Abstract
Background
Intervention fidelity and participant-level variables, such as negative attitudes towards condoms, are important variables to consider in the successful implementation of evidence-based HIV prevention interventions. Mujer Segura is an intervention that has been shown to be efficacious at reducing condomless sex for female sex workers (FSWs) in Mexico (1).
Purpose
We examined main effects of fidelity, negative condom attitudes, and their interaction on the effectiveness of the Mujer Segura intervention at reducing condomless sex at intervention follow-up.
Methods
528 FSWs recruited from 13 cities across Mexico participated in the Mujer Segura intervention. We measured negative condom attitudes at baseline (comprising of beliefs and outcome evaluations), and condomless sex with clients at baseline and 6 month follow-up. Fidelity was measured by a fidelity checklist completed by independent raters; the sum of potentially 43 total elements completed by the counselor constituted fidelity.
Results
Complete fidelity was found in only 15.1% (n=73) of sessions. There was no significant main effect of intervention fidelity on condomless sex with clients at follow-up. There was a significant and positive main effect of negative condom attitudes, and a significant two-way interaction. At lower levels of fidelity, negative condom attitudes predicted greater condomless sex acts, whereas at higher levels of fidelity, the effect of condom attitudes became weaker. The results also indicated that the interaction between negative condom attitudes and fidelity were driven primarily by negative condom beliefs, as opposed to negative condom outcome evaluations.
Conclusions
Ensuring treatment fidelity in an HIV prevention intervention is particularly important when participants have negative attitudes towards condoms.
Compared to HIV prevention research focused on the development and evaluation of interventions designed to reduce risks for HIV, there is a dearth of science on the implementation of evidence-based HIV interventions (2). Whereas having rigorous control over study activities is a primary concern in efficacy trials, treatment fidelity is a primary concern in implementation studies (3,4). In order to achieve maximum effectiveness in community-based settings, an intervention must be implemented with high levels of fidelity (5). That is, the delivery of the intervention must be adhered to as prescribed by the intervention developer to include the necessary elements, or the critical features of the intervention’s intent and design, which are thought to be responsible for its effectiveness.
Previous research has focused on testing the role of distal community and organizational factors in fidelity (3,6). Less is known about how or whether participant-related factors also play a role in affecting fidelity and outcomes. One key participant-factor in studying health behavior change is attitudes towards the behavior. According to theories on health behavior change, including the Theory of Reasoned Action (7,8), attitudes towards a behavior are comprised of one’s beliefs about the outcome of the behavior and one’s evaluations of the outcome. More positive attitudes towards the behavior are more likely to predict behavior change. Support for the theory, including the particular notion that attitudes predict behavior, has been found in condom use research, and in condom use research with female sex workers (9–12).
As a population that remains among the highest at risk for HIV, female sex workers (FSWs) are a critical population for whom to target interventions as well as fidelity research. FSWs have reported that sex without condoms may at times be seen as more preferable than using a condom, since male clients will often pay more for condomless sex (13). In addition, many FSWs believe that condoms cause a man to lose his erection and make sex less enjoyable (14). Overall, FSWs from different parts of the world report negative condom attitudes (15–18). Unless adequately addressed by an intervention, holding negative attitudes towards condoms should make it less likely for FSWs to demonstrate behavior change. Therefore, fidelity may play a critical role particularly for those participants who report more negative attitudes towards condoms.
In 2004 to 2006 we tested the efficacy of a brief behavioral intervention promoting condom use with 924 FSWs in two Mexican cities along the southeastern U.S. border (1). Participants were randomized to receive individualized counseling from either the active intervention, called Mujer Segura (“Healthy Woman”) which used motivational interviewing and behavior change principles (e.g., Theory of Reasoned Action) to increase condom use with clients, or a time-equivalent didactic control condition. At six month follow-up, compared to those in the didactic control condition, participants in Mujer Segura demonstrated significant decreases in the total number of condomless sex acts and STI incidence.
