Abstract
Aims/Introduction
Psoriasis, a chronic autoimmune skin disorder, is believed to contribute to cardiovascular diseases and metabolic syndrome. Psoriasis's association with the components of metabolic syndrome has been reported previously. However, large‐scale cross‐sectional studies about psoriasis and metabolic syndrome are rare in China.
Materials and Methods
We assessed the prevalence of metabolic syndrome in Chinese psoriasis patients and controls.
Results
A total of 859 psoriasis patients and 1,718 controls were recruited in an age‐ and sex‐matched cross‐sectional study. Metabolic syndrome occurred in 14.3% of the psoriasis patients as opposed to 10.0% of the control participants (P = 0.001). Psoriasis patients had a higher prevalence of overweight/obesity, hyperglycemia and dyslipidemia when compared with controls. Meanwhile, psoriasis patients with metabolic syndrome were older, and had an older age of onset and a longer disease duration when compared with those without metabolic syndrome.
Conclusions
The prevalence of metabolic syndrome is higher in the Chinese psoriatic population, which can favor cardiovascular events. The present study strengthens the value of treating psoriasis patients not only dealing with the skin lesions, and we suggest appropriate screening and relevant health education be carried out in the treatment of psoriasis patients.
Keywords: Metabolic syndrome, Prevalence, Psoriasis
Introduction
As a common chronic recurrent skin disease, psoriasis occurs all around the world, but its prevalence varies substantially1, 2, 3. The latest data have shown that psoriasis occurs in 0.47% of the Chinese population, and the prevalence and incidence of psoriasis have been increasing year‐by‐year4. Genetic tendency and environmental influence were both important ingredients, which contributed to its pathomechanism1. Psoriasis can be associated with several comorbidities. Recently, psoriasis has been linked to metabolic syndrome and its components, along with atherosclerosis and myocardial infarction5, 6. Metabolic syndrome includes abdominal obesity, hypertension, dyslipidemia and glucose intolerance, which can favor cardiovascular events7. Among these elementary risk factors, central obesity and glucose intolerance are regarded as the most important8. However, the interaction between these two processes during the course of the disease is still unknown. It is thought that genetic susceptibility and overlapping inflammatory pathways are potentially linked and underlying this association of psoriasis with metabolic syndrome9.
Although numerous epidemiological studies have shown that psoriasis is closely related to metabolic syndrome, such reports are rare in China, especially large‐scale cross‐sectional studies. In order to survey the association between psoriasis and metabolic syndrome in the Chinese population, a hospital‐based cross‐sectional study was applied.
Material and Methods
Patient selection
In the present study, 859 adult psoriasis patients and 1,718 non‐psoriatic individuals were recruited. The patients and the controls were 1:2 age‐ and sex‐matched. We included 859 psoriasis patients who visited the Department of Dermatology at Peking Union Medical College Hospital, Beijing, China, between the years of 2005 and 2015 as participants of the present study. A total of 440 of them were inpatients, whereas the other 419 were outpatients. The psoriasis patients were diagnosed based on clinical manifestation of psoriasis, and the clinical subtypes were classified into psoriasis vulgaris, pustular psoriasis, erythrodermic psoriasis, arthritic psoriasis and mixed psoriasis10. Patients who had received any kind of systemic treatment, such as acitretin, ciclosporin or biologics, during the preceding 1 month and those with secondary dyslipidemia were excluded. Controls were selected from the Department of Physical Examination Center of Peking Union Medical College Hospital in 2015. They had no hepatic disorders, kidney dysfunction or infectious diseases. The protocol was approved by the institutional review board of Peking Union Medical College Hospital.
