Abstract
Background
Although Escherichia coli is a common cause of bacterial enteritis in Korea, reports on community-acquired E. coli enteritis in Korean children are scarce. This study aimed to determine the clinical characteristics and pathotype distribution of community-acquired E. coli enteritis diagnosed by a multiplex polymerase chain reaction (PCR) assay in Korean children.
Materials and Methods
The medical records of children aged 18 years or less who were diagnosed with acute gastroenteritis by the attending physician between 2013 and 2016 were retrospectively reviewed. The clinical characteristics of children diagnosed with E. coli enteritis were investigated and compared with those diagnosed with Salmonella enteritis. E. coli and Salmonella infections were diagnosed by a stool PCR assay.
Results
Among 279 children, in whom PCR assays for E. coli and Salmonella spp. were performed, Salmonella enteritis and E. coli enteritis were diagnosed in 43 (15.4%) and 39 (14.0%) children, respectively. Among the 39 children with E. coli enteritis, enteropathogenic E. coli (n=21, 53.8%) and enteroaggregative E. coli (n=15, 38.4%) were the most common causative agents. Empirical antibiotics were administered to 33 (84.6%) children. A total of 31 (79.5%) children developed fever, and 25 (80.6%) of them had the fever for 3 days or less, which resolved a median of 1 day (range 0-3 days) after hospitalization. The most frequent gastrointestinal symptom was diarrhea (n=36, 92.3%). Significantly more children with E. coli enteritis were aged 2 years or less as compared with those with Salmonella enteritis (41.0% vs. 21.9%, P = 0.021). Children with Salmonella enteritis more frequently complained of fever (97.7% vs. 79.5%, P = 0.012), abdominal pain (90.7% vs. 64.1%, P = 0.004), and hematochezia (46.5% vs. 10.3%, P <0.001) than those with E. coli enteritis. Erythrocyte sedimentation rate and C-reactive protein levels were significantly higher in children with Salmonella enteritis than those with E. coli enteritis (P <0.001).
Conclusion
Enteropathogenic E. coli was the most frequent pathotype in Korean children with E. coli enteritis that caused mild clinical symptoms. A stool PCR assay for E. coli may be useful for epidemiological purpose and for an early diagnosis of E. coli enteritis.
Keywords: Escherichia coli, Polymerase chain reaction, Child, Korea
Introduction
Escherichia coli is the major component of the normal intestinal flora; however, some pathogenic strains cause significant infectious diseases, such as gastroenteritis, urinary tract infection, and sepsis/meningitis [1]. Among the diarrheagenic E. coli (DEC) causing gastroenteritis, the enterotoxigenic E. coli (ETEC) is a common cause of traveler's diarrhea in developed countries, while the enteropathogenic E. coli (EPEC) as well as ETEC are common causes of bacterial enteritis among younger children in developing countries [1]. In addition, Shiga toxin-producing E. coli (STEC) causes a severe complication, hemolytic uremic syndrome [1]. In Korea, outbreaks of food poisoning in schools due to enteroaggregative E. coli (EAEC) and ETEC have occurred [2,3]. Nevertheless, most hospitals in Korea performed stool cultures for Salmonella spp. and Shigella spp. to evaluate patients with diarrhea because special media and biochemical methods are required for the identification of DEC in stool samples [4]. Accordingly, the molecular methods for identifying DEC in stool samples were developed [1], and several assays based on the polymerase chain reaction (PCR) test are now available. Moreover, multiplex PCR assays that can simultaneously evaluate several diarrheagenic pathogens including bacteria, viruses, and parasites were developed [5].
