Abstract
Purpose
The aim of this study was to identify the most accurate and reliable quantitative radiographic parameters for assessing vertical and horizontal instability in different Rockwood grades of acromioclavicular joint (ACJ) separations. Furthermore, the effect of projectional variation on these parameters was investigated in obtaining lateral Alexander view radiographs.
Methods
A Sawbone model of a scapula with clavicle was mounted on a holding device, and acromioclavicular dislocations as per the Rockwood classification system were simulated with the addition of horizontal posterior displacement. Projectional variations for each injury type were performed by tilting/rotating the Sawbone construct in the coronal, sagittal or axial plane. Radiographic imaging in the form of an anterior–posterior Zanca view and a lateral Alexander view were taken for each injury type and each projectional variation. Five newly defined radiographic parameters for assessing horizontal and vertical displacement as well as commonly used coracoclavicular distance view were measured. Reliability, validity and the effect of projectional variation were investigated for these radiographic measurements.
Results
All radiographic parameters showed excellent intra- and interobserver reliability. The validity was excellent for the acromial centre line to dorsal clavicle (AC–DC) in vertical displacement and for the glenoid centre line to posterior clavicle (GC–PC) in horizontal displacement, whilst the remaining measurements showed moderate validity. For AC–DC and GC–PC, convergent validity expressed strong correlation to the effective distance and discriminant validity demonstrated its ability to differentiate between various grades of ACJ dislocations. The effect of projectional variation increased with the degree of deviation and was maximal (3 mm) for AC–DC in 20° anteverted malpositioning and for GC–PC in 20° retroverted malpositioning.
Conclusions
AC–DC and the GC–PC are two novel quantitative radiographic parameters of vertical and horizontal instability in ACJ dislocations that demonstrate excellent reliability and validity with reasonable inertness to malpositioning. The use of AC–DC for assessing vertical displacement and GC–PC for assessing horizontal displacement in a single Alexander view is recommended to guide the appropriate management of ACJ dislocations. A better appreciation of the degree of horizontal instability, especially in lower Rockwood grades (II, III) of ACJ dislocations, may improve management of these controversial injuries.
Keywords: Acromioclavicular joint, AC joint, AC joint separation, Dislocation, Radiographic parameters, AC–DC, GC–PC, Instability, Horizontal instability, Vertical instability, Intra- and interobserver reliability, Validity, Rockwood classification
Introduction
Acromioclavicular joint (ACJ) dislocations are a common injury in the young active population [1–3]. They are invariably classified as per the Rockwood classification [4]. This system is based on the comparative examination of bilateral anterior–posterior stress radiographs and evaluation of the coracoclavicular (CC) distance relative to the uninjured side. This allows an assessment of vertical instability. Several studies have shown that dynamic instability in the horizontal plane is associated with inferior clinical outcomes [5–7]. Except for Type-4 injuries, the Rockwood classification system does not assess horizontal instability. Furthermore, we do not understand what effect horizontal instability may have on the quantitative assessment of vertical instability. The combined posterior–superior dislocation of the clavicle with respect to the acromion may lead to an unpredictable effect on the radiographic CC distance due to projection—a possible underestimation of the CC distance for example, may inappropriately influence non-operative management of potential high grade injuries.
To our knowledge, there is no reliable way of quantifying both vertical and horizontal instability in ACJ dislocations. The majority of radiographic parameters assessing horizontal instability that have been described in the literature to date are semi quantitative and do not account for the projectional differences that may lead to inaccuracies [8–10]. Several authors have proposed the use of different radiographic views to assess horizontal instability [1, 11, 12]. The Alexander view is one such view [13], but the radiographic projection of the ACJ in these views are very sensitive to subtle differences in anatomical position of the ACJ in the coronal, sagittal and axial planes relative to the radiograph beam. This makes comparative assessment (injured side vs uninjured side) with the use of bilateral Alexander views unreliable.
The aim of this study was to identify novel quantitative radiographic parameters for assessing not only vertical but horizontal instability in different Rockwood grades of ACJ dislocations and to investigate the effect of the projectional variation of these parameters in obtaining Alexander view radiographs. In detail, the study includes (1) the analysis of the reliability for the radiographic parameters, (2) the assessment of the validity compared to effective distance and within injury types and (3) the calculation of deviation within projectional variations.
Materials and methods
Sawbone modelling of ACJ dislocations
A Sawbone model of a scapula with clavicle (Pacific Research Laboratories, Inc., Vashon, WA, USA) was mounted on a specifically designed holding device (Fig. 1). This system allowed precise positioning of the clavicle relative to the acromion in order to simulate ACJ dislocations with both vertical and horizontal displacement. A radiopaque ball was fixed to the lateral border of the acromion along the line of the inferior border of the acromion and the lateral clavicle to allow calibration during radiographic analysis.
Fig. 1.

Sawbone modelling. Specially designed holding device where a Sawbone Model was mounted. This model allows to simulate different ACJ dislocation as well as navigation in axial, sagittal and coronal direction according to measurement protocol
The Sawbone model was then setup to simulate ACJ dislocations as per the Rockwood classification system (Grades I to V) with the addition of horizontal posterior displacement for each injury type (Table 1). The degree of displacement simulated for each type of injury was based on the measurement of the height/width of the clavicle. This measurement was then utilized to simulate the appropriate vertical and horizontal instability for each injury type.
Table 1.