The relevant characteristics of all individuals including age, sex, ethnic group, weight, height, blood pressure and so on were recorded, and body mass index was calculated. All patients and controls were assessed to determine the presence of hypertension and type 2 diabetes mellitus. In addition, the disease duration, subtype and age of onset were all collected as well. We used the Psoriasis Area and Severity Index (PASI) to assess the disease severity. After an overnight fast (at least 8 h), venous blood samples were collected from the anterior cubital vein in all participants under complete aseptic conditions, and were analyzed for fasting serum glucose (FBG), triglyceride and serum high‐density lipoprotein (HDL) cholesterol in the clinical biochemistry laboratory. The serum samples were analyzed by using Beckman Coulter AU5400/5800 (Brea, CA, USA). FBG was estimated by the hexokinase method, and triglyceride and HDL cholesterol were measured by enzymatic colorimetric assay. The presence of obesity/overweight, elevation of blood pressure, high FBG and triglycerides levels, and low HDL cholesterol levels were also evaluated and recorded. Many organizations have proposed diagnostic criteria for metabolic syndrome, and the criteria we used were obtained from the Chinese Diabetes Society in April of 2004, which were more suitable for Chinese people (Table 1)11.
Table 1.
Diagnosis criteria of metabolic syndrome recommended by the Chinese Diabetes Society10
| To establish a diagnosis of metabolic syndrome, any three out of the four following criteria should be fulfilled: | |
| Components | Index |
| Overweight or obesity | BMI ≥ 25.0 kg/m2 |
| Hyperglycemia | FBG ≥6.1 mmol/L and/or receiving therapy for diabetes mellitus |
| High blood pressure | Blood pressure ≥140/90 mmHg and/or receiving therapy for hypertension |
| Dyslipidemia | Fasting blood triglycerides ≥1.7 mmol/L and/or fasting blood HDL cholesterol <0.9 mmol/L for men or <1.0 mmol/L for women |
BMI, body mass index; FBG, fasting blood glucose; HDL, high‐density lipoprotein.
Statistical analysis
Continuous data were expressed as mean ± standard deviation. Categorical parameters were expressed as the number (percentage) of patients. Differences between groups were calculated by the χ2‐test or Mann–Whitney non‐parametric test, where appropriate. A P‐value of <0.05 was taken to show statistical significance. Data were analyzed using SPSS (IBM, Armonk, NY, USA) and Prism software (GraphPad Software, San Diego, CA, USA).
Results
Prevalence of metabolic syndrome and its components in psoriasis patients and controls
A total of 2,577 participants were investigated in two groups: the psoriasis group (n = 859) and the control group (n = 1,718). Psoriasis patients had a higher body mass index, diastolic blood pressure and triglycerides, and a lower FBG and HDL cholesterol level compared with the controls (Tables 2 and 3). The systolic blood pressure was similar between the cases and controls (Table 2). Meanwhile, we compared the prevalence of components of metabolic syndrome between the psoriasis and the control group. The psoriasis group had a higher prevalence of overweight/obesity, hyperglycemia, hypertriglyceridemia and low HDL cholesterol. The psoriasis group suffered more commonly from metabolic syndrome when compared with the control group (14.3% vs 10.0%, P = 0.001; Table 3). Similar results were found when the data were analyzed with the criteria of the National Cholesterol Education Program‐Adult Treatment Plan III (25.1% vs 17.5%, P < 0.0001) and International Diabetes Federation (21.7% vs 15.5%, P = 0.0001) for metabolic syndrome. The prevalence of metabolic syndrome in the psoriasis group and control group by age is shown in a histogram (Figure 1). The prevalence of metabolic syndrome in the psoriasis group was higher than the control group in every age class. The prevalence of metabolic syndrome in the psoriasis group sharply increased in participants aged in their 40s, and peaked in participants aged in their 60s. In marked contrast, the prevalence of metabolic syndrome in the control group increased in participants aged in their 40s, and gradually increased in participants aged in their 60s.
Table 2.