In Korea, stool PCR assays were performed in order to detect the presence of DEC [6,7,8,9], which has been the most frequent cause of bacterial enteritis since the 2000s [6,7]. However, the clinical characteristics and the distribution of pathotypes of community-acquired E. coli enteritis have been rarely reported in Korean children [10,11]. In addition, previous studies performed stool PCR assays using stool samples obtained from patients with diarrhea not only caused by acute gastroenteritis (AGE) but also caused by various clinical conditions [8,9,10]. Respiratory tract infections, urinary tract infections, allergic reactions, and some medications as well as AGE can cause acute diarrhea especially in children [12]; therefore, it is very difficult to differentiate between true diarrheagenic pathogens and intestinal colonizers in patients with diarrhea caused by various clinical conditions.
In the present study, the clinical characteristics and pathotype distribution of community-acquired AGE due to DEC diagnosed by a multiplex PCR assay were investigated in Korean children, and only those diagnosed with AGE by the attending physician were included. The results of this study help predict the clinical usefulness of a stool PCR assay in children with community-acquired AGE.
Materials and Methods
1. Patients and study design
Among children aged 18 years or less, who were hospitalized in the Department of Pediatrics, Seoul St. Mary's Hospital, College of Medicine, the Catholic University of Korea between January 2013 and December 2016, those in whom stool PCR assays for DEC and Salmonella spp. were performed were investigated. Among them, children who complained of gastrointestinal (GI) symptoms, such as vomiting, diarrhea, and abdominal pain, with or without fever, and who were diagnosed with AGE by the attending physician were included in the present study, and their medical records were retrospectively reviewed. Children with chronic underlying disorders and those prematurely born were excluded from this study. Those who complained of diarrhea longer than 2 weeks and in whom GI symptoms developed 48 hours after hospitalization were also excluded.
Demographic data including sex and age as well as clinical characteristics including accompanying GI symptoms, fever duration, and results of blood and stool tests were obtained from children diagnosed with E. coli enteritis using the multiplex PCR assay. The information was compared with that of the children diagnosed with Salmonella enteritis.
This study was approved by the Institutional Review Board of Seoul St. Mary's Hospital with waiver for informed consent (Approval No.: KC17RESI0677).
2. Laboratory tests
Stool samples collected from the hospitalized children were immediately transferred to the laboratories, and were kept in 2-8°C. The DNA was extracted from the stool samples using the QIAamp DNA Stool Mini Kit (50) (Qiagen, Germantown, MD, USA). An in-house multiplex PCR assay targeting virulence genes, which were specific for each of the five pathotypes (EAEC, enteroinvasive E. coli [EIEC], EPEC, ETEC, STEC), was performed in accordance with the method introduced by Antikainen et al. [13]. In addition, an in-house PCR assay targeting the invA gene specific for Salmonella spp. was also performed in the same stool sample according to the method reported by Cunningham et al. [14]. Table 1 describes the target genes and sequences of primers for the PCR assay. The PCR assay was considered the goldstandard to diagnose E. coli and Salmonella infections in the present study.
Table 1. Target genes and primer sequences for diarrheagenic Escherichia coli according to pathotypes and Salmonella spp.
| Bacteria | Target genes | Primers (5' to 3') |
|---|---|---|
| Enteropathogenic E. coli | eaeA | F: TCAATGCAGTTCCGTTATCAGTT |
| R: GTAAAGTCCGTTACCCCAACCTG | ||
| escV | F: ATTCTGGCTCTCTTCTTCTTTATGGCTG | |
| R: CGTCCCCTTTTACAAACTTCATCGC | ||
| Shiga toxin-producing E. coli | stx1 | F: CGATGTTACGGTTTGTTACTGTGACAGC |
| R: AATGCCACGCTTCCCAGAATTG | ||
| stx2 | F: GTTTTGACCATCTTCGTCTGATTATTGAG | |
| R: AGCGTAAGGCTTCTGCTGTGAC | ||
| Enteroinvasive E. coli | ipaH | F: GAAAACCCTCCTGGTCCATCAGG |
| R: GCCGGTCAGCCACCCTCTGAGAGTAC | ||
| Enterotoxigenic E. coli | elt | F: GAACAGGAGGTTTCTGCGTTAGGTG |
| R: CTTTCAATGGCTTTTTTTTGGGAGTC | ||
| estIb | F: TGTCTTTTTCACCTTTCGCTC | |
| R: CGGTACAAGCAGGATTACAACAC | ||
| Enteroaggregative E. coli | aggR | F: ACGCAGAGTTGCCTGATAAAG |
| R: AATACAGAATCGTCAGCATCAGC | ||
| Salmonella spp. | invA | F: TGCATAATGCCAGACGAAAGAG |
| R: ATCATTTCTATGTTCGTCATTCCA |
F, forward; R, reverse
3. Statistical analysis
The investigated factors were compared between children with E. coli enteritis and those with Salmonella enteritis using the SPSS 21 program (IBM Corporation, Armonk, NY, USA). Categorical and continuous factors were compared using the chi-square and Mann-Whitney tests, respectively. The statistical significance was defined as a two-tailed P-value <0.05.