In the current study, we examine the interaction between negative attitudes towards condoms and intervention fidelity in impacting condomless sex among FSWs who participated in the Mujer Segura intervention across 13 cities in Mexico. We hypothesized that when elements of the intervention are more likely to be missed by the counselor (i.e., lower fidelity), participants who report greater negative condom attitudes at baseline will fail to demonstrate behavior change at follow-up. Specifically, for FSWs who report greater negative condom attitudes, those who receive fewer elements of the intervention (lower fidelity) should report more condomless sex with clients at follow-up compared to FSWs who receive more elements of the intervention (higher fidelity).
Method
Recruitment and Implementation Model
Participants were 558 FSWs recruited in 13 study sites across eight states in Mexico. Participants within sites were randomized into the intervention arm of Mujer Segura or the control condition. Each site was a local clinic of the Mexican Foundation for Family Planning (MexFam), a community based organization (CBO) that provides sexual health and women’s reproductive health services. To be included in the study, participants had to be biologically female, at least 18 years of age, self-identify as an FSW, report having traded sex for drugs, money, shelter or other material benefit in the previous 2 months, have had condomless vaginal or anal sex with a client at least once during the previous 2 months, have no previous HIV-positive test result, and agree to be tested for HIV and STIs at baseline and six-month follow-up. Time-location sampling was used to recruit participants (18,19,20,21). Interested participants were referred to the MexFam clinic where they completed a screening interview.
As described elsewhere (22), the implementation model used was the “train-the-trainer” approach. Specifically, an internal trainer from each of the 13 sites/CBOs received intensive training from the intervention developers and from counselors who delivered Mujer Segura in the efficacy study (1). Then, the internal trainer trained other CBO staff to be counselors.
Procedure
Eligible participants were scheduled for a two-hour baseline session, which included the consent procedure, a face-to-face interview, and our 30-minute Mujer Segura sexual risk reduction counseling or a time-equivalent control condition (1). All assessments and counseling took place at the clinic sites. The baseline interview, which was used with over 1000 Mexican FSWs in our previous studies, took 30 minutes to complete. The survey had previously been translated into Spanish and back-translated into English. Interviews were conducted by trained outreach workers using computer-assisted personal interviewing (CAPI, NOVA software, MD, USA). All study measures were approved by ethical review boards for human subjects research at the University of California, San Diego and the Mexican Foundation for Family Planning. FSWs were reimbursed $60 USD total or its equivalent for completing baseline ($30) and for completing the six-month follow-up ($30) interview.
Measures
Sociodemographics
Participants were asked about their age, education, marital status, children, whether sex work is their main source of income, and years employed as a sex worker.
Negative condom attitudes
Participants completed scales on their beliefs about the outcome of using condoms and their evaluation of using condoms. In line with the Theory of Reasoned Action, beliefs and evaluations comprise attitudes towards the behavior. For beliefs, participants responded to three items: “I believe that condoms interfere with sexual pleasure;” “I believe that stopping to put on a condom ruins the moment;” and “Using a condom will feel unnatural.” Response choices were 1=strongly disagree, 2=disagree, 3=agree, 4=strongly agree. The items were aggregated to create a sum score with higher values indicating more negative beliefs towards using condoms (α = 0.72). For evaluation, participants responded to three items: “My always using condoms during vaginal intercourse with my clients during the next month would be…;” “My always using condoms during anal intercourse with my clients during the next month would be…;” and “My always using condoms or dental dam for oral sex with my clients during the next month would be…” Response choices ranged from 1=very bad to 3=neither good nor bad to 5=very good. Items were reverse coded and aggregated to create a sum score with higher values indicating more negative evaluations of using condoms with clients (α = 0.89). The two scales were z-scored then averaged to create the variable “negative condom attitudes” with higher scores indicating greater negative condom attitudes.