Descriptive characteristics of the psoriasis group and control group
| Cases (n = 859) | Controls (n = 1,718) | P‐value | |
|---|---|---|---|
| Sex (male/female) | 547/312 | 1094/624 | 1.0000 |
| Age at enrollment (years) | 41.29 ± 15.12 | 41.29 ± 15.11 | >0.9999 |
| BMI (kg/m2) | 24.28 ± 3.790 | 23.88 ± 3.501 | 0.0091 |
| FBG (mmol/L) | 5.249 ± 1.425 | 5.275 ± 0.9226 | <0.0001 |
| SBP (mmHg) | 119.9 ± 13.99 | 121.7 ± 18.08 | 0.1071 |
| DBP (mmHg) | 77.78 ± 9.751 | 75.40 ± 11.23 | <0.0001 |
| Triglyceride (mmol/L) | 1.674 ± 1.605 | 1.332 ± 0.9659 | <0.0001 |
| HDL cholesterol (mmol/L) | 1.080 ± 0.3263 | 1.360 ± 0.3438 | <0.0001 |
Data are shown as mean ± standard deviation, or as n (%). BMI, body mass index; DBP, diastolic blood pressure; FBG, fasting blood glucose; HDL, high‐density lipoprotein; SBP, systolic blood pressure.
Table 3.
Prevalence of metabolic syndrome and its components of cases and controls
| Cases (n = 859) | Controls (n = 1,718) | P‐value | OR | 95% CI | |
|---|---|---|---|---|---|
| Overweight/obesity, n (%) | 354 (41.2) | 619 (36.0) | 0.0106 | 1.245 | 1.052–1.472 |
| Hyperglycemia, n (%) | 124 (14.4) | 172 (10.0) | 0.0009 | 1.516 | 1.184–1.941 |
| High blood pressure, n (%) | 182 (21.2) | 358 (20.8) | 0.8373 | 1.021 | 0.8354–1.248 |
| Triglycerides ≥1.7 mmol/L, n (%) | 271 (31.6) | 375 (21.8) | <0.0001 | 1.651 | 1.373–1.984 |
| HDL cholesterol <0.9 mmol/L (M) or <1.0 mmol/L (F), n (%) | 255 (29.7) | 124 (7.2) | <0.0001 | 5.427 | 4.294–6.859 |
| Metabolic syndrome, n (%) | 123 (14.3) | 171 (10.0) | 0.0010 | 1.512 | 1.180–1.937 |
CI, confidence interval; HDL, high‐density lipoprotein; OR, odds ratio.
Figure 1.
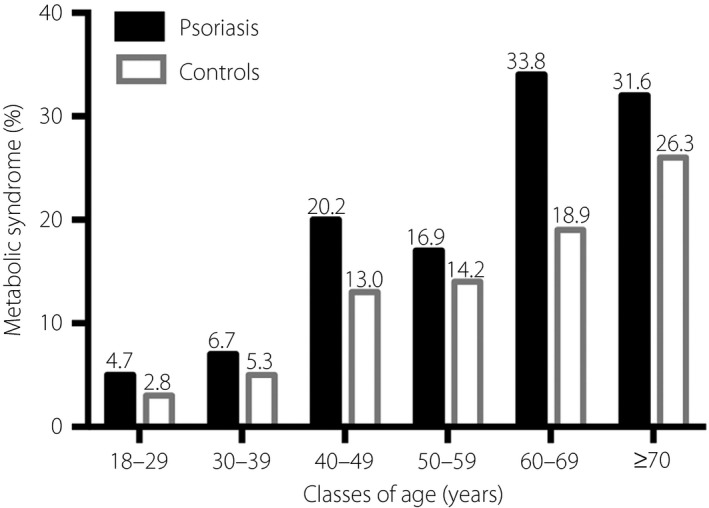
The prevalence of metabolic syndrome in different age classes. The prevalence of metabolic syndrome in psoriasis group was higher than control group in every age class.
Subtype and disease severity of psoriasis in psoriasis patients with and without metabolic syndrome
The psoriasis patients were then stratified into subgroups with and without metabolic syndrome. The characteristics of both subgroups are summarized in Table 4. We compared the age, sex, ethnic group, age of onset, disease duration and subtypes of psoriasis between these two subgroups. Patients in the metabolic syndrome subgroup were older, and had an older age of onset and longer disease duration compared with the other. However, there was no significant difference in the prevalence of metabolic syndrome in the regard to sex, ethnic group and clinical subtypes of psoriasis. As PASI was collected from just some of the psoriasis patients, we divided the 585 psoriasis patients with PASI into two groups: 74 patients that had metabolic syndrome and the remaining 511 who did not have metabolic syndrome. The present investigation shows no significant difference in disease severity between these two subgroups (Table 4).
