To the Editor: A lumbar epidural block is used to treat patients with a herniated intervertebral disc, spinal stenosis, or lumbosacral radiculopathy. This approach reduces radicular pain by decreasing inflammation of nerve roots through epidural corticosteroid injection.[1] Patients with moderate-to-severe spinal stenosis who taking various anticoagulant agents have more risk for epidural hematoma. For patients on anticoagulation therapy, guidelines have been established to decrease the risk of bleeding and its potentially devastating complications. We report a case of an 81-year-old man with an unexpected lumbar epidural hematoma, who achieved a good outcome with conservative management.
An 81-year-old male visited our pain center with lower back pain and discomfort in both lower extremities of 20 years duration. Symptoms were more severe on the left side. The patient had received posterior lumbar interbody fusion on L3–L5 8 years ago. The initial pain intensity was 8/10 on the numeric rating scale for pain. He had been taking clopidogrel, aspirin, and beraprost following infrarenal abdominal aortic aneurysm repair since 2013. The chief complaint was of lower back pain with neurogenic claudication and numbness of the left buttock through the posterior thigh. On physical examination, there was no weakness in either legs, and Patrick's test was negative. In addition, there was no evidence of arteriosclerosis obliterans. He was taking 375 mg acetaminophen and 37.5 mg tramadol twice a day, gabapentin 400 mg/d, beraprost 20 mg/d, and oxycodone 5 mg for rescue medication. His coagulation profile was within normal limits after discontinuation of clopidogrel and aspirin for 7 days. Lumbar magnetic resonance imaging (MRI) showed bilateral foraminal stenosis, which was moderate on the left side. Electromyography showed no evidence of lumbosacral radiculopathy or peripheral neuropathy of the lower extremities.
We decided to perform lumbar interlaminar epidural nerve injections on L4–L5 level. The patient was placed in the prone position, and the lower back was prepared and draped in a sterile fashion. An epidural block was performed through the interlaminar space of L4–L5 with a blunt 22-gauge Tuohy needle using the paramedian approach. The epidural space was confirmed using a loss-of-resistance technique and fluoroscopic imaging. There was neither blood nor cerebrospinal fluid on aspiration. Five milliliters of injectate containing 3000 U hyaluronidase, 4 ml saline, 5 mg dexamethasone, and 5 ml 0.5% lidocaine was administered. A fluoroscope was used to confirm the depth and location, after which water-soluble contrast (Iobrix®) was injected, revealing bilateral epidural spread with no intrathecal, subdural, or intravascular uptake.
Three weeks after the epidural block, the patient reported severe worsening of the lower back pain and radiating left leg pain. An unpleasant tingling sensation and numbness in his left leg and buttock remained. Neurologic examination showed nonspecific findings. Magnetic resonance images were obtained immediately and showed an epidural hematoma of 1.4 cm × 4.1 cm at the L5–S1 level. The hematoma was large enough to cause severe thecal sac compression [Figure 1a and 1b]. The patient did not have symptoms of cauda equina syndrome or any neurological deficiency. More serious complications, such as epidural hematoma and epidural abscess, have been reported in epidural blocks with anticoagulation therapy. In collaboration with the neurosurgery department, we explored potential delayed epidural space-occupying lesions, which are thought to be quite rare. The neurosurgeon suggested close observation and follow-up in the outpatient clinic. The patient had regular monthly follow-ups with oral medication for pain control and close observation to identify motor weakness and voiding difficulty. A follow-up lumbar spine MRI was obtained at 10 months after the epidural block [Figure 1c and 1d], which showed no evidence of residual epidural hematoma. Although the patient reported mild residual radiating pain on the left side, the overall symptoms had been significantly alleviated.
Figure 1.
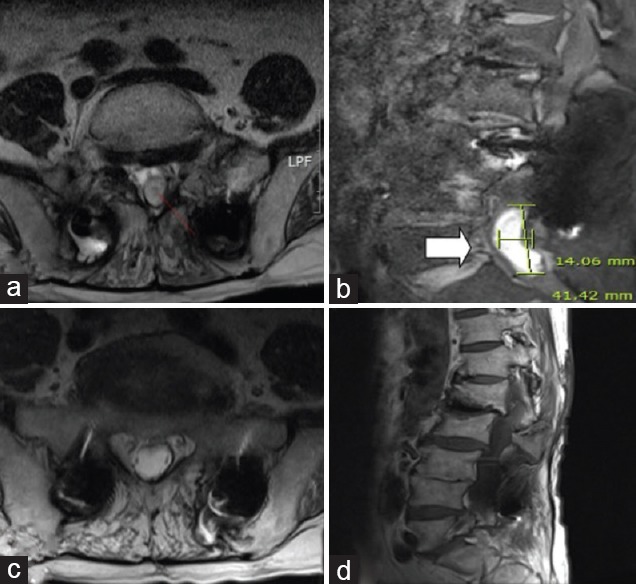
Axial (T2 weighted; a) and sagittal (T1 weighted; b) MRI image after 3 weeks epidural block through the interlaminar approach at L4–L5. Hyperintense mass on T1-weighted (white arrow) pushing on anterior aspect of the spinal cord at the L5-S1 level (white arrow: epidural hematoma). Axial (T2 weighted; c) and sagittal (T1 weighted; d) MRI image after 10 months. The figure shows complete resolution of the hematoma shown in the previous images. MRI: Magnetic resonance imaging.
Epidural steroid injections (ESIs) are generally considered safe and effective for the relief of radicular pain, as well as pain from other spinal conditions. Complications after ESIs are rare, but can include local discomfort, infection, dural puncture, postdural puncture headache, epidural hematoma, and nerve injury. Although the precise incidence of epidural hematomas after ESIs remains unclear, the incidence of epidural hematomas after epidural anesthesia ranges between 1/150,000 and 1/220,000. Spinal canal is a confined space; an expanding space-occupying lesion may develop which may compress the contents of the spinal canal and can lead to catastrophic nerve ischemia such as permanent neurologic damage.[2] Thus, epidural hematomas can cause irreversible damage. It is therefore important to rule out spinal cord compression caused by an epidural hematoma.[3] If decompression is performed within 24 h of the initial symptoms, nerve injury can be minimized. The volume of the hematoma may play an important role in neurologic recovery, but this can vary depending on the relative size of the individual's spinal canal.
The American Society of Regional Anesthesia announced that prostacyclin (PGI2) analogs, such as beraprost, should be discontinued at least 5 days before spinal procedures.[4] Complications secondary to the ESI are associated with two key factors: preexisting severe spinal stenosis and a history of chronic anticoagulation treatment. Anatomically, a reduction in the spinal canal space secondary to stenosis can increase the risk of compression of surrounding structures, and epidural fibrosis associated with spinal stenosis can cause bleeding.[5] In addition, an epidural scar in postspinal surgery syndrome is a possible etiology of epidural hematoma. Furthermore, the fragility of epidural venous plexus is responsible for increasing bleeding tendency.
Initially, our patient was administered multiple anticoagulation agents, but just prior to the epidural block, he was administered beraprost only. In some cases, the shape of the hematoma is associated with the rate of spontaneous recovery. Nevertheless, the amount of hematoma cannot be used as a predictive factor for treatment. Immediate surgical decompression may not be required if neuroimaging and clinical examinations suggest that spinal epidural hematoma could resolve spontaneously. A cause of spontaneously resolved epidural hematoma is resorption of leaked epidural venous plexus. Conservative treatment may be considered in epidural hematoma patients without significant neurological deficits.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Ning-Ning Wang
REFERENCES
- 1.Desai MJ, Dua S. Perineural hematoma following lumbar transforaminal steroid injection causing acute-on-chronic lumbar radiculopathy: A case report. Pain Pract. 2014;14:271–7. doi: 10.1111/papr.12047. doi: 10.1111/papr.12047. [DOI] [PubMed] [Google Scholar]
- 2.Page J, Moisi M, Oskouian RJ. Lumbar epidural hematoma following interlaminar fluoroscopically guided epidural steroid injection. Reg Anesth Pain Med. 2016;41:402–4. doi: 10.1097/AAP.0000000000000387. doi: 10.1097/aap.0000000000000387. [DOI] [PubMed] [Google Scholar]
- 3.Lee MH, Song JH, Lee DI, Ahn HS, Park JW, Cha YD, et al. Newly developed urinary retention and motor weakness of lower extremities in a postherpetic neuralgia patient. Korean J Pain. 2013;26:76–9. doi: 10.3344/kjp.2013.26.1.76. doi: 10.3344/kjp.2013.26.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horlocker TT, Wedel DJ, Rowlingson JC, Enneking FK, Kopp SL, Benzon HT, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Third Edition) Reg Anesth Pain Med. 2010;35:64–101. doi: 10.1097/aap.0b013e3181c15c70. doi: 10.1016/s1084-208x(99)80031-7. [DOI] [PubMed] [Google Scholar]
- 5.Gungor S, Aiyer R. Epidural hematoma development contralateral to dura after lumbar transforaminal epidural steroid injection. Pain Manag. 2017;7:367–75. doi: 10.2217/pmt-2017-0012. doi: 10.2217/pmt-2017-0012. [DOI] [PubMed] [Google Scholar]