Condomless sex
In an open format participants were asked how many times they had vaginal and anal sex (in separate questions) with regular and non-regular (in separate questions) male clients in the past month, and how many times they used a condom for vaginal and anal sex (in separate questions) with regular and non-regular (in separate questions) male clients in the past month. For the purpose of this paper, we were only interested in the entire sum of condomless vaginal and anal sex acts with regular and non-regular clients. We took the difference for each type of sex act to compute condomless sex, and then created a sum score for the outcome variable “total condomless vaginal and anal sex acts with clients in the past month.”
Fidelity
Raters listened to recordings of counseling sessions and completed a fidelity checklist to indicate which and how many of the 43 total intervention elements were completed by the counselor (Range = 4 to 43). This variable was positively skewed (−2.03, SE=0.11), with at least 39 (90.7%) elements completed in 54.2% of sessions. Complete fidelity was found in 15.1% (n=73) of sessions. In our analyses, we used fidelity as a continuous variable (number of intervention elements completed by the counselor).
Current Sample
A total of 529 (94.8%) FSWs completed the follow-up assessment. All but one completed the items assessing sexual risk behavior at follow-up. In terms of fidelity, 483 (91.5%) sessions were rated and used in analyses.
We tested whether the FSWs who participated in sessions that were not rated for fidelity differed from those included in the present analyses on negative condom attitudes and on condomless sex with clients at baseline and follow-up (controlling for site clustering). FSWs in sessions that were not rated and were not included in the present analyses reported significantly less condomless sex at baseline than the analyzed FSWs (B = −0.35, χ2 = 8.88, 95% CI −0.58 to −0.12, p = 0.003). There were no differences between analyzed and not rated sessions on condomless sex at follow-up (controlling for condomless sex at baseline; B = −0.01, χ2 = 0.27, 95% CI −0.05 to 0.03, p = 0.60), or negative condom attitudes (B = −0.06, χ2 = 0.36, 95% CI −0.27 to 0.15, p = 0.55). Thus, participants included in the present analyses did not differ in their negative condom attitudes or behavior change in response to the intervention from participants in sessions that were not rated. However, participants in sessions that were not rated reported less condomless sex at baseline.
Data Analysis
We examined sample characteristics on sociodemographic variables. To test our hypothesis that fidelity interacted with negative condom attitudes to predict condomless sex with clients, we modeled the data using generalized estimating equations (GEE). GEE allows us to adjust for site clustering, and appropriately model the distribution of the outcome. We conducted GEE to predict condomless vaginal and anal sex acts with clients at follow-up using a negative binomial distribution and log link function. We specified an exchangeable covariance structure and controlled for condomless sex with clients at baseline, as well as all possible two-way and three-way interactions. We also entered main effects of age, years of education, marital status, having any children, and number of years employed as a sex worker as covariates. Because the two subscales assessing negative condom attitudes were weakly correlated (r=.26) at baseline, we conducted separate models for each of the condom attitudes sub-scales (i.e., beliefs and evaluations).
Results
The mean age was 33.34 years (SD = 9.55). Participants had completed an average of 7.10 years of education (SD=3.25), 26.1% were married, 89.2% had children, and almost all (97.5%) reported that sex work was their main source of income. The average number of years employed as a sex worker was 6.70, with wide variation (SD=6.92). The mean total of condomless sex acts with clients at follow-up was 5.55 (SD = 10.99), and the mean of negative condom attitudes was .005 (SD = 0.78).
Results from the GEE models are summarized in Table 1. None of the sociodemographic covariates was statistically significant. There were no significant main effects of baseline condomless sex or intervention fidelity on condomless sex with clients at follow-up. Negative condom attitudes were significant and positively predictive of condomless sex with clients at follow-up. As hypothesized, the interaction between fidelity and negative condom attitudes was statistically significant. This interaction is displayed in Figure 1. At lower levels of fidelity, negative condom attitudes predict greater condomless sex acts, whereas at higher levels of fidelity, the effect of condom attitudes became weaker. We conducted a post-hoc analysis to test the slope for those achieving 100% fidelity. There was no effect of negative condom attitudes on condomless sex with FSWs who received the intervention with 100% fidelity (B = −0.19, Wald χ2 = 0.19, 95% CI −1.06 to 0.67, p = 0.66). The results also indicate that the interaction between negative condom attitudes and fidelity were driven primarily by beliefs, as opposed to outcome evaluations of condom use (rightmost columns of Table 1).
Table 1.
Model results predicting condomless sex with clients at follow-up (among female sex workers participating in Mujer Segura in 13 cities across Mexico, n=483)
| Model Parameter | Combined (Beliefs and Evaluations) Attitudes Measure | Beliefs (Only) Measure | Evaluations (Only) Measure | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| B | Wald χ2 | 95% CI | B | Wald χ2 | 95% CI | B | Wald χ2 | 95% CI | |
| Main Effects | |||||||||
| Condomless sex with clients reported at baseline | −.02 | .16 | −.14, .10 | −.01 | .05 | −.07, .06 | −.03 | .29 | −.13, .08 |
| Negative condom attitudes | 2.02 | 19.52*** | 1.12, 2.91 | 1.67 | 7.40 ** | 0.47, 2.87 | .68 | 6.58 ** | .16, 1.19 |
| Intervention fidelity | .01 | .12 | −.02, .03 | .00 | .055 | −.03, .04 | .00 | .00 | .01, .00 |
| Two-Way Interaction Effects | |||||||||
| Baseline condomless sex × Negative condom attitudes | −.10 | 3.48 | −.20, .01 | −.08 | 8.82 ** | −.14, −.03 | −.05 | .93 | −.15, .05 |
| Baseline condomless sex × Intervention fidelity | .00 | .21 | −.00, .00 | .00 | .11 | −.00, .00 | .00 | .39 | −.00, .00 |
| Negative condom attitudes × Intervention fidelity | −.05 | 11.24 *** | −.07, −.02 | −.04 | 5.26 * | −.07, −.01 | −.01 | 2.52 | −.03, .00 |
| Three-Way Interaction Effect | |||||||||
| Baseline condomless sex × Negative condom attitudes × Intervention Fidelity | .00 | 2.74 | .00, .01 | .00 | 7.06** | .00, .00 | .00 | .54 | −.00, .00 |
Notes: Results from models using generalized estimating equations to control for site clustering; age, years of education, marital status, having any children, and years employed as a FSW were entered as control variables (none were statistically significant in the model);
p < .001,
p < .01,
p < .05
Figure 1.
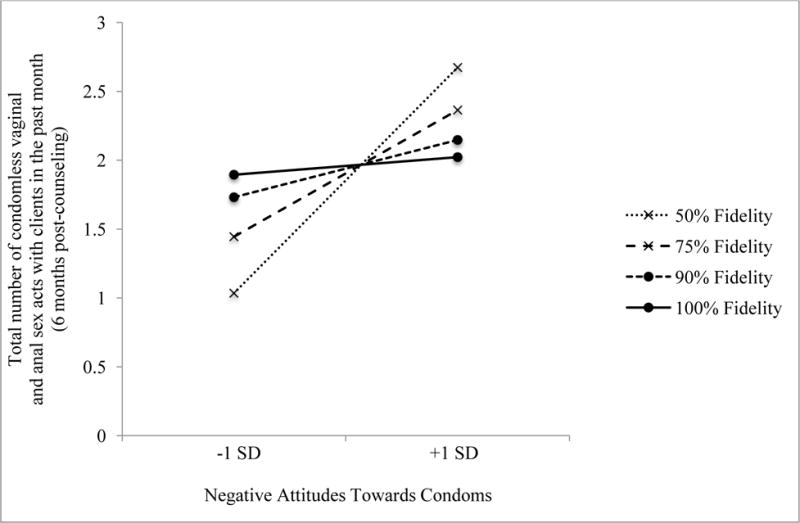
Predicted values of condomless sex at follow-up by the interaction effect between baseline negative condom attitudes and fidelity
We also conducted sensitivity analyses to examine whether there is a critical level of fidelity at which the interaction is no longer statistically significant. Our results show a significant interaction between attitudes towards condoms and fidelity when fidelity was dichotomized as higher (completing all 43 intervention elements) vs lower (less than complete fidelity; completing 42 or fewer elements). We found that the results stayed consistent (i.e., the interaction effect between attitudes towards condoms and fidelity remained statistically significant at p < .05) when those in the “higher fidelity” category included those who completed at least 39, 40, 41, 42, or all 43 elements (in separate analyses). However, once the “higher fidelity” category included those who completed at least 38 elements, the interaction effect became non-significant. This suggests that the finding applies to those whose counselor achieved at last 90% fidelity (i.e., completing at least 39 out of 43 elements). In sum, our finding is not limited to only those who miss one or more intervention element(s); the finding may extend to those who miss no more than 10% of the intervention elements (achieve at least 90% fidelity).
Discussion
In this study we examined negative condom attitudes and fidelity in the implementation of an evidence-based HIV prevention intervention for FSWs. We hypothesized that when there is lower fidelity (i.e., when more elements of the intervention are missed by the counselor) participants who report greater negative condom attitudes at baseline will fail to demonstrate behavior change at follow-up. As predicted, we found that greater negative condom attitudes at baseline predicted more condomless sex with clients at follow-up among FSWs who received fewer components of the intervention (lower fidelity), compared to FSWs in interventions achieving greater fidelity.
The findings of this study suggest that it is important to take participant factors, like attitudes towards the behavior, into account when examining fidelity and outcomes in implementation research. FSWs who reported greater negative condom attitudes at baseline reported more condomless sex acts with clients at follow-up when fidelity was lower. In contrast, in sessions in which more of the elements of the intervention were received by the participant (greater fidelity), negative condom attitudes was not significantly associated with condomless sex. The data suggest that negative condom attitudes should not play a role in affecting outcomes so long as the intervention counselor achieves at least 90% fidelity.
Complete fidelity (all 43 elements completed) occurred in 15% of the sample and more than half of the sessions achieved at least 90% fidelity. The implementation model used for this study was the “train-the-trainer” approach. To achieve high fidelity across all sessions, more training may be needed for all counselors or ongoing consultation or coaching in the model (23,24). Future research might also examine self- and/or outside monitoring of fidelity and feedback in real time for sessions in which the participant reports being unready to change. This is consistent with calls for “personalized medicine” that focus on unique characteristics of patients in the delivery of health interventions (25).
Our results suggest that when a counselor is less adherent, a variable such as negative condom attitudes is able to negatively affect outcomes. Although we found an interaction effect between condom attitudes and fidelity, the variables might also be related in a mediation process that should be investigated in future research. In their conceptual model of implementation fidelity, Carroll and colleagues hypothesized that participant responsiveness predicts fidelity, such that when a participant appears unresponsive or has low interest in the intervention, the counselor will be more likely to skip or miss items, leading to lower fidelity and poorer outcomes (4). Under this hypothesis, it might have been possible that when a FSW began to discuss her negative beliefs and evaluations of using condoms, the counselor may have been more likely to skip intervention elements, which in turn may lead to negative intervention outcomes.
The results of this study should be interpreted in light of the limitations. The FSWs in this study were recruited in Mexico and were all Hispanic, and therefore we are unable to generalize the findings to FSWS in other regions and cultures. As described, we are unable to tease apart the direction of the relationship between negative condom attitudes and fidelity. Further, our measure of fidelity was not able to capture some important nuances of fidelity, including not merely whether the counselor completed intervention elements, but also how well he or she did so. The measure of negative condom attitudes has been used in our previous research with the same population (1), but has not been fully evaluated in terms of its psychometric properties. The data suggest that the results were driven by beliefs about condom use affecting pleasure and the sexual experience, and not by outcome evaluations. These types of beliefs are thus critical to address in condom use interventions. Future intervention research should also examine whether constructs like motivation and behavioral intentions also interact with fidelity to affect outcomes. Not all counseling sessions were recorded and rated, and FSWs tended to report safer sex behaviors in sessions that were not rated. Therefore the results may be limited to FSWs who report higher sex risk behavior. Despite these limitations, the current study sheds important light on HIV intervention implementation research, showing that it is necessary to also consider beliefs about the targeted behavior when studying fidelity and overall effectiveness.
Acknowledgments
Funding: This study was funded by the National Institute of Mental Health (grant number R01 MH087054, T. L. Patterson, P.I.). In addition, preparation of the manuscript was supported by a career development award to the first author from the National Institute on Drug Abuse (K01 DA036447, E. V. Pitpitan, P.I.).
Footnotes
Conflct of Interest: the authors declare that they have no conflicts of interest.
Compliance with Ethical Standards: All procedures involving human participants, including the informed consent process, were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all individual participants included in the study.
References
- 1.Patterson TL, Mausbach B, Lozada R, Staines-Orozco H, Semple SJ, Fraga-Vallejo M, et al. Efficacy of a brief behavioral intervention to promote condom use among female sex workers in Tijuana and Ciudad Juarez, Mexico. Am J Public Health. 2008 Nov;98(11):2051–7. doi: 10.2105/AJPH.2007.130096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelly JA, Heckman TG, Stevenson LY, Williams PN, Ertl T, Hays RB, et al. Transfer of research-based HIV prevention interventions to community service providers: fidelity and adaptation. AIDS Educ Prev Off Publ Int Soc AIDS Educ. 1999;12(5 Suppl):87–98. [PubMed] [Google Scholar]
- 3.Durlak JA, DuPre EP. Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol. 2008;41(3–4):327–350. doi: 10.1007/s10464-008-9165-0. [DOI] [PubMed] [Google Scholar]
- 4.Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci. 2007;2(1):40. doi: 10.1186/1748-5908-2-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moving From the Lab to the Field: The Role of Fidelity and Achieved Relative Intervention Strength. Journal of Research on Educational Effectiveness. 2(1) [Internet]. [cited 2015 Jul, 22]. Available from: http://www.tandfonline.com/doi/abs/10.1080/19345740802539325#.Va_VbrczDSe. [Google Scholar]
- 6.Castro FG, Barrera M, Jr, Martinez CR., Jr The cultural adaptation of prevention interventions: Resolving tensions between fidelity and fit. Prev Sci. 2004;5(1):41–45. doi: 10.1023/b:prev.0000013980.12412.cd. [DOI] [PubMed] [Google Scholar]
- 7.Fishbein M. A theory of reasoned action: some applications and implications. 1979 [cited 2016 Mar 28]; Available from: http://psycnet.apa.org/psycinfo/1982-21121-001. [PubMed]
- 8.Fishbein M, Ajzen I. Belief, attitude, intention and behaviour: An introduction to theory and research. Addison-Wesley; 1975. [Google Scholar]
- 9.Albarracin D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: a meta-analysis. Psychol Bull. 2001;127(1):142. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Predictors of Sexual Intercourse and Condom Use Intentions A… : Nursing Research [Internet] LWW. [cited 2016 Mar 28]. Available from: http://journals.lww.com/nursingresearchonline/Fulltext/2004/05000/Predictors_of_Sexual_Intercourse_and_Condom_Use.4.aspx.
- 11.Gu J, Lau JTF, Chen X, Liu C, Liu J, Chen H, et al. Using the theory of planned behavior to investigate condom use behaviors among female injecting drug users who are also sex workers in China. AIDS Care. 2009;21(8):967–75. doi: 10.1080/09540120802657548. [DOI] [PubMed] [Google Scholar]
- 12.Jamner S, Wolitski RJ, Corby NH, Fishbein M. Using the theory of planned behavior to predict intention to use condoms among female sex workers Margaret. Psychol Health. 1998;13(2):187–205. [Google Scholar]
- 13.Strathdee SA, Lozada R, Semple SJ, Orozovich P, Pu M, Staines-Orozco H, et al. Characteristics of female sex workers with US clients in two Mexico-US border cities. Sex Transm Dis. 2008 Mar;35(3):263–8. doi: 10.1097/OLQ.0b013e31815b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morisky DE, Tiglao TV, Sneed CD, Tempongko SB, Baltazar JC, Detels R, et al. The effects of establishment practices, knowledge and attitudes on condom use among Filipina sex workers. AIDS Care. 1998 Apr;10(2):213–20. doi: 10.1080/09540129850124460. [DOI] [PubMed] [Google Scholar]
- 15.Morisky DE, Stein JA, Chiao C, Ksobiech K, Malow R. Impact of a social influence intervention on condom use and sexually transmitted infections among establishment-based female sex workers in the Philippines: A multilevel analysis. Health Psychol. 2006;25(5):595–603. doi: 10.1037/0278-6133.25.5.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basuki E, Wolffers I, Devillé W, Erlaini N, et al. Reasons for not using condoms among female sex workers in Indonesia. AIDS Educ Prev. 2002;14(2):102. doi: 10.1521/aeap.14.2.102.23901. [DOI] [PubMed] [Google Scholar]
- 17.Yang H, Li X, Stanton B, Fang X, Zhao R, Dong B, et al. Condom use among female sex workers in China: role of gatekeepers. Sex Transm Dis. 2005;32(9):572. doi: 10.1097/01.olq.0000175418.48665.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bucardo J, Semple SJ, Fraga-Vallejo M, Davila W, Patterson TL. A qualitative exploration of female sex work in Tijuana, Mexico. Arch Sex Behav. 2004 Aug;33(4):343–51. doi: 10.1023/B:ASEB.0000028887.96873.f3. [DOI] [PubMed] [Google Scholar]
- 19.Pawa D, Firestone R, Ratchasi S, Dowling O, Jittakoat Y, Duke A, et al. Reducing HIV risk among transgender women in Thailand: a quasi-experimental evaluation of the sisters program. 2013 doi: 10.1371/journal.pone.0077113. [cited 2015 Jun 11]; Available from: http://dx.plos.org/10.1371/journal.pone.0077113. [DOI] [PMC free article] [PubMed]
- 20.Yadav G, Saskin R, Ngugi E, Kimani J, Keli F, Fonck K, et al. Associations of sexual risk taking among Kenyan female sex workers after enrollment in an HIV-1 prevention trial. J Acquir Immune Defic Syndr 1999. 2005 Mar 1;38(3):329–34. [PubMed] [Google Scholar]
- 21.Strathdee SA, Abramovitz D, Lozada R, Martinez G, Rangel MG, Vera A, et al. Reductions in HIV/STI incidence and sharing of injection equipment among female sex workers who inject drugs: results from a randomized controlled trial. PloS One. 2013;8(6):e65812. doi: 10.1371/journal.pone.0065812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patterson TL, Semple SJ, Chavarin CV, Mendoza DV, Santos LE, Chaffin M, et al. Implementation of an efficacious intervention for high risk women in Mexico: protocol for a multi-site randomized trial with a parallel study of organizational factors. Implement Sci. 2012;7(1):105. doi: 10.1186/1748-5908-7-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chaffin M, Hecht D, Bard D, Silovsky JF, Beasley WH. A Statewide Trial of the SafeCare Home-based Services Model With Parents in Child Protective Services. Pediatrics. 2012 Mar 1;129(3):509–15. doi: 10.1542/peds.2011-1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Webster-Stratton CH, Reid MJ, Marsenich L. Improving therapist fidelity during implementation of evidence-based practices: Incredible years program. Psychiatr Serv Wash DC. 2014 Jun 1;65(6):789–95. doi: 10.1176/appi.ps.201200177. [DOI] [PubMed] [Google Scholar]
- 25.McPhee B, Skinta MD, Paul J, Dilley JW. Single-Session Personalized Cognitive Counseling to Change HIV Risk Behavior Among HIV-Negative Men Who Have Sex With Men: A Two-Part Case Study. Cogn Behav Pract. 2012 May;19(2):328–37. [Google Scholar]