Results
1. Characteristics of children with E. coli enteritis
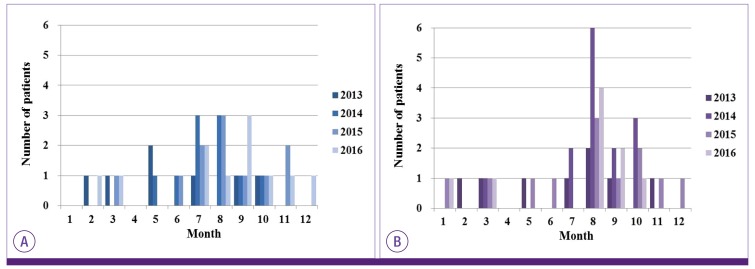
Within the study period, multiplex PCR assays for DEC were performed in 279 children who were diagnosed with AGE. Based on the PCR assay results, Salmonella enteritis and E. coli enteritis were diagnosed in 43 (15.4%) and 39 (14.0%) children, respectively (Table 2). Eight (2.9%) children were positive for Salmonella spp. and E. coli. These eight children were excluded from the comparison between children with Salmonella and E. coli enteritis because they represent the characteristics of both bacterial infections. There was a food-borne outbreak of salmonellosis in a middle school adjacent to our hospital in August 2014; however, any outbreaks of E. coli enteritis were not identified during the study period. Figure 1 shows the yearly and monthly distribution of patients diagnosed with E. coli and Salmonella enteritis.
Table 2. Distribution of bacterial pathogens.
| Pathogen | Age group | Total (n = 82) | |||
|---|---|---|---|---|---|
| 0–2 years (n = 25) | 3–5 years (n = 29) | >5 years (n = 28) | |||
| Salmonella spp. | 9 | 21 | 13 | 43 | |
| Escherichia coli | 16 | 8 | 15 | 39 | |
| EPEC | 11 (68.8) | 4 (50.0) | 4 (26.7) | 19 (48.7) | |
| EAEC | 4 (25.0) | 1 (12.5) | 6 (40.0) | 11 (28.2) | |
| ETEC | 0 | 2 (25.0) | 0 | 2 (5.1) | |
| STEC | 0 | 0 | 1 (6.7) | 1 (2.6) | |
| EIEC | 0 | 0 | 0 | 0 | |
| EPEC + STEC | 1 (6.3) | 0 | 1 (6.7) | 2 (5.1) | |
| EAEC + ETEC | 0 | 1 (12.5) | 1 (6.7) | 2 (5.1) | |
| EAEC + EIEC | 0 | 0 | 2 (13.3) | 2 (5.1) | |
EPEC, enteropathogenic E. coli; EAEC, enteroaggregative E. coli; ETEC, enterotoxigenic E. coli; STEC, Shiga toxin-producing E. coli; EIEC, enteroinvasive E. coli.
Figure 1.