Table 4.
Descriptive characteristics of subgroups in psoriatic patients
| Metabolic syndrome subgroup (n = 123) | Non‐metabolic syndrome subgroup (n = 736) | P‐value | |
|---|---|---|---|
| Sex (male/female) | 82/41 | 465/271 | 0.4566 |
| Age at enrollment (years) | 50.50 ± 13.60 | 39.75 ± 14.81 | <0.001 |
| Ethnic group (Han/minorities) | 121/2 | 704/32 | 0.2109 |
| Age at onset of psoriasis (years) | 36.11 ± 16.12 | 28.06 ± 13.74 | <0.0001 |
| Duration of psoriasis (years) | 14.40 ± 11.88 | 11.68 ± 10.44 | 0.0234 |
| Subtype of psoriasis, n (%) | |||
| Psoriasis vulgaris | 83 (67.5) | 560 (76.1) | 0.2458 |
| Pustular psoriasis | 11 (8.9) | 62 (8.4) | |
| Erythrodermic psoriasis | 16 (13.0) | 59 (8.0) | |
| Arthritic psoriasis | 11 (8.9) | 45 (6.1) | |
| Mixed psoriasis | 2 (1.6) | 10 (1.4) | |
| PASI |
16.64 ± 13.56 (n = 74) |
15.14 ± 14.18 (n = 511) |
0.2579 |
| Severity of psoriasis, n (%) | |||
| Mild (PASI <3) | 14 (18.9) | 97 (19.0) | 0.1029 |
| Moderate (3 ≤ PASI < 10) | 14 (18.9) | 155 (30.3) | |
| Severe (PASI ≥10) | 46 (62.2) | 259 (50.7) | |
PASI, Psoriasis Area and Severity Index.
Discussion
In the present study, we showed that metabolic syndrome, overweight/obesity, hyperglycemia and dyslipidemia were more prevalent in psoriasis patients than controls in the Chinese population. Psoriasis patients with metabolic syndrome were older, and had an older age of onset and a longer disease duration compared with those without metabolic syndrome.
Recently, an increasing number of epidemiological studies have shown that psoriasis is closely related to metabolic syndrome and cardiovascular factors. A previous study showed that metabolic syndrome was more prevalent in psoriasis patients compared with non‐psoriatic individuals in Italy (26.84% vs 15.16%, P = 0.0001; adjusted odds ratio 1.96)12. Love et al.13 carried out a cross‐sectional health survey including 6,549 participants, and concluded that metabolic syndrome was more common among psoriasis patients than controls (40% vs 23%, odds ratio 2.16) in the general USA population. Cohen et al.14 showed that the prevalence of metabolic syndrome was higher in psoriasis patients, which was consistent with Gironde's report15. However, there have been some controversies as well. Kim et al.16 investigated 490 psoriasis patients and 682 controls for cardiovascular risk factors, and found no statistical correlation between psoriasis and metabolic syndrome in Korean patients. The different results might be due to the low prevalence of metabolic syndrome in both groups, the genetic and racial differences, and so on.
In the present study, we found that metabolic syndrome was present in 14.3% of the psoriasis group as compared with 10.0% of the control group. The components of metabolic syndrome (obesity, hyperglycemia and dyslipidemia) were more significantly common in psoriasis patients than controls. It is important to emphasize that association alone was proven, and not causality. The underlying mechanism between metabolic comorbidities and psoriasis is unknown. Further prospective research with well‐designed longitudinal studies is urgently required to precisely elucidate the association. However, we propose that psoriasis could be used as a novel risk factor for the metabolic syndrome.
