Abstract
Background
Recent years have seen a marked increase in laser-pointer-related injuries, which sometimes involve severe retinal damage and irreversible visual impairment. These injuries are often caused by untested or incorrectly classified devices that are freely available over the Internet.
Methods
We reviewed pertinent publications retrieved by a systematic search in the PubMed and Web of Science databases and present our own series of clinical cases.
Results
We identified 48 publications describing a total of 111 patients in whom both acute and permanent damage due to laser pointers was documented. The spectrum of damage ranged from focal photoreceptor defects to macular foramina and retinal hemorrhages associated with loss of visual acuity and central scotoma. On initial presentation, the best corrected visual acuity (BCVA) was less than 20/40 (Snellen equivalent) in 55% of the affected eyes and 20/20 or better in 9% of the affected eyes. Treatment options after laser-pointer-induced ocular trauma are limited. Macular foramina and extensive hemorrhages can be treated surgically. In our series of 7 cases, we documented impaired visual acuity, central visual field defects, circumscribed and sometimes complex changes of retinal reflectivity, and intraretinal fluid. Over time, visual acuity tended to improve, and scotoma subjectively decreased in size.
Conclusion
Laser pointers can cause persistent retinal damage and visual impairment. In view of the practically unimpeded access to laser pointers (even high-performance ones) over the Internet, society at large now needs to be more aware of the danger posed by these devices, particularly to children and adolescents.
Lasers have become an indispensable part of everyday life. They are used in a variety of applications in modern medicine and industry, as well as for private purposes. Due to a significant cost reduction in recent years, reasonably priced high-power laser diodes in the form of laser pointers have become available. The ease with which these can be obtained through allegedly safe online shops has also contributed to a rise in their use. However, laser pointers purchased online often prove to be untested direct imports. An increased incidence of laser pointer attacks both in public and in private has lead to greater public and scientific interest in laser pointer injury (1).
Depending on wavelength, radiation power, exposure time, localization, and spot size, laser pointers can cause extensive photothermal injury to the eye, which can lead to blindness. The retina is the primary site of injury caused by photocoagulation. The blink reflex and aversion responses are protective mechanisms against injury caused by devices with a radiation output of less than 1 mW (2). This class of laser only causes damage if the exposure time exceeds 0.25 s, which approximately corresponds to the time lag of the natural blink reflex (according to DIN EN 60825–1). However, only part of the population can be expected to have this blink reflex, meaning that these natural protective mechanisms are inadequate (3).
Although the optical radiation output of laser pointers is officially regulated (4) and tested laser pointers should not exceed a power of 1 mW (2)—which is comparatively harmless under most conditions—untested and incorrectly classified devices pose a risk of permanent retinal injury. These devices, which are usually operated with standard batteries, frequently emit light in the green spectrum at an output often significantly exceeding permitted limits (5). In addition, non-certified green laser pointers, in contrast to red laser pointers, are able to emit light at different wavelengths, including invisible infrared radiation (6).
This article presents data from a systematic literature review and describes the morphological and functional characteristics of retinal injury caused by laser pointers with prohibited power output levels in seven children. The objective of the article is to draw attention to the potential hazard posed by laser pointers and to raise awareness of these dangers among children and adolescents in particular.
Methods
Literature search strategy and inclusion/exclusion criteria
This systematic review was compiled according to the PRISMA criteria (7) and included an electronic literature search in PubMed and Web of Science up to and including January 2017 using the keywords “laser pointer retina,” “laser pointer maculopathy,” “laser pointer eye,” and “laser pointers.”
Case reports and case series reporting original clinical data on laser pointer-induced retinal injuries were included in the analysis. Anatomical or theoretical articles, as well as articles not published in German or English, were excluded. Two independent reviewers (JB, PH) identified suitable studies according to the criteria listed below on the basis of title and abstract, as well as the full text of articles where necessary.
Patients
Seven patients that presented to the Department of Ophthalmology, University of Bonn, Bonn, Germany and the Department of Ophthalmology, St. Franziskus Hospital, Münster, Germany, following laser pointer injury were included in the analysis. The diagnosis of laser-induced retinopathy was based on patient medical history and morphological changes consistent with this diagnosis.
Clinical examination and imaging
All patients underwent a standardized clinical examination and retinal imaging. Some patients underwent (micro-)perimetry, as well as fluorescein angiography or full-field electroretinography (ERG).
Results
Literature search
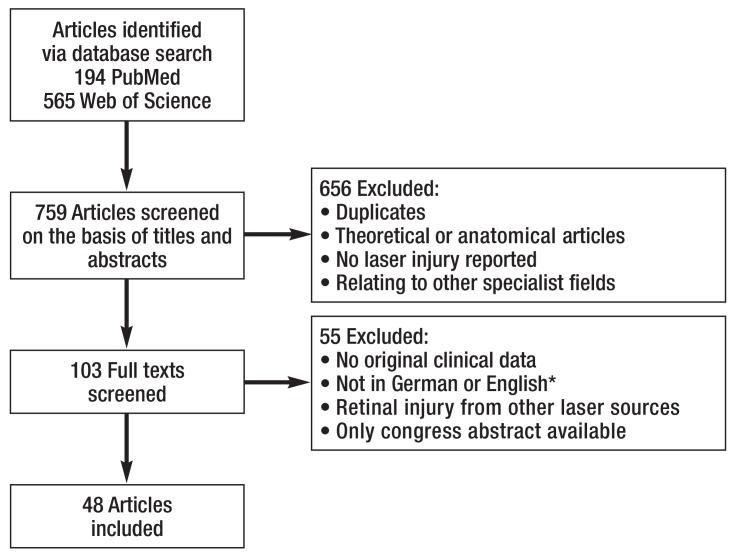
The systematic literature search identified a total of 48 articles that met the inclusion criteria (Figure).
Figure.
PRISMA flow diagram of the literature search
*Six publications were excluded primarily for language reasons
Study characteristics
Of the articles included, 41 came from Europe, North America, or Australia, while seven came from the Middle East or Asia. Since 2000, there has been an increase in reported cases alongside an increase in the number of published articles. A total of 111 cases were documented (average: 2.7 patients per study, range 1–17 patients). Overall, 45 reports included follow-up, ranging from a few days to 4 years (36 cases >6 months). As far as reported, 26 patients exhibited bilateral, 32 right-sided, and 27 left-sided injury. With regard to the laser pointers reported, 51% of injuries were caused by blue, 28% by green, and 21% by red laser pointers. The radiation output power of the measured laser pointers (n = 33) ranged from less than 5 mW (n = 11) to over 1000 mW (n = 3). Upon presentation, best corrected visual acuity (BCVA) was reduced to less than 20/40 (Snellen equivalent) in 55% of eyes, 5% of eyes showed reduced visual acuity of finger counting, while BCVA was 20/20 in 9% of eyes. The reasons for this pronounced visual loss included hemorrhage and extensive injury due to prolonged exposure. Central scotoma was described in 37 patients. Fundoscopy findings included circumscribed yellowish lesions in the area of the fovea (n = 37) (8– 12), hemorrhage (n = 16) (12– 16), pigment changes (hypo- and hyperpigmentation) (n = 59) (14, 16– 22), as well as macular hole formation (n = 26) (12, 13, 23– 26). Table 1 provides an overview of findings.
Table 1. Visual acuity and common injury patterns following laser pointer exposure*.
| Visual acuity following laser pointer injury | ||||
| Total number of eyes | Counting fingers | <20/40 | >20/40 | 20/20 |
| 137 | 9 | 75 | 62 | 12 |
| Most frequently described fundoscopic changes following laser pointer injury | ||||
| Total number of patients | Yellow foveal lesions | Hemorrhage | Pigment changes | Macular holes |
| 111 | 37 | 16 | 59 | 26 |
* In a first step, the visual acuity (Snellen equivalent) of all eyes was divided into two groups (<20/40 and >20/40); therefore, patients with a visual acuity of counting fingers were also classified into the <20/40 group and patients with a visual acuity of 20/20 into the >20/40 group.
High-resolution optical coherence tomography (OCT) demonstrated morphological retinal changes such as focal loss or disruption of retinal layers (8, 9, 11, 17, 18, 21, 22), macular holes (12, 13, 23, 24, 26), and cystoid changes or thickening (12, 17, 19) in all patients. Findings associated with prolonged exposure additionally showed streak lesions and, subsequently, fibrotic changes (27). ERG revealed no pathological changes (21).
A number of articles (9– 11, 16) have reported the use of prednisolone in different strengths both topically and systemically. In the long-term follow-up (>6 months), 28 of 36 patients showed an increase in visual acuity, while other patients showed stable visual acuity. OCT revealed persistent retinal defects; no cases of full recovery have been described as of yet.
Case reports
Patient characteristics are summarized in Table 2. All children and adolescents (five boys, two girls) reported receiving a laser pointer beam in the eyes while playing and, at initial presentation, described disturbing central visual field deficits in the affected eye, which occurred immediately following laser exposure. Although these could not be quantified using conventional perimetry, they were demonstrated using Amsler grid testing and microperimetry.
Table 2. Characteristics of the patients included*.
|
Patient (P) |
Age (years) |
Reason for referral | Symptoms | Eye |
Visual acuity (Snellen equivalent) |
Morphological changes |
Laser pointer output/ wavelength |
Initial presentation (month/ year) |
Follow-up interval (months) |
Visual acuity at follow-up |
| P1 | 12 | Emergency presentation |
Scotoma, reduced vision |
OS | 20/50 | Yellow lesion, pigment changes, intraretinal fluid | 45 mW 540 nm |
12/2014 | 20 | 20/20 |
| P2 | 15 | Emergency presentation |
Scotoma | OD/OS | OD: 20/20OS: 20/25 | Yellow lesion, pigment changes, structural loss of the outer retina | 92 mW 540 nm |
10/2014 | 33 | OD:20/20 OS: 20/20 |
| P3 | 15 | Emergency presentation |
Scotoma | OS | 20/20 | Pigment changes, structural loss in the outer retina | 65 mW 540 nm |
07/2014 | 1 | 20/20 |
| P4 | 9 | Suspected inherited retinal dystrophy (Stargardt’s disease) |
Scotoma | OD | 20/25 | Structural loss in the outer retina | 95 mW 532 nm |
02/2016 | 11 | 20/16 |
| P5 | 13 | Incidental finding of retinal edema |
Scotoma, incidental finding |
OS | 20/20 | Structural loss in the outer retina | 32 mW 540 nm |
06/2015 | 20 | 20/16 |
| P6 | 15 | Suspected macular dystrophy |
Scotoma | OD/OS | OD: 20/25OS: 20/25 | Pigment changes, structural loss in the outer retina | NP | 05/2016 | – | – |
| P7 | 13 | Suspected macular dystrophy |
Scotoma | OD | OD: 20/25 | Pigment changes, structural loss in the outer retina | NP | 06/2016 | – | – |
* Multimodal retinal imaging included high-resolution optical coherence tomography (OCT), fundus autofluorescence, infrared reflections, and multicolor imaging (each using Spectralis HRA + OCT, Heidelberg Engineering) and fundus photography (Zeiss, Visucam).
Humphrey visual field analysis (30–2) or fundus-controlled (micro-)perimetry (CenterVue SpA) was performed in individual patients to detect scotoma.
The spectral composition (central wavelength) and optical radiation output of the laser pointers were measured using a spectroradiometer (PR-655, Photo Research) and a silicon photodiode power meter (PM320E+S121C, Thorlabs) under controlled conditions (darkened room, at maximum laser pointer supply voltage) in repeated measurements
NP, not performed; OS, left eye; OD, right eye
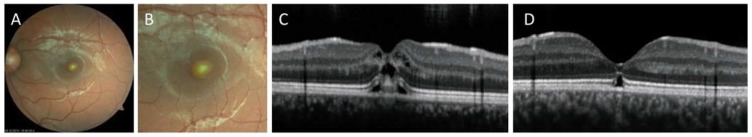
OCT imaging showed altered retinal reflectivity in all patients. Cystoid macular edema was detected in two patients by OCT. Fundoscopy revealed striking circumscribed, yellowish lesions and pigment changes; however, no bleeding was observed in the foveal region. Although anatomical changes to the inner retinal layers normalized to a large extent during the course of follow-up, lesions in the outer retina and retinal pigment epithelium persisted in all children (Figure). No patients exhibited secondary complications such as choroidal neovascularization during the follow-up period. Visual acuity increased in all patients, but the reported central visual field deficits persisted.
The laser pointers were purchased over the Internet in six cases and at a street market in one case. The optical radiation output power could be measured in five cases, all green laser pointers (central wavelength: 532–540 nm, likely generated by infrared-pumped laser diode technology). Peak values reached 32–95 mW (maximum value at a measuring time of at least 10 s) (Table 2). The radiation output power was either not given at all or labeled incorrectly on all devices.
Discussion
Laser pointer glare and retinal injuries caused by laser pointers have increased considerably in recent years and now represent a relevant problem. For example, the German Air Traffic Control (Deutsche Flugsicherung) reports more than 500 cases of laser glare to the police annually (personal communication, Ute Otterbein, German Air Traffic Control Press Office), while the US Federal Aviation Administration has documented a significant increase in glare since 2004 (2004: 46 cases, 2016: 7442 cases). However, besides the systematic documentation of incidents in aviation, a high number of unreported glare incidents and injuries can be assumed both in the public and the private setting. For example, an increasing number of case reports on laser pointer injury have been published in recent years (2005–2010: six publications, 2011–2016: 36 publications). Likewise, a growing number of children and adolescents have presented to the authors‘ hospital in recent years with retinal injury following laser pointer misuse. The frequency of these injuries points to the ease with which even high-powered laser pointers can be obtained, their frequent misrepresentation as a toy, and the lack of awareness about the hazards they pose. For example, the actual output power of the laser pointers investigated at our institution differed by as much as a hundred-fold from the power output stated on the label. In one case, the laser was correctly labeled as <200 mW, but, as such, should not have been available for sale in Germany.
Lasers, and thus also laser pointers, are classified according to the European standard DIN EN 60825–1 in the “Technical specification on lasers as or in consumer products” issued by the German Federal Institute for Occupational Safety and Health (Bundesanstalt für Arbeitsschutz und Arbeitsmedizin) (28) (Table 3), and the handling of lasers is regulated by the German Employers‘ Liability Insurance Associations. However, the legal situation appears to be inadequate in terms of the purchase and possession of laser pointers. Although only laser pointers up to laser class 2 (<1 mW) are allowed to be sold to private individuals in Germany and the distributor is obliged to provide instructions for use and correct labeling, laser pointers with significantly higher output powers or incorrectly labeled output powers are no rarity, not least due to online shops. Since laser pointers do not fall under the Weapons Act, the possession of even high-powered laser pointers is not punishable by law unless a third party is affected. Therefore, the German Radiation Protection Commission recommends that the possession and purchase of class 3B and class 4 laser pointers be regulated by law in order to prevent misuse. Due to their hazard potential, class 3B and 4 laser pointers should be classified accordingly, e.g., as weapons (29).
Table 3. Laser pointer classification according to the European standard DIN EN 60825–1 (28).
| Laser class | Hazard or potential for injury |
Typical ouptput power P (continuous wave laser) |
Typical use |
| 1 | Safe under reasonably foreseeable conditions | P <0.4 mw | Scanner checkouts, DVD players |
| 1M | Hazardous to the eye when using telescopic optical instruments (otherwise as in class 1) | P <0.4 mw; but the beam diameter is greater than 7 mm | |
| 2 | Direct intrabeam viewing must be avoided—retinal injury is possible at intrabeam viewing times exceeding 0.25 s |
P <1 mw | Laser pointers, laser spirit levels |
| 2M | Hazardous to the eye when using telescopic optical instruments (otherwise as in class 2) |
P <1 mw; but the beam diameter is greater than 7 mm |
|
| 3A | Hazardous to the eye only when using telescopic optical instruments |
P <5 mw; but the beam diameter is greater than 7 mm and the power density is related to the same pupil diameter as in class 2 lasers | |
| 3R | Hazardous to the eye | P <5 mw | Show and projection lasers, material processing lasers |
| 3B | Always hazardous to the eye | P <500 mw | |
| 4 | Always hazardous to the eye and skin | P >500 mW |
Laser pointer glare usually causes temporary loss of vision, which can result, e.g., in pilots‘ reduced capacity to coordinate tasks, but does not cause functional or morphological damage to the eye. In contrast, laser pointer misuse can cause irreversible retinal damage. This depends on the wavelength, radiation output power, duration of exposure, spot size of the laser, and the localization of damage (30). In principle, light can cause thermal, photomechanical, and photochemical damage to the retina. Laser pointer injuries primarily involve photothermal damage. This is more pronounced in short-wavelength light (green laser pointer; wavelength 490–575 nm) compared with long-wavelength light (red laser pointer; wavelength 635–750 nm) (19). The radiant energy absorbed by tissue causes local tissue to heat-up, which can lead to protein denaturation, loss of cell integrity, and secondary inflammatory reactions. Retinal pigment epithelium contains large amounts of melanin, which functions as a light absorber under physiological conditions and is also the largest absorber of energy in laser exposure. As such, the retinal pigment epithelium is assumed to be the site of greatest damage (31); however, the vulnerable photoreceptors located apically in its immediate vicinity are also at risk (32).
The eye‘s vulnerability to laser radiation has been evidenced by accidents in laboratories, industry, therapeutic applications, and in the military environment. The effects of laser exposure have been investigated experimentally in a monkey model (32); in humans, photocoagulation could be induced at an exposure time of less than 10 s and a power of 5 mW (20) or at a higher output and shorter exposure time (18, 33).
The morphology of retinal injuries caused by laser pointers is higly variable. Using multimodal imaging, including OCT, injuries can be detected and closely followed-up. During the acute stage and in addition to disruption of the retinal pigment epithelium, the outer retina frequently exhibits hyperreflectivity, accompanied by persistent disruption of the outer retinal layers (8, 9). Laser-induced macular holes may develop directly following exposure or in the further course (12, 26, 30, 34, 35). In some cases, these close up without intervention (26, 36). However, if macular holes persist, surgical intervention may achieve an increase in visual acuity (12, 26). Although none of our patients exhibited post-exposure retinal hemorrhage, hemorrhage has been described in different retinal layers elsewhere (12– 16, 37). Apart from focal retinal defects caused by laserpointer, streak-like lesions have been described as well. Whereas focal lesions often indicate accidental injury or injury caused by a third party, streak lesions can point to self-inflicted injury (27).
Possible differential diagnoses of laser pointer injuries include retinal dystrophies, as well as inflammatory and ischemic retinopathies. Zhang et al. described five patients investigated to rule out retinal dystrophy, all of whom had laser pointer-related phenocopies of retinal dystrophies (21). Even in the case of insufficient patient history, laser pointer injuries can be differentiated from genetic retinal diseases using multimodal imaging rather than genetic diagnostic testing. Laser pointer injury findings remain stable following acute damage, whereas genetic retinal diseases are characterized by bilaterality and slow progression. Furthermore, electrophysiological investigation techniques can provide the key to diagnosis.
An increase in visual acuity was observed in all our patients during the course of treatment, which is consistent with reports in the literature (10, 15, 16, 21). The clinical course of laser pointer injury is characterized by a sudden visual deterioration, followed by an increase in visual acuity over a number of weeks. However, this depends on the extent and location of retinal damage, as well as possible complications, and some patients experience long-term visual impairment (38). Even in the case of good visual acuity, damage close to the fovea and the resultant scotoma can lead to permanent impairment in everyday life
Laser pointer injury rarely leads to secondary complications. Laser-induced perforation of Bruch‘s membrane can cause secondary choroidal neovascularizations (CNV) up to years after laser pointer injury (16, 37). Experimental use has been made of this in a mouse model of CNV to study age-dependent macular degeneration (AMD) (39).
The treatment options for laser pointer injuries are limited. Systemic corticosteroids were used in differing regimes and with differing results following exposure; however, there are no clear recommendations on management as yet (9, 30). The systemic use of corticosteroids showed a protective effect in animal models (40). An experimental monkey model using methylprednisolone showed enhanced photoreceptor survival following laser injury (40). Systematic studies that demonstrate a functional improvement are challenging to design and lacking to date. Due to the generally favorable natural course, it is difficult to judge whether treatment is superior to a natural course. Although none of our patients received systemic corticosteroid treatment, a detailed discussion of this generally well tolerated treatment option should be conducted with the patient. Should CNV develop, intravitreal injection of vascular endothelial growth factor (VEGF) inhibitors is indicated (16).
In summary, powerful laser pointers pose a considerable hazard to the eye, and injury can be diagnosed using multimodal imaging and followed-up in the long term. Even if most retinal injury is partially reversible, surgical intervention involving pars plana vitrectomy may be necessary in some cases. Persistent retinal damage is evident on the retina and functional impairment may persist for a prolonged period of time. In addition to potential governmental regulatory measures, public awareness of laser pointer injuries needs to be heightened. Physicians from a variety of disciplines can make a valuable contribution in this regard.
Figure:
Funduscopy and OCT findings at initial presentation and follow-up of patient 1 (left eye) following laser pointer injury.
A + B) Yellowish lesions and pigment epithelial changes in the macular region were observed by fundoscopy at initial presentation.
C) OCT detected changes in retinal reflectivity and intraretinal fluid.
D) Persistent retinal changes were observed over the 20-month follow-up period.
Key Messages.
Laser pointers commercially available in Europe can have dangerously high output powers and may be misclassified.
The natural blink reflex and aversion responses are only partially able to protect against injury from laser pointers up to laser class 2 (<1 mW).
The spectrum of acute symptoms of laser pointer injury includes reduced visual acuity, retinal hemorrhage, and macular hole formation, whereby persistent retinal damage involving central scotoma is possible. Complications can occur as late as years after injury.
If injury is limited, the natural course is mostly favorable and visual acuity may recover. The use of corticosteroids has been described, while surgical intervention may be necessary in the case of extensive bleeding or macular holes.
In Internet online shops, high power laser pointers are readily accessible, and there are currently no adequate access controls in place. Social awareness of the hazards they pose needs to be heightened, particularly among children.
Acknowledgments
Translated from the original German by Christine Schaefer-Tsorpatzidis.
Our sincere thanks go to Dr. Georg Spital and Dr. Benedikt Book at the Department of Ophthalmology, St. Franziskus Hospital, Münster, Germany, for providing two patient cases involving laser pointer injuries. We would also like to thank them for their well-founded input during the revision of the manuscript.
We would also like to thank Niklas Domdei at the Department of Ophthalmology, University of Bonn, Bonn, Germany for measuring the laser pointers.
Footnotes
Conflict of interests
The authors state that they have no conflict of interest.
References
- 1.Houston S. Aircrew exposure to handheld laser pointers: the potential for retinal damage. Aviat Space Environ Med. 2011;82:921–922. doi: 10.3357/asem.3070.2011. [DOI] [PubMed] [Google Scholar]
- 2.Bundesanstalt für Arbeitsschutz und Arbeitsmedizin. Technische Spezifikation zu Lasern als bzw. in Verbraucherprodukte(n) 2014. www.baua.de/DE/Themen/Anwendungssichere-Chemikalien-und-Produkte/Produktsicherheit/Laserprodukte/pdf/Technische-Spezifikation-Laser.html (last accessed on 2nd November 2017) [Google Scholar]
- 3.Reidenbach HD, Hofmann J, Dollinger K, Ott G. Abwendungsreaktionen des Menschen gegenüber sichtbarer Laserstrahlung Schriftreihe der Bundesanstalt für Arbeitsschutz und Arbeitsmedizin 2006. Bremerhaven: Wirtschaftsverlag NW. 2006 [Google Scholar]
- 4.International Electrotechnical Commission. Safety of laser products: part 1—equipment classification and requirements. IEC. 2014 60825-1. [Google Scholar]
- 5.Ajudua S, Mello MJ. Shedding some light on laser pointer eye injuries. Pediatr Emerg Care. 2007;23:669–672. doi: 10.1097/PEC.0b013e31814b2dc4. [DOI] [PubMed] [Google Scholar]
- 6.Hadler J Tobares EL, Dowell M. Random testing reveals excessive power in commercial laser pointers. J Laser Appl. 2013;25 032007. [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339 b2535. [PMC free article] [PubMed] [Google Scholar]
- 8.Lally DR, Duker JS. Foveal injury from a red laser pointer. JAMA Ophthalmol. 2014;132 doi: 10.1001/jamaophthalmol.2014.34. [DOI] [PubMed] [Google Scholar]
- 9.Hossein M, Bonyadi J, Soheilian R, Soheilian M, Peyman GA. SD-OCT features of laser pointer maculopathy before and after systemic corticosteroid therapy. Ophthalmic Surg Lasers Imaging. 2011;42 Online:e135–e138. doi: 10.3928/15428877-20111208-03. [DOI] [PubMed] [Google Scholar]
- 10.Dirani A, Chelala E, Fadlallah A, Antonios R, Cherfan G. Bilateral macular injury from a green laser pointer. Clin Ophthalmol. 2013;7:2127–2130. doi: 10.2147/OPTH.S53024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hohberger B, Bergua A. Selbst verursachte laserinduzierte Makulopathie im Jugendalter. Ophthalmologe. 2017;114 doi: 10.1007/s00347-016-0293-x. [DOI] [PubMed] [Google Scholar]
- 12.Alsulaiman SM, Alrushood AA, Almasaud J, et al. High-power handheld blue laser-induced maculopathy: the results of the King Khaled Eye Specialist Hospital Collaborative Retina Study Group. Ophthalmology. 2014;121:566–572 e1. doi: 10.1016/j.ophtha.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Shenoy R, Bialasiewicz AA, Bandara A, Isaac R. Retinal damage from laser pointer misuse—case series from the military sector in Oman. Middle East Afr J Ophthalmol. 2015;22:399–403. doi: 10.4103/0974-9233.159780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wyrsch S, Baenninger PB, Schmid MK. Retinal injuries from a handheld laser pointer. N Engl J Med. 2010;363:1089–1091. doi: 10.1056/NEJMc1005818. [DOI] [PubMed] [Google Scholar]
- 15.Kandari JA, Raizada S, Razzak AA. Accidental laser injury to the eye. Ophthalmic Surg Lasers Imaging. 2010::1–5. doi: 10.3928/15428877-20100215-26. [DOI] [PubMed] [Google Scholar]
- 16.Xu K, Chin EK, Quiram PA, Davies JB, Parke DW, Almeida DR. Retinal injury secondary to laser pointers in pediatric patients. Pediatrics. 2016;138 doi: 10.1542/peds.2016-1188. pii: e20161188. [DOI] [PubMed] [Google Scholar]
- 17.Turaka K, Bryan JS, Gordon AJ, Reddy R, Kwong HM, Sell CH. Laser pointer induced macular damage: case report and mini review. Int Ophthalmol. 2012;32:293–297. doi: 10.1007/s10792-012-9555-z. [DOI] [PubMed] [Google Scholar]
- 18.Ziahosseini K, Doris JP, Turner GS. Laser eye injuries Maculopathy from handheld green diode laser pointer. BMJ. 2010;340 doi: 10.1136/bmj.c2982. c2982. [DOI] [PubMed] [Google Scholar]
- 19.Robertson DM, McLaren JW, Salomao DR, Link TP. Retinopathy from a green laser pointer: a clinicopathologic study. Arch Ophthalmol. 2005;123:629–633. doi: 10.1001/archopht.123.5.629. [DOI] [PubMed] [Google Scholar]
- 20.Luttrull JK, Hallisey J. Laser pointer-induced macular injury. Am J Ophthalmol. 1999;127:95–96. doi: 10.1016/s0002-9394(98)00254-2. [DOI] [PubMed] [Google Scholar]
- 21.Zhang L, Zheng A, Nie H, et al. Laser-induced photic injury phenocopies macular dystrophy. Ophthalmic Genet. 2016;37:59–67. doi: 10.3109/13816810.2015.1059458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thanos S, Bohm MR, Meyer zu Horste M, Schmidt PF. Retinal damage induced by mirror-reflected light from a laser pointer. BMJ Case Rep. 2015 doi: 10.1136/bcr-2015-210311. pii: bcr2015210311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Petrou P, Patwary S, Banerjee PJ, Kirkby GR. Bilateral macular hole from a handheld laser pointer. Lancet. 2014;383 doi: 10.1016/S0140-6736(14)60757-1. [DOI] [PubMed] [Google Scholar]
- 24.Dhoot DS, Xu D, Srivastava S. High-powered laser pointer injury resulting in macular hole formation. J Pediatr. 2014;164 doi: 10.1016/j.jpeds.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 25.Simonett JM, Scarinci F, Labriola LT, Jampol LM, Goldstein DA, Fawzi AA. A case of recurrent, self-inflicted handheld laser retinopathy. J AAPOS. 2016;20:168–170. doi: 10.1016/j.jaapos.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 26.Alsulaiman SM, Alrushood AA, Almasaud J, et al. Full-thickness macular hole secondary to high-power handheld blue laser: natural history and management outcomes. Am J Ophthalmol. 2015;160:107–13 e1. doi: 10.1016/j.ajo.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 27.Bhavsar KV, Wilson D, Margolis R, et al. Multimodal imaging in handheld laser-induced maculopathy. Am J Ophthalmol. 2014;159:227–231. doi: 10.1016/j.ajo.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 28.Berufsgenossenschaft der Feinmechanik und Elektrotechnik. Betrieb von Lasereinrichtungen. Anwendung der Unfallverhütungsvorschrift „Laserstrahlung“ BGV B2 auf neue Laserklassen und MZB-Werte nach DIN EN 60 825-1(VDE 0837-1): 2001-11 [Google Scholar]
- 29.Strahlenschutzkommission Blendattacken durch Laser. Empfehlung der Strahlenschutzkommission 246 Sitzung der Strahlenschutzkommission am 02/03 Dezember 2010. www.ssk.de/SharedDocs/Beratungsergebnisse_PDF/2010/2010_12.pdf?__blob=publicationFile (last accessed on 25 September 2017) [Google Scholar]
- 30.Barkana Y, Belkin M. Laser eye injuries. Surv Ophthalmol. 2000;44:459–478. doi: 10.1016/s0039-6257(00)00112-0. [DOI] [PubMed] [Google Scholar]
- 31.Hunter JJ, Morgan JI, Merigan WH, Sliney DH, Sparrow JR, Williams DR. The susceptibility of the retina to photochemical damage from visible light. Prog Retin Eye Res. 2012;31:28–42. doi: 10.1016/j.preteyeres.2011.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marshall J, Hamilton AM, Bird AC. Histopathology of ruby and argon laser lesions in monkey and human retina A comparative study. Br J Ophthalmol. 1975;59:610–630. doi: 10.1136/bjo.59.11.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ueda T, Kurihara I, Koide R. A case of retinal light damage by green laser pointer (Class 3b) Jpn J Ophthalmol. 2011;55:428–430. doi: 10.1007/s10384-011-0031-5. [DOI] [PubMed] [Google Scholar]
- 34.Bernstein PS, Steffensmeier A. Optical coherence tomography before and after repair of a macular hole induced by an unintentional argon laser burn. Arch Ophthalmol. 2005;123:404–405. doi: 10.1001/archopht.123.3.404. [DOI] [PubMed] [Google Scholar]
- 35.Mainster MA, Stuck BE, Brown J. Assessment of alleged retinal laser injuries. Arch Ophthalmol. 2004;122:1210–1217. doi: 10.1001/archopht.122.8.1210. [DOI] [PubMed] [Google Scholar]
- 36.Thach AB, Lopez PF, Snady-McCoy LC, Golub BM, Frambach DA. Accidental Nd: YAG laser injuries to the macula. Am J Ophthalmol. 1995;119:767–773. doi: 10.1016/s0002-9394(14)72783-7. [DOI] [PubMed] [Google Scholar]
- 37.Fujinami K, Yokoi T, Hiraoka M, Nishina S, Azuma N. Choroidal neovascularization in a child following laser pointer-induced macular injury. Jpn J Ophthalmol. 2010;54:631–633. doi: 10.1007/s10384-010-0876-z. [DOI] [PubMed] [Google Scholar]
- 38.Sethi CS, Grey RH, Hart CD. Laser pointers revisited: a survey of 14 patients attending casualty at the Bristol Eye Hospital. Br J Ophthalmol. 1999;83:1164–1167. doi: 10.1136/bjo.83.10.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lambert V, Lecomte J, Hansen S, et al. Laser-induced choroidal neovascularization model to study age-related macular degeneration in mice. Nat Protoc. 2013;8:2197–2211. doi: 10.1038/nprot.2013.135. [DOI] [PubMed] [Google Scholar]
- 40.Brown J, Hacker H, Schuschereba ST, Zwick H, Lund DJ, Stuck BE. Steroidal and nonsteroidal antiinflammatory medications can improve photoreceptor survival after laser retinal photocoagulation. Ophthalmology. 2007;114:1876–1883. doi: 10.1016/j.ophtha.2007.04.035. [DOI] [PubMed] [Google Scholar]