The mysterious phenomenon known as the nocebo effect describes the effects of negative expectancies. This is in contrast to positive expectations that trigger placebo effects (1). In evolutionary terms, nocebo and placebo effects coexist to favor perceptual mechanisms that anticipate threat and dangerous events (nocebo effects) and promote appetitive and safety behaviors (placebo effects). In randomized placebo-controlled clinical trials, patients that receive placebos often report side effects (nocebos) that are similar to those experienced by patients that receive the investigational treatment (2). Information provided during the informed consent process and divulgence of adverse effects contribute to nocebo effects in clinical trials (1). Nocebo (and placebo) effects engage a complex set of neural circuits in the central nervous system that modulate the perception of touch, pressure, pain and temperature (1, 3, 4). Commercial features of drugs such as price and labeling influence placebos (5, 6). On page 105 of this issue, Tinnermann et al. (7) show that price also impacts nocebo effects.
Tinnermann et al. evaluated the responses of healthy participants who received two placebo creams labeled with two distinct prices and presented in two boxes that had marketing characteristics for expensive and cheap medication. The creams were described as products that relieve itch but induce local pain sensitization (hyperalgesia). All creams, including controls, were identical and contained no active ingredients. Nocebo hyperalgesic effects were larger for the “more expensive” cream than for the “cheaper” cream. Combined cortico-spinal imaging revealed that the expensive price value increased activity in the prefrontal cortex. Furthermore, brain regions such as the rostral anterior cingulate cortex (rACC) and the periacqueductal gray (PAG), encoded the differential nocebo effects between the expensive and cheaper treatments. Expectancies of higher pain-related side effects associated with the expensive cream may have triggered a facilitation of nociception processes at early subcortical areas and the spinal cord [which are also involved in placebo-induced reduction of pain (8)]. The rACC showed a deactivation and favored a subsequent activation of the PAG and spinal cord resulting in an increase of the nociceptive inputs. This finding suggests that the rACC-PAG-spinal axis may orchestrate the effects of pricing on nocebo hyperalgesia (see the figure).
Figure 1.
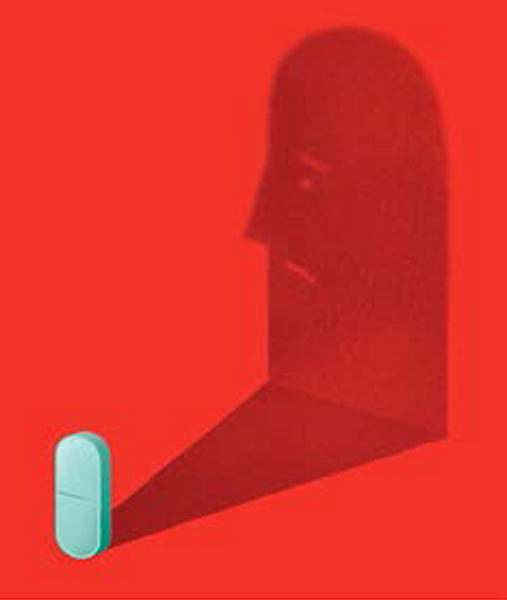
Medication price and labeling create expectancies of side effects that can lead to nocebo hyperalgesia that is in turn, mediated by an activation of the rACC-PAG-spinal cord coupling.
The anticipation of forthcoming painful stimulation makes healthy study participants perceive non-painful and low-painful stimulations as painful and high-painful, respectively (9). Verbally-induced nocebo effects are as strong as those induced through actual exposure to high pain (9). Moreover, receiving a placebo after simulating an effective analgesic treatment compared to receiving the same placebo intervention after a treatment perceived as ineffective produce a 49.3% versus 9.7% placebo induced pain reduction, respectively (10). The relationship between prior either unsuccessful or successful pain relief interventions and placebo analgesic effects is linked to a higher activation of the bilateral posterior insulae, and reduced activation of the right dorsolateral prefrontal cortex (11).
Informing patients that a treatment has been stopped, compared to a covert treatment interruption, impacts the response to morphine, diazepan or deep brain stimulation in post-operative acute pain, anxiety or idiopathic Parkinson’s disease, respectively (12). Patients openly informed about the interruption of each intervention experience a sudden increase of pain, anxiety or bradykinesia (a manifestation of Parkinson’s disease), whereas a hidden interruption does not (12). Neuroimaging approaches support the clinical observation. For example, the action of the analgesic, remifentanil, is over-ridden by activation of the hippocampus that occurs when healthy participants that receive heat painful stimulations are misleadingly told that the remifentanil administration was interrupted (13). These findings provide evidence that communication of treatment discontinuation might at least in part, lead to nocebo effects with aggravation of symptoms.
In placebo-controlled clinical trials, nocebo effects can influence patients’ clinical outcomes and treatment adherence. The Lipid-Lowering Arm of the Anglo-Scandinavian Cardiac Outcomes Trial shows that atorvastatin induced in the same individuals an excess rate of muscle-related adverse events in the non-blinded (ie. patients knew they were taking atorvastatin) non-randomized three year follow-up phase but not in the initial blinded five year phase when patients and physicians were unaware of the treatment allocation (atorvastatin or placebo) (14). Misleading information about side effects for statins via public claims has led to treatment discontinuation and increased fatal strokes and heart attacks (14).
Given that nocebo effects contribute to perceived side effects and may influence clinical outcomes and patients’ adherence to medication we should consider how to avoid them in clinical trials and practices (15). For example, nocebo effects might be reduced by tailoring patient-clinician communication to balance truthful information about adverse events with expectations of outcome improvement, exploring patients’ treatment beliefs and prior negative therapeutic history, and paying attention to framing (ie, treatment description) and contextual effects (ie, price). Through an understanding of the physiological mechanisms, strategies could be developed to reduce nocebo effects.
Acknowledgments
This research is funded by the U.S. National Institutes of Health (NIDCR, R01DE025946, L.C.).
References
- 1.Colloca L, Miller FG. The nocebo effect and its relevance for clinical practice. Psychosom Med. 2011;73:598. doi: 10.1097/PSY.0b013e3182294a50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barsky AJ, Saintfort R, Rogers MP, Borus JF. Nonspecific medication side effects and the nocebo phenomenon. JAMA. 2002;287:622. doi: 10.1001/jama.287.5.622. [DOI] [PubMed] [Google Scholar]
- 3.Blasini M, Corsi N, Klinger R, Colloca L. Nocebo and pain: an overview of the psychoneurobiological mechanisms. PAIN Reports. 2017;2:e585. doi: 10.1097/PR9.0000000000000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tracey I. Getting the pain you expect: mechanisms of placebo, nocebo and reappraisal effects in humans. Nat Med. 2010;16:1277. doi: 10.1038/nm.2229. [DOI] [PubMed] [Google Scholar]
- 5.Waber RL, Shiv B, Carmon Z, Ariely D. Commercial features of placebo and therapeutic efficacy. JAMA. 2008;299:1016. doi: 10.1001/jama.299.9.1016. [DOI] [PubMed] [Google Scholar]
- 6.Kam-Hansen S, et al. Altered placebo and drug labeling changes the outcome of episodic migraine attacks. Sci Transl Med. 2014;6:218ra215. doi: 10.1126/scitranslmed.3006175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tinnermann A, Geuter S, Sprenger C, Finsterbusch J, Büchel C. Interactions Between Brain and Spinal Cord Mediate Value Effects in Nocebo Hyperalgesia. Science. 2017;358:105. doi: 10.1126/science.aan1221. [DOI] [PubMed] [Google Scholar]
- 8.Eippert F, Finsterbusch J, Bingel U, Buchel C. Direct evidence for spinal cord involvement in placebo analgesia. Science. 2009;326:404. doi: 10.1126/science.1180142. [DOI] [PubMed] [Google Scholar]
- 9.Colloca L, Sigaudo M, Benedetti F. The role of learning in nocebo and placebo effects. Pain. 2008;136:211. doi: 10.1016/j.pain.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Colloca L, Benedetti F. How prior experience shapes placebo analgesia. Pain. 2006;124, 126 doi: 10.1016/j.pain.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 11.Kessner S, Wiech K, Forkmann K, Ploner M, Bingel U. The Effect of Treatment History on Therapeutic Outcome: An Experimental Approach. JAMA Intern Med. 2013;1 doi: 10.1001/jamainternmed.2013.6705. [DOI] [PubMed] [Google Scholar]
- 12.Colloca L, Lopiano L, Lanotte M, Benedetti F. Overt versus covert treatment for pain, anxiety, and Parkinson's disease. Lancet Neurol. 2004;3:679. doi: 10.1016/S1474-4422(04)00908-1. [DOI] [PubMed] [Google Scholar]
- 13.Bingel U, et al. The effect of treatment expectation on drug efficacy: imaging the analgesic benefit of the opioid remifentanil. Sci Transl Med. 2011;3:70ra14. doi: 10.1126/scitranslmed.3001244. [DOI] [PubMed] [Google Scholar]
- 14.Gupta A, et al. Adverse events associated with unblinded, but not with blinded, statin therapy in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid-Lowering Arm (ASCOT-LLA): a randomised double-blind placebo-controlled trial and its non-randomised non-blind extension phase. Lancet. 2017;389:2473. doi: 10.1016/S0140-6736(17)31075-9. [DOI] [PubMed] [Google Scholar]
- 15.Colloca L, Finniss D. Nocebo effects, patient-clinician communication, and therapeutic outcomes. JAMA. 2012;307:567. doi: 10.1001/jama.2012.115. [DOI] [PMC free article] [PubMed] [Google Scholar]