We showed a higher body mass index level and a higher prevalence of overweight in psoriasis patients than those in the controls (41.2% vs 36.0%, P = 0.011). These results further support previous epidemiological studies, which identified obesity as a risk factor for psoriasis progression17. Obesity, especially abdominal obesity, is now regarded as a chronic inflammatory status in which pro‐inflammatory adipokines and cytokines are secreted continuously leading to the development of metabolic syndrome and cardiovascular disease18. The psoriasis probably interacts with obesity bidirectionally, considering the fact that obesity predisposes to psoriasis and psoriasis favors obesity. Importantly, both psoriasis and obesity shared many cytokines in the pathophysiological process, which also results in metabolic syndrome19.
In addition, we found that psoriasis patients with metabolic syndrome were older, and had an older age of onset and a longer disease duration when compared with the others, whereas the sex, ethnic group and subtype of psoriasis were similar. The present results suggest that psoriasis duration might be a risk factor for metabolic syndrome. The most likely explanation for this is that depression, diet and inflammatory cytokines induced by psoriasis lead to metabolic syndrome20. The chronic maintaining inflammatory level in psoriasis patients might be the intrinsic criminal behind this result21. The finding that higher age at disease onset was closely related to elevated risk of metabolic syndrome was in agreement with previous studies22, 23. The present study showed no significant association between metabolic syndrome and psoriasis using PASI, which was consistent with the findings from studies of South‐East Asian patients10, 24.
A major strength of the present study was the enrollment of a large number of Chinese psoriasis patients, which to our knowledge was the largest‐scale cross‐sectional study on the possible association between psoriasis and metabolic syndrome in China. However, our study presented some limitations. First, our study was carried out in a tertiary care medical center, and thus patients enrolled in this study were biased toward having higher disease severity. Second, it was a cross‐sectional study, and the directionality of the causal association could not be determined. Third, the present result was based on a single‐center study carried out among a northeast Chinese population that might not be representative of the general population.
In conclusion, the prevalence of metabolic syndrome and some cardiovascular risks (obesity, hyperglycemia and dyslipidemia) was higher in psoriasis patients. The results supported that psoriasis is a pre‐atherosclerotic disease. The present study strengthens the value of treating psoriasis by not only dealing with the skin lesions, and we suggest appropriate screening and relevant health education be carried out in the management of psoriasis patients.
Disclosure
The authors declare no conflict of interest.
Acknowledgments
This present study was supported by the Natural Science Foundation of Beijing Municipality, China (Grant NO. 7152117). We thank our clinical colleagues Dr Teng Zhu, Dr Fenghui Ye and Dr Wei Rao from the Department of Dermatology, and Dr Hao Nie from the Department of Vascular Surgery for their technical assistance and helpful discussions and comments on the manuscript.
J Diabetes Investig 2018; 9: 39–43
References
- 1. Grozdev I, Korman N, Tsankov N. Psoriasis as a systemic disease. Clin Dermatol 2014; 32: 343–350. [DOI] [PubMed] [Google Scholar]
- 2. Griffiths CEM, Barker JNWN. Pathogenesis and clinical features of psoriasis. Lancet 2007; 370: 263–271. [DOI] [PubMed] [Google Scholar]
- 3. Parisi R, Symmons DPM, Griffiths CEM, et al Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol 2013; 133: 377–385. [DOI] [PubMed] [Google Scholar]
- 4. Ding X, Wang T, Shen Y, et al Prevalence of psoriasis in China: a population‐based study in six cities. Eur J Dermatol 2012; 22: 663–667. [DOI] [PubMed] [Google Scholar]
- 5. Schwandt A, Bergis D, Dapp A, et al Psoriasis and diabetes: a multicenter study in 222078 Type 2 diabetes patients reveals high levels of depression. J Diabetes Res 2015; 2015: 792968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Coumbe AG, Pritzker MR, Duprez DA. Cardiovascular risk and psoriasis: beyond the traditional risk factors. Am J Med 2014; 127: 12–18. [DOI] [PubMed] [Google Scholar]
- 7. Grundy SM. Pre‐diabetes, metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol 2012; 59: 635–643. [DOI] [PubMed] [Google Scholar]
- 8. Tyrovolas S, Koyanagi A, Garin N, et al Diabetes mellitus and its association with central obesity and disability among older adults: a global perspective. Exp Gerontol 2015; 64: 70–77. [DOI] [PubMed] [Google Scholar]
- 9. Sales R, Torres T. Psoriasis and metabolic syndrome. Acta Dermatovenerol Croat 2014; 22: 169–174. [PubMed] [Google Scholar]
- 10. Kokpol C, Aekplakorn W, Rajatanavin N. Prevalence and characteristics of metabolic syndrome in South‐East Asian psoriatic patients: a case‐control study. J Dermatol 2014; 41: 898–902. [DOI] [PubMed] [Google Scholar]
- 11. Chinese Diabetes Society . Advice on the metabolic syndrome of Chinese people. Foreign Med 2004; 31: 310–311 (Chinese). [Google Scholar]
- 12. Parodi A, Aste N, Calvieri C, et al Metabolic syndrome prevalence in psoriasis: a cross‐sectional study in the Italian population. Am J Clin Dermatol 2014; 15: 371–377. [DOI] [PubMed] [Google Scholar]
- 13. Love TJ, Qureshi AA, Karlson EW, et al Prevalence of the metabolic syndrome in psoriasis: results from the National Health and Nutrition Examination Survey, 2003–2006. Arch Dermatol 2011; 147: 419–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cohen AD, Sherf M, Vidavsky L, et al Association between psoriasis and the metabolic syndrome. A cross‐sectional study. Dermatology 2008; 216: 152–155. [DOI] [PubMed] [Google Scholar]
- 15. Gisondi P, Tessari G, Conti A, et al Prevalence of metabolic syndrome in patients with psoriasis: a hospital‐based case‐control study. Br J Dermatol 2007; 157: 68–73. [DOI] [PubMed] [Google Scholar]
- 16. Kim GW, Park HJ, Kim HS, et al Analysis of cardiovascular risk factors and metabolic syndrome in Korean patients with psoriasis. Ann Dermatol 2012; 24: 11–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Setty AR, Curhan G, Choi HK. Obesity, waist circumference, weight change, and the risk of psoriasis in women: Nurses’ Health Study II. Arch Intern Med 2007; 167: 1670–1675. [DOI] [PubMed] [Google Scholar]
- 18. Hercogová J, Ricceri F, Tripo L, et al Psoriasis and body mass index. Dermatol Ther 2010; 23: 152–154. [DOI] [PubMed] [Google Scholar]
- 19. Sterry W, Strober BE, Menter A. Obesity in psoriasis: the metabolic, clinical and therapeutic implications. Report of an interdisciplinary conference and review. Br J Dermatol 2007; 157: 649–655. [DOI] [PubMed] [Google Scholar]
- 20. Nisa N, Qazi MA. Prevalence of metabolic syndrome in patients with psoriasis. Indian J Dermatol Venereol Leprol 2010; 76: 662–665. [DOI] [PubMed] [Google Scholar]
- 21. Itani S, Arabi A, Harb D, et al High prevalence of metabolic syndrome in patients with psoriasis in Lebanon: a prospective study. Int J Dermatol 2016; 55: 390–395. [DOI] [PubMed] [Google Scholar]
- 22. Kutlu S, Ekmekci TR, Ucak S, et al Prevalence of metabolic syndrome in patients with psoriasis. Indian J Dermatol Venereol Leprol 2011; 77: 193–194. [DOI] [PubMed] [Google Scholar]
- 23. Rosa DJ, Machado RF, Matias FA, et al Influence of severity of the cutaneous manifestations and age on the prevalence of several cardiovascular risk factors in patients with psoriasis. J Eur Acad Dermatol Venereol 2012; 26: 348–353. [DOI] [PubMed] [Google Scholar]
- 24. Chularojanamontri L, Wongpraparut C, Silpa‐Archa N, et al Metabolic syndrome and psoriasis severity in South‐East Asian patients: an investigation of potential association using current and chronological assessments. J Dermatol 2016; 43: 1424–1428. [DOI] [PubMed] [Google Scholar]


