Abstract
The objective of the present study was to investigate the expression of S100B protein in serum of patients with brain metastases from small cell lung cancer (SCLC), and its clinical significance. A total of 138 patients with SCLC were selected from June 2013 to December 2015. Simultaneously, 138 healthy adult volunteers (healthy controls) were selected in the medical examination center of People's Hospital of Rizhao. Among the 138 patients with SCLC, 48 had liver metastases and 44 had brain metastases. Of the remaining 46 patients, 20 were initially diagnosed with SCLC and 26 underwent surgery and postoperative chemotherapy. The levels of serum S100B in patients and healthy controls were measured by ELISA, and analyzed by SPSS 20.0 statistical software. The serum S100B protein levels in patients with SCLC were significantly higher than those in healthy controls (p<0.05). Among the subgroups of patients with SCLC, the levels of serum S100B in patients with brain metastases were significantly higher than in the other subgroups (p<0.05). No significant differences were found between the other subgroups, except for the brain metastases group. We found that serum S100B protein expression levels were significantly reduced in patients with brain metastases after cobalt-60 radiotherapy (p<0.05). During follow-up, we found that higher expression of S100B protein was usually associated with poorer prognosis, higher mortality rate at 1 year, and lower survival rate. In conclusion, S100B protein can serve as a serological marker for brain metastases from SCLC, which provides important theoretical support for early detection of brain metastases.
Keywords: small cell lung cancer, brain metastases, S100B protein
Introduction
In many developed and developing countries, the occurrence and mortality from lung cancer rank in first place among all malignant tumors. In China, deaths caused by lung cancer account for 20% of total cancer deaths, and this represents the highest rates of occurrence and mortality in the world (1). Lung cancer can be divided into non-small cell lung cancer (SCLC) and SCLC according to the different pathological types. The occurrence of SCLC accounts for 13 to 20% of the total number of cases of lung cancer, and its occurrence is closely related to the intensity and duration of smoking (1–3). SCLC is characterized by rapid development and high invasion ability, and is often accompanied by secondary tumor syndrome and early metastasis. Therefore, distant metastases such as dangerous brain metastases, can often be found upon diagnosis of SCLC, and are associated with poor prognosis. In some patients, distant metastases serve as evidence for the initial diagnosis of SCLC (4). Therefore, the timely use of more sensitive methods to detect the degree of cancer metastasis is key to improving the prognosis of SCLC. Among various serological markers, S100B protein is a nervous system-specific protein. Generally, S100B protein is highly expressed in glial cells and Schwann cells (3). The amount of S100B in serum is very low under physiological conditions. However, serum S100B protein can increase in response to increased blood-brain barrier permeability caused by damaged nerve cells or other pathological conditions (2,3). For example, increased levels of serum S100B are detectable in patients with Alzheimer's disease (4).
This study aimed to provide theoretical support for the early detection of brain metastases by detecting the expression of serum S100B protein at different stages in patients with SCLC.
Patients and methods
Patients
A total of 138 patients who underwent single valve replacement surgery under general anesthesia were selected from June 2013 to December 2015. The mean age of patients was 66.5±9.8 years. The mean age of healthy controls was 67.3±12.1 years. This study was approved by the Ethics Committee of People's Hospital of Rizhao. Signed written informed consents were obtained from the patients.
Inclusion criteria
i) Patients with SCLC diagnosed by videography and pathology; and ii) patients who signed the informed consent.
Exclusion criteria
i) Patients treated with immunosuppressive agents; ii) patients with acute and chronic bacterial and/or viral infections; iii) patients with autoimmune diseases; iv) patients with connective tissue diseases; v) patients with malignant tumors; vi) patients with liver and kidney dysfunction; vii) patients with chronic muscular diseases; viii) patients with peripheral vascular diseases, chronic heart failure, thyroid diseases, liver and kidney dysfunction, liver and kidney tumors, severe trauma within the past 6 months, and those with history of surgery; ix) patients with diabetes mellitus; x) patients with New York cardiac function grade III or IV; xi) patients with myocardial infarction, percutaneous coronary angioplasty, and coronary artery bypass grafting; patients with recent use of adrenal cortex hormones or other immunomodulator drugs; and xii) patients and family members who failed in cooperation, and patients with a history of mental illness.
Sample collection
Fasting elbow vein blood (3 ml) was extracted in the morning, and collected in ordinary plastic tubes. A total of 1.8 ml of blood samples was placed in anti-coagulant tubes with 0.2 ml of 3.8% sodium citrate, followed by centrifugation (1116.2 × g) for 10 min at 1 h after collection. Serum was harvested, placed in 0.5 ml EP tubes, and stored at −30°C. Serum samples were tested within 1 month after extraction.
ELISA
i) Serum pretreatment, EDTA or heparin was used as anti-coagulant. After collection, samples were centrifuged (1,750 × g) for 30 min at 2–8°C; ii) ELISA plates were placed at room temperature for 20 min; iii) the wells for standards and samples were established, and 50 µl of standard solution was added to the standard wells; iv) a total of 50 µl of samples was added to sample wells, while blank wells were not treated; v) a total of 100 µl of horseradish peroxidase-labeled antibody was added to each well, and the samples were sealed and incubated in a thermostatic chamber for 60 min; vi) liquid was discarded, and 350 µl of washing solution was added and removed after 1 min. The washing step was repeated 4–5 times; vii) a total of 50 µl of solution A and 50 µl of solution B were added to each well at 37°C in the dark, and incubated for 15 min; viii) stop solution (50 µl) was added, and the absorbance (OD value) was measured at 450 nm within 15 min after adding the stop solution; and ix) a standard curve was constructed, and the levels of serum S100B were calculated. The ELISA kit was from Wuhan Boster Biological Engineering Co., Ltd. (Wuhan, China).
Classification of S100B protein expression level
Serum S100B protein expression levels were divided from + to ++++ as follows: +, 0–0.35 ng/µl; ++, 0.36–0.70 ng/µl; +++, 0.71–1.05 ng/µl; and ++++, 1.06–1.4 ng/µl.
Statistical analysis
SPSS 17.0 statistical software (IBM, Armonk, NY, USA) was used for data analysis. Numerical data are presented as mean ± standard deviation (mean ± SD). Repeated measures analysis of variance (ANOVA) was used to analyze the repeated measurements of data. The independent-samples t-test was used for comparisons between groups. The paired t-test was used for comparisons within groups. Categorical data were analyzed by χ2 test. P<0.05 was considered to indicate a statistically significant difference.
Results
Clinical staging of enrolled patients
Among the 138 patients with SCLC, 44 cases with brain metastases were identified. Other types of metastases were found in 48 cases. Of the remaining 46 cases, 20 were initially diagnosed with SCLC and without metastases, and 26 underwent surgery and postoperative chemotherapy. The remaining 26 cases underwent surgery and postoperative chemotherapy (Table I).
Table I.
Clinical staging of enrolled patients.
| Cases | Other types of metastases | Brain metastases | Initial diagnosis without metastases | Surgery and postoperative chemotherapy |
|---|---|---|---|---|
| 138 | 44 (32%) | 48 (35%) | 20 (14%) | 26 (19%) |
The expression of S100B in patients with SCLC and healthy controls
We found that serum S100B protein level was significantly higher in patients with SCLC compared with healthy controls (p<0.05) (Table II).
Table II.
The expression of S100B in patients with SCLC and healthy controls.
| Groups | Cases | Age (years) | BMI (kg/m2) | Course of disease (months) | S100B (ng/µl) |
|---|---|---|---|---|---|
| Patients with SCLC | 138 | 67.3±12.1 | 21.3±3.4 | – | 0.055±0.001 |
| Healthy controls | 138 | 66.5±9.8 | 20.9±2.1 | 8.2±3.9 | 1.243±0.427 |
| T-value | – | 1.28 | 2.12 | – | 21.87 |
| P-value | – | 0.32 | 0.14 | – | 0.002 |
SCLC, small cell lung cancer.
Subgroup analysis of SCLC patients
Among the subgroups of patients with SCLC, the levels of serum S100B in patients with brain metastases were significantly higher than in other subgroups (p<0.05). There were no significant differences in serum S100B protein level between the healthy control group and other subgroups, except the brain metastases group (p>0.05) (Table III).
Table III.
The comparison of S100B expression in SCLC subgroups.
| Subgroups | Cases | S100B (ng/µl) |
|---|---|---|
| Brain metastases | 48 | 2.138±0.174 |
| Other types of metastases | 44 | 0.203±0.106 |
| No metastases | 20 | 0.128±0.032 |
| Healthy control | 138 | 0.055±0.001 |
| F-value | – | 22.87 |
| P-value | – | 0.001 |
SCLC, small cell lung cancer.
The expression of S100B in patients with brain metastases from SCLC after exposure to cobalt-60. We found that the levels of S100B in patients with brain metastases from SCLC were significantly reduced after 3 weeks of cobalt-60 irradiation compared with those before treatment (p<0.05) (Table IV).
Table IV.
The expression of S100B in patients with brain metastases from SCLC after exposure to cobalt-60.
| Parameters | Cases | S100B (ng/µl) |
|---|---|---|
| Before treatment | 48 | 2.138±0.174 |
| After treatment | 48 | 1.017±0.212 |
| T-value | – | 31.82 |
| P-value | – | 0.005 |
SCLC, small cell lung cancer.
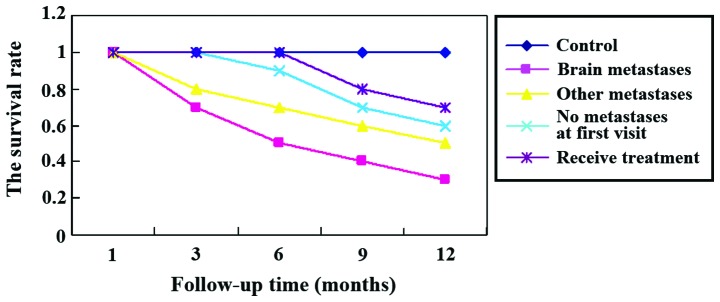
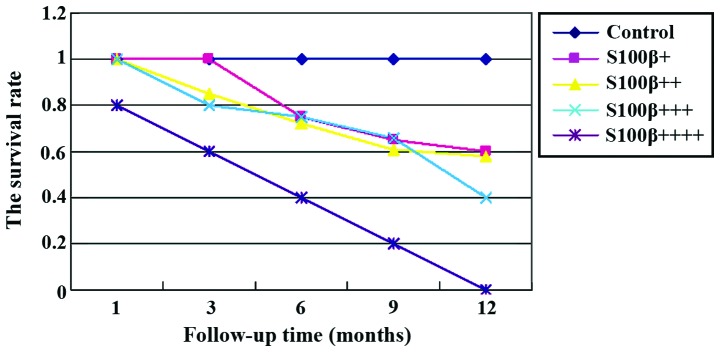
Survival analysis
At the 1 year follow-up, we found that the mortality rate of patients with brain metastases was significantly higher than that of other groups (p<0.05). Further statistical analyses showed that higher expression of S100B protein was usually associated with poorer prognosis, higher mortality rate at 1 year, and lower survival rate (Figs. 1 and 2).
Figure 1.
Survival analysis. The mortality rate of patients with brain metastases was significantly higher than that of other groups (p<0.05).
Figure 2.
The comparison of survival rates of patients with different levels of S100B. Statistical analysis showed that higher expression of S100B protein was usually associated with poorer prognosis, higher mortality rate at 1 year, and lower survival rate.
Discussion
SCLC accounts for roughly 20% of cases of lung cancer. SCLC generally presents with a high degree of malignancy, short doubling time, and early and extensive metastasis. SCLC is sensitive to chemotherapy and radiotherapy. The early remission rate is high. However, the drug resistance rate is also high, leading to a high recurrence rate. Systemic chemotherapy is the main method of treatment for SCLC. Each year, ~15% of newly diagnosed cases of lung cancer are SCLC. The incidence of SCLC increases with age, and ~45% of patients are over the age of 70 (1,2). Therefore, early diagnosis of SCLC metastasis is an area of intense research (5–8).
S100B is a 10.4 kDa protein expressed in astrocytes. Its main synthetic process is accomplished by synaptic nodules in the brain. It is one of the EF-hand proteins that belongs to the low molecular weight acidic calcium-binding protein superfamily (9). This protein is primarily metabolized by the kidneys, and the waste is excreted with urine. The expression levels of S100B are consistent among different races, and no differences in expression were found between males and females or between day and night (10). Although S100B is not specifically expressed in the central nervous system, its concentration in brain tissue is significantly higher than in other tissues (80–90% of S100B can be found in the brain). Therefore, the protein can serve as an early marker of brain injury (9). Besides the brain, S100B is synthesized in adipose tissue (11), skin melanoma (12,13) and T cells (14). The mechanism of secretion of S100B protein after activation of astrocytes remains unknown. The function of the S100B protein secreted by astrocytes depends on its concentration, it has a neurotrophic effect at low concentration (nmol), and is neurotoxic at high concentration (mmol) (9). At nanomolar levels, S100B has a stimulatory effect on astrocytes, and can induce glial hyperplasia in vitro (15).
Kawata et al reported that the S100B protein cooperates with other serological markers such as neuron-specific enolase, glial fibril acidic protein, and tau protein, and has good clinical value for the accurate diagnosis of mild traumatic brain injury (16). Duarte-Rojo et al found that serum S100B concentrations were significantly higher in patients with cirrhosis compared with those in healthy volunteers, and S100B concentrations were further increased with hepatic encephalopathy (17,18). Therefore, S100B, as a serological biomarker, may have important clinical significance for the early diagnosis of hepatic encephalopathy (17–20). We found that patients with brain metastases from SCLC were usually accompanied by varying degrees of increase of S100B protein expression. Moreover, the increased S100B protein was found not to be a marker for the early detection of other types of metastasis from SCLC. There were no differences in the levels of S100B between patients with non-brain metastases from SCLC and the healthy control group. This suggests that the increase of S100B protein level is more specific in brain metastases. In general, the sensitivities of imaging methods such as PET-CT are usually poor for the diagnosis of brain metastases, leading to misdiagnosis of early brain metastases, which in turn affect the quality of life of patients. In addition, we found that the level of serum S100B was closely related to prognosis, higher expression was associated with shorter survival time. Previous studies have shown that S100B can accumulate in the extracellular matrix after the death of astrocytes, or cell disintegration caused by substantial damage. Under these conditions, the S100B concentration is approximately at the micromolar level, and causes neurotoxicity (20). Therefore, large amounts of S100B protein aggregation not only cause neurotoxic damage, but also greatly reduce patient survival time. However, we found that S100B protein expression levels were reduced along with reduced nerve damage caused by cancer cells after radiotherapy. Therefore, we believe that serum S100B protein has important clinical significance for the early detection of brain metastases from SCLC.
In conclusion, S100B protein can be used as a serological marker for brain metastases from SCLC, and has important clinical value for the early detection of brain metastases.
References
- 1.Charpidou A, Tsagouli S, Gkiozos I, Grapsa D, Moutsos M, Kiagia M, Syrigos K. Bone metastases in patients with small cell lung carcinoma: Rate of development, early versus late onset, modality of treatment, and their impact on survival. A single-institution retrospective cohort study. Clin Exp Metastasis. 2016;33:453–460. doi: 10.1007/s10585-016-9789-7. [DOI] [PubMed] [Google Scholar]
- 2.Higgins E, Edwards G, Tanguay J, Button M. 93P: Chemoradiotherapy with radical intent for small cell lung cancer (SCLC): A 5 year retrospective review. J Thorac Oncol. 2016;11(Suppl 4):S97. doi: 10.1016/S1556-0864(16)30206-4. [DOI] [Google Scholar]
- 3.Peng L, Xu L, Ouyang W. Role of peripheral inflammatory markers in postoperative cognitive dysfunction (POCD): A meta-analysis. PLoS One. 2013;8:e79624. doi: 10.1371/journal.pone.0079624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scott DA, Evered LA, Silbert BS. Cardiac surgery, the brain, and inflammation. J Extra Corpor Technol. 2014;46:15–22. [PMC free article] [PubMed] [Google Scholar]
- 5.Potter DS, Galvin M, Brown S, Lallo A, Hodgkinson CL, Blackhall F, Morrow CJ, Dive C. Inhibition of PI3K/BMX cell survival pathway sensitizes to BH3 mimetics in SCLC. Mol Cancer Ther. 2016;15:1248–1260. doi: 10.1158/1535-7163.MCT-15-0885. [DOI] [PubMed] [Google Scholar]
- 6.Gridelli C, Casaluce F, Sgambato A, Monaco F, Guida C. Treatment of limited-stage small cell lung cancer in the elderly, chemotherapy vs. sequential chemoradiotherapy vs. concurrent chemoradiotherapy: That's the question. Transl Lung Cancer Res. 2016;5:150–154. doi: 10.21037/tlcr.2016.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi X, Duan H, Liu X, Zhou L, Liang Z. Genetic alterations and protein expression in combined small cell lung cancers and small cell lung cancers arising from lung adenocarcinomas after therapy with tyrosine kinase inhibitors. Oncotarget. 2016;7:34240–34249. doi: 10.18632/oncotarget.9083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahn S, Hwang SH, Han J, Choi YL, Lee SH, Ahn JS, Park K, Ahn MJ, Park WY. Transformation to small cell lung cancer of pulmonary adenocarcinoma: Clinicopathologic analysis of six cases. J Pathol Transl Med. 2016;50:258–263. doi: 10.4132/jptm.2016.04.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sen J, Belli A. S100B in neuropathologic states: The CRP of the brain? J Neurosci Res. 2007;85:1373–1380. doi: 10.1002/jnr.21211. [DOI] [PubMed] [Google Scholar]
- 10.Ikeda Y, Umemura K. Analysis of reference values of serum S100B concentrations of Japanese adults. Rinsho Byori. 2005;53:395–399. (In Japanese) [PubMed] [Google Scholar]
- 11.Hidaka H, Endo T, Kawamoto S, Yamada E, Umekawa H, Tanabe K, Hara K. Purification and characterization of adipose tissue S-100b protein. J Biol Chem. 1983;258:2705–2709. [PubMed] [Google Scholar]
- 12.Cocchia D, Michetti F, Donato R. Immunochemical and immuno-cytochemical localization of S-100 antigen in normal human skin. Nature. 1981;294:85–87. doi: 10.1038/294085a0. [DOI] [PubMed] [Google Scholar]
- 13.Kindblom LG, Lodding P, Rosengren L, Baudier J, Haglid K. S-100 protein in melanocytic tumors. An immunohistochemical investigation of benign and malignant melanocytic tumors and metastases of malignant melanoma and a characterization of the antigen in comparison to human brain. Acta Pathol Microbiol Immunol Scand A. 1984;92:219–230. [PubMed] [Google Scholar]
- 14.Takahashi K, Isobe T, Ohtsuki Y, Sonobe H, Yamaguchi H, Akagi T. S-100 protein positive human T-lymphocyte. Am J Clin Pathol. 1985;83:69–72. doi: 10.1093/ajcp/83.1.69. [DOI] [PubMed] [Google Scholar]
- 15.Selinfreund RH, Barger SW, Pledger WJ, Van Eldik LJ. Neurotrophic protein S100 beta stimulates glial cell proliferation. Proc Natl Acad Sci USA. 1991;88:3554–3558. doi: 10.1073/pnas.88.9.3554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kawata K, Liu CY, Merkel SF, Ramirez SH, Tierney RT, Langford D. Blood biomarkers for brain injury: What are we measuring? Neurosci Biobehav Rev. 2016;68:460–473. doi: 10.1016/j.neubiorev.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duarte-Rojo A, Ruiz-Margáin A, Macias-Rodriguez RU, Cubero FJ, Estradas-Trujillo J, Muñoz-Fuentes RM, Torre A. Clinical scenarios for the use of S100β as a marker of hepatic encephalopathy. World J Gastroenterol. 2016;22:4397–4402. doi: 10.3748/wjg.v22.i17.4397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee R, Yeung AW, Hong SE, Brose MS, Michels DL. Principles of medical oncology. Asian Pac J Surg Oncol. 2015;1:39–46. [Google Scholar]
- 19.Smithers BM, Li A, Kelly SL, Wilson MK, Chaturvedi A, Samoukovic K. Staging of non-small cell lung cancer and small cell lung cancer. Asian Pac J Surg Oncol. 2015;1:125–140. [Google Scholar]
- 20.Kowgier M, Qiu LA, Tse H. Surgery for small cell lung cancer. Asian Pac J Surg Oncol. 2015;1:171–180. [Google Scholar]