Overview of the seven simulated ACJ dislocations
| Simulated ACJ dislocations according to Rockwood classification | Vertical displacement to superior (%) | Horizontal displacement to posterior (%) |
|---|---|---|
| Control | 0 | 0 |
| RW II-0 | 50 | 0 |
| RW II-25 | 50 | 25 |
| RW III-0 | 100 | 0 |
| RW III-50 | 100 | 50 |
| RW IV-100 | 200 | 100 |
| RW V-200 | 200 | 200 |
Rockwood classification (RW) with vertical displacement served as basis (first column) and was combined with the addition of horizontal displacement for each injury type. The degree of displacements are given in percentage based on the measurement of the height/width of the clavicle (= 100%)
Projectional variations
Projectional variation was simulated for every Rockwood grade of ACJ dislocation. Therefore, the Sawbone construct was tilted in the coronal (medial–lateral) and sagittal (anterior–posterior) planes, and rotated in the axial plane (anteversion-retroversion). The projectional variations for each injury type were simulated with 10° and 20° in any direction, resulting in one neutral position and twelve variations as follows:
Sagittal—Flexion and Extension—+20°/+ 10°/−10°/−20°
Coronal—Abduction and Adduction—+20°/+ 10°/−10°/−20°
Axial—Ante- and Retroversion—+20°/+ 10°/−10°/−20°
Radiographic imaging
Radiographic imaging included computed tomography (CT) scanning and conventional radiography. Once the Sawbone model was setup to simulate a particular Rockwood grade of ACJ dislocation, CT scans were performed on a Siemens Somatom Definition Flash System (Siemens, Erlangen, Germany) with the following scanning parameters: tube voltage 140 kV/; tube current 350mAs; matrix 512 × 512; slice thickness 0.6 mm. Then, a series of radiographs were taken for each injury type with the neutral position and with the simulated projectional variations (Fig. 2). First, an anterior–posterior (AP) Zanca view radiograph [14] was taken with the standardized technique. The radiographic tube to image distance was 120 cm. The central beam was directed to the midpoint of the centre of the glenoid including an angle of 10° cranial tilt of the beam. Second, an lateral Alexander view radiograph [13] focusing on the centre of the glenoid was taken. In total, 2 × 91 radiographs and 7 CT were obtained for further analysis. All images were assigned an identification number in random order and stored in the picture archiving and communications system (PACS).
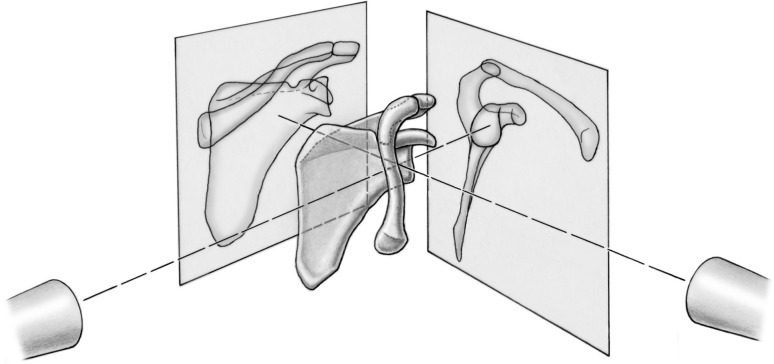
Fig. 2.
Overview of the radiographic imaging. First, an anterior–posterior Zanca view radiograph was taken with the standardized technique and second, a lateral Alexander view radiograph with an angle of 10° cranial tilt of the beam
Radiographic measurements
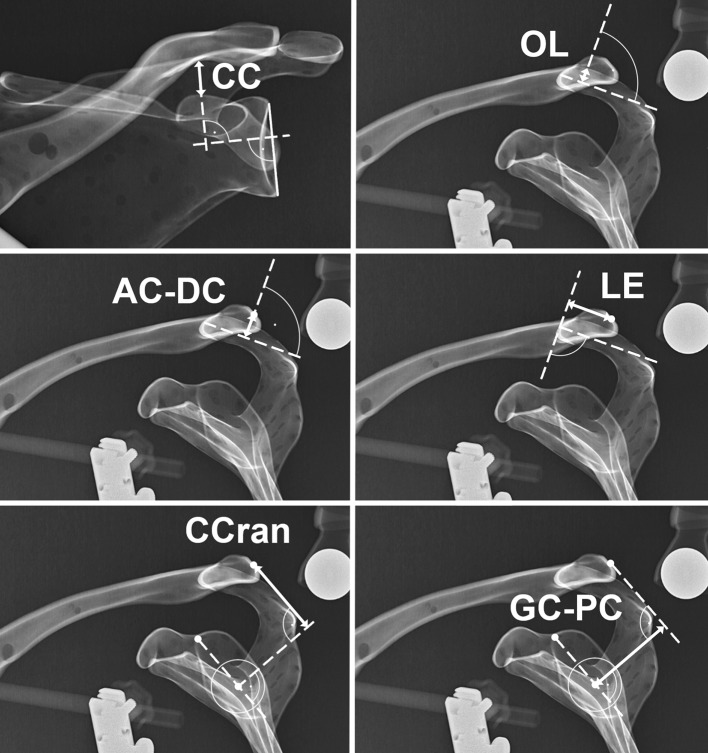
On the AP Zanca view, the commonly used and often published CC distance was measured as the distance between the knee of the coracoid and the inferior cortex of the clavicle for vertical displacement. Five new parameters were defined for radiographic analysis in the lateral Alexander view as shown in Fig. 3. The acromial centre line to dorsal clavicle (AC–DC) and centre cranialization (CCran) for vertical displacement, and maximal overlap (OL) [15], lateral extension (LE) and the glenoid centre line to posterior clavicle (GC–PC) for horizontal displacement.
Fig. 3.
Illustration of the six performed radiographic measurements. On the anterior–posterior Zanca view, coracoclavicular distance (CC) was measured for vertical displacement. On the Alexander view, acromial centre line to dorsal clavicle (AC–DC) and centre cranialization (CCran) were measured for vertical displacement and Maximal Overlap (OL), Lateral Extension (LE) and glenoid centre line to posterior clavicle (GC–PC) for horizontal displacement
The AC–DC was defined as the vertical distance between the mid-acromion level and the midpoint of the lateral clavicle, measured perpendicular to the mid-acromion level. The CCran was defined as vertical distance from the centre of the glenoid circle to the midpoint of the lateral clavicle. A line drawn from the centre of the glenoid circle intersecting through the 12 o’clock position on the glenoid face (posterior base of coracoid) was used as the reference. A line perpendicular to this reference line was then drawn from the centre of the glenoid circle. A parallel line to reference line was drawn from the midpoint of the lateral clavicle. The vertical distance from the midpoint of the lateral clavicle with respect to the perpendicular line from the centre of the glenoid circle was then measured as the vertical displacement.
The GC–PC was analogously measured for posterior displacement. The posterior distance on the perpendicular line from the centre of the glenoid to the parallel line through the midpoint of the lateral clavicle was the posterior displacement of the clavicle with respect to the centre of the glenoid. The OL represents the maximal overlap distance of the lateral clavicle and the acromion, and the LE describes the posterior distance between a perpendicular line to the mid-acromion level and the midpoint of the lateral clavicle. All six radiographic parameters were presented in mm and measured in the PACS with an accuracy of one decimal.
