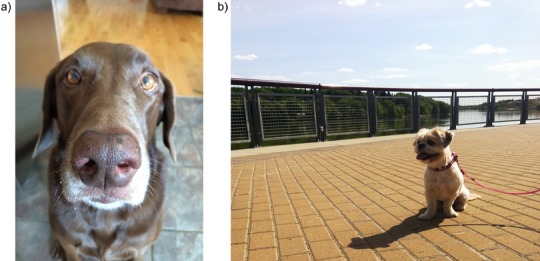
Pets facilitate physical activity: (a) Making time for my dog; (b) my dog gets me out on the trails.
Teams
Playing a team sport with friends made participants more likely to engage in the activity because it helped maintain relationships outside the programme. Participants' photographs in this theme captured images of team sports and exercising with friends (photographs not shown). The benefits of collective group activities were greater enjoyment and ease of participation as well as the creation of a large support network: “Getting involved inside a group so you have a support system around. There is someone to keep you going and keep you committed.” Team sports kept participants committed to staying active: “A group makes it easier not to quit.” Teams required a member to be accountable to multiple people; if a team member chose to forfeit a game, it directly influenced the entire team: “If you don't go, you'll kind of let the team down.”
Group classes
Several participants took photographs of group exercise classes and indicated that these helped them maintain PA (photographs not shown). Obligations such as monetary investment and pre-scheduled times for group classes helped participants prioritize their time to include PA. One student commented, “An activity that's like planned already that I have to go to, as opposed to just going to the gym—I'm more likely to go if it seems like an obligation.” Another commented, “Having the commitment to go at a certain time and doing a certain activity to kind of force yourself to do some exercising.” A spin class participant noted that paying money and signing up for the class kept her accountable to going and gave structure to the week. One participant mentioned that several MPT students from the previous year had signed up for a half-marathon together, which inspired students in the current year to train together.
Theme 3: Environment
Weather
Participants' photographs and discussions indicated that the weather was both a barrier to and a facilitator of PA. One participant stated that “rain … stops me from biking to school.” Participants admitted that they participated in fewer outdoor activities during cool or wet weather (see Figure 3a) and described being more active in favourable weather (see Figure 3b): “In the winter it's a lot harder to get up before class, where now I find it's a lot easier. Daylight hours, I think, play a role.” Another participant acknowledged that she was “more physically active in the summer.”
Figure 3.

Weather can hinder or support physical activity: (a) Rain is a barrier to staying active; (b) just having scenery on a nice day, (you) are more likely to go out and exercise
Built environment
Participants acknowledged that living arrangements enhanced their PA levels: “I live in a big building, where I have to take four flights of stairs every day. And it also has a nice exercising room” (see Figure S7 online). Living close to a fitness facility also facilitated PA: “Having the facility there that's close to my house … makes it really easy to get to and a good resource to use for activities” (see Figure S8 online). Active forms of transportation to and from university were also discussed as facilitators to PA: “Over the week I really wish I could maybe not drive to school; it's kind of an impeding factor … riding a bike to school [may improve this]” (see Figure S9 online). This was confirmed by another participant: “With mid-terms, I knew I wasn't going to get to the gym … so instead of driving to school, I biked to school all week, so it's not really a lot of physical activity, but at least it's something.”
The design of the university campus and School of Physical Therapy building affected PA behaviours. One participant stated that the building “limits me from participating in as much physical activity as I'd like,” and another thought that the school had limited resources and equipment available for students' recreational use. However, participants identified the positive aspects of having the Physical Activity Complex on the far side of campus:
I took a picture of the Physical Activity Complex, and I think it's very beneficial for students … because it's right on campus and it's very convenient for us to access to go to the gym whenever we want … all the equipment you can think of … you can go to the track and do runs upstairs, squash boards, you can do rock climbing, and so it's all the equipment that is all there. Especially for students like us, we can't really afford to go other places, like, yeah, getting membership at other places, which are pretty expensive for us, and then we can't really afford it, so having this included in our tuition, I guess, makes it more accessible (see Figure 4).
Figure 4.

Convenient and affordable access to facilities is beneficial.
Theme 4: Master of Physical Therapy programming
Time intensive
Participants indicated that the MPT programme structure was a common barrier to PA. One participant stated, “The thing about our schedule is that it's a full-time job, that you're here that often. But then you go home, and you spend just as much time going over the things you just did or doing assignments or more” (see Figure S10 online). Participants often said that they needed to balance their schedule around the challenges presented by the programme, such as long school days, studying commitments, and group work, which were barriers to PA. Specifically, participants often had only limited time for exercise after organizing group work around the conflicting schedules of multiple classmates.
Alternate schedule
Several participants found committing to recreational activities at the university difficult because their class schedules frequently shifted between on-campus modules and off-campus clinical placements. One participant shared her frustrations as follows: “Can you join a league because all of a sudden you're gone on placement?” One solution that participants suggested was to collaborate with other health sciences institutions, which might share similar scheduling challenges. Others highlighted the fact that they seek out activities that are readily available to them at various times in the year (see Figure 5).
Figure 5.

Seeking out readily available physical activities is a solution to sedentary behaviour.
Sitting and sedentary behaviour
Participants emphasized how prolonged periods of sitting, and spending long hours in a classroom, negatively affected their health (see Figure 6). Most participants perceived their high SB level to be directly linked to the amount of time they spent sitting—both in the classroom and studying outside scheduled class hours. The MPT programme required students to attend class for up to 8 hours a day, which affected participants' energy levels. Participants felt conflicted because they were engaging in SB by sitting in classes that taught them the benefits of PA. A participant indicated with one photograph, “[We are] studying all the time; it was nice to study on my balcony. It's been kind of sunny out, but yes, same general conflict as everyone else … [studying and sitting] just take away from your activity time” (see Figure S11 online).
Figure 6.

Prolonged sitting has a negative impact on health.
Suggested solutions
In the discussions that ensued, students offered solutions that encouraged light PA over SB—such as including mandatory stretch breaks in class, incorporating PA into the school curriculum, and incorporating sit-to-stand desks into classrooms—as ways of offsetting the amount of sitting time in class. Although these suggestions did not address the barriers to increasing the amount of time spent in MVPA, participants indicated that spending more time in light PA may be more beneficial than maintaining long periods of SB.
Discussion
Health care professionals, including physical therapists, are in key positions to promote behavioural changes that increase PA among their clients and the general population, particularly in this societal context in which rates of chronic conditions are on an increase.23 The general Canadian population continues to experience diminishing levels of PA and increasing time spent in SB, both of which perpetuate the development of chronic conditions. Critical transition periods can influence lifestyle behaviour throughout the life span, including transitioning to university.20,21,34 Health care professionals who are more active themselves are more likely to confidently prescribe PA to clients and patients.18 PA levels that develop in young adulthood are known to track into later adulthood.11,16,35 Therefore, ensuring that University of Saskatchewan MPT students maintain recommended PA levels and limit SB during their training may support them in prescribing PA in their future clinical practices.
In this study, 25.7% of the student participants met the recommended PA guidelines, but the majority of participants fell short. These data confirm results from other studies that have explored PA behaviour among university students.10,12–14,36,37 Furthermore, participants spent approximately 11 hours per day engaged in SB. It is difficult to confidently ascertain why these higher levels of SB exist among our study participants; however, the qualitative photovoice data provide insight into the possible reasons for the observed PA and SB levels.
Participants were keenly aware of the importance of living an active lifestyle, yet they described numerous barriers to their ability to maintain consistent PA levels. Barriers to PA included academic pressure to perform, inconsistent and interrupted scheduling due to clinical placements outside their university community, limited time, fatigue, classroom design, and weather. These themes are consistent with findings from other studies that have explored barriers to PA among university students and health care professionals.17,19,20,23,34
Including photovoice methodology in the study enabled the participants to identify the facilitators to living a healthy lifestyle and suggest potential solutions to the identified barriers. These facilitators included social supports, purchasing memberships to instill a sense of obligation, active transportation, and team sports. Many of these identified facilitators have been described by others.19,21 Participants also suggested formally scheduling time to integrate PA into their curricula and courses, adding mandatory stretch breaks to classes, and incorporating innovative classroom designs that promote frequent position changes—all of which could offset the amount of time that participants spend in SB.
These suggestions corroborate the conclusions of other studies regarding the need for university programmes to consider integrating PA and sports into the curricula to address identified barriers.21 Data from the present study support the notion that incorporating enhanced stretch breaks and providing light PA alternatives to sitting during class would at least decrease or interrupt prolonged sitting time. Designing classrooms to promote frequent position changes during class or study time and addressing SB levels using standing desks or strategically placed treadmill or ergometer desks may help to address the perceived barriers.38
The use of photovoice in this study enabled participants to be active agents of change and apply their professional training and knowledge of behavioural change and health promotion to their university context. Participants were actively engaged in the research process through photovoice, which further informed their first-hand understanding of the complexities and relationships of the diverse socio-ecological factors that influence healthy choices. Participants were compelled to call other MPT students, faculty, and administrators to action, explore their own PA and SB levels, and work collaboratively to find ways to make PA choices the easier choices in the university setting.
The results of this study must be considered in light of several limitations. First, accelerometers have a limited ability to capture movement that is not step based (e.g., cycling or swimming). In addition, accelerometers do not record the increased energy expenditure associated with upper body movement, such as occurs during resistance training, and therefore could have underestimated the students' overall activity.15 Second, the cut-points we used to break down PA into different intensities, and thereby transfer the accelerometer data into meaningful information, may not correlate with other accelerometer data because of a lack of standardized protocols.
A third limitation was using convenience sampling to recruit participants; as a result, those who participated in the study could have had a heightened interest in their level of activity or inactivity. This could lead to possible bias—that is, perhaps many were already motivated and engaged and therefore more likely to take steps to address inactivity and SB. Fourth, both the act of wearing an accelerometer and engaging in photovoice might lead to immediate changes in behaviour; this was not accounted for in the analysis. A final limitation was including only one data collection time point: Data collection took place during June, when favourable weather may have biased results to increased PA levels (reflected in participant comments about the influence of weather).
Conclusions
Healthy lifestyle choices, such as increasing PA and decreasing SB, have a significant effect on students' health and should be a fundamental behaviour modelled by physical therapists. Physical therapists play a vital role in promoting health among individuals and populations,18,23 and students are expected to support and facilitate health-promoting behaviour with their future clients and patients.9 MPT students must be instilled with strong values about active living to ensure that they maintain optimal health and to build their confidence in prescribing PA in their future clinical practice. Further research is required into other MPT university programmes across Canada to expand our exploration and understanding of objective PA and SB patterns among MPT students, to highlight the commonalities among various facilitators of and barriers to engaging in an active lifestyle at university, and to clarify solutions to the identified barriers. Such initiatives will enable MPT students to obtain first-hand knowledge of the complex problem-solving skills required to support healthy lifestyles in individuals and populations while at the same time facilitating their ability to achieve optimal health throughout their studies.
Key Messages
What is already known on this topic
Despite the known health benefits of physical activity (PA),33 only a small percentage of Canadian adults (15%) meet the recommended Canadian Society for Exercise Physiology guidelines.15 Canadians report high levels of sedentary behaviour (SB), which may independently pose an increased risk of developing chronic conditions.1,4,6 Physical therapists are generally more active than the general population,18 and these exercise and PA experts are well positioned to prescribe PA to clients and patients.22,23 The PA levels of health care professionals are correlated with their confidence in prescribing PA in clinical practice.18,23,39 Therefore, Master of Physical Therapy (MPT) students not only should receive training in exercise and PA prescription and develop skills that facilitate behavioural change but also must be supported in maintaining recommended PA and curbing SB throughout their university studies.
What this study adds
This study provides a snapshot of objective PA levels and SB among a population of MPT students, along with their perceptions of the facilitators of and barriers to maintaining a healthy lifestyle. Integrating photovoice methods into the study enabled the participants to be actively engaged in the research process, encouraging them to be active agents of change in their programme while enhancing their opportunities to apply health promotion knowledge to their lived experience. The results of this study are relevant to other graduate students and programmes across Canada because low PA levels and too much SB challenge the health of both university students and the general population. The solutions identified by the participants are relevant to other MPT programmes across Canada as the profession builds a community of skilled, knowledgeable, and clinically competent physical therapists who are supported in living active, healthy lives during their training and beyond.
Supplementary Material
Supplement 1
Contributor Information
Tracey Smetaniuk, School of Physical Therapy, University of Saskatchewan, Saskatoon, Sask..
Darren Johnson, School of Physical Therapy, University of Saskatchewan, Saskatoon, Sask..
Jeremy Creurer, School of Physical Therapy, University of Saskatchewan, Saskatoon, Sask..
Kristi Block, School of Physical Therapy, University of Saskatchewan, Saskatoon, Sask..
Magdalena Schlegel, School of Physical Therapy, University of Saskatchewan, Saskatoon, Sask..
Scotty Butcher, School of Physical Therapy, University of Saskatchewan, Saskatoon, Sask..
Sarah N. Oosman, School of Physical Therapy, University of Saskatchewan, Saskatoon, Sask..
References
- 1. Biswas A, Oh PI, Faulkner GE, et al. . Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–32. https://doi.org/10.7326/M14-1651. Medline:25599350 [DOI] [PubMed] [Google Scholar]
- 2. Canadian Society of Exercise Physiologists. Canadian physical activity and sedentary behaviour guidelines [Internet]. Ottawa: The Society; 2012. [cited 2015 May 31]. Available from: http://www.csep.ca/CMFiles/Guidelines/CSEP_Guidelines_Handbook.pdf [Google Scholar]
- 3. Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56(11):2655–67. https://doi.org/10.2337/db07-0882. Medline:17827399 [DOI] [PubMed] [Google Scholar]
- 4. Owen N, Healy GN, Matthews CE, et al. . Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105–13. https://doi.org/10.1097/JES.0b013e3181e373a2. Medline:20577058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Owen N. Sedentary behavior: understanding and influencing adults' prolonged sitting time. Prev Med. 2012;55(6):535–9. https://doi.org/10.1016/j.ypmed.2012.08.024. Medline:22968124 [DOI] [PubMed] [Google Scholar]
- 6. Maher C, Olds T, Mire E, et al. . Reconsidering the sedentary behaviour paradigm. PLoS One. 2014;9(1):e86403 https://doi.org/10.1371/journal.pone.0086403. Medline:24454968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Statistics Canada. Directly measured physical activity of Canadian adults, 2007 to 2011 [Internet]. Ottawa: Statistics Canada; 2015. [cited 2016 Apr 7]. Available from: http://www.statcan.gc.ca/pub/82-625-x/2013001/article/11807-eng.htm [Google Scholar]
- 8. McMurray A, Clendon J. Primary health care in practice. 4th ed. Chatswood (NSW), Australia: Elsevier Australia; 2011. [Google Scholar]
- 9. Canadian Physiotherapy Association. Description of physiotherapy in Canada [Internet]. Ottawa: The Association; 2012. [cited 2015 Jun 5]. Available from: https://physiotherapy.ca/description-physiotherapy [Google Scholar]
- 10. Keating XD, Guan J, Piñero JC, et al. . A meta-analysis of college students' physical activity behaviors. J Am Coll Health. 2005;54(2):116–26. https://doi.org/10.3200/JACH.54.2.116-126. Medline:16255324 [DOI] [PubMed] [Google Scholar]
- 11. Larouche R, Laurencelle L, Shephard RJ, et al. . Life transitions in the waning of physical activity from childhood to adult life in the Trois-Rivières study. J Phys Act Health. 2012;9(4):516–24. https://doi.org/10.1123/jpah.9.4.516. Medline:22592870 [DOI] [PubMed] [Google Scholar]
- 12. Downs A, Van Hoomissen J, Lafrenz A, et al. . Accelerometer-measured versus self-reported physical activity in college students: implications for research and practice. J Am Coll Health. 2014;62(3):204–12. https://doi.org/10.1080/07448481.2013.877018. Medline:24377672 [DOI] [PubMed] [Google Scholar]
- 13. Raynor DA, Jankowiak NM. Accelerometry-determined adherence to the 2008 physical activity guidelines for Americans among college students. J Health Educ. 2010;41(6):353–62. https://doi.org/10.1080/19325037.2010.10599164 [Google Scholar]
- 14. Scarapicchia TM, Sabiston CM, Faulkner G. Exploring the prevalence and correlates of meeting health behaviour guidelines among university students. Can J Public Health. 2015;106(3):e109–14. https://doi.org/10.17269/cjph.106.4784. Medline:26125235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Colley RC, Garriguet D, Janssen I, et al. . Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011;22(1):7–14. Medline:21510585 [PubMed] [Google Scholar]
- 16. Rouse PC, Biddle SJ. An ecological momentary assessment of the physical activity and sedentary behaviour patterns of university students. Health Educ J. 2010;69(1):116–25. https://doi.org/10.1177/0017896910363145 [Google Scholar]
- 17. Steen O, Prebtani AP. Physical activity patterns among resident and staff physicians in Hamilton teaching hospitals. Can J Gen Int Med. 2015;10(1):29–33 [Google Scholar]
- 18. Chevan J, Haskvitz EM. Do as I do: exercise habits of physical therapists, physical therapist assistants, and student physical therapists. Phys Ther. 2010;90(5):726–34. https://doi.org/10.2522/ptj.20090112. Medline:20299411 [DOI] [PubMed] [Google Scholar]
- 19. Lovell GP, El Ansari W, Parker JK. Perceived exercise benefits and barriers of non-exercising female university students in the United Kingdom. Int J Environ Res Public Health. 2010;7(3):784–98. https://doi.org/10.3390/ijerph7030784. Medline:20617003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Martínez-Lemos RI, Puig-Ribera AM, García-García O. Perceived barriers to physical activity and related factors in Spanish university students. Open J Prev Med. 2014;4(4):164–74. https://doi.org/10.4236/ojpm.2014.44022 [Google Scholar]
- 21. Deliens T, Deforche B, De Bourdeaudhuij I, et al. . Determinants of physical activity and sedentary behaviour in university students: a qualitative study using focus group discussions. BMC Public Health. 2015;15:201 https://doi.org/10.1186/s12889-015-1553-4. Medline:25881120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dean E. Physical therapy in the 21st century (part I): toward practice informed by epidemiology and the crisis of lifestyle conditions. Physiother Theory Pract. 2009;25(5-6):330–53. https://doi.org/10.1080/09593980802668027. Medline:19842862 [DOI] [PubMed] [Google Scholar]
- 23. Shirley D, van der Ploeg HP, Bauman AE. Physical activity promotion in the physical therapy setting: perspectives from practitioners and students. Phys Ther. 2010;90(9):1311–22. https://doi.org/10.2522/ptj.20090383. Medline:20651009 [DOI] [PubMed] [Google Scholar]
- 24. Nair JM, Nemeth LS, Sommers M, et al. . Alcohol use, misuse, and abuse among nursing students: a photovoice study. J Addict Nurs. 2016;27(1):12–23. https://doi.org/10.1097/JAN.0000000000000107. Medline:26950838 [DOI] [PubMed] [Google Scholar]
- 25. Minkler M, Wallerstein N. Community based participatory research for health. San Francisco: Jossey-Bass; 2003. [Google Scholar]
- 26. Wang C, Burris MA. Photovoice: concept, methodology, and use for participatory needs assessment. Health Educ Behav. 1997;24(3):369–87. https://doi.org/10.1177/109019819702400309. Medline:9158980 [DOI] [PubMed] [Google Scholar]
- 27. Murphy SL. Review of physical activity measurement using accelerometers in older adults: considerations for research design and conduct. Prev Med. 2009;48(2):108–14. https://doi.org/10.1016/j.ypmed.2008.12.001. Medline:19111780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ayabe M, Kumahara H, Morimura K, et al. . Epoch length and the physical activity bout analysis: an accelerometry research issue. BMC Res Notes. 2013;6:20 https://doi.org/10.1186/1756-0500-6-20. Medline:23331772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Troiano RP, Berrigan D, Dodd KW, et al. . Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. https://doi.org/10.1249/mss.0b013e31815a51b3. Medline:18091006 [DOI] [PubMed] [Google Scholar]
- 30. Garcia AC, Sykes L, Matthews J, et al. . Perceived facilitators of and barriers to healthful eating among university students. Can J Diet Pract Res. 2010;71(2):e28–33. https://doi.org/10.3148/71.2.2010.69. Medline:20525417 [DOI] [PubMed] [Google Scholar]
- 31. Seitz CM, Strack RW, Rice R, et al. . Using the photovoice method to advocate for change to a campus smoking policy. J Am Coll Health. 2012;60(7):537–40. https://doi.org/10.1080/07448481.2012.688781. Medline:23002802 [DOI] [PubMed] [Google Scholar]
- 32. Richard L, Gauvin L, Raine K. Ecological models revisited: their uses and evolution in health promotion over two decades. Annu Rev Public Health. 2011;32(1):307–26. https://doi.org/10.1146/annurev-publhealth-031210-101141. Medline:21219155 [DOI] [PubMed] [Google Scholar]
- 33. ParticipACTION Advisory Groups. Active Canada 20/20: a physical activity strategy & change agenda for Canada, creating a culture of an active nation [Internet]. Consultation draft Toronto: The Groups; 2011. [cited 2016 Mar 25]. Available from: http://sportbc.com/files/Active-Canada-2020-E.pdf [Google Scholar]
- 34. Gómez-López M, Gallegos AG, Extremera AB. Perceived barriers by university students in the practice of physical activities. J Sports Sci Med. 2010;9(3):374–81. Medline:24149629 [PMC free article] [PubMed] [Google Scholar]
- 35. Buckworth J, Nigg C. Physical activity, exercise, and sedentary behavior in college students. J Am Coll Health. 2004;53(1):28–34. https://doi.org/10.3200/JACH.53.1.28-34. Medline:15266727 [DOI] [PubMed] [Google Scholar]
- 36. Irwin JD. Prevalence of university students' sufficient physical activity: a systematic review. Percept Mot Skills. 2004;98(3 Pt 1):927–43. https://doi.org/10.2466/pms.98.3.927-943. Medline:15209309 [DOI] [PubMed] [Google Scholar]
- 37. Fountaine CJ, Liguori GA, Mozumdar A, et al. . Physical activity and screen time sedentary behaviors in college students. Int J Exerc Sci. 2011;4(2):102–12 [Google Scholar]
- 38. Neuhaus M, Eakin EG, Straker L, et al. . Reducing occupational sedentary time: a systematic review and meta-analysis of evidence on activity-permissive workstations. Obes Rev. 2014;15(10):822–38. https://doi.org/10.1111/obr.12201. Medline:25040784 [DOI] [PubMed] [Google Scholar]
- 39. Stanford FC, Durkin MW, Stallworth JR, et al. . Comparison of physical activity levels in physicians and medical students with the general adult population of the United States. Phys Sportsmed. 2013;41(4):86–92. https://doi.org/10.3810/psm.2013.11.2039. Medline:24231600 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement 1