Yeraly and monthly distribution of patients with Escherichia coli (A) and Salmonella enteritis (B)
Thirty-three (84.6%) of the 39 children with E. coli enteritis were infected by a single pathotype, whereas six (15.4%) children were infected by two or more pathotypes (Table 2). Including the co-infected cases, the EPEC (n = 21, 53.8%) was the most frequent E. coli pathotype, followed by the EAEC (n = 15, 38.4%). A total of 28 (71.8%) children were males, and the median age of the enrolled children was 4 years (range: 0-17 years) with 16 (41.0%) children aged 2 years or less (Table 3). Fever developed in 31 (79.5%) children: the median duration of fever was 3 days (range: 1-10 days), and 25 (80.6%) children had a fever for 3 days or less. Diarrhea (n = 36, 92.3%) was the most frequent GI symptom, followed by abdominal pain (n = 25, 64.1%) and vomiting (n = 24, 61.5%). Hematochezia occurred in four (10.3%) children.
Table 3. Characteristics of children with Salmonella enteritis and Escherichia coli enteritis.
| Factor | Salmonella enteritis (n = 43) | Escherichia coli enteritis (n = 39) | P-value | |
|---|---|---|---|---|
| Age group | 0.021 | |||
| 0–2 years | 9 (20.9) | 16 (41.0) | ||
| 3–5 years | 21 (48.8) | 8 (20.5) | ||
| > 5 years | 13 (30.2) | 15 (38.5) | ||
| Sex, male | 19 (44.2) | 28 (71.8) | 0.012 | |
| Other concomitant diagnoses | 5 (11.6) | 2 (5.1) | 0.436 | |
| Accompanying symptoms | ||||
| Fever | 42 (97.7) | 31 (79.5) | 0.012 | |
| Diarrhea | 43 (100.0) | 36 (92.3) | 0.103 | |
| Abdominal pain | 39 (90.7) | 25 (64.1) | 0.004 | |
| Vomiting | 18 (41.9) | 24 (61.5) | 0.075 | |
| Hematochezia | 20 (46.5) | 4 (10.3) | <0.001 | |
| Fever duration | <0.001 | |||
| No fever | 2 (4.7) | 8 (20.5) | ||
| 1–3 days | 17 (39.5) | 25 (64.1) | ||
| ≥4 days | 24 (55.8) | 6 (15.4) | ||
| Concurrent enteral viruses | ||||
| Rotavirusa | 0 (0.0) | 7 (18.9) | 0.005 | |
| Norovirusb | 1 (2.6) | 3 (8.3) | 0.351 | |
| Stool microscopic examinationc | ||||
| White blood cells | 18 (42.9) | 11 (29.7) | 0.227 | |
| Occult blood | 21 (50.0) | 8 (21.6) | 0.009 | |
| Blood tests | ||||
| White blood cell count (/mm3) | 7,440 (4,700–16,940) | 9,350 (1,950–24,520) | 0.061 | |
| Absolute neutrophil count (/mm3) | 4,851 (1,968–12,367) | 6,150 (332–22,313) | 0.134 | |
| Erythrocyte sedimentation rated (mm/hr) | 28 (5–68) | 15 (2–48) | <0.001 | |
| C-reactive proteine (mg/dL) | 5.92 (0.27–26.42) | 1.78 (0.02–10.25) | <0.001 | |
aRotavirus was tested in 39 children with Salmonella enteritis and 37 children with E. coli enteritis.
bNorovirus was tested in 38 children with Salmonella enteritis and 36 children with E. coli enteritis.
cStool microscopic examination was performed in 42 children with Salmonella enteritis and 37 children with E. coli enteritis.
dErythrocyte sedimentation rate was measured in 41 children with Salmonella enteritis and 34 children with E. coli enteritis.
eC-reactive protein levels were measured in 43 children with Salmonella enteritis and 38 children with E. coli enteritis.
Microscopic stool examinations were performed in 37 children: white blood cells (WBCs) were observed in 11 (29.7%) children, while occult blood (OB) was positive in eight (21.6%) children. The rotavirus was identified in seven (17.9%) of the 37 tested children, while norovirus was identified in three (8.3%) of the 36 tested children. Blood tests upon admission revealed the following results: a median WBC count of 9,350/mm3 (range: 1,950-24,520/mm3), a median erythrocyte sedimentation rate (ESR) of 15 mm/hr (range: 2-48 mm/hr) in the 34 children tested, and a median C-reactive protein (CRP) level of 1.78 mg/dL (range: 0.02-10.25 mg/dL) in the 38 children tested.
Empirical antibiotics were administered to 33 (84.6%) children. Aminopenicillin and β-lactamase inhibitor combination (n = 14, 35.9%) was most frequently administered, followed by a third-generation cephalosporin (n = 11, 28.2%). A total of 20 (51.3%) children received aminoglycoside concomitantly with a β-lactam agent. Fever resolved a median of 1 day (range: 0-3 days) after hospitalization.
2. Comparison between children with E. coli and Salmonella enteritis
In the comparison made between 39 children with E. coli enteritis and 43 children with Salmonella enteritis, results showed that those with E. coli enteritis were more likely males (71.8% vs. 44.2%, P = 0.012) and aged 2 years or less (41.0% vs. 21.9%, P = 0.021, Table 3). By contrast, children with Salmonella enteritis more frequently complained of fever (97.7% vs. 79.5%, P = 0.012), abdominal pain (90.7% vs. 64.1%, P = 0.004), and hematochezia (46.5% vs. 10.3%, P < 0.001) than those with E. coli enteritis. Fever lasted for 3 days or less in 84.6% of children with E. coli enteritis; however, it lasted for 4 days or more in 55.8% of children with Salmonella enteritis (P <0.001). Stool OB was more likely positive in children with Salmonella enteritis than those with E. coli enteritis (50.0% vs. 21.6%, P = 0.009). The ESR and CRP levels were significantly higher in children with Salmonella enteritis than those with E. coli enteritis (P < 0.001).
Discussion
In the present study, the clinical characteristics of children diagnosed with E. coli enteritis and the distribution of E. coli pathotypes in those patients were investigated. The EPEC was the most frequent pathotype in Korean children with community-acquired E. coli enteritis, and E. coli enteritis showed milder clinical symptoms than Salmonella enteritis.
The pathotype distribution of DEC in patients with AGE was reported in various geographic areas and showed different distributions according to the participants' age, enrolled countries, and the degree of urbanization in the same country. For example, the ETEC was most common among diarrhea children in seven developing countries in Africa and Asia [15], whereas EPEC was most common in American children [16]. Another study conducted in the other areas of the United States reported EAEC as the most common pathotype in childhood diarrhea [17]. Although EAEC was the most common pathotype in adult and pediatric American patients with diarrhea [18], EPEC was most frequent in Europe [19]. In Nigeria, EPEC was most frequent in the urban areas, ETEC was most common in the rural areas [20], and EPEC was most common in both urban and rural areas in China [21]. In summary, EPEC and EAEC were common pathotypes in developed countries and urbanized areas replacing ETEC. In Korea, ETEC was the most frequent cause of E. coli enteritis in the 1980s [10]; however, EPEC was reported as the most frequent cause in the 2000s [11]. The nationwide surveillance results of the Korean Centers for Disease Control and Prevention showed that EPEC was the most frequent cause of bacterial diarrhea in the 2010s, followed by EAEC [7]. Therefore, a periodical nationwide surveillance for the pathotype distribution of DEC is necessary in each country to identify the changing trend.
The present study showed that children with E. coli enteritis experienced a milder clinical course than those with Salmonella enteritis: the frequencies of GI symptoms and fever were lower, and the fever duration was shorter in children with E. coli enteritis than those with Salmonella enteritis. If we consider that hematochezia occurred significantly more and the ESR and CRP levels increased in children with Salmonella enteritis than in those with E. coli enteritis, E. coli infection should cause weaker GI inflammation than Salmonella infection. Because 25.6% of the children with E. coli enteritis were also positive for rotavirus or norovirus, some types of E. coli may be simple colonizers rather than true GI pathogens, and mild clinical manifestations of E. coli enteritis might represent those of the mixed viral AGE. Actually, the GI colonization of EPEC, the most frequent pathotype in this study, has been previously reported [22]. However, milder clinical manifestations of E. coli enteritis compared with Salmonella enteritis were also previously reported [11,23], and rotavirus or norovirus rather than E. coli could be simple colonizers.
This study showed that the short fever duration in E. coli enteritis could represent its own mild natural clinical course of E. coli enteritis. However, most of the enrolled children received empirical antibiotics that are known to be effective for E. coli infection. Although antibiotic therapy for E. coli enteritis is not routinely recommended, it shortened the clinical course of EPEC, ETEC, and EIEC infections [1,24]. Therefore, the administered antibiotics might shorten the clinical course of E. coli enteritis in our patients. If so, a stool PCR assay for E. coli infection helps the early diagnosis and early improvement of clinical symptoms of E. coli enteritis through early antibiotic therapy. In addition, rapid detection of STEC infection by a PCR assay, in which antibiotic therapy may cause hemolytic uremic syndrome, can prevent the development of severe complications by excluding antibiotic therapy for those cases. In contrast, if we consider that only 14.0% of the children, in whom stool PCR assays were performed, were positive for E. coli, a multiplex PCR assay targeting more GI pathogens including E. coli will be more cost-effective than a PCR assay targeting only E. coli.
This study had some limitations. First, we could not determine a recent diarrhea history prior to the enrollment of participants in this study due to the retrospective study design. Therefore, it was difficult to determine whether the identified enteral viruses represented prolonged excretion caused by previous diarrhea illness. Second, this study included only hospitalized children; therefore, those with milder symptoms were excluded, and the proportion of Salmonella and E. coli infection in AGE children (32.3%) might be overestimated. In addition, Clostridium difficile and Campylobacter spp., which were reported as major GI pathogens [8,16,18,25], were not routinely tested in the enrolled patients. Therefore, the exact epidemiology of bacterial enteritis was not determined in this study. Third, the possibility of EPEC colonization was not absolutely excluded. The pathogenic capacity of EPEC depends on the immune status and age of the infected host, the serotype and genotype of the infected EPEC, and the colony count of infected EPEC [22]. Although this study only included children primarily diagnosed with AGE in order to exclude the role of enteric colonizing E. coli, a quantitative PCR assay and concomitant culture study can be more useful for excluding colonization status.
In conclusion, E. coli caused relatively milder GI manifestations, and EPEC was the most frequent pathotype in Korean children with E. coli enteritis. A stool PCR assay for E. coli is useful in epidemiological studies and helpful in the early diagnosis and improvement of the clinical course of E. coli enteritis.
Footnotes
Conflict of Interest: No conflict of interest.
References
- 1.Nataro JP, Kaper JB. Diarrheagenic Escherichia coli. Clin Microbiol Rev. 1998;11:142–201. doi: 10.1128/cmr.11.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cho SH, Kim J, Oh KH, Hu JK, Seo J, Oh SS, Hur MJ, Choi YH, Youn SK, Chung GT, Choe YJ. Outbreak of enterotoxigenic Escherichia coli O169 enteritis in schoolchildren associated with consumption of kimchi, Republic of Korea, 2012. Epidemiol Infect. 2014;142:616–623. doi: 10.1017/S0950268813001477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shin J, Oh SS, Oh KH, Park JH, Jang EJ, Chung GT, Yoo CK, Bae GR, Cho SH. An outbreak of foodborne illness caused by enteroaggregative Escherichia coli in a high school in South Korea. Jpn J Infect Dis. 2015;68:514–519. doi: 10.7883/yoken.JJID.2014.460. [DOI] [PubMed] [Google Scholar]
- 4.Bennett WE, Jr, Tarr PI. Enteric infections and diagnostic testing. Curr Opin Gastroenterol. 2009;25:1–7. doi: 10.1097/MOG.0b013e32831ba094. [DOI] [PubMed] [Google Scholar]
- 5.Binnicker MJ. Multiplex molecular panels for diagnosis of gastrointestinal infection: performance, result interpretation, and cost-effectiveness. J Clin Microbiol. 2015;53:3723–3728. doi: 10.1128/JCM.02103-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho SH, Shin HH, Choi YH, Park MS, Lee BK. Enteric bacteria isolated from acute diarrheal patients in the Republic of Korea between the year 2004 and 2006. J Microbiol. 2008;46:325–330. doi: 10.1007/s12275-008-0015-4. [DOI] [PubMed] [Google Scholar]
- 7.Kim NO, Cha I, Kim JS, Chung GT, Kang YH, Hong S. The prevalence and characteristics of bacteria causing acute diarrhea in Korea, 2012. Ann Clin Microbiol. 2013;16:174–181. [Google Scholar]
- 8.Lee J, Kim J, Cho H, Oh K, Uh Y, Yoon KJ. Detection of bacterial and viral pathogens in stool specimens using multiplex PCR. J Lab Med Qual Assur. 2015;37:141–147. [Google Scholar]
- 9.Lee S, Park YJ, Lee HK, Kim SY, Kim JY, Lee SY, Yoo JK. Detection of 13 enteric bacteria and 5 viruses causing acute infectious diarrhea using multiplex PCR from direct stool specimens. Ann Clin Microbiol. 2013;16:33–38. [Google Scholar]
- 10.Kim KH, Suh IS, Kim JM, Kim CW, Cho YJ. Etiology of childhood diarrhea in Korea. J Clin Microbiol. 1989;27:1192–1196. doi: 10.1128/jcm.27.6.1192-1196.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang JY, Choi JE, Shin S, Yoon JH. Diagnosis of enteropathogens in children with acute gastroenteritis: one year prospective study in a single hospital. Korean J Pediatr Gastroenterol Nutr. 2006;9:1–13. [Google Scholar]
- 12.Gupta R. Diarrhea. In: Wyllie R, Hyams JS, Kay M, editors. Pediatric gastrointestinal and liver disease. 5th ed. Piladelphia, PA: Elsevier; 2016. pp. 104–114. [Google Scholar]
- 13.Antikainen J, Tarkka E, Haukka K, Siitonen A, Vaara M, Kirveskari J. New 16-plex PCR method for rapid detection of diarrheagenic Escherichia coli directly from stool samples. Eur J Clin Microbiol Infect Dis. 2009;28:899–908. doi: 10.1007/s10096-009-0720-x. [DOI] [PubMed] [Google Scholar]
- 14.Cunningham SA, Sloan LM, Nyre LM, Vetter EA, Mandrekar J, Patel R. Thrre-hour molecular detection of Campylobacter, Salmonella, Yersinia, and Shigella species in feces with accuracy as hish as that of culture. J Clin Microbiol. 2010;48:2929–2933. doi: 10.1128/JCM.00339-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, Wu Y, Sow SO, Sur D, Breiman RF, Faruque AS, Zaidi AK, Saha D, Alonso PL, Tamboura B, Sanogo D, Onwuchekwa U, Manna B, Ramamurthy T, Kanungo S, Ochieng JB, Omore R, Oundo JO, Hossain A, Das SK, Ahmed S, Qureshi S, Quadri F, Adegbola RA, Antonio M, Hossain MJ, Akinsola A, Mandomando I, Nhampossa T, Acácio S, Biswas K, O'Reilly CE, Mintz ED, Berkeley LY, Muhsen K, Sommerfelt H, Robins-Browne RM, Levine MM. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet. 2013;382:209–222. doi: 10.1016/S0140-6736(13)60844-2. [DOI] [PubMed] [Google Scholar]
- 16.Stockmann C, Pavia AT, Graham B, Vaughn M, Crisp R, Poritz MA, Thatcher S, Korgenski EK, Barney T, Daly J, Rogatcheva M. Detection of 23 gastrointestinal pathogens among children who present with diarrhea. J Pediatric Infect Dis Soc. 2017;6:231–238. doi: 10.1093/jpids/piw020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen MB, Nataro JP, Bernstein DI, Hawkins J, Roberts N, Staat MA. Prevalence of diarrheagenic Escherichia coli in acute childhood enteritis: a prospective controlled study. J Pediatr. 2005;146:54–61. doi: 10.1016/j.jpeds.2004.08.059. [DOI] [PubMed] [Google Scholar]
- 18.Nataro JP, Mai V, Johnson J, Blackwelder WC, Heimer R, Tirrell S, Edberg SC, Braden CR, Glenn Morris J, Jr, Hirshon JM. Diarrheagenic Escherichia coli infection in Baltimore, Maryland, and New Haven, Connecticut. Clin Infect Dis. 2006;43:402–407. doi: 10.1086/505867. [DOI] [PubMed] [Google Scholar]
- 19.Spina A, Kerr KG, Cormican M, Barbut F, Eigentler A, Zerva L, Tassios P, Popescu GA, Rafila A, Eerola E, Bastista J, Maass M, Aschbacher R, Olsen KE, Allerberger F. Spectrum of enteropathogens detected by the FilmArray GI Panel in a multicentre study of community-acquired gastroenteritis. Clin Microbiol Infect. 2015;21:719–728. doi: 10.1016/j.cmi.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 20.Ifeanyi CI, Ikeneche NF, Bassey BE, Al-Gallas N, Ben Aissa R, Boudabous A. Diarrheagenic Escherichia coli pathotypes isolated from children with diarrhea in the Federal Capital Territory Abuja, Nigeria. J Infect Dev Ctries. 2015;9:165–174. doi: 10.3855/jidc.5528. [DOI] [PubMed] [Google Scholar]
- 21.Wang X, Wang J, Sun H, Xia S, Duan R, Liang J, Xiao Y, Qiu H, Shan G, Jing H. Etiology of childhood infectious diarrhea in a developed region of China: compared to childhood diarrhea in a developing region and adult diarrhea in a developed region. PLoS One. 2015;10(4):e0142136. doi: 10.1371/journal.pone.0142136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu J, Torres AG. Enteropathogenic Escherichia coli: foe or innocent bystander? Clin Microbiol Infect. 2015;21:729–734. doi: 10.1016/j.cmi.2015.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rathaur VK, Pathania M, Jayara A, Yadav N. Clinical study of acute childhood diarrhoea caused by bacterial enteropathogens. J Clin Diagn Res. 2014;8:PC01–PC05. doi: 10.7860/JCDR/2014/6677.4319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Velarde JJ, Brerry AA, Nataro JP. Diarrhea-causing and dysentery-causing Escherichia coli. In: Cherry J, Demmler-Harrison GJ, Kaplan SL, Steinbach WJ, Hotez P, editors. Feigin and Cherry's textbook of pediatric infectious diseases. 7th ed. Philadelphia, PA: Saunders Elsevier; 2014. pp. 1449–1465. [Google Scholar]
- 25.Fiedoruk K, Daniluk T, Rozkiewicz D, Zaremba ML, Oldak E, Sciepuk M, Leszczynska K. Conventional and molecular methods in the diagnosis of community-acquired diarrhoea in children under 5 years of age from the north-eastern region of Poland. Int J Infect Dis. 2015;37:145–151. doi: 10.1016/j.ijid.2015.06.028. [DOI] [PubMed] [Google Scholar]