Intra- and interobserver reliability
Intra- and interobserver reliability was assessed using the following radiographs: the neutral rotation radiograph of each grade of ACJ dislocation and additional 4 randomly selected radiographs with 10° tilt/rotation in any direction, resulting in total 35 radiographs. The measurements were taken by three examiners (PS, JW, SR). Each examiner was blinded and independent to the other measurements. One examiner (SR) assessed the measurements two times at an interval of two weeks in order to determine intraobserver reliability.
Validity
Validity was assessed with determination of convergent validity and discriminant validity. Convergent validity occurs when the scales of a measurement correlate as expected with the related scales of another measurement. For this purpose, the radiographic parameters were compared with the effective distances measured on 3-dimensional reconstructions of CT scans for each grade of dislocation. An independent radiologist who was not involved in the study determined the horizontal and vertical distance between the acromion and clavicle. Discriminant validity is the ability to detect relevant differences between different subgroups and is assessed by calculating the effect size between the different injury types.
The study was done in accordance with the Guidelines of Good Clinical Practice. According to the Swiss Human Research Act, this study does not require any IRB approval because neither human beings nor biological material were involved.
Statistical analysis
Results are expressed as a mean with standard deviation (SD) and with 95% confidence interval (95% CI) where appropriate. Inter- and intraobserver reliability was determined by using the two-way random intraclass correlation coefficient (ICC) assuming single measurement and absolute agreement for each radiographic parameter (ICC (2,1)) [16] and presented with a 95% CI. The ICC values were interpreted with use of the classification suggested by Munro [17] with >0.9 indicates very high reliability. For further analysis, the mean of all observers were used. Convergent validity, indicating whether radiographic parameters correlate to effective distance, was determined by using Pearson correlation coefficient r. Correlation coefficient was calculated three times to estimate how rotational deviations influence the result: First calculation with only the perfect projections included (n = 7), second calculation with the additional 10 degrees deviations (n = 49) and third calculation considers all projection deviations (n = 91). The degree of correlation was defined with less than 0.2 equalled poor, 0.2–0.4 low, 0.4–0.6 moderate, 0.6–0.8 good, and >0.8 excellent. Discriminant validity, indicating whether measurements discriminate between the ACJ dislocation groups, was assessed by an independent ANOVA test and the calculation of the effect size with η 2. The sample size to determine the reliability was based on the optimal design for reliability studies as described by Walter et al. [18] Minimum ICC was set at 0.8 and expected at 0.9. With three measurement replicates in 33 samples, a significance level of 0.05 with a power of 80% was obtained. Statistical significance was set as p < 0.05. Statistical data analysis was performed with the use of SPSS (IBM SPSS Statistics for Windows, Version 21.0, Armonk, NY, USA: IBM Corp.) and the use of R: a language and environment for statistical computing (R Core Team, 2016. R Foundation for Statistical Computing, Vienna, Austria).
Results
Reliability
All radiographic parameters showed excellent intra- and interobserver reliability (Table 2).
Table 2.
Reliability and validity results for the six radiographic parameters
| Reliability | Validity | ||||
|---|---|---|---|---|---|
| Intraobserver R. | Interobserver R. | Convergent V. | Discriminant V. | ||
| ICC 2,1 (95% CI) [n = 35, 2 measures] | ICC 2,1 (95% CI) [n = 35, 3 observer] | Pearson’s r [n = 7, neutral] | Pearson’s r [n = 49/91, w/variation] | ES η 2 [n = 91] | |
| Vertical displacement | |||||
| CC | 0.956 (0.712–0.993) | 0.985 (0.928–0.997) | 0.833* | 0.778*/0.706* | 0.743 |
| AC–DC | 0.993 (0.982–0.997) | 0.998 (0.996–1.000) | 0.972* | 0.960*/0.939* | 0.952 |
| CCran | 0.827 (-0.440–0.956) | 0.964 (0.909–0.984) | 0.495 | 0.460*/0.473* | 0.905 |
| Horizontal displacement | |||||
| OL | 0.805 (0.647–0.897) | 0.945 (0.906–0.970) | −0.488 | −0.433*/−0.385* | 0.587 |
| LE | 0.925 (0.855–0.961) | 0.987 (0.977–0.993) | 0.387 | 0.383*/0.346* | 0.713 |
| GC–PC | 0.985 (0.970–0.992) | 0.995 (0.991–0.997) | 0.968* | 0.962*/0.952* | 0.964 |
Reliability is calculated for intra- and interobserver measurement and presented with intraclass Coefficient (ICC 2,1) and 95% Confidence Interval (95% CI). Convergent validity are presented by Pearson’s correlation coefficient (Pearson’s r) and are calculated for neutral orientation only (n = 7), 10° projectional variation included (n = 49) and 20° projectional variation included (n = 91). Discriminant validity is represented by effect size (ES η 2)
* Values are significant at level <0.05
Validity
Whereas the validity was excellent for AC–DC in vertical displacement and for GC–PC in horizontal displacement, the remaining measurements showed moderate validity (Table 2).
The convergent validity, which represents the correlation between a radiographic parameter and the effective distance measured on CT, was 0.972 for AC–DC and 0.968 for GC–PC. Despite radiographic projectional variation of up to 20° due to malpositioning, convergent validity remained excellent for AC–DC and GC–PC with only marginal decrease in the correlation coefficient.
The discriminant validity, which represents a parameters ability to distinguish between different grades of ACJ separations, was excellent for AD-DC (0.952) and for GC–PC (0.964). Although CCran also demonstrated good discriminant validity (0.905), this measurements do not increase or decrease with an increase in vertical displacement between the different grades of ACJ separation as illustrated in Table 3. Hence, it has no utility in clinical practice.
Table 3.
Radiographic parameters and effective CT distance for each injury type
| Parameter | Control mean (SD) [mm] | RW II-0 mean (SD) [mm] | RW II-25 mean (SD) [mm] | RW III-0 mean (SD) [mm] | RW III-50 mean (SD) [mm] | RW IV-100 mean (SD) [mm] | RW V-200 mean (SD) [mm] | p value |
|---|---|---|---|---|---|---|---|---|
| Vertical displacement | ||||||||
| Effective | 1 | 6 | 6 | 11.3 | 11.5 | 19.2 | 25 | |
| CC | 12.6 (1.9) | 17.2 (2.0) | 16.7 (1.6) | 20.5 (1.8) | 17.1 (2.2) | 17.5 (1.9) | 23.5 (2.1) | <0.001* |
| AC–DC | 2.3 (1.9) | 6.9 (1.9) | 9.1 (1.8) | 11.4 (2.2) | 13.0 (1.4) | 17.9 (1.3) | 33 (3.7) | <0.001* |
| CCran | 48.9 (2.8) | 55.2 (1.3) | 52.7 (1.3) | 55.9 (2.0) | 48.5 (1.6) | 46.6 (1.7) | 66.6 (3.3) | <0.001* |
| Horizontal displacement | ||||||||
| Effective | 1 | 1 | 3 | 1 | 5.5 | 11 | 11 | |
| OL | 10.8 (1.0) | 11.2 (2.2) | 12.3 (2.3) | 9.5 (4.0) | 12.5 (1.7) | 12.4 (1.9) | −5.2 (12.3) | <0.001* |
| LE | 18.6 (3.7) | 11.9 (3.2) | 17.1 (3.5) | 12.8 (3.2) | 22.1 (3.3) | 27.6 (2.8) | 11.8 (5.2) | <0.001* |
| GC–PC | 32.1 (2.0) | 32.2 (1.3) | 37.7 (2.1) | 37.4 (1.5) | 43.9 (1.2) | 50.9 (0.9) | 55.3 (2.4) | <0.001* |
Data are presented with mean and standard deviations (SD) as absolute value measured in millimetre (mm). SD derives from projectional variations. Differences were tested for significance with independent ANOVA analysis and presented with p-value
*Values are significant at level <0.05
The individual values with 95% CI for AC–DC (Fig. 4a) and GC–PC (Fig. 4b) demonstrate that these measurements differentiate worsening severity of the ACJ dislocation effectively. In contrast, the CC distance does not differentiate the various grades of injury as well (Fig. 4c). Although the width of the 95% CI for AC–DC and GC–PC increases with the degree of projectional variation, minor deviations are negligible because they are less extensive than differences between injury type. Whereas vertical displacement measured by AC–DC is able to differentiate between all ACJ dislocations groups, the horizontal displacement measured by GC–PC is unable to clearly differentiate between the control and RWII-0 groups, as well as RWII-25 and RWIII-0 groups.
Fig. 4.
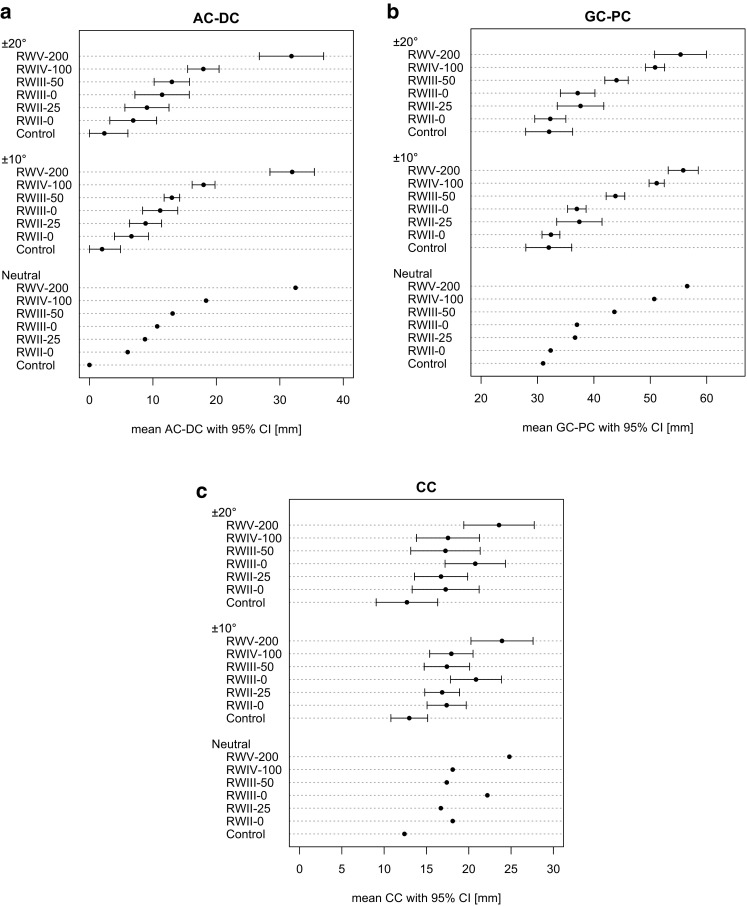
Effect of projectional variation for each type of injury. Mean and 95%CI are presented for each ACJ dislocation group depending of the amount of projectional variations included (neutral n = 7, 10 degrees n = 49 and 20 degrees n = 91). AC–DC is represented in a left, GC–PC in b middle and CC in c left
Projectional variation
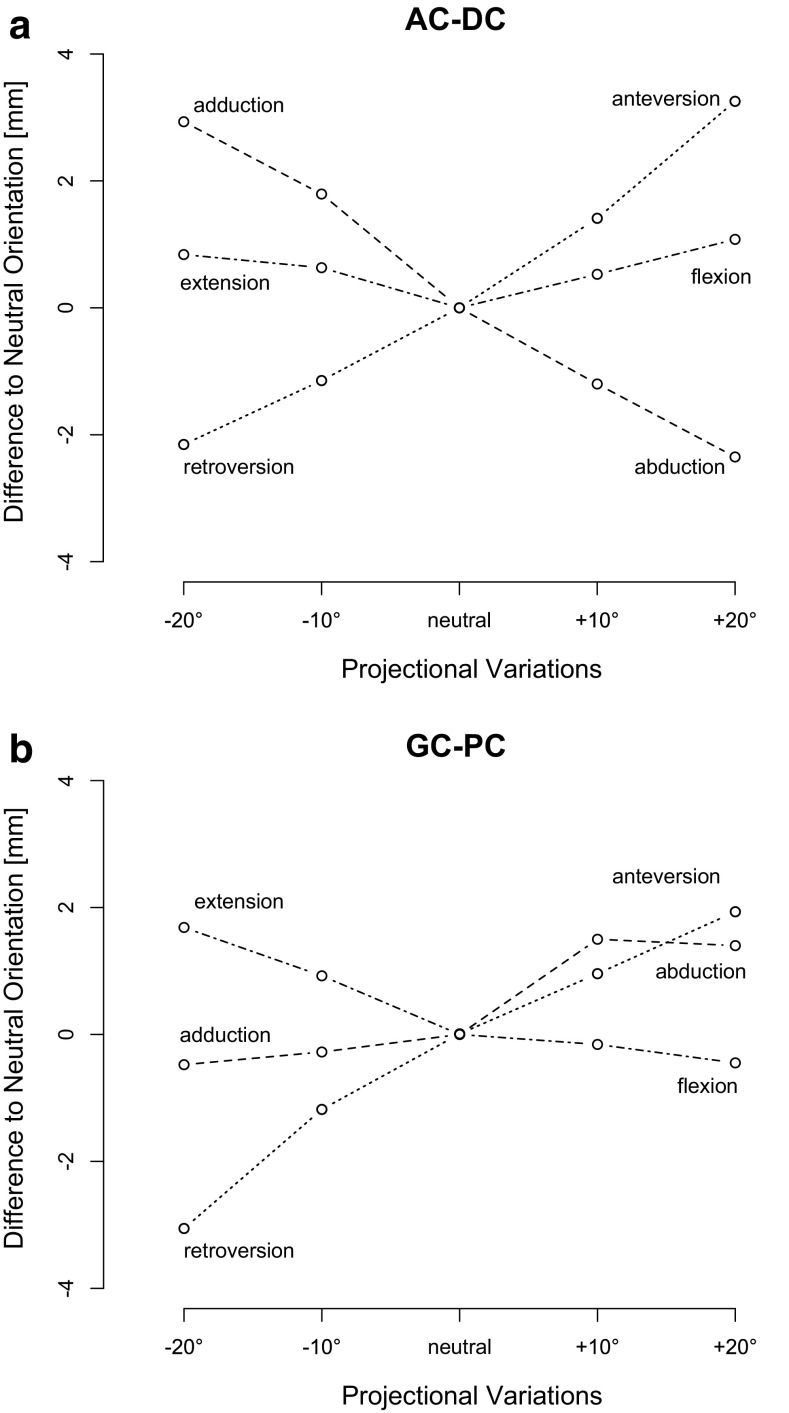
The effect of projectional variation due to malpositioning error on AC–DC measurements for vertical instability is less than one millimetre for deviation in the sagittal plane, and a maximum of 3.2 mm for 20° of anteversion (Fig. 5a). Malpositioning with abduction and retroversion tends to slightly underestimate the true value, whilst adduction and anteversion leads to a slight overestimation. For GC–PC measurements, a projectional variation of 20° retroversion leads to 3.1 mm difference. (Figure 5b). Extension, anteversion and abduction slightly overestimate the true value to within 2 mm, whilst adduction and flexion demonstrate negligible (< 0.3 mm) deviation.
Fig. 5.
Effect of projectional variation relating to the malposition. Mean deviations of the projectional variations (±10°, ±20°) are shown for AC–DC (a) and GC–PC (b) compared to neutral. Mean values are calculated including the different injuries. Lower values indicate underestimation, higher values overestimation. Axial variations are shown in dotted, sagittal variations dot dashed and coronal variation dashed
Discussion
The most important finding of the present study was the identification of two novel quantitative radiographic parameters of vertical (AC–DC) and (GC–PC) displacement in ACJ dislocations that are reasonably inert to projectional variations and may influence the management of these common injuries.
Despite ACJ separations being frequent injuries, there is still controversy around when surgical intervention is indicated. Although we readily assess vertical instability utilizing the commonly used Rockwood classification, we largely ignore the presence and/or degree of horizontal instability as a factor in managing these injuries either operatively or non-operatively. The assessment of vertical instability in the frontal plane radiographs as per the Rockwood system is known to be affected by projectional variances in obtaining radiographs [4]. Horizontal instability with painful posterior translation of the clavicle may result in further instability and subsequent deterioration in scapulothoracic rhythm [19, 20]. Hence, it has been considered as a potential indication for operative stabilization [21]. The presence and degree of horizontal instability is semi-quantitatively assessed in the lateral Alexander view [7, 22, 23] or by obtaining single or multiple Axillary views [10]. But standard Axillary radiographs have been shown to mimic posterior subluxation of the lateral end of the clavicle [11]. To date, there has been a lack of precise and reliable quantitative methods of assessing ACJ instability that are relatively inert to the projectional variations and that are inherent in obtaining radiographs. The aim of this study was to identify accurate, reliable, quantitative radiographic parameters for the assessment of ACJ separations that are largely unaffected by the inherent projectional variations in obtaining radiographs. Such standardized parameters may significantly influence the management of these common injuries.
Static imaging does not allow us to assess the ligamentous structures that maintain ACJ stability—dynamic or stress views are necessary. Although both Tossy et al. [24] and Rockwood [4] have discussed ACJ separations in the context of the CC and AC ligaments, their radiographic classification systems is largely based on the vertical displacement in the coronal plane, except for the type IV injury. The Rockwood classification, using the CC distances and axillary views have showed a poor inter- and intraobserver reliability and additional 3 dimensional CT reconstruction of the ACJ does not provide further insight [25]. There was poor agreement even among experienced surgeons as confirmed by Kraeutler et al. [26].
This study indicates that the intra- and interobserver agreement on CC distances in the frontal plane for vertical displacement was excellent. However, AC–DC also demonstrated excellent reliability as a quantitative radiographic parameter for vertical instability in the Alexander view with considerably greater validity in comparison with CC distance. Hence, AC–DC was found to have not only the best agreement among surgeons but also the best convergent validity with the strongest correlation between AC–DC measurements and the actual effective vertical displacement. Additionally, the discriminant validity determined by the effect size showed excellent ability of AC–DC in differentiating various grades of ACJ dislocation. In contrast, the CC distance was less discriminant. The measurement of a low CC distance in the Zanca view despite the presence of significant posterior displacement in the horizontal plane suggests that the Rockwood system may underestimate the severity of ACJ separations and therefore misguide surgeons towards non-operative management and poor outcomes [27, 28]. This hypothesis is supported by both, Nemec et al. [29] and Schaefer et al. [30] who demonstrated a different degree of AC ligament injury on MRI in comparison with the original radiographic Rockwood classification system. Interestingly, up to 25% additional ligament injuries were detected by MRI.
The importance of AC ligaments conferring stability was first described in 1917 [31]. Recent studies [19, 20] reemphasized its biomechanical role [19, 20, 32] in maintaining horizontal stability [33, 34]. The lack of attention to horizontal instability may be a reason why non-operative management of even Rockwood type I and II injuries results in clinical failure in up to 27%, which then requires delayed surgical intervention.
This study found that GC–PC had excellent convergent and discriminant validity as a quantitative radiographic parameter for horizontal instability in the lateral Alexander view. And furthermore, it demonstrated excellent intra- and interobserver reliability as well. To our knowledge, the GC–PC is the only quantitative radiographic parameter that allows accurate assessment of the horizontal displacement and is able to differentiate between the various Rockwood injury types. But GC–PC was not able to clearly differentiate between the Control and RWII-0 nor the RWII-25 and RWIII-0. Interestingly, the ISAKOS consensus group [35] has subdivided type III injuries into IIIA (which is the same as RWIII-0 in our study) as well as a type IIIB which describes an overriding clavicle on the cross-body adduction view. Most authors, including the ISAKOS group [7, 36, 37], recommend non-operative management for all these injuries (RWII-0, RWII-25 and RWIII-0) in the general population, hence GC–PC would still make a significant contribution to guiding management decisions despite its limitation in differentiating between the less severe injury types.
Rahm et al. [11], Gastaud et al. [38] and others [10, 39–41] have all shown that despite standardized protocols, classic axillary views are not recommended to assess posterior translation. Our assessment of the effect of projectional variation on our novel quantitative parameters demonstrated that even with 10° and 20° of malpositioning in various planes included, AC–DC and GC–PC continuously increased with increasing severity of ACJ separation. For AC–DC, the maximum mean difference to neutral was 3.2 mm in 20° of anteverted malpositioning, all the other projectional variations lead to a mean difference of less than 2 mm. The various mean projectional variations had even less of an impact on GC–PC with a maximum of 3.1 mm demonstrated with 20° of retroverted malpositioning. A comparative assessment of these quantitative radiographic parameters for ACJ separation to a normal uninjured control side may demonstrate a slight overestimation of AC–DC if the shoulder is too anteverted or adducted. And an underestimation is possible if the shoulder is too abducted or retroverted for AC–DC and anteverted for GC–PC. Both increase in anteversion and retroversion can generally be detected if the glenoid is not centred within the Y formed by the lateral and medial border of the scapula on the Alexander view.
Malpositioning errors may have an impact on the ability to differentiate between RWII and both RWIII injury subtypes in the vertical plane although the ability to differentiate between these less severe injury subtypes may not make a significant impact towards guiding management whilst in the horizontal plane the projectional error has the greatest impact on differentiating between RWII-25 and RWIII0 and both injury types that are treated non-operatively [7, 10, 36, 37, 42–44]. Hence, in terms of clinical decision-making in ACJ separations, projection errors would have the greatest impact on the use of CC distance in the vertical plane.
This study has several limitations. It is an in vitro study which utilizes one Sawbone scapular model in different orientations and therefore it does not fully represent the subtle anatomical variations between patients. A further limitation is the static and not dynamic experimental setup in our study. Absolute distances may change in a cadaver or clinical setup, and our values cannot be directly transferred to clinical practice. The clinical relevance of these new parameters and its role in guiding management of ACJ separations can only be fully understood and validated with a prospective clinical study. Reliable radiographic assessment of vertical and horizontal stability has an important role in guiding management, but the patients’ symptoms, functional demands and clinical examination findings are invaluable. Then, our analysis is based on radiographs with a predefined centre of the radiograph beam. This has become the standard setup for shoulder radiographs and it may not apply to radiographs obtained in other ways. The influence of variations on the radiograph centring and film focus distance was not analysed. This study did, however, analyse the data of different orientations of the model and its influence on these distances which was reported to be minor. This possibility indicates that the variation of the radiograph centring may not have a significant contribution to the overall results. The conclusions are therefore only directly transferable to radiographs centred on the glenoid centre.
Conclusion
AC–DC and GC–PC are two novel quantitative radiographic parameters of vertical and horizontal instability in ACJ dislocations that demonstrate excellent reliability and validity. They are both measured on lateral Alexander radiographic views with reasonable inertness to projectional errors. The CC distance may underestimate the severity of ACJ separations especially when there is horizontal instability. We recommend the use of AC–DC for assessing vertical displacement and GC–PC for assessing horizontal displacement in a single Alexander view to guide the appropriate management of ACJ separations. A better appreciation of the degree of horizontal instability, especially in lower Rockwood grades (II, III) of ACJ dislocations, may improve management of these controversial injuries.
Acknowledgements
The authors thank to Jennifer Cullmann Bastian, a radiologist at our department, for her assistance in taking the radiographs and for measuring the effective distances on CT and to Klaus Oberli for the creation of Fig. 2.
List of abbreviations
- ACJ
Acromioclavicular Joint
- AC
Acromioclavicular
- CC
Coracoclavicular
- RW
Rockwood Classification
- CT
Computed tomography
- AP
Anterior–posterior
- CC
Distance coracoclavicular distance (radiographic parameter)
- AC–DC
Acromial centre line to dorsal clavicle (radiographic parameter)
- CCran
Centre cranialization (radiographic parameter)
- OL
Maximal Overlap (radiographic parameter)
- LE
Lateral Extension (radiographic parameter)
- GC–PC
Glenoid centre line to posterior clavicle (radiographic parameter)
- ICC
Intraclass coefficient
- SD
Standard deviation
- 95%CI
95% Confidence Interval
- ES
Effect Size
Authors’ contribution
MAZ conceived and carried out the study design, participated in coordination of data acquisition, gave substantial contribution in interpretation of data and drafted the manuscript. PS participated in data acquisition and measured the radiograph parameters. BA participated in data acquisition and measured the radiograph parameters. LB performed the statistical analysis, and the interpretation of data was involved in drafting the manuscript and revised the manuscript critically for statistical properness. JW participated in data acquisition and measured the radiograph parameters. MHM performed the radiographic protocol and participated in data acquisition. BKM carried out the study design, conceived the testing setup and created the 3D hoist and participated in data acquisition. MS carried out the study design, conceived the testing setup and created the 3D hoist and participated in data acquisition. SR participated in data acquisition, measured the radiograph parameters, was involved in clinical interpretation and drafted the manuscript. All authors read and approved the final manuscript.
Compliance with ethical standards
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
No grant was received for this study.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
References
- 1.Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35(2):316–329. doi: 10.1177/0363546506298022. [DOI] [PubMed] [Google Scholar]
- 2.Saccomanno MF, DEI C, Milano G. Acromioclavicular joint instability: anatomy, biomechanics and evaluation. Joints. 2014;2(2):87–92. doi: 10.11138/jts/2014.2.2.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tauber M. Acromioclavicular injuries in professional athletes. Orthopade. 2014;43(3):249–255. doi: 10.1007/s00132-013-2148-3. [DOI] [PubMed] [Google Scholar]
- 4.Rockwood CA., Jr . Injuries to the acromioclavicular joint. In: Rockwood CA Jr, Green DP, editors. Fractures in adults, Vol. 1. 2. Philadelphia: JB Lippincott; 1984. pp. 860–910. [Google Scholar]
- 5.Hedtmann A, Fett H, Ludwig J. Management of old neglected posttraumatic acromioclavicular joint instability and arthrosis. Orthopade. 1998;27(8):556–566. doi: 10.1007/s001320050267. [DOI] [PubMed] [Google Scholar]
- 6.Metzlaff S, Rosslenbroich S, Forkel PH, Schliemann B, Arshad H, Raschke M, Petersen W. Surgical treatment of acute acromioclavicular joint dislocations: hook plate versus minimally invasive reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):1972–1978. doi: 10.1007/s00167-014-3294-9. [DOI] [PubMed] [Google Scholar]
- 7.Scheibel M, Droschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011;39(7):1507–1516. doi: 10.1177/0363546511399379. [DOI] [PubMed] [Google Scholar]
- 8.Cisneros LN, Reiriz JS. Prevalence of remaining horizontal instability in high-grade acromioclavicular joint injuries surgically managed. Eur J Orthop Surg Traumatol. 2017;27(3):323–333. doi: 10.1007/s00590-016-1898-0. [DOI] [PubMed] [Google Scholar]
- 9.Schneider MM, Balke M, Koenen P, Frohlich M, Wafaisade A, Bouillon B, Banerjee M. Inter- and intraobserver reliability of the Rockwood classification in acute acromioclavicular joint dislocations. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2192–2196. doi: 10.1007/s00167-014-3436-0. [DOI] [PubMed] [Google Scholar]
- 10.Tauber M, Koller H, Hitzl W, Resch H. Dynamic radiologic evaluation of horizontal instability in acute acromioclavicular joint dislocations. Am J Sports Med. 2010;38(6):1188–1195. doi: 10.1177/0363546510361951. [DOI] [PubMed] [Google Scholar]
- 11.Rahm S, Wieser K, Spross C, Vich M, Gerber C, Meyer DC. Standard axillary radiographs of the shoulder may mimic posterior subluxation of the lateral end of the clavicle. J Orthop Trauma. 2013;27(11):622–626. doi: 10.1097/BOT.0b013e31828f912c. [DOI] [PubMed] [Google Scholar]
- 12.Wellmann M, da Silva G, Lichtenberg S, Magosch P, Habermeyer P. Instability pattern of acromioclavicular joint dislocations type Rockwood III: relevance of horizontal instability. Orthopade. 2013;42(4):271–277. doi: 10.1007/s00132-013-2085-1. [DOI] [PubMed] [Google Scholar]
- 13.Alexander OM. Radiography of the acromioclavicular articulation. Med Radiogr Photogr. 1954;30(2):34–39. [PubMed] [Google Scholar]
- 14.Zanca P. Shoulder pain: involvement of the acromioclavicular joint. (Analysis of 1,000 cases) Am J Roentgenol Radium Ther Nucl Med. 1971;112(3):493–506. doi: 10.2214/ajr.112.3.493. [DOI] [PubMed] [Google Scholar]
- 15.Minkus M, Hann C, Scheibel M, Kraus N. Quantification of dynamic posterior translation in modified bilateral Alexander views and correlation with clinical and radiological parameters in patients with acute acromioclavicular joint instability. Arch Orthop Trauma Surg. 2017 doi: 10.1007/s00402-017-2691-1. [DOI] [PubMed] [Google Scholar]
- 16.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 17.Munro BH. Statistical Methods for Health Care Research. 5. Philadelphia: Lippincott Williams and Wilkins; 2005. pp. 243–249. [Google Scholar]
- 18.Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Stat Med. 1998;17(1):101–110. doi: 10.1002/(SICI)1097-0258(19980115)17:1<101::AID-SIM727>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 19.Dawson PA, Adamson GJ, Pink MM, Kornswiet M, Lin S, Shankwiler JA, Lee TQ. Relative contribution of acromioclavicular joint capsule and coracoclavicular ligaments to acromioclavicular stability. J Shoulder Elbow Surg. 2009;18(2):237–244. doi: 10.1016/j.jse.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 20.Jari R, Costic RS, Rodosky MW, Debski RE. Biomechanical function of surgical procedures for acromioclavicular joint dislocations. Arthroscopy. 2004;20(3):237–245. doi: 10.1016/j.arthro.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 21.Simovitch R, Sanders B, Ozbaydar M, Lavery K, Warner JJ. Acromioclavicular joint injuries: diagnosis and management. J Am Acad Orthop Surg. 2009;17(4):207–219. doi: 10.5435/00124635-200904000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Alexander OM. Dislocation of the acromioclavicular joint. Radiography. 1949;15(179):260. [PubMed] [Google Scholar]
- 23.Waldrop JI, Norwood LA, Alvarez RG. Lateral roentgenographic projections of the acromioclavicular joint. Am J Sports Med. 1981;9(5):337–341. doi: 10.1177/036354658100900511. [DOI] [PubMed] [Google Scholar]
- 24.Tossy JD, Mead NC, Sigmond HM. Acromioclavicular separations: useful and practical classification for treatment. Clin Orthop Relat Res. 1963;28:111–119. [PubMed] [Google Scholar]
- 25.Cho CH, Hwang I, Seo JS, Choi CH, Ko SH, Park HB, Dan J. Reliability of the classification and treatment of dislocations of the acromioclavicular joint. J Shoulder Elbow Surg. 2014;23(5):665–670. doi: 10.1016/j.jse.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 26.Kraeutler MJ, Williams GR, Jr, Cohen SB, Ciccotti MG, Tucker BS, Dines JS, Altchek DW, Dodson CC. Inter- and intraobserver reliability of the radiographic diagnosis and treatment of acromioclavicular joint separations. Orthopedics. 2012;35(10):e1483–e1487. doi: 10.3928/01477447-20120919-16. [DOI] [PubMed] [Google Scholar]
- 27.Mouhsine E, Garofalo R, Crevoisier X, Farron A. Grade I and II acromioclavicular dislocations: results of conservative treatment. J Shoulder Elbow Surg. 2003;12(6):599–602. doi: 10.1016/S1058-2746(03)00215-5. [DOI] [PubMed] [Google Scholar]
- 28.Schlegel TF, Burks RT, Marcus RL, Dunn HK. A prospective evaluation of untreated acute grade III acromioclavicular separations. Am J Sports Med. 2001;29(6):699–703. doi: 10.1177/03635465010290060401. [DOI] [PubMed] [Google Scholar]
- 29.Nemec U, Oberleitner G, Nemec SF, Gruber M, Weber M, Czerny C, Krestan CR. MRI versus radiography of acromioclavicular joint dislocation. AJR Am J Roentgenol. 2011;197(4):968–973. doi: 10.2214/AJR.10.6378. [DOI] [PubMed] [Google Scholar]
- 30.Schaefer FK, Schaefer PJ, Brossmann J, Hilgert RE, Heller M, Jahnke T. Experimental and clinical evaluation of acromioclavicular joint structures with new scan orientations in MRI. Eur Radiol. 2006;16(7):1488–1493. doi: 10.1007/s00330-005-0093-1. [DOI] [PubMed] [Google Scholar]
- 31.Cadenat FM. The treatment of dislocations and fractures of the outer end of the clavicle. Int Clin. 1917;1:145–169. [Google Scholar]
- 32.Costic RS, Labriola JE, Rodosky MW, Debski RE. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004;32(8):1929–1936. doi: 10.1177/0363546504264637. [DOI] [PubMed] [Google Scholar]
- 33.Debski RE, Parsons IM, 3rd, Fenwick J, Vangura A. Ligament mechanics during three degree-of-freedom motion at the acromioclavicular joint. Ann Biomed Eng. 2000;28(6):612–618. doi: 10.1114/1.1304848. [DOI] [PubMed] [Google Scholar]
- 34.Luis GE, Yong CK, Singh DA, Sengupta S, Choon DS. Acromioclavicular joint dislocation: a comparative biomechanical study of the palmaris-longus tendon graft reconstruction with other augmentative methods in cadaveric models. J Orthop Surg Res. 2007;2:22. doi: 10.1186/1749-799X-2-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beitzel K, Mazzocca AD, Bak K, Itoi E, Kibler WB, Mirzayan R, Imhoff AB, Calvo E, Arce G, Shea K, Upper Extremity Committee of ISAKOS ISAKOS upper extremity committee consensus statement on the need for diversification of the rockwood classification for acromioclavicular joint injuries. Arthroscopy. 2014;30(2):271–278. doi: 10.1016/j.arthro.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 36.Korsten K, Gunning AC, Leenen LP. Operative or conservative treatment in patients with Rockwood type III acromioclavicular dislocation: a systematic review and update of current literature. Int Orthop. 2014;38(4):831–838. doi: 10.1007/s00264-013-2143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith TO, Chester R, Pearse EO, Hing CB. Operative versus non-operative management following Rockwood grade III acromioclavicular separation: a meta-analysis of the current evidence base. J Orthop Traumatol. 2011;12(1):19–27. doi: 10.1007/s10195-011-0127-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gastaud O, Raynier JL, Duparc F, Baverel L, Andrieu K, Tarissi N, Barth J. Reliability of radiographic measurements for acromioclavicular joint separations. Orthop Traumatol Surg Res. 2015;101(8 Suppl):S291–S295. doi: 10.1016/j.otsr.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 39.Barth J, Duparc F, Baverel L, Bahurel J, Toussaint B, Bertiaux S, Clavert P, Gastaud O, Brassart N, Beaudouin E, De Mourgues P, Berne D, Duport M, Najihi N, Boyer P, Faivre B, Meyer A, Nourissat G, Poulain S, Bruchou F, Menard JF, dA Francaise Societe. Prognostic factors to succeed in surgical treatment of chronic acromioclavicular dislocations. Orthop Traumatol Surg Res. 2015;101(8 Suppl):S305–S311. doi: 10.1016/j.otsr.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 40.Bernageau J, Patte D. The radiographic diagnosis of posterior dislocation of the shoulder (author’s transl) Rev Chir Orthop Reparatrice Appar Mot. 1979;65(2):101–107. [PubMed] [Google Scholar]
- 41.Rokous JR, Feagin JA, Abbott HG. Modified axillary roentgenogram. A useful adjunct in the diagnosis of recurrent instability of the shoulder. Clin Orthop Relat Res. 1972;82:84–86. doi: 10.1097/00003086-197201000-00012. [DOI] [PubMed] [Google Scholar]
- 42.Bannister GC, Wallace WA, Stableforth PG, Hutson MA. The management of acute acromioclavicular dislocation. A randomised prospective controlled trial. J Bone Joint Surg Br. 1989;71(5):848–850. doi: 10.1302/0301-620X.71B5.2684990. [DOI] [PubMed] [Google Scholar]
- 43.Longo UG, Ciuffreda M, Rizzello G, Mannering N, Maffulli N, Denaro V. Surgical versus conservative management of Type III acromioclavicular dislocation: a systematic review. Br Med Bull. 2017 doi: 10.1093/bmb/ldx003. [DOI] [PubMed] [Google Scholar]
- 44.Tauber M. Management of acute acromioclavicular joint dislocations: current concepts. Arch Orthop Trauma Surg. 2013;133(7):985–995. doi: 10.1007/s00402-013-1748-z. [DOI] [PubMed] [Google Scholar]