To the Editor: Primary central nervous system lymphoma (PCNSL) is defined as lymphoma confined to the brain, spinal cord, eye, or leptomeninges. Ocular involvement can be detected in about 20% of PCNSL patients with primary vitreous retinal lymphoma (PVRL), which is generally a high-grade diffuse large B-cell lymphoma, being the most common subtype. The incidence of PVRL is extremely low, with 300–380 new cases diagnosed each year in the United States, which is equivalent to an annual incidence of approximately 4.8 cases per million. PVRL typically affects seniors aged 60–85 years, while seldom occurs in younger patients.[1] Here, we report a case of young PVRL.
A 38-year-old male was presented to Department of Ophthalmology, Peking Union Medical College Hospital, with blurred vision and floaters in the right eye for 2 years. On admission, his best-corrected visual acuity was 0.01 in the right eye and 0.25 in the left eye; intraocular pressure was 16 mmHg in the right eye and 21 mmHg in the left eye; the right eye had mild anterior chamber inflammation with small mutton-fat keratic precipitates, 2+ flare, and 3+ cells, respectively [Figure 1a]; dilated examination revealed vitreous hemorrhage with invisible fundus [Figure 1b]; and no significant finding was noted in the left eye. B-scan ultrasound revealed vitreous opacity, retinal detachment, and subretinal lesions in the right eye. Diagnostic vitrectomy was performed in the right eye, and yellow-white lesions with massive preretinal hemorrhage were observed in the posterior pole [Figure 1c]. Vitreous cytology revealed large atypical lymphoid cells which were CD19+, CD20+, CD22+ on flow cytometry, and gene rearrangement analysis was positive for IgK. Interleukin (IL)-10 was 10576.11 pg/ml and IL-6 was 8414.36 pg/ml (IL-10/IL-6 ratio >1) in the aqueous humor. Optical coherence tomography (OCT) showed multiple hyperreflective signals in the inner retina and hyperreflective subretinal infiltration in the right eye [Figure 1d]. Brain magnetic resonance imaging was insignificant. All of the above lineages of evidences pointed to the diagnosis of PVRL in the right eye (diffuse large B-cell).
Figure 1.
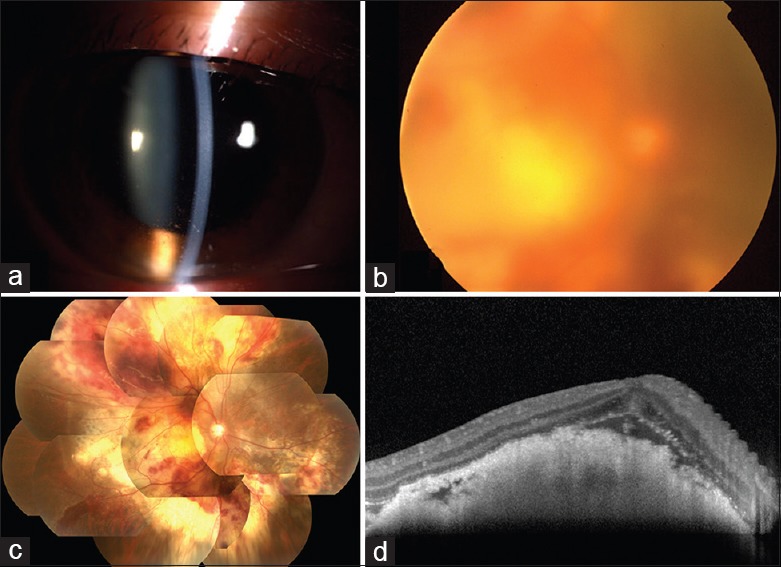
A 38-year-old male presenting with primary vitreous retinal lymphoma in the right eye. (a) Anterior segment photography of the right eye showed mild anterior chamber inflammation with small mutton-fat keratic precipitates, 2+ flare, and 3+ cells. (b) Fundus photography of the right eye revealed vitreous hemorrhage and a blurred fundus before surgery and (c) yellow-white lesions with massive preretinal hemorrhage in the posterior pole after vitrectomy. (d) Optical coherence tomography showed multiple hyperreflective signals in the inner retina and subretinal hyperreflective infiltration.
PVRL typically affects seniors aged 60–85 years although younger patients have been reported. Patients with PVRL may be unilaterally or bilaterally involved and usually present with painless loss of vision and floaters. Neurological symptoms such as personality alterations and changes in alertness may also be present when the central nervous system (CNS) is involved. Ophthalmic examination of PVRL typically reveals mild anterior chamber cells and more prominent vitreous cells with floating clumps. Typical fundus findings are scattered white-yellow lesions and subretinal or subpigment epithelial infiltrates.[1]
This patient, however, was a young male and was initially presented with vitreous hemorrhage and indiscernible fundus. The retinal lesions on B-scan ultrasound suggested the possibility of masquerade syndrome, which was later confirmed by an aqueous tap and a diagnostic vitrectomy. For patients with clear media, however, OCT and fundus fluorescein angiography (FFA) are also useful for diagnosis of PVRL and should be obtained immediately.[2]
The clinical picture of PVRL, however, is highly heterogeneous and often mimics other diseases such as chronic uveitis and acute retinal necrosis (ARN). Since uveitis and ARN are usually diagnosed based only on clinical manifestations, one should always keep in mind that PVRL is a potential masquerader, and when treatments are less effective than expected, efforts should be made in pursuit of evidences of PVRL in both the eyes and the CNS.
Although vitreous or retinal tissue biopsy combined with cytology is the gold standard for diagnosis of PVRL, neoplastic cells are very fragile and often mixed with nonneoplastic inflammatory cells, limiting the sensitivity of cytology ranging from 31% to 66.7%.[3] Fortunately, the sensitivity can be significantly improved by further analyses including immunohistochemistry, flow cytometry, cytokine analysis, and gene rearrangements by PCR. Cytokine analysis of vitreous fluid and aqueous humor has shown an elevated IL-10 >100 pg/ml or IL-10/IL-6 ratio >1 in B-cell PVRL.[4] In our case, although direct cytopathology was unavailable, the diagnosis of PVRL (diffuse large B-cell lymphoma) was established by multiple lineages of supportive evidences combining flow cytometry, gene rearrangement of vitreous specimen, and cytokine analysis of aqueous humor sample.
As for treatment of PVRL, intravitreal injection of methotrexate (MTX) or rituximab and ocular radiotherapy are recommended; in cases with CNS involvement, high-dose MTX combining other chemotherapeutic agents are suggested. These treatments have improved the survival of PVRL to more than 3 years.[5]
In conclusion, PVRL can present with a variety of clinical manifestations that mimic other diseases. A high index of suspicion and a close follow-up are essential for the diagnosis of PVRL. B-scan ultrasound, OCT, and FFA are useful to detect signs suggestive of PVRL, and multiple lineages of evidences including cytopathology, flow cytometry, gene rearrangement, and cytokine analysis are useful to establish a conclusive diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Xin Chen
REFERENCES
- 1.Chan CC, Rubenstein JL, Coupland SE, Davis JL, Harbour JW, Johnston PB, et al. Primary vitreoretinal lymphoma: A report from an International Primary Central Nervous System Lymphoma Collaborative Group symposium. Oncologist. 2011;16:1589–99. doi: 10.1634/theoncologist.2011-0210. doi: 10.1634/theoncologist.2011-0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Egawa M, Mitamura Y, Hayashi Y, Naito T. Spectral-domain optical coherence tomographic and fundus autofluorescence findings in eyes with primary intraocular lymphoma. Clin Ophthalmol. 2014;8:335–41. doi: 10.2147/OPTH.S58114. doi: 10.2147/OPTH.S58114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodriguez EF, Sepah YJ, Jang HS, Ibrahim M, Nguyen QD, Rodriguez FJ, et al. Cytologic features in vitreous preparations of patients with suspicion of intraocular lymphoma. Diagn Cytopathol. 2014;42:37–44. doi: 10.1002/dc.23059. doi: 10.1002/dc.23059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hwang CS, Yeh S, Bergstrom CS. Diagnostic vitrectomy for primary intraocular lymphoma: When, why, how? Int Ophthalmol Clin. 2014;54:155–71. doi: 10.1097/IIO.0000000000000022. doi: 10.1097/IIO.0000000000000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Omuro AM, DeAngelis LM, Yahalom J, Abrey LE. Chemoradiotherapy for primary CNS lymphoma: An intent-to-treat analysis with complete follow-up. Neurology. 2005;64:69–74. doi: 10.1212/01.WNL.0000148641.98241.5E. doi: 10.1212/01.WNL.0000148641.98241.5E. [DOI] [PubMed] [Google Scholar